Abstract
Background
Osteogenesis imperfecta (OI) is a heterogeneous connective tissue disorder characterized by increased bone fragility and a series of extraskeletal manifestations. Approximately 90 % of OI cases are caused by type I collagen variants encoded by the collagen type I alpha 1 (COL1A1) or type I alpha 2 (COL1A2) gene. Lumbar Scheuermann’s disease is an atypical type of Scheuermann’s disease accompanied by Schmorl’s nodes and irregular endplates but without pronounced kyphosis. Although the etiology of Scheuermann’s disease is unclear, genetic and environmental factors are likely.
Case presentation
Here, we report a 32-year-old male patient who experienced multiple brittle fractures. Gene sequencing revealed a heterozygous mutation, c.4048G > A (p.G1350S), in the COL1A2 gene, and the patient was diagnosed with OI. Magnetic resonance imaging of his thoracolumbar spine revealed multiple Schmorl’s nodes.
Conclusions
This is the first reported case of OI coexisting with the spinal presentation of Scheuermann’s disease. It is speculated that the COL1A2 gene mutation might be an underlying novel genetic cause of Scheuermann’s disease. In conclusion, this case demonstrates the relationship between Scheuermann’s disease and OI for the first time and enriches the genotype-phenotype spectrum of OI.
Similar content being viewed by others
Background
Osteogenesis imperfecta (OI), also known as brittle bone disease, is a heritable skeletal dysplasia characterized by reduced bone mass, susceptibility to fracture, and variable associated connective tissue disorders. Extraskeletal manifestations include blue sclerae, hearing loss, dentinogenesis imperfecta, muscle weakness, scoliosis, joint laxity, easy bruising, and cardiac valve abnormalities [1]. Approximately 90 % of OI cases are caused by mutations in the type I alpha 1 (COL1A1) or type I alpha 2 (COL1A2) gene, which encode the α1 and α2 chains of type I collagen, respectively. Type I collagen is the most abundant protein present in the bone, skin, and tendon, and OI has become more fully understood as a predominantly collagen-related disorder [2].
Scheuermann’s disease, also known as Scheuermann kyphosis, is an osteochondrosis of the spine first described in 1921 [3]. Classic Scheuermann’s disease (type I) is characterized by painful, fixed, dorsal kyphosis occurring in adolescents, and radiographic manifestations include vertebral wedging, irregularity of the vertebral endplate, and Schmorl’s nodes [4]. In 1987, Blumenthal et al. first proposed lumbar Scheuermann’s disease (type II or atypical), which is characterized by Schmorl’s nodes and irregularity of the vertebral endplate but without severe clinical kyphosis [5]. The etiology of Scheuermann’s disease remains unclear, though it may be caused by excessive mechanical stress on a weakened vertebral endplate with defective growth. A hereditary component is considered to be a contributing factor [6].
Here, we report a patient with OI caused by a heterozygous mutation in the COL1A2 gene (NM_000089): c.4048G > A (p.G1350S). Imaging of the thoracolumbar spine showed the characteristics of Scheuermann’s disease. To our knowledge, this is the first reported case of OI with Scheuermann’s disease presentation. The detected COL1A2 gene mutation might be an underlying novel genetic cause of Scheuermann’s disease.
Case Presentation
A 32-year-old man who experienced a recurrent fracture after sudden syncope was admitted to the First Hospital of China Medical University. Six months before the current time, he had sudden syncope while lying in bed; he felt low back pain after regaining consciousness. A computed tomography (CT) scan in the local hospital indicated multiple thoracolumbar fractures, and he was treated with external belt fixation. One month prior, he experienced another sudden syncope episode when he while sitting in the driver’s seat but before driving; he felt pain in his left shoulder upon waking. X-ray analysis indicated multiple fractures of the left proximal humerus, and he was treated with external fixation. He was then admitted to our hospital for further examination.
Laboratory assessment revealed elevated β-C-terminal telopeptides of type I collagen (β-CTX) (981.8 pg/ml; normal range<584 pg/ml) and N-terminal propeptides of type I collagen (P1NP) (81.93 ng/ml; normal range 20.00–80.00 ng/ml) and decreased 25(OH)D3 (12.99 ng/ml); serum calcium (2.3 mmol/L), phosphorus (1.27 mmol/L), magnesium (0.96 mmol/L), alkaline phosphatase (ALP) (93 U/L; normal range 35–100 U/L) and parathyroid hormone (PTH) (24.92 pg/ml; normal range 15.00–65.00 pg/ml) levels were normal. HLA-B27, arterial blood gas, kidney function, and liver function were all within normal ranges.
X-ray radiographs of the skull, bilateral hands, left shoulder joint, and bilateral hips were performed. The skull image revealed a suspicious light transmission shadow at the left frontal bone. A bone island was detected in the left thumb proximal phalanx. The bilateral hips showed mild degenerative changes, and a comminuted fracture of the left greater tuberosity of the humerus were observed on X-ray and CT scans of the left shoulder joint. Magnetic resonance imaging (MRI) of thoracic and lumbar vertebrae is shown in Fig. 1, revealing L3 vertebral compression fracture, local kyphosis, spinal canal stenosis, and cauda equina compression. Vertebral endplate alterations were found in L1 to S1, and L2-S1 disc bulges and slight L4-S1 disc protrusions were noted. Schmorl’s nodes were observed in multiple thoracic and lumbar vertebrae (T8, T12, L1, and L5). Although bone mineral density (BMD) examined by dual-energy X-ray absorptiometry (DXA) of the hip joint was normal, the L2 (0.820 g/cm2, Z-score − 1.4) and L4 (0.877 g/cm2, Z-score − 1.7) BMD values were low.
Magnetic resonance imaging (MRI) of the thoracolumbar spine. L3 vertebral compression fracture, local kyphosis, spinal canal stenosis, and cauda equina compression were observed. Vertebral endplate alterations were found in L1 to S1, and L2-S1 disc bulges and slight L4-S1 disc protrusions were noted. Schmorl’s nodes were observed in multiple thoracic and lumbar vertebrae (T8, T12, L1, and L5). (a) T1WI of the thoracic vertebra. (b) T2WI of the thoracic vertebra. (c) T1WI of the lumbar vertebra. (d) T2WI of the thoracic vertebra. T1WI, T1-weighted images; T2WI, T2-weighted images
The electrocardiogram performed indicated sinus tachycardia, and his heart rate was 107 beats/min. Cardiac ultrasound showed ventricular septum hypertrophy (9–11 mm), but left ventricular systolic function was normal in the resting state. CT angiography of the head and neck arteries indicated thinning of the right vertebral artery.
The patient had a 4-year history of hypertension. The patient had not suffered from any fracture in the past. His father had hypertension and cerebral thrombosis, and he had a 9-year-old son with Kawasaki disease. His mother and sister were healthy. The patient presented with normal stature and appearance (height, 173 cm; weight, 72 kg; BMI, 24 kg/m2; lack of blue sclera). The patient also had normal teeth and hearing, and no obvious kyphosis was observed.
Genetic testing and mutation analysis
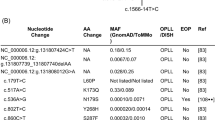
Blood samples were collected from the patient and his family members, and genomic DNA was extracted using a blood extraction kit (Tian Jing Biochemical Technology Beijing, Ltd.). Gene regions, including splicing and coding regions of exons, of a panel of genes associated with bone metabolism were amplified by PCR and then sequenced using the Illumina NextSeq 500 system (Illumina, San Diego, CA, USA). Variations were confirmed by Sanger sequencing (ABI 3730, Applied Biosystems, Foster City, CA, USA). This analysis revealed a heterozygous mutation in COL1A2 (NM_000089; c.4048G > A, (p.G1350S)) in the proband. Family investigation revealed that the proband’s sister and her daughter (his niece) carry this mutation. The proband’s sister was found to be an asymptomatic heterozygous carrier, and the niece previously experienced a fracture of the ankle and had mild dentinogenesis imperfecta without blue sclera (Fig. 2). Predictions for the c.4048G > A mutation in COL1A2 are as follows: PolyPhen2 (Probably damaging, score = 1), FATHMM (Tolerated, score=-1.11), SIFT (Deleterious, score = 0.002) and PROVEAN (Deleterious, score=-4.84).
Pedigree and genetic analysis of the COL1A2 gene in the proband and his family. (a) Pedigree. (b) Mutation analysis revealed a heterozygous mutation of the COL1A2 gene, c.4048G > A (p.G1350S), in the proband (II-4). The proband’s sister (II-1) and her daughter (III-1) harbor the same mutation. The proband’s sister was an asymptomatic heterozygous carrier. The sister’s daughter had mild dentinogenesis imperfecta
Discussion and conclusion
Here, we describe a patient with OI caused by a heterozygous mutation in the COL1A2 gene (NM_000089): c.4048G > A, (p.G1350S). Imaging of the spine showed the characteristics of Scheuermann’s disease.
OI, which is commonly known as brittle bone disease, is a relatively rare connective tissue disorder with significant bone manifestations. The prevalence of OI is one in 15–20,000 births [2]. Approximately 90 % of OI cases are caused by mutations in the COL1A1 or COL1A2 gene, leading to a decreased amount of normal type I collagen or production of type I collagen with abnormal structure. Type I collagen is the main protein component of the bone, skin, ligament, tendon, and many other connective tissues. Type I collagen is a heterotrimer containing two α1(I) chains and one α2(I) chain. It is synthesized as a procollagen molecule, and each proα(I) chain contains a typical triple-helical domain of more than 1,000 residues, consisting of a repeating Gly–Xaa–Yaa sequence, which is flanked by two globular extensions, the amino (N-) and carboxyl (C-) terminal propeptides. The two-terminal propeptides are cleaved after the triple helix is formed. Quantitative type I collagen defects often lead to mild OI, whereas structural defects can cause moderate to severe OI. The most common mutation causing structural defects is a single-nucleotide variant resulting in glycine replacement in the essential Gly–Xaa–Yaa triplets [1]. In the present case, mutation of the COL1A2 gene occurred at nucleotide 4048, leading to glycine to serine alteration at p.1350, which is located in the C-terminal propeptide region (p.1120-p.1366). Fewer than 5 % of mutations occur in the C-propeptide domain of procollagen [7]. Once the C-propeptide trimer is folded, the triple-helical region folds in a zipper-like manner toward the N-terminus [8]. A previous study showed that the C-terminal propeptide of proα2(I) is crucial for efficient assembly of type I procollagen heterotrimers [7]. Compared with the proα1(I)-C-propeptide, pathogenic proα2(I)-C-propeptide variants are less common and generally associated with a milder form of OI. Cultured dermal fibroblast cells from patients with pathogenic proα2(I)-C-propeptide synthesize proα2(I) chains that are slow to assemble with proα1(I) chains to form heterotrimers and are retained intracellularly, which might be exposed to altered posttranslational modification. Some alterations, such as c.3952_3953 ins T and c.3487 T > C, lead to the uncharacteristic formation of proα1(I) homotrimers [9]. Compared with the heterotrimer, fiber formation by the homotrimer is impaired, with increased resistance to proteinases [8]. Overall, the mechanisms by which C-propeptide defects cause OI are not well understood. Possible explanations include a reduced type I collagen content in the extracellular matrix, delayed chain initiation and altered posttranslational modification of type I collagen, leading to decreased bone mineralization and bone strength; misfolded type I procollagen heterotrimers can be partly retained in cells, accumulating and increasing endoplasmic reticulum stress [7]. In the present case, the patient’s height was normal; despite generally normal bone imaging, he had multiple brittle fractures. Both heterozygous carriers, the patient’s sister did not exhibit any phenotype of OI, though her daughter experienced one fracture and had mild dentinogenesis imperfecta. Therefore, the COL1A2 (c.4048G > A) mutation appears to be disease causing and result in mild type I OI in this pedigree.
Thus far, four cases of COL1A2 c.G4048A have been reported [10,11,12]. Yasuhiro Hamatani et al. described a 53-year-old male patient with the COL1A2 c.G4048A mutation; diagnoses were OI and mucopolysaccharidosis type (MPS) III, though no gene mutation associated with MPS was discovered. The patient had a short stature, scoliosis, bone fractures, severe mitral regurgitation, and heart failure. Pathological analysis revealed acidic mucopolysaccharide accumulation and relatively few clumps of collagen fibers in the myocardial interstitium, valves, and aorta [10]. Thickening of the interventricular septum was also found in our patient. Nevertheless, considering a 4-year history of hypertension, it is unclear whether this change is related to the type I collagen variant. Huanzheng Li et al. used second-generation sequencing to carry out mutation detection and prenatal diagnosis in an OI family with COL1A2 c.G4048A. The proband had a short stature, blue sclera, and fragility fractures. In contrast, our patient did not have a short stature or blue sclera, different from the above two cases. Another two cases (patient numbers #0001692 and #0002869) are present in Osteogenesis Imperfecta Variant Database (https://www.le.ac.uk/), though the related phenotypes are not reported. One patient (#0001692) was diagnosed with type I OI; however, changes were not found in the affected daughter. Therefore, the COL1A2 c.G4048A mutation results in heterogeneous clinical manifestations in different families and different individuals in a given family.
As early as 1921, Scheuermann described a rigid kyphosis deformity of the thoracic or thoracolumbar spine, known as Scheuermann’s disease [3]. The prevalence of Scheuermann’s disease varies widely in different regions, ranging between 0.4 and 10 % [13]. Although the etiology of Scheuermann’s disease remains unknown, it shows a familial tendency, but the genetic pattern is not clear. Scheuermann’s disease may involve autosomal dominant inheritance. Some environmental factors, such as excess mechanical stress, might also play a role [4]. Lumber Scheuermann’s disease, also known as atypical Scheuermann’s disease or type II Scheuermann’s disease, was first described by Greene et al. in 1987 [5] and is characterized by significant Schmorl’s nodes and endplate irregularity at the thoracolumbar junction without severe clinical kyphosis [14]. A multicenter study reported that the prevalence of the lumbar type in Europe is 8 %, with no significant difference between the sexes [15]. Nevertheless, the prevalence in China has yet to be determined. Schmorl’s node is a herniation of the nucleus pulposus through the endplate into the adjacent vertebral body [16]. The primary function of the vertebral endplate, which is composed of a cartilaginous and an osseous component, is to prevent the intervertebral disc nucleus pulposus from being embedded in the vertebral body and at the same time has the effect of balancing and dispersing stress [17]. Histological studies of Scheuermann’s disease have revealed disorganized endochondral ossification, reduced collagen levels, and increased mucopolysaccharide levels in the vertebral endplate [4]. Some candidate pathogenic genes resulting in Scheuermann’s disease have been reported. For instance, a patient harboring an Arg75-Cys mutation in the collagen type II alpha 1 (COL2A1) gene was found to experience childhood-onset progressive osteoarthritis and vertebral changes, similar to Scheuermann’s disease [18]. Another mutation in the COL2A1 gene (c.1636G > A, p.G546S) was detected in a girl presenting with hip dysplasia and Scheuermann’s osteochondritis [19]. The tryptophan allele of the collagen type IX alpha 3 (COL9A3) gene has also been associated with Scheuermann’s disease and intervertebral disk degeneration [20]. Bertrand Isidor et al. reported a boy with a de novo deletion of the Cullin 4B (CUL4B) gene, mutation of which commonly leads to syndromic X-linked mental retardation (XLMR). In addition to classic presentations of XLMR, such as mental retardation, minor facial anomalies, short stature, hypogonadism, and ataxia, the boy also displayed vertebral anomalies consistent with Scheuermann’s disease and aortic valvular dysplasia, which were new findings [21]. Although an association between Scheuermann’s disease and COL1A1 and COL1A2 was suspected, linkage analysis of three pedigrees failed to identify a relationship [22].
OI’ s spinal manifestations include scoliosis, kyphosis, craniocervical junction abnormalities, and lumbosacral pathology [23]. To our knowledge, presentations of Scheuermann’s disease have not been previously reported in OI. The COL1A2 c.G4048A gene mutation may hamper the normal formation of type I collagen, affecting the ratio of mucopolysaccharide to collagen and rendering the defective endplates more prone to herniation. Therefore, it is speculated that a fraction of Scheuermann’s disease cases might have underlying dysplasia of bone or cartilage. As a form of skeletal dysplasia, OI might contribute to the occurrence and development of Scheuermann’s disease. Previous studies have indicated that Scheuermann’s disease has a strong association with inheritance, however, related pathogenic genes have not been fully uncovered. With the development of gene sequencing techniques, the pathogenic genes involved in Scheuermann’s disease warrant further study, which helps deepen our understanding of this disease.
We diagnosed this OI patient with Scheuermann’s disease presentation based on multidisciplinary cooperation, including endocrinology, orthopedics, and imaging. Although abnormal fragility fractures may suggest underlying skeletal dysplasia, they might not be given sufficient attention, especially if the fractures are not severe. This case report indicates that it is necessary to pay attention to a history of fragility fractures coexisting with abnormal bone imaging findings. If possible, a detailed examination should be carried out. Strengthening multidisciplinary cooperation may be helpful for the diagnosis and treatment of diseases.
There are some limitations to this article. First, we did not perform lumbar MRI for other family members. Second, experiments using cells to explore the function of the mutant protein were lacking. Therefore, we report this patient as a case report, and further investigation is necessary.
In conclusion, we report an OI patient with the heterozygous c.4048G > A (p.G1350S) mutation in the COL1A2 gene who at the same time exhibited Scheuermann’s disease presentation. This is the first study to reveal the relationship between OI and Scheuermann’s disease. This case enriches the phenotype of OI and offers new insight into the genetic basis of Scheuermann’s disease.
Availability of data and materials
The authors declare that all data used during the study appear in the submitted article.
Abbreviations
- OI:
-
Osteogenesis imperfecta
- COL1A1:
-
Collagen type I alpha 1
- COL1A2:
-
Collagen type I alpha 2
- MRI:
-
Magnetic resonance imaging
- CT:
-
Computed tomography
- β-CTX:
-
β-C-terminal telopeptides of type I collagen
- P1NP:
-
N-terminal propeptides of type I collagen
- ALP:
-
Alkaline phosphatase
- PTH:
-
Parathyroid hormone
- BMD:
-
Bone mineral density
- DXA:
-
Dual-energy X-ray absorptiometry
- MPS:
-
Mucopolysaccharidosis
- COL2A1:
-
Collagen type II alpha 1
- COL9A3:
-
Collagen type IX alpha 3
- CUL4B:
-
Cullin 4B
- XLMR:
-
X-linked mental retardation
References
Marini JC, Forlino A, Bächinger HP, Bishop NJ, Byers PH, Paepe A, Fassier F, Fratzl-Zelman N, Kozloff KM, Krakow D, et al. Osteogenesis imperfecta. Nature reviews Disease primers. 2017;3:17052.
Forlino A, Marini JC. Osteogenesis imperfecta. Lancet. 2016;387(10028):1657–71.
Scheuermann HW. The classic: kyphosis dorsalis juvenilis. Clinical orthopaedics and related research 1977(128):5–7.
Palazzo C, Sailhan F, Revel M. Scheuermann’s disease: an update. Joint bone spine. 2014;81(3):209–14.
Blumenthal SL, Roach J, Herring JA. Lumbar Scheuermann’s. A clinical series and classification. Spine. 1987;12(9):929–32.
Damborg F, Engell V, Nielsen J, Kyvik KO, Andersen M, Thomsen K. Genetic epidemiology of Scheuermann’s disease. Acta Orthop. 2011;82(5):602–5.
Symoens S, Hulmes DJ, Bourhis JM, Coucke PJ, De Paepe A, Malfait F. Type I procollagen C-propeptide defects: study of genotype-phenotype correlation and predictive role of crystal structure. Hum Mutat. 2014;35(11):1330–41.
Sharma U, Carrique L, Vadon-Le Goff S, Mariano N, Georges RN, Delolme F, Koivunen P, Myllyharju J, Moali C, Aghajari N, et al. Structural basis of homo- and heterotrimerization of collagen I. Nature communications. 2017;8:14671.
Pace JM, Wiese M, Drenguis AS, Kuznetsova N, Leikin S, Schwarze U, Chen D, Mooney SH, Unger S, Byers PH. Defective C-propeptides of the proalpha2(I) chain of type I procollagen impede molecular assembly and result in osteogenesis imperfecta. J Biol Chem. 2008;283(23):16061–7.
Hamatani Y, Nakashima J, Ohta-Ogo K, Amaki M, Koga M, Aoyama D, Marume K, Sawada K, Nakashima Y, Shibata A, et al. Mitral Regurgitation and Heart Failure as the First Presentation in a Patient with Features of Two Connective Tissue Disorders: A Rare Combination of Mucopolysaccharidosis and Osteogenesis Imperfecta? Intern Med. 2018;57(15):2209–15.
Wang Y, Cui Y, Zhou X, Han J. Development of a high-throughput resequencing array for the detection of pathogenic mutations in osteogenesis imperfecta. PLoS One. 2015;10(3):e0119553.
Li H, Tang S, Chen C, Xiang Y, Wu J, Dong X, Wu R, Xu X. Molecular and prenatal diagnosis of a family with Osteogenesis imperfect by next generation sequencing. Chinese Journal of Birth Health Heredity. 2019;27(06):654–6.
Makurthou AA, Oei L, El Saddy S, Breda SJ, Castaño-Betancourt MC, Hofman A, van Meurs JB, Uitterlinden AG, Rivadeneira F, Oei EH. Scheuermann disease: evaluation of radiological criteria and population prevalence. Spine. 2013;38(19):1690–4.
Wenger DR, Frick SL. Scheuermann kyphosis. Spine. 1999;24(24):2630–9.
Armbrecht G, Felsenberg D, Ganswindt M, Lunt M, Kaptoge SK, Abendroth K, Aroso A, Banzer D, Bhalla AK, Dequeker J, et al. Vertebral Scheuermann’s disease in Europe: prevalence, geographic variation and radiological correlates in men and women aged 50 and over. Osteoporos Int. 2015;26(10):2509–19.
Kyere KA, Than KD, Wang AC, Rahman SU, Valdivia-Valdivia JM, La Marca F, Park P. Schmorl’s nodes. European spine journal: official publication of the European Spine Society the European Spinal Deformity Society the European Section of the Cervical Spine Research Society. 2012;21(11):2115–21.
Wang Y, Videman T, Battié MC. Lumbar vertebral endplate lesions: prevalence, classification, and association with age. Spine. 2012;37(17):1432–9.
Löppönen T, Körkkö J, Lundan T, Seppänen U, Ignatius J, Kääriäinen H: Childhood-onset osteoarthritis, tall stature, and sensorineural hearing loss associated with Arg75-Cys mutation in procollagen type II gene (COL2A1). Arthritis and rheumatism 2004, 51(6):925–932.
Al Kaissi A, Laccone F, Karner C, Ganger R, Klaushofer K, Grill F. [Hip dysplasia and spinal osteochondritis (Scheuermann’s disease) in a girl with type II manifesting collagenopathy]. Der Orthopade. 2013;42(11):963–8.
Karppinen J, Pääkkö E, Paassilta P, Lohiniva J, Kurunlahti M, Tervonen O, Nieminen P, Göring HH, Malmivaara A, Vanharanta H, et al. Radiologic phenotypes in lumbar MR imaging for a gene defect in the COL9A3 gene of type IX collagen. Radiology. 2003;227(1):143–8.
Isidor B, Pichon O, Baron S, David A, Le Caignec C. Deletion of the CUL4B gene in a boy with mental retardation, minor facial anomalies, short stature, hypogonadism, and ataxia. American journal of medical genetics Part A. 2010;152a(1):175–80.
McKenzie L, Sillence D. Familial Scheuermann disease: a genetic and linkage study. J Med Genet. 1992;29(1):41–5.
Wallace MJ, Kruse RW, Shah SA. The Spine in Patients With Osteogenesis Imperfecta. J Am Acad Orthop Surg. 2017;25(2):100–9.
Acknowledgements
This work was supported by the Distinguished Professor at the Educational Department of Liaoning Province (No. [2015]153). We thank the patient and his family for their consent to publish this case report.
Funding
This work was supported by the Distinguished Professor at the Educational Department of Liaoning Province (No. [2015]153).
Author information
Authors and Affiliations
Contributions
WSW and TXC collected the patient’s data. WSW prepared the first draft of the manuscript. LYS, TXC, and SZY participated in the diagnostic assessment and treatment of the patient. LSB and ZHY performed the imaging assessment. WXL helped with the genetic analysis and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from all individuals included in the study for participation as well as publication of this report and any accompanying images.
Competing interests
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Wang, X., Teng, X. et al. Lumbar Scheuermann’s disease found in a patient with osteogenesis imperfecta (OI) caused by a heterozygous mutation in COL1A2 (c.4048G > A): a case report. BMC Musculoskelet Disord 22, 525 (2021). https://doi.org/10.1186/s12891-021-04401-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-021-04401-7