Abstract
Background
Delirium is a common complication of hip surgery patients. It is necessary to investigate the epidemiological characteristics and related risk factors of delirium after hip fracture surgery, to provide evidence supports for the prevention and management of delirium.
Methods
Hip fracture patients admitted to our hospital for surgical treatment from March 2018 to March 2020 were identified as participants. The characteristics and laboratory examinations in patients with and without postoperative delirium were compared and analyzed. Logistic regression analyses were conducted to ascertain the independent risk factors, and the area under the curve (AUC) were calculated to analyze the predictive value.
Results
A total of 568 postoperative patients with hip fracture were included, the incidence of delirium in postoperative patients with hip fracture was 14.44 %. The preoperative albumin (OR 4.382, 2.501 ~ 5.538), history of delirium (OR 2.197, 1.094 ~ 3.253), TSH (OR1.245, 1.077 ~ 1.638), the resting score on the first postoperative day (OR1.235, 0.944 ~ 1.506) and age(OR1.185, 0.065 ~ 1.814) were the independent risk factors for the postoperative delirium in patients with hip fracture(all p < 0.05). The AUC of albumin, history of delirium, TSH, the resting score on the first postoperative day and age were 0.794, 0.754, 0.746, 0.721 and 0.689 respectively.
Conclusions
The incidence of delirium in postoperative patients with hip fracture is rather high, especially for patients with old age and history of delirium. Monitoring albumin, TSH and resting score may be beneficial to the management of postoperative delirium.
Similar content being viewed by others
Background
Hip fracture is a very common kind of disease in clinically elderly patients. According to reports, by 2050, the number of patients with hip fractures each year around the world is about 4.5 million[1, 2]. The incidence of hip fractures in the elderly has increased year by year, with female patients accounting for 75 % of all hip fracture patients[3]. This has also brought great challenges and pressures to clinical medical workers throughout world. How to treat and care for these patients correctly and effectively has become a top priority for clinical research. Surgical treatment has become the first choice for the treatment of hip fracture patients[4]. But at the same time, surgical treatment has also brought a series of postoperative complications, which needs to be highly valued and prevented by us.
Delirium is a very common postoperative complication in elderly patients with hip fractures[5]. Its main manifestations are unconsciousness, difficulty concentrating, disorder of perception and thinking and disturbance of sleep[6]. Among elderly hip fracture patients, the incidence of delirium is 20–50 %[7]. Delirium may cause huge adverse impact on patients, which may extend the postoperative recovery of patients, increase the medical expense and burden, and prolong the length of hospital stay, and even increase the mortality[8]. Therefore, the prevention and treatment of postoperative delirium are crucial to the prognosis of patients with hip fracture.
There are several studies[9,10,11] on the possible risk factors for postoperative delirium in elderly hip fracture patients, but the results remain inconsistent or even conflicting. There are many possible risk factors reported, including age, education background, alcohol consumption, anesthesia and blood loss etc. However, the independent risk factors for the postoperative are not yet clear, which needs further verifications. Therefore, we attempted to conduct this retrospective study to identify the potentially relevant risk factors for the postoperative delirium in patients with hip fracture.
Methods
Ethical concerns
This study has been approved by the Ethics Committee of our Hospital (approval number: 201800387-2a), all patients signed the written informed consent.
Patients
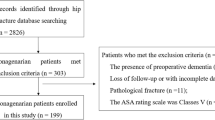
The hip fracture patients admitted to our hospital for surgical treatment from March 2018 to March 2020 were identified as study population. The selection criteria for patients were: (1) age > 18 years; (2) the patients undergone surgical treatment for hip fracture; (3) the patient was willing to participate in this study and signed the written inform consent. The exclusion criteria were: (1) multiple fractures rather than only hip fracture; (2) pathological fractures caused by tumors; (3) the hip fractures more than 20 days from the time of injury; (4) patients with dementia or known mental illness; (5) patients with aphasia and hearing impairment; (6) Patients who did not sign informed consent or lost follow-up.
Laboratory examination
All patients undergone preoperative laboratory examinations. The items of laboratory examinations included blood type, albumin, blood sugar, blood creatinine, urea nitrogen, thyroxine (T4), serum thyroid stimulating hormone (TSH), coagulation function, blood gas analysis, electrocardiogram, chest radiography, echocardiography and vascular ultrasound of both lower extremities.
Delirium assessment
The diagnosis of delirium referred to the standards established by the the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association, and we used the consciousness assessment method (CAM)[12] as a diagnostic tool. CAM included the following four aspects: (1) acute onset, mood changes; (2) inattention; (3) disordered thinking; (4) changes in consciousness level. If the patient has items 1 and 2 at the same time, plus either 3 or 4, then delirium can be diagnosed. All patients who met the inclusion criteria were divided into two groups according to whether postoperative delirium occurred: delirium group and non-delirium group.
Outcome assessment and collection
The baseline collected information included the age, weight, height, time of injury, the complicated diseases such as hypertension, diabetes mellitus et al. All patients underwent surgery under general anesthesia or lumbar anesthesia, and postoperative intravenous analgesia (PCA) was used. Postoperative assessment was performed by an anesthesiologist and a geriatrician. At 4 pm on the first and second days after surgery, CAM were used to assess whether delirium occurred and its severity, and visual analog score (VAS) was used to evaluate the pain of rest and motion status.
Statistical analysis
SPSS 22.0 statistical software was used for data analysis in this study, and t-test was used for the comparison of continuous data between two groups; chi-square test was used for the comparison of categorical data between two groups. The independent risk factors were screened out using logistic regression analysis, and we drew the receiver operating curve (ROC) and calculated the area under the curve (AUC) to analyze its predictive value. p < 0.05 was considered that the difference was statistically significant.
Results
The information of patients
A total of 568 postoperative patients with hip fracture were included, of which 82 patients had delirium and 486 patients did not have delirium. The incidence of delirium in postoperative patients with hip fracture was 14.44 %. As Table 1 presented, there were significant difference on the age, history of delirium between patients with delirium and without delirium (all p < 0.05). And there were significant differences on the gender, BMI, hypertension, diabetes mellitus, hyperlipidemia, type of fracture, preoperative ADL score and the method of anesthesia between two groups (all p > 0.05).
The comparison of preoperative laboratory examination and postoperative VAS score.
As Table 2 presented, there were significant difference on the preoperative albumin, TSH and the rest score on the first postoperative day (all p < 0.05). There were no significant differences on the preoperative hemoglobin, blood sugar, creatinine, urea nitrogen, T3, T4, FT3, FT4, PaO2, PaCO2, the motion score on the first postoperative day and the VAS on the second postoperative day between two groups(all p > 0.05).
The risk factors for the post-operative delirium in patients with hip fracture.
As Table 3 showed, logistic regression analyses indicated that the preoperative albumin (OR 4.382, 2.501 ~ 5.538), history of delirium (OR 2.197, 1.094 ~ 3.253), TSH (OR1.245, 1.077 ~ 1.638), the resting score on the first postoperative day (OR1.235, 0.944 ~ 1.506) and age(OR1.185, 0.065 ~ 1.814) were the independent risk factors for the postoperative delirium in patients with hip fracture(all p < 0.05).
The predictive value analysis.
Figure 1 presented the ROC of the potential factors for the post-operative delirium in patients with hip fracture. As indicated in Table 4, the AUC of albumin, history of delirium, TSH, the resting score on the first postoperative day and age were 0.794, 0.754, 0.746, 0.721 and 0.689 respectively.
Discussion
Hip fractures seriously endanger the physical and mental health of the elderly and the quality of life[13]. The hip fractures are associated with inability to mobile and a series of complications such as decubitus ulcers, lung infections[14, 15]. At present, for hip fracture patients, surgical treatment, including fracture internal fixation and hip replacement, is the main and preferred method of treatment[16]. However, the surgical treatment itself can also lead to many postoperative complications. Delirium a is one of the most common and serious complications after surgery for hip fracture patients[17]. The pathogenesis of postoperative delirium is very complicated, and so far, it has not been clarified. In recent years, there are many emerging hypotheses, including the central neurotransmitter theory, the brain metabolic level change theory, surgical stress theory and neuroinflammation hypothesis et al[18,19,20]. In this present study, 82 of the 568 patients have postoperative delirium, the incidence of postoperative delirium is14.44 %. Previous study[21] has reported that the incidence of postoperative delirium in elderly patients with hip fracture is about 20.5 %, which is consistent with our findings. And we have found that preoperative albumin, history of delirium, TSH, the resting score on the first postoperative day and age were the independent risk factors for the postoperative delirium in patients with hip fracture. It is suggested that the above risk factors may be the focus of prevention and treatment of delirium during the perioperative period, and preventions and early warning should be performed with target on those risks.
Delirium is an acute brain dysfunction that manifests as distracted attention, declined recognition, disturbances of circadian clock, emotional and mental disorders[22]. Its incidence increases with age, and it can reach 14 % in people over 85 years of age[23]. In the surgical field, patients with hip fractures over 65 years of age have a higher incidence of postoperative delirium[24]. This study also confirmed that age is a risk factor for postoperative delirium. Previous studies[25,26,27] have shown that for every increased year of age, the incidence of delirium increases by 1.13 times. The hip fracture is generally seen in elderly patients, and elderly patients with multiple systemic diseases such as central nervous system degeneration, which are prone to nerve dysfunction after surgical stress. Therefore, the use of clustered perioperative strategies, such as accelerated surgical rehabilitation strategies, has important clinical significance for reducing the incidence of delirium[28].
It’s been reported that about 20–65 % of the elderly have different degrees of albumin deficiency[29, 30]. In addition to maintaining plasma osmotic pressure, binding with various ligands, as well as anticoagulation and maintaining acid-base balance, albumin also has the function of antioxidant, scavenging free radicals and protecting microcirculation[31]. Preoperative hypoalbuminemia directly affects the pharmacological effects of anesthetic drugs, resulting in uncertainty in the dose selection and duration of action, which can directly or indirectly affect postoperative neural function[32]. Consistent with previous reports[33, 34], this study also confirms that preoperative hypoproteinemia is associated with postoperative delirium. This result shows that actively correcting preoperative hypoproteinemia is of great significance for the prevention and treatment of postoperative delirium in patients with hip fracture.
Postoperative pain is closely related to the occurrence of delirium, and good postoperative analgesia is an important measure to prevent delirium[35]. The results of this study indicate that only resting VAS on the first postoperative day is an independent risk factor for delirium. As one of the important noxious stimuli, acute pain can activate a variety of neurotransmitter transmission pathways, produce a synergistic effect of inflammatory response and oxidative stress response, which may eventually lead to delirium[36]. Therefore, patients with hip fractures should pay attention to pain management and actively implement early multimodal analgesic strategies, such as the use of nerve block, local infiltration of wound anesthesia, etc. Besides, reasonable sedation should be implemented. For hospitals with monitoring conditions, using dexmedetomidine in small doses can relieve anxiety and exert its advantages in reducing delirium.
Studies[37, 38] on the correlation between subclinical thyroid dysfunction and dementia and cognitive dysfunction suggest that compared with normal thyroid function, patients with subclinical hyperthyroidism (TSH < 0.45 mU/L) has higher risk of cognitive dysfunction within the onset of 5 to 9 years, and subclinical hypothyroidism is not significantly related to cognitive dysfunction. Although there has been no report on the correlation between subclinical thyroid dysfunction and delirium, the results in this study have indicated that subclinical hyperthyroidism may be a risk factor for postoperative delirium. The potential reasons may be that hyperthyroidism can lead to neuronal necrosis and increased oxidative stress, and some target genes of thyroid hormone may be related to the coupling of neurons[39]. Besides, the occurrence of dementia is related to the reduction of choline in the brain[40]. Some studies[41, 42] have found that in patients with untreated hyperthyroidism, the ratio of choline/creatinine in the brain decreases, and it can return to normal after drug treatment. Therefore, TSH should be used as a routine screening indicator for patients with hip fracture.
The following limitations in this present study should be considered. Firstly, our study is a retrospective analysis with a small sample size, some biases may be existed, and it can be underpower to detect the potential risks. Secondly, some other potential risks such as time to surgery, estimated blood loss during the surgery have been reported to be associated with the postoperative delirium, we could not include those factors into analysis due to the lack of information. Further investigations are needed to identify the potential risks and treatment of postoperative delirium.
Conclusions
In conclusion, the prevalence of postoperative delirium in hip fracture patients is relatively high. At the same time, preoperative albumin, history of delirium, TSH, the resting score on the first postoperative day and age were the independent risk factors for the postoperative delirium in patients with hip fracture. Clinicians should correctly assess the patient’s physical state and function of various organs before the operation, improve the patient’s nutritional status. However, given the small size of our study, it’s necessary to conduct more related researches to elucidate the prevention and management of deliriums in clinical settings.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- BMI:
-
Body mass index
- ADL:
-
Ability of daily living
- CAM:
-
Consciousness assessment method
- PCA:
-
Postoperative intravenous analgesia
- VAS:
-
Visual analog score
- ROC:
-
Receiver operating curve
- AUC:
-
Area under the curve
- PaO2 :
-
Partial pressure of oxygen
- PaCO2 :
-
Partial pressure of carbon dioxide
- T3:
-
Triiodothyronine
- T4:
-
Total thyroxine
- FT3:
-
Free triiodothyronine
- FT4:
-
Free thyroxine
- TSH:
-
Thyroid stimulating hormone
References
Guzon-Illescas O, Perez Fernandez E, Crespi Villarias N, Quiros Donate FJ, Pena M, Alonso-Blas C, Garcia-Vadillo A, Mazzucchelli R. Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res. 2019;14(1):203.
Albrecht JS, Al Kibria G, Gruber-Baldini A, Magaziner J. Risk of Mortality in Individuals with Hip Fracture and Traumatic Brain Injury. J Am Geriatr Soc. 2019;67(1):124–7.
Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018;19(1):369.
Jantzen C, Madsen CM, Lauritzen JB, Jorgensen HL. Temporal trends in hip fracture incidence, mortality, and morbidity in Denmark from 1999 to 2012. Acta Orthop. 2018;89(2):170–6.
Lee PJ, Shorten GD. Delirium after hip fracture surgery. J Clin Anesth. 2019;58:119–20.
Yang Y, Zhao X, Dong T, Yang Z, Zhang Q, Zhang Y. Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res. 2017;29(2):115–26.
Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, van der Laan L. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421–30.
Civinini R, Paoli T, Cianferotti L, Cartei A, Boccaccini A, Peris A, Brandi ML, Rostagno C, Innocenti M. Functional outcomes and mortality in geriatric and fragility hip fractures-results of an integrated, multidisciplinary model experienced by the “Florence hip fracture unit. Int Orthop. 2019;43(1):187–92.
Smith TO, Cooper A, Peryer G, Griffiths R, Fox C, Cross J. Factors predicting incidence of post-operative delirium in older people following hip fracture surgery: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2017;32(4):386–96.
Ravi B, Pincus D, Choi S, Jenkinson R, Wasserstein DN, Redelmeier DA. Association of Duration of Surgery With Postoperative Delirium Among Patients Receiving Hip Fracture Repair. JAMA Netw Open. 2019;2(2):e190111.
Patel V, Champaneria R, Dretzke J, Yeung J. Effect of regional versus general anaesthesia on postoperative delirium in elderly patients undergoing surgery for hip fracture: a systematic review. BMJ Open. 2018;8(12):e020757.
McNicoll L, Pisani MA, Ely EW, Gifford D, Inouye SK. Detection of delirium in the intensive care unit: comparison of confusion assessment method for the intensive care unit with confusion assessment method ratings. J Am Geriatr Soc. 2005;53(3):495–500.
Bhandari M, Swiontkowski M. Management of Acute Hip Fracture. N Engl J Med. 2017;377(21):2053–62.
Roberts KC, Brox WT, Jevsevar DS, Sevarino K. Management of hip fractures in the elderly. J Am Acad Orthop Surg. 2015;23(2):131–7.
Sanzone AG. Current Challenges in Pain Management in Hip Fracture Patients. J Orthop Trauma. 2016;30(Suppl 1):1–5.
Tay E. Hip fractures in the elderly: operative versus nonoperative management. Singapore Med J. 2016;57(4):178–81.
de Jong L, van Rijckevorsel V, Raats JW, Klem T, Kuijper TM, Roukema GR. Delirium after hip hemiarthroplasty for proximal femoral fractures in elderly patients: risk factors and clinical outcomes. Clin Interv Aging. 2019;14:427–35.
Zhang X, Tong DK, Ji F, Duan XZ, Liu PZ, Qin S, Xu KH, Di-Li XT. Predictive nomogram for postoperative delirium in elderly patients with a hip fracture. Injury. 2019;50(2):392–7.
Halaas NB, Blennow K, Idland AV, Wyller TB, Raeder J, Frihagen F, Staff AC, Zetterberg H, Watne LO. Neurofilament Light in Serum and Cerebrospinal Fluid of Hip Fracture Patients with Delirium. Dement Geriatr Cogn Disord. 2018;46(5–6):346–57.
Li C, Bai S, Song X. Retrospective study on risk factors associated with postoperative delirium in elderly hip fracture patients. Chinese Journal of Orthopaedics. 2018;38(4):250–6.
Milbrandt EB, Deppen S, Harrison PL, Shintani AK, Speroff T, Stiles RA, Truman B, Bernard GR, Dittus RS, Ely EW. Costs associated with delirium in mechanically ventilated patients. Crit Care Med. 2004;32(4):955–62.
Arshi A, Lai WC, Chen JB, Bukata SV, Stavrakis AI, Zeegen EN. Predictors and Sequelae of Postoperative Delirium in Geriatric Hip Fracture Patients. Geriatr Orthop Surg Rehabil. 2018;9:2151459318814823.
Tao L, Xiaodong X, Qiang M, Jiao L, Xu Z. Prediction of postoperative delirium by comprehensive geriatric assessment among elderly patients with hip fracture. Ir J Med Sci. 2019;188(4):1311–5.
Wang CG, Qin YF, Wan X, Song LC, Li ZJ, Li H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J Orthop Surg Res. 2018;13(1):186.
Abrahamsen B, Laursen HVB, Skjodt MK, Jensen MH, Vestergaard P. Age at hip fracture and life expectancy in Denmark - Secular trends over two decades. Bone. 2020;130:115083.
Arai K, Suzuki N, Murayama T, Kondo N, Otsuka H, Koizumi M, Hosaka N, Fujikawa R, Yanabashi K, Sasage Y, et al. Age at the time of hip fracture in patients with rheumatoid arthritis is 4 years greater than it was 10 years before, but is still younger than that of the general population. Mod Rheumatol. 2020;30(1):64–9.
Aamodt G, Renolen R, Omsland TK, Meyer HE, Rabanal KS, Sogaard AJ. Ethnic differences in risk of hip fracture in Norway: a NOREPOS study. Osteoporos Int 2020.
Bouxsein ML, Zysset P, Gluer CC, McClung M, Biver E, Pierroz DD, Ferrari SL, Target IOFWGoHBSaaT. Perspectives on the non-invasive evaluation of femoral strength in the assessment of hip fracture risk. Osteoporos Int. 2020;31(3):393–408.
Slor CJ, Witlox J, Adamis D, Jansen R, Houdijk APJ, van Gool WA, de Jonghe JFM, Eikelenboom P. The trajectory of C-reactive protein serum levels in older hip fracture patients with postoperative delirium. Int J Geriatr Psychiatry. 2019;34(10):1438–46.
Oh ES, Li M, Fafowora TM, Inouye SK, Chen CH, Rosman LM, Lyketsos CG, Sieber FE, Puhan MA. Preoperative risk factors for postoperative delirium following hip fracture repair: a systematic review. Int J Geriatr Psychiatry. 2015;30(9):900–10.
Hov KR, Berg JP, Frihagen F, Raeder J, Hall R, Wyller TB, Watne LO. Blood-Cerebrospinal Fluid Barrier Integrity in Delirium Determined by Q-Albumin. Dement Geriatr Cogn Disord. 2016;41(3–4):192–8.
Yuan Y, Han YZ, Ji XJ, Shi CM, Li ZQ, Zhou Y, Yang QG, Wang G, Guo XY. [Risk factors associated with delirium for patients with hip fracture under the orthogeriatric unit mode]. Zhonghua Yi Xue Za Zhi. 2018;98(40):3235–9.
Li QH, Yu L, Yu ZW, Fan XL, Yao WX, Ji C, Deng F, Luo XZ, Sun JL. Relation of postoperative serum S100A12 levels to delirium and cognitive dysfunction occurring after hip fracture surgery in elderly patients. Brain Behav. 2019;9(1):e01176.
Shin JE, Kyeong S, Lee JS, Park JY, Lee WS, Kim JJ, Yang KH. A personality trait contributes to the occurrence of postoperative delirium: a prospective study. BMC Psychiatry. 2016;16(1):371.
Bellelli G, Mazzola P, Morandi A, Bruni A, Carnevali L, Corsi M, Zatti G, Zambon A, Corrao G, Olofsson B, et al. Duration of postoperative delirium is an independent predictor of 6-month mortality in older adults after hip fracture. J Am Geriatr Soc. 2014;62(7):1335–40.
Matcuk GR Jr, Mahanty SR, Skalski MR, Patel DB, White EA, Gottsegen CJ. Stress fractures: pathophysiology, clinical presentation, imaging features, and treatment options. Emerg Radiol. 2016;23(4):365–75.
Nomoto S, Kinno R, Ochiai H, Kubota S, Mori Y, Futamura A, Sugimoto A, Kuroda T, Yano S, Murakami H, et al. The relationship between thyroid function and cerebral blood flow in mild cognitive impairment and Alzheimer’s disease. PLoS One. 2019;14(4):e0214676.
Ling XW, Howe TS, Koh JS, Wong MK, Ng AC. Preoperative thyroid dysfunction predicts 30-day postoperative complications in elderly patients with hip fracture. Geriatr Orthop Surg Rehabil. 2013;4(2):43–9.
Noda M. Thyroid Hormone in the CNS: Contribution of Neuron-Glia Interaction. Vitam Horm. 2018;106:313–31.
Shea TB. Choline and phosphatidylcholine may maintain cognitive performance by multiple mechanisms. Am J Clin Nutr. 2019;110(6):1268–9.
Ylilauri MPT, Voutilainen S, Lonnroos E, Virtanen HEK, Tuomainen TP, Salonen JT, Virtanen JK. Associations of dietary choline intake with risk of incident dementia and with cognitive performance: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am J Clin Nutr. 2019;110(6):1416–23.
Strupp BJ, Powers BE, Velazquez R, Ash JA, Kelley CM, Alldred MJ, Strawderman M, Caudill MA, Mufson EJ, Ginsberg SD. Maternal Choline Supplementation: A Potential Prenatal Treatment for Down Syndrome and Alzheimer’s Disease. Curr Alzheimer Res. 2016;13(1):97–106.
Acknowledgements
None.
Funding
This study was funded by Natural Science Foundation of Xinjiang Uygur Autonomous Region(2017D01C287).
Author information
Authors and Affiliations
Contributions
W X, C Z designed research; W X, H M conducted research; W X and W L analyzed data; W X wrote the first draft of manuscript; C Z had primary responsibility for final content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Our study has been approved by the ethics committee of The First Affiliated hospital of XinJiang Medical University (2018101184).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xu, W., Ma, H., Li, W. et al. The risk factors of postoperative delirium in patients with hip fracture: implication for clinical management. BMC Musculoskelet Disord 22, 254 (2021). https://doi.org/10.1186/s12891-021-04091-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-021-04091-1