Abstract
Purpose
The present study aimed to compare the capabilities of preoperative usual and maximal gait speeds in predicting functional recovery in patients who have undergone total hip arthroplasty (THA).
Methods
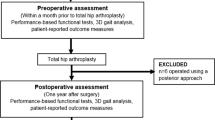
Primary and unilateral THAs were performed in 317 patients, and the proportion of patients who achieved unassisted walking (functional recovery) 5 days postoperatively was recorded as an outcome measure. Preoperative functional assessment included hip pain, leg muscle strength, range of motion (ROM), and gait speed evaluations. The capabilities of preoperative usual and maximal gait speeds in predicting functional recovery were compared based on the areas under the curves (AUCs) of receiver operating characteristic (ROC) curves. Further, ROC curves were constructed using two models: 1. a model of gait speed only and 2. a clinical model including age, sex, leg muscle strength, and ROM.
Results
On the AUCs for predictive ability of functional recovery, maximal gait speed was greater than usual gait speed (0.66 and 0.70, respectively). The AUC for maximal gait speed was as large as that of the clinical model (0.70 and 0.70, respectively).
Conclusion
Our results suggest that maximal gait speed is a simple and useful prognostic indicator of functional recovery in patients who have undergone THA.
Similar content being viewed by others
Introduction
Patients with end-stage osteoarthritis (OA) who undergo total hip arthroplasty (THA) demonstrate reduced pain and improved physical function and health-related quality of life [1]. Owing to rising healthcare-related costs and an increase in the demand for THA, it is necessary to develop a strategy for reducing the length of hospital stay and for the efficient and appropriate discharge of patients after treatment. Poor functional recovery during hospital stay is a common complication following major operations [2]. Preoperative identification of such patients using valid tools enables clinicians to plan postoperative resources accordingly [2, 3].
Conventional factors, such as age, sex, body-mass index (BMI), range of motion (ROM), and muscle strength can only limitedly justify the variance in the postoperative functional recovery among patients [4, 5]; in contrast, performance-based measures may predict functional recovery better than conventional patient factors [6]. In previous studies, it has been reported that functional indicators such as timed up-and-go (TUG) and sit-to-stand tests are useful in predicting postoperative recovery [7,8,9,10,11]. In addition, the Osteoarthritis Research Society International (OARSI) guidelines recommend a 30 s chair-stand test, a 40 m fast-paced walk test, and a stair-climb test as the core set of performance measures for OA patients [12]. However, due to restrictions such as advancing ages of patients and limited spaces for evaluation, all of these evaluations are often difficult to perform.
Evaluation of gait speed does not require a large space and can be performed in a short time even for elderly patients because it requires less time and less burden on the patient than conventional tests [13]. In addition, a recent systematic review reports that a detailed assessment of gait parameters before and after surgery can capture a patient’s functional recovery very clearly [14]. However, many of these studies predict a functional recovery time of two to three months after surgery. Although Oosting et al. [6] reported on the usefulness of usual gait speed for predicting functional recovery early in the postoperative period, the usefulness of maximal gait speed has not been investigated. As mentioned earlier, OARSI recommends assessment of maximal gait speed, and it is not clear whether the usual or maximal gait speed is useful for predicting early functional recovery. By comparing the predictive capabilities of preoperative usual and maximal gait speeds, the present study aimed to clarify the usefulness of gait speed in predicting functional recovery in patients who underwent THA.
Methods
The study protocol was approved by the Ethics Committee of Kitasato University Hospital (permit number: B18–088), and was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Study population
This was a retrospective study. Primary and unilateral THA were performed in 336 patients at our hospital between November 2015 and March 2018. After excluding 11 patients who were unable to walk before surgery and 8 patients with perioperative complications including postoperative cerebral infarction (n = 1), load limitation due to bone vulnerability (n = 2), fractures during surgery (n = 2), and those with deep venous thrombosis that needed treatment early after surgery (n = 3), 317 patients were included in this study.
Data collection
Clinical characteristics
Patient characteristics, including age, gender, BMI, comorbidities, preoperative functional assessment, length of hospital stay, and discharge, were collected from electronic medical records. In addition, time taken to achieve walking over a distance of 50 m with or without a walking aid and the proportion of patients achieving unassisted walking on postoperative day 5 were recorded as outcome measures. Functional recovery was evaluated daily and defined as the ability to walk over a distance of 50 m without human assistance, regardless of the use of a walking aid.
Preoperative functional assessment
Hip pain, knee extensor and hip abductor muscle strength, hip flexion ROM, and gait speed were assessed 1–3 days before operation by one of seven physical therapists who had received training for more than one month. Hip pain on the affected side during walking was assessed using a visual analog scale. Muscle strength was determined by measuring maximum voluntary isometric knee extensor and hip abductor strength on the affected side using a hand-held dynamometer with a restraining belt [15] (μTas; ANIMA, Tokyo, Japan). Measurements were obtained twice, with the highest values expressed as relative to body weight (%BW) used in the analysis. Hip flexion on the affected side was used to evaluate ROM. Usual and maximal gait speeds were measured by timing the patients walking at their usual or maximal pace with any necessary assistive devices over the middle 10 m of a 16-m walkway. A digital stopwatch was used to time subjects as they walked over a 10-m distance. Subjects were provided with 3 m to accelerate and decelerate before and after the test distance. For the usual speed walking trials, they were instructed to walk at their normal comfortable speed. For the maximal speed walking trials, they were asked to walk as fast as they could safely without running. First, usual gait speed was measured, and then, maximal speed was measured. Between each measurement, 30-s rest was taken.
Standard management
A rehabilitation program is shown in Appendix. A standard rehabilitation program comprising weight bearing, as tolerated with a walking aid, was started on the day after surgery, and patients were allowed to eliminate walking aids whenever comfortable. Physical therapy was performed once a day on weekdays, and it included progressively improving walking ability, other functional activities, and walking stairs according to the needs and progress of an individual patient. Patients participated in a progressive program involving range of motion exercises, strengthening exercises, and functional training. Patients were allowed to use analgesics for pain as needed. Patients were discharged from the hospital on consultation with their caregivers, surgeons, nurses, and physical therapists, according to the following criteria: ability to walk independently with a walking aid, and if necessary, climb stairs, remain in a stable medical condition, and exhibit adequate wound healing. Discharge disposition in this study was defined as a rehabilitation facility or home, and the patients were transferred to a rehabilitation facility if they could not achieve the criteria at 1 week after surgery.
Statistical analysis
Cox regression analysis constructing two predictive models was used to determine the prognostic capabilities of gait speed for predicting time to functional recovery: Model 1, age + sex; Model 2, Model 1 + hip and knee muscle strength + ROM.
We constructed receiver operating characteristic (ROC) curves to compare the predictive ability of usual and maximal gait speed for functional recovery on postoperative day 5. The areas under the curves (AUCs) of ROC curves were compared according to the method of DeLong et al. [16] We also constructed ROC curves for functional recovery at 5 days after the operation using two models: gait speed only and clinical model including age, sex, hip and knee muscle strength, and ROM.
The Kaplan–Meier method was used to evaluate functional recovery and comparisons were performed by the log-rank test. Patients were divided into 3 groups based on tertile of gait speed. Subgroup analyses of gait speed were performed to examine by means of Cox regression analyses with adjustment for age and sex as potential confounders, including age stratified at < 65 years, 65–74 years, and ≥ 75 years, and sex. Hazard ratios (HRs) are reported with corresponding 95% confidence intervals (CIs).
Data are presented as the means ± standard deviation or as percentages. Statistical analyses were performed using SPSS version 22.0 (IBM Corporation, Armonk, NY), STATA version 13.0 (StataCorp, College Station, TX), and R version 3.1.2 (The R Foundation for Statistical Computing, Vienna, Austria). In all analyses, P < 0.05 was taken to indicate statistical significance.
Results
The characteristics of all patients included in the study are shown in Table 1. The patients had a mean age of 64.7 ± 11.8 years old, mean BMI of 24.5 ± 4.6 kg/m2, and 82.3% (261/317) were female. The mean time to functional recovery was 6.4 ± 3.1 days.
The associations of usual and maximal gait speeds with time to functional recovery as determined by Cox regression analyses are presented in Table 2. Even after adjusting for age, sex, muscle strength, and ROM (Model 2), the usual and maximal gait speeds were independently associated with functional recovery (HR = 2.32, 95% CI = 1.30–4.12; P = 0.004; HR = 1.97, 95% CI = 1.30–2.97; P = 0.001, respectively).
We compared the AUCs of usual and maximal gait speed using ROC analysis. Predictive ability of maximal gait speed for functional recovery on postoperative day 5 was significantly higher than those of usual gait speed (P = 0.028, Fig. 1). The AUC for maximal gait speed (0.70, 95% CI: 0.64–0.76) was as large as those for clinical model (0.70, 95% CI: 0.64–0.76) including age, sex, hip and knee muscle strength, and ROM as shown in Fig. 2 (P = 0.947).
On Kaplan–Meier analysis plotting tertiles of maximal gait speed, proportion of functional recovery was significantly higher in the fast gait speed group than the middle and slow gait speed group (log-rank, P < 0.001; Fig. 3). In addition, the middle gait speed group had also significantly higher proportion of functional recovery than the slow gait speed group (P < 0.001). Maximal gait speed was also consistently associated with the time to functional recovery across various subgroups after adjusting for age and sex as shown in Fig. 4.
Discussion
The present study indicated an independent association between gait speed and functional recovery after THA. The predictive capability of maximal gait speed was higher than that of usual gait speed and equivalent to clinical model including age, sex, hip and knee muscle strength, and ROM. Patients with fast gait speed showed significantly faster functional recovery than those patients with slow gait speed. In addition, various subgroups of patients with fast gait speed consistently showed higher rates of functional recovery after adjusting for age and sex. Based on the results of the present study, maximal gait speed may be useful for predicting the functional recovery after THA.
Delay in functional recovery also contributes to prolongation of length of hospital stay. However, there have been few reports regarding factors related to functional recovery in inpatients following THA. Oosting et al. reported that age > 70 years old, presence of comorbidities, TUG score > 10.5 s, and usual walking speed < 1.0 m/s were risk factors for delayed functional recovery [6], while Elings et al. reported that male sex, age ≥ 70 years, BMI ≥25 kg/m2, American Society of Anesthesiologists score of 3, Charnley score of B or C, and TUG score of ≥12.5 s were significant risk factors [17]. In addition, Unnanuntana et al. reported that age, sex, and BMI were factors affecting ambulation distance at discharge as a measure of functional recovery [18]. These indicators appear to be important factors related to functional recovery. However, it is necessary to examine multiple factors for prediction, and this may be difficult from a practical viewpoint. The results of the present study indicated that maximal gait speed as a single index showed comparable predictive power as clinical model including age, sex, muscle strength, and ROM. The results of the present study suggested that preoperative assessment of maximal gait speed is a simple and useful predictive index for functional recovery after THA.
Previous studies have reported that functional indicators such as TUG and sit-to-stand test are useful in predicting postoperative recovery [7,8,9,10, 14, 19,20,21,22]. In addition, with the increasing age of patients who undergo artificial joint replacement, the importance of evaluating physical frailty has been reported in recent years [23]. Currently, various methods are used to assess physical frailty, but due to its simplicity and predictive capability, gait speed has become a core strategy to evaluate physical frailty. Gait speed has been shown to predict morbidity and mortality in various populations [24, 25]. In addition, the evaluation of gait speed is reliable and accurately measures even frail older adults with cognitive dysfunction, which is common comorbidity in the elderly population [26]. Importantly, several studies have indicated that the single measurement of gait speed outperformed other multicomponent frailty scales in predicting outcomes [27, 28]. Based on this available evidence, the European orthopedic expert group advises the use of gait speed to measure physical performance in daily practice [29]. These studies and guidelines also support the usefulness of gait speed, and the results of this study are consistent with these findings.
In recent reports of THA surgery, the average length of a hospital stay has been shortened year by year due to progress in surgery and the introduction of enhanced recovery after surgery (ERAS) [30]. Achieving walking independence in 5 days as reported in the current study is certainly a longer time than those reported above. According to a recent meta-analysis, the average hospital stay worldwide is 2–13 days, which varies greatly by country and medical facility, from early discharge being more common in the United States, to hospitalization of a week or longer usual for other countries [31]. In this study, functional recovery at 5 days was adopted with reference to a previous study [17].
Limitations
This study had several limitations. First, this was a retrospective, single-center study. Second, although multivariate analysis was performed, many factors related to functional recovery have been reported, and other factors that were not measured, such as cognitive impairment, smoking history, and medication like analgesics [4, 32], may have resulted in residual bias. Third, the study population included only Asian patients after THA. Fourth, this study does not measure other performance tests such as TUG or sit-to-stand test, so it was not able to compare the usefulness of gait speed with other performance tests. Further studies are required to validate the utility of maximal gait speed as a predictor of functional recovery in other populations or as compared with other evaluations.
Conclusion
Preoperative maximal gait speed was shown to be associated with early functional recovery following THA. The results presented here suggested that the preoperative maximal gait speed may be a simple and useful prognostic indicator for functional recovery after THA.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due that individual privacy could be compromised, but are available from the corresponding author on reasonable request.
Abbreviations
- AUC:
-
Area under the curve
- BMI:
-
Body-mass index
- BW:
-
Body weight
- CI:
-
Confidence interval
- ERAS:
-
Enhanced recovery after surgery
- HR:
-
Hazard ratio
- OA:
-
Osteoarthritis
- OARSI:
-
Osteoarthritis Research Society International
- ROC:
-
Receiver operating characteristic
- ROM:
-
Range of motion
- THA:
-
Total hip arthroplasty
- TUG:
-
Timed up-and-go
References
Neuprez A, Neuprez AH, Kaux JF, Kurth W, Daniel C, Thirion T, et al. Total joint replacement improves pain, functional quality of life, and health utilities in patients with late-stage knee and hip osteoarthritis for up to 5 years. Clin Rheumatol. 2019. https://doi.org/10.1007/s10067-019-04811-y.
Malani PN. Functional status assessment in the preoperative evaluation of older adults. JAMA. 2009;302(14):1582–3.
Baldini G, Ferreira V, Carli F. Preoperative preparations for enhanced recovery after surgery programs: a role for prehabilitation. Surg Clin North Am. 2018;98(6):1149–69.
Elings J, Hoogeboom TJ, van der Sluis G, van Meeteren NL. What preoperative patient-related factors predict inpatient recovery of physical functioning and length of stay after total hip arthroplasty? A systematic review. Clin Rehabil. 2015;29(5):477–92.
Hofstede SN, Gademan MG, Vliet Vlieland TP, Nelissen RG, Marang-van de Mheen PJ. Preoperative predictors for outcomes after total hip replacement in patients with osteoarthritis: a systematic review. BMC Musculoskelet Disord. 2016;17:212.
Oosting E, Hoogeboom TJ, Appelman-de Vries SA, Swets A, Dronkers JJ, van Meeteren NL. Preoperative prediction of inpatient recovery of function after total hip arthroplasty using performance-based tests: a prospective cohort study. Disabil Rehabil. 2016;38(13):1243–9.
Nankaku M, Tsuboyama T, Akiyama H, Kakinoki R, Fujita Y, Nishimura J, et al. Preoperative prediction of ambulatory status at 6 months after total hip arthroplasty. Phys Ther. 2013;93(1):88–93.
Petis SM, Howard JL, Lanting BA, Somerville LE, Vasarhelyi EM. Perioperative predictors of length of stay after total hip arthroplasty. J Arthroplasty. 2016;31(7):1427–30.
Poitras S, Au K, Wood K, Dervin G, Beaulé PE. Predicting hospital length of stay and short-term function after hip or knee arthroplasty: are both performance and comorbidity measures useful? Int Orthop. 2018;42(10):2295–300.
Poitras S, Wood KS, Savard J, Dervin GF, Beaule PE. Predicting early clinical function after hip or knee arthroplasty. Bone Joint Res. 2015;4(9):145–51.
Elibol N, Unver B, Karatosun V, Gunal I. Relationship between self-reported and performance-based tests in assessment of patients with total hip arthroplasty. Hip Int. 2018;28(5):566–70.
Dobson F, Hinman RS, Roos EM, Abbott JH, Stratford P, Davis AM, et al. OARSI recommended performance-based tests to assess physical function in people diagnosed with hip or knee osteoarthritis. Osteoarthr Cartil. 2013;21(8):1042–52.
Barker KL, Batting M, Schlüssel M, Newman M. The reliability and validity of the figure of 8 walk test in older people with knee replacement: does the setting have an impact? Physiotherapy. 2019;105(1):76–83.
Bahl JS, Nelson MJ, Taylor M, Solomon LB, Arnold JB, Thewlis D. Biomechanical changes and recovery of gait function after total hip arthroplasty for osteoarthritis: a systematic review and meta-analysis. Osteoarthr Cartil. 2018;26(7):847–63.
Katoh M, Yamasaki H. Comparison of reliability of isometric leg muscle strength measurements made using a hand-held dynamometer with and without a restraining belt. J Phys Ther Sci. 2009;21:37–42.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Elings J, van der Sluis G, Goldbohm RA, Galindo Garre F, de Gast A, Hoogeboom TJ, et al. Development of a risk stratification model for delayed inpatient recovery of physical activities in patients undergoing total hip replacement. J Orthop Sports Phys Ther. 2016;46(3):135–43.
Unnanuntana A, Rebolledo BJ, Gladnick BP, Nguyen JT, Sculco TP, Cornell CN, et al. Does vitamin D status affect the attainment of in-hospital functional milestones after total hip arthroplasty? J Arthroplasty. 2012;27(3):482–9.
Gerhardt DMJM, Mors TGT, Hannink G, Van Susante JLC. Resurfacing hip arthroplasty better preserves a normal gait pattern at increasing walking speeds compared to total hip arthroplasty. Acta Orthop. 2019;90(3):231–6.
Yoo JI, Cha YH, Kim KJ, Kim HY, Choy WS, Hwang SC. Gait analysis after total hip arthroplasty using direct anterior approach versus anterolateral approach: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):63.
Gomi M, Maezawa K, Nozawa M, Yuasa T, Sugimoto M, Hayashi A, et al. Early clinical evaluation of total hip arthroplasty by three-dimensional gait analysis and muscle strength testing. Gait Posture. 2018;66:214–20.
Foucher KC, Freels S. Preoperative factors associated with postoperative gait kinematics and kinetics after total hip arthroplasty. Osteoarthr Cartil. 2015;23(10):1685–94.
Schmucker AM, Hupert N, Mandl LA. The impact of frailty on short-term outcomes after elective hip and knee arthroplasty in older adults: a systematic review. Geriatr Orthop Surg Rehabil. 2019;10:2151459319835109.
Studenski S, Perera S, Patel K, Rosano C, Faulkner K, Inzitari M, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50–8.
Kamiya K, Hamazaki N, Matsue Y, Mezzani A, Corrà U, Matsuzawa R, et al. Gait speed has comparable prognostic capability to six-minute walk distance in older patients with cardiovascular disease. Eur J Prev Cardiol. 2018;25(2):212–9.
Chan WLS, Pin TW. Reliability, validity and minimal detectable change of 2-minute walk test, 6-minute walk test and 10-meter walk test in frail older adults with dementia. Exp Gerontol. 2019;115:9–18.
Afilalo J, Mottillo S, Eisenberg MJ, Alexander KP, Noiseux N, Perrault LP, et al. Addition of frailty and disability to cardiac surgery risk scores identifies elderly patients at high risk of mortality or major morbidity. Circ Cardiovasc Qual Outcomes. 2012;5:222–8.
Kim DH, Kim CA, Placide S, Lipsitz LA, Marcantonio ER. Preoperative frailty assessment and outcomes at 6 months or later in older adults undergoing cardiac surgical procedures: a systematic review. Ann Intern Med. 2016;165:650–60.
Beaudart C, Rolland Y, Cruz-Jentoft AJ, Bauer JM, Sieber C, Cooper C, et al. Assessment of muscle function and physical performance in daily clinical practice : a position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif Tissue Int. 2019;105(1):1–14.
Drew S, Judge A, Cohen R, Fitzpatrick R, Barker K, Gooberman-Hill R. Enhanced recovery after surgery implementation in practice: an ethnographic study of services for hip and knee replacement. BMJ Open. 2019;9(3):e024431.
Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta-analysis. Postgrad Med J. 2017;93(1106):736–42.
Goplen CM, Verbeek W, Kang SH, Jones CA, Voaklander DC, Churchill TA, et al. Preoperative opioid use is associated with worse patient outcomes after total joint arthroplasty: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20(1):234.
Acknowledgements
The authors thank the orthopedics staff for their support and the patients who participated in this study.
Funding
No external funding was received for this study.
Author information
Authors and Affiliations
Contributions
MS, YN, KK, MT, MF and AM contributed to the conception and design of this study. MS, YN, KF, KU and NT contributed to the acquisition of data. MS, YN and KK contributed to the analysis of data. MS and KK were major contributors in writing the manuscript and all authors contributed to the interpretation of the data and drafting of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Kitasato University Hospital (permit number: B18–088), and was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rehabilitation program
Day 1 after surgery:
Cold pack or ice pack to manage pain, inflammation, and swelling
Start exercises (ankle pumps and quadriceps sets)
Start transfers
Observe hip precautions
Day 2:
Continue as above with emphasis on decreasing pain and swelling and promoting independence with functional activities
Start walking with a standard walker for 50 m and weight bearing as tolerated
Start passive/active assisted/active range of motion (P/AA/AROM) exercises
Start muscle strengthening exercises (e.g., quadriceps sets in full knee extension and gluteal sets)
Perform bed mobility and transfers with minimum assistance
Observe hip precautions
Days 3–7:
Continue as above with emphasis on achieving a proper gait pattern with an assistance device
Perform bed mobility and transfers independently
Ambulate with a T-cane for 50 m
Start activities of daily living training (e.g., dressing activities, climbing stairs, cutting nails, and bathing activities)
Instruct home exercises (e.g., supine: ankle pumps, quad sets, hamstring sets, gluteal sets, assisted heel slides, and hip abduction; seated: long arc quad and knee flexion; and standing: hip flexion with knee bend, knee flexion, heel raises, terminal knee extension, hip abduction, and mini-squats)
Observe hip precautions
After Day 7:
Continue as above
Ambulate with a T-cane for 50 m independently
If necessary, climb stairs independently
Observe hip precautions
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Shibuya, M., Nanri, Y., Kamiya, K. et al. The maximal gait speed is a simple and useful prognostic indicator for functional recovery after total hip arthroplasty. BMC Musculoskelet Disord 21, 84 (2020). https://doi.org/10.1186/s12891-020-3093-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-3093-z