Abstract
Background
A significant proportion of the overall cost of total hip arthroplasty (THA) results from the inpatient hospital stay following the procedure. Considering the substantial and increasing number of these procedures performed annually, shifting to an outpatient model of care where the patient is discharged home the same day as their surgery represents a potential for significant cost savings. The potential significant impact of an outpatient care model on constrained healthcare budgets and lack of high-quality evidence regarding its effectiveness warrants a rigorous comparative trial. The purpose of this prospective, randomized controlled trial is to evaluate outpatient care pathways for THA. Specifically, our objectives are to compare the rate of serious adverse events and estimate the cost-effectiveness of outpatient compared to standard inpatient THA.
Methods
We will include patients undergoing primary THA whom have an American Society of Anaesthetists status equal to or less than three, live within a 60-min driving distance of the institution and have an adult to accompany them home postoperatively and stay with them overnight. Consenting patients will be randomized to be discharged on the same day as surgery, as outpatients, or as inpatients according to standard of care (minimum of one night in hospital) using a modified Zelen consent model. The primary outcome measure is the incidence of serious adverse events at 30 days postoperative. Participants and their caregivers will complete secondary outcomes measures at each follow-up visit including patient-reported outcome measures and self-reported cost questionnaires.
Discussion
This protocol is the first randomized trial to use blinding to evaluate outpatient THA compared to standard overnight stay and first to prospectively perform a full economic evaluation. It is also the first adequately powered trial to prospectively assess the safety of outpatient THA. Successful completion of this study could have the potential to provide clinical evidence for the role of outpatient THA in current practice.
Trial registration
This study was retrospectively registered on ClinicalTrials.gov (NCT03026764) on March 9th, 2016.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Osteoarthritis (OA) is a leading cause of disability and reduced quality of life, presenting a substantial, growing burden to patients and the healthcare system [1]. Total hip arthroplasty (THA) is an established, effective intervention for advanced OA. The prevalence of hip OA is rapidly increasing, resulting in a rising demand for care. The number of THA procedures is projected to grow by 71% between 2014 and 2030 in the US [2]. Currently, THA, along with total knee arthroplasty (TKA), have a significant impact on healthcare budgets, costing approximately $1.2 billion in annual spending in Canada [3]. These staggering numbers highlight the critical need to improve care delivery.
A significant proportion of the overall cost of joint replacement results from the inpatient hospital stay following the procedure. Historically, the standard procedure following THA required an inpatient hospital stay of two and a half to 3 weeks, however the introduction of less invasive surgical techniques, improved medical and analgesia management and comprehensive rehabilitation have enabled shorter inpatient stays. Today, the median inpatient stay following THA is 3 days in Canada [3]. A desire for greater autonomy by the patients as well as patients wanting early mobilization to accelerate recovery and return to activities has led some clinicians to consider an outpatient arthroplasty program. The proposed benefits of outpatient arthroplasty include similar patient outcomes with significantly lower hospital costs, and improved patient satisfaction, independence, and autonomy. However, there is a lack of high-quality evidence comparing clinical outcomes of outpatient to inpatient arthroplasty models of care.
A retrospective analysis of over 50,000 THA and TKA procedures found no differences in 30-day major complications or readmissions among patients with a zero to two-day hospital stay compared to those discharged on day three or four postoperative [4]. Small cohort studies [5,6,7,8] suggest lower costs for outpatients and improved patient satisfaction but have inherent biases as they are limited to carefully selected patients in privatized health systems.
It is estimated that up to 20% of the overall cost of THA can be attributed to the inpatient stay in hospital at our institution [9]. By discharging patients as outpatients, it could be possible to have substantial savings. Although these preliminary calculations are encouraging, it is not sufficient to effect change solely to achieve cost control, without consideration of safety, effectiveness and patient satisfaction. Further, it is unknown whether the financial savings will be outweighed by additional postoperative costs, increased readmissions or decreased quality of care. A full economic evaluation that simultaneously evaluates cost and effectiveness is crucial prior to implementation. The lack of high-quality evidence regarding its effectiveness warrants a rigorous comparative trial.
The purpose of this study is to evaluate outpatient care pathways for THA. Specifically, our objectives are to compare the rate of serious adverse events and estimate the cost-effectiveness of outpatient compared to standard inpatient THA using a patient-blinded, randomized clinical trial.
Methods/design
Study setting
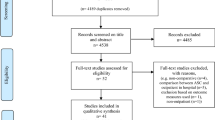
Patients will be recruited from two orthopaedic centers in Canada (London Health Science’s University Hospital, London ON and St. Michael’s Hospital, Toronto ON). The surgeons will screen potential participants in their clinics and provide an overview of the research study (Fig. 1).
Eligibility criteria
We will include patients undergoing primary THA. Eligible patients will have an American Society of Anesthetists (ASA) status equivalent or less than three, the ability to read and understand English, live within a 60 min commute distance of the institution, have access to a phone, and sufficient caregiver support. We will exclude patients with a history of anesthesia related complications, narcotic dependency, anaphylaxis to penicillin, significant psychosocial issues that influence safety, or cognitive issues that preclude the ability to understand instructions. We will also exclude patients whom have fibromyalgia, are skeletally immature, have an active or suspected latent infection in or about the joint, bone stock inadequate for support or fixation of the prosthesis, are unable to go to their home after surgery, have neuromotor conditions, significant pain management issues or obesity that significantly impacts their ability to mobilize (Table 1).
Interventions
All patients will undergo a primary unilateral THA. All THA procedures will be performed using a direct anterior surgical approach according to the surgeon’s standard of care. The specific surgical pathway details (anesthetic, implants, etc.) will not be standardized for this study to maintain generalizability.
Both inpatient and outpatient care models begin with comprehensive preoperative patient education to equip the patient with a reasonable set of goals and expectations about their surgery, medications, pain management and rehabilitation. Immediately following surgery, the primary goals are to treat pain, nausea and hypovolemia. The combination of this early rehabilitation program, with a muscle sparing technique, is vital to the rapid recovery process. The surgical technique minimizes blood loss, provides a stable construct to facilitate immediate weightbearing, minimizes soft tissue trauma and includes a peri-articular injection. Home-based physical therapy should begin immediately, with a focus on ambulation.
Perioperative care and discharge protocols will be similar for both care models. Standard discharge criteria includes: ability to use required gait aids, appropriate pain control, control or absence of nausea and vomiting, hemostasis at the surgical wound, hemodynamically stable with appropriate laboratory values, alert and oriented, able to use the bathroom, meets the hospital standard targets from physiotherapy for discharge, given take-home medications, and in the company of a caregiver. Potential complications are also discussed so the patient understands the normal course of recovery as well as signs or symptoms that may be cause for concern and additional consultation.
Patients randomized to inpatient
Patients allocated to the inpatient group will be discharged home according to standard protocol at each site (typically one to 4 days postoperative).
Patients randomized to outpatient
Patients allocated to the outpatient group will be discharged home on the same day as the procedure. These patients will receive an additional physiotherapy session prior to surgery where they are instructed to practice certain skills such as bed transfer, cane/crutches use and gait training.
Outcomes
We will collect outcome data preoperatively and at follow-up visits at discharge, 2 weeks, 6 weeks and 3 months postoperative, which is in keeping with usual practice patterns. We will record anaesthesia and surgical time and blood loss for each procedure and demographic information including date of birth, sex, height, weight, smoking status, and comorbidities.
Primary outcome
Given that the primary concern with sending patients home earlier than usual is an increase in the number or severity of early post-operative complications, our primary outcome is any serious adverse event within the first 30 days postoperative. A serious adverse event is defined as any untoward medical occurrence that results in death, is life-threatening, requires inpatient hospitalization or causes prolongation of existing hospitalization, results in persistent or significant disability or incapacity, or requires intervention to prevent permanent impairment or damage [10,11,12].
Secondary outcomes
Our secondary outcomes include patient-reported satisfaction, health-related quality of life (HRQOL), function, pain, and caregiver assistance. Patients will be asked to rate satisfaction with pain control, safety and quality of care on either a 100-mm visual analogue scale (VAS) with a score of 100 representing the highest possible satisfaction, or on a five to seven-point ordinal scale (completely satisfied to completely unsatisfied).
We will measure HRQOL using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), which includes three arthritis-specific domains of pain, stiffness and physical function. It has demonstrated content, cross-sectional and construct validity, good internal consistency reliability and moderate to high test retest reliability in patients undergoing THA and TKA [13]. To measure function, we will use the Harris Hip Score (HHS) [14]; a valid and reliable objective functional measure completed by the surgeon. We will measure general health using the 12-Item Short Form Health Survey (SF-12v2) and the European Quality of Life Scale (EQ-5D). The SF-12 evaluates limitations on physical and social activities, activities of daily living, pain, mental health and well-being, and perceptions of health and is valid, reliable, and responsive in patients with arthritis [15]. The EQ-5D index includes domains of mobility, self-care, usual activities, pain, anxiety and depression and has good test retest reliability and cross-sectional construct validity in patients with arthritis [16]. We will measure pain using a self-administered Numeric Pain Rating Scale (Pain NRS), ranging from 0 (no pain) to 10 (worst). We will measure the level of assistance provided by the caregiver throughout the recovery period using the Caregiver Assistance Scale (CAS) [17] and Caregiver Strain Index (CSI) [18].
Cost
We will ask patients to report any calls to the surgeon’s office, the on-call resident, the orthopaedic outpatient clinic, emergency room visits or hospitalizations for the first 2 weeks postoperative. Patients will also complete a healthcare resource use diary at each follow-up. The diary includes information on emergency room visits, hospitalizations, family doctor, specialist, healthcare professional or outpatient clinic visits, tests, procedures, and prescription or over-the-counter medications and any other miscellaneous costs related to their joint replacement. We will also record employment status and time-off paid employment, homemaking or volunteer activities, for both patients and caregivers.
We will obtain surgical procedure costs from our institutions’ case costing department. The unit costs for additional resource use following surgery can be found in provincial fee schedules and drug benefit formularies. The average Canadian wage reported by Statistics Canada will be applied to place a monetary figure on time off paid employment, for both patients and their caregivers and the current value of minimum wage in the province of Ontario to account for lost time for those who were retired, as well as time away from volunteer or home making activities.
The total cost will be determined by multiplying the quantity of resource use by the corresponding unit cost, summing the total cost over each follow up interval, and then calculating the mean cost at each follow-up time point, as well as an overall mean cost for the entire study period.
Participant timeline
Patients will be screened and consent obtained at the time of booking for surgery and baseline assessments will occur at the preoperative visit within 3 months of surgery. On the day of discharge from hospital, we will obtain a pain score from participants and provide them with a daily diary to record costs for the first 2 weeks. Postoperatively, participants will be seen at 2 weeks, 6 weeks and 3 months for follow-up.
We will ask caregivers to complete questionnaires preoperatively and at 2 weeks postoperatively (Table 2).
Recruitment
Patients presenting to the clinic will first be booked for THA by their surgeon. The surgeon will then assess whether the patient is eligible for possible outpatient discharge and will broadly discuss the study with the patient. The surgeon will then ask if the patient is interested in hearing more about the study and whether the research assistant may contact them with further information. Once patient approval is received, the patient is contacted by the research assistant with more information. All patients will be given the necessary time to consider their participation in the study and to provide informed consent if willing to participate.
Randomization
Concealment mechanism/implementation
Potential participants will be initially screened by their treating surgeon and approached for participation by the research assistant. To reduce selection bias, patients are randomized into group using a stratified and blocked scheme after eligibility has been fully determined. The research assistant will confirm their eligibility and, after obtaining consent, will enter the patient’s date of birth and whether they’ve had previous experience with THA before randomizing the patient via a web-based randomization system to inpatient or outpatient.
Allocation (sequence generation)
All participants will be randomized by the research assistant using a 1:1 ratio for inpatient to outpatient. Randomization will be stratified by surgeon and previous experience with THA (had a THA on the contralateral limb or were the caregiver for someone whom had a THA). All patients will be analyzed according to the treatment group as assigned regardless of when they were discharged.
Blinding
To reduce detection bias, patients will be unaware that they were randomly assigned to a discharge plan and remain blinded to the presence of a comparison group until they reach the end of the study. Participants are kept blinded to group allocation using a modified Zelen consent model [19]. In this design, eligible patients are randomized to the intervention prior to providing consent to minimize the risk of bias associated with knowledge of the alternative intervention. We posit that patients with a bias for inpatient care who are randomized to the outpatient group may be more likely to return to seek additional care significantly biasing costs. Alternatively, patients with a strong preference for outpatient care who are randomized to the inpatient group may bias measures of satisfaction. Thus, patients are asked to consent to participation in a research study evaluating the outcomes and costs associated with patients undergoing THA; they are not told about randomization, the existence of an alternative group, or the between-groups objectives. At the end of the study, all patients are informed about the deception and asked to consent to having their data used for analysis.
As data collection occurs on the day of discharge from the hospital, it is not possible to blind the research assistant responsible for collecting patient-reported outcomes, however since outcomes are patient-reported, we do not expect an increase in the risk of detection bias. We are also unable to blind investigators to group allocation.
Sample size
A retrospective analysis of over 50,000 THA and TKA procedures found no differences in 30-day major complications or readmissions among patients with a zero to two-day hospital stay compared to those discharged on day three or four postoperative [4]. The rate of serious adverse events in the inpatient group is expected to be greater than 5 % [20]. To define a non-inferiority margin we agreed that no more than a 5 % increase in the risk of serious adverse event (risk difference ≥ 6% favouring inpatient care) was acceptable. If the risk in the inpatient group ranges between five to 8 % and there is truly no difference in risk of serious adverse event between the groups, then a maximum of 506 patients are required to be 80% certain that the upper limit of a one-sided 95% confidence interval will exclude a difference in favour of the inpatient group of more than 6 % [21]. Given that the primary outcome is being measured at 30-days postoperative, we anticipate a low lost-to-follow-up rate. Previous studies conducted at the lead study site in similar patients demonstrate loss to follow up rates less than 1 % for the first 30 days. Therefore, to account for a potential 1 % dropout rate we inflated our sample size to 511.
Plan for statistical analysis
We will present the incidence of serious adverse events by group at 30 days postoperative and calculate a risk difference and relative risk with 95% confidence intervals around the estimates. The mean and standard deviation for all continuous outcomes (Satisfaction, WOMAC, SF-12, HHS, Pain NRS, and CAS) will be calculated for each group at each time point and calculate the mean between-group difference with 95% confidence interval. Linear mixed models, using a covariance structure that allows for correlations between measurements to decline as they are further apart in time will be used to evaluate improvements in function after surgery since this provides a powerful approach to analyze complex longitudinal data while controlling for important covariates such as gender, comorbidities, age and surgeon/site. All data will be analyzed according to the intention-to-treat principle with an as treated analysis also performed.
We will conduct a cost-effectiveness analysis from both a Canadian healthcare payer and societal perspective using the incidence of adverse events as our effectiveness outcome to estimate cost-effectiveness at 3 months postoperative. We will determine cost-effectiveness using the net benefit regression (NBR) framework to estimate the incremental net benefit (INB) of outpatient arthroplasty [22]. An intervention is considered to be cost-effective if the INB is greater than zero. NBR also provides a means to adjust for potentially confounding factors and therefore allows greater statistical efficiency and a more precise estimate of the INB. To characterize the statistical uncertainty around our estimate of INB we will calculate 95% confidence intervals, and a cost-effectiveness acceptability curve [23].
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Data collection methods
Follow-up assessments for this study coincide with the standard of care follow-up schedule for the surgeons at our centre. During each visit, the research assistant will administer the questionnaires to the participants and ensure they are completed. Alternatively, participants are also given the option to complete questionnaires online by directly accessing the electronic data capture (EDC) system (Empower Health Research). The HHS will be completed by the treating surgeon at the three-month visit.
Data management
Participants have the option to complete questionnaires either in hard copy or using the EDC system (Empower Health Research).
Discussion
This protocol is for a multi-centered randomized controlled trial to assess the safety and cost-effectiveness of outpatient total hip arthroplasty compared to standard inpatient care. There is currently a lack of high-quality studies evaluating the safety and effectiveness of outpatient THA. Most studies that have assessed safety have used US national databases [24,25,26,27,28,29] or observational cohort designs [30,31,32,33] with only one published randomized trial [34]. Previous prospective studies have also been underpowered to detect differences in complication rates between outpatient and inpatient care groups. Due to the already low rates of serious adverse events after THA, reported from 3.8% up to 8.6% in the literature, [20, 35, 36] sample sizes must be sufficiently large to include a sufficient number of events to support clinical conclusions. Our protocol will be the first adequately powered prospective study to evaluate the safety of outpatient THA.
One strength of our study protocol is the use of a modified Zelen consent model [19], as one of the difficulties with assessing outpatient discharge in comparison with standard inpatient care is potential patient biases. This design allows us to avoid these biases as patients with a strong preference for either group are not made aware of the alternative intervention. A weakness of the randomized trial by Goyal et al. (2017) was the lack of blinding which led to a significant number of crossovers due to personal preference [34]. Our use of a modified Zelen consent model [19] should help to address this issue and reduce the number of crossovers in our study. Future studies looking to evaluate outpatient THA should also consider use of this design to strengthen their conclusions and reduce patient crossover.
Our study will be the first to perform a full economic evaluation in conjunction with a large randomized trial and will use both healthcare payer and societal perspectives. No full economic evaluations have been published to compare outpatient to standard inpatient care thus far. This is an important gap in the literature as international health economic guidelines suggest policy and clinical decisions should be supported by evidence produced when cost is evaluated simultaneously with effect in a full economic evaluation [37, 38]. Previous studies have evaluated cost alone [5, 6] and none in conjunction with a prospective trial. These studies have also only included direct costs associated with the procedures and hospital costs. Including a broader perspective and incorporating indirect costs such as time off work and caregiver assistance are important to consider, ensuring that costs possibly saved from reduced hospital stays are not shifted elsewhere in the recovery pathway. To truly know whether outpatient THA is less costly than inpatient care, as the literature currently suggests [5, 6], broader perspectives (ie. healthcare payer and societal) should be assessed. The use of multiple perspectives also helps to broaden the interpretability of study results and is recommended by international health economic guidelines [37]. The importance of costing perspective is highlighted in a paper by Primeau et al. (2019) where the conclusions of the study changed depending on the perspective used [39].
Our protocol hopes to address several gaps in the current literature with a large and adequately powered sample size to assess safety, the use of blinding with a modified Zelen consent model [19], and assessing costs in conjunction with a prospective randomized trial for a full economic evaluation. Conclusions from our study should help to inform clinical decision making in the use of outpatient care programs in standard practice for THA. Recruitment for the study is currently ongoing.
Availability of data and materials
Not applicable.
Abbreviations
- ASA:
-
American Society of Anesthetists
- CAS:
-
Caregiver Assistance Scale
- CSI:
-
Caregiver Strain Index
- EDC:
-
Electronic data capture
- EQ-5D:
-
European Quality of Life Scale
- HHS:
-
Harris Hip Score
- HRQOL:
-
Health-related quality of life
- INB:
-
Incremental net benefit
- NBR:
-
Net benefit regression
- OA:
-
Osteoarthritis
- Pain NRS:
-
Numeric Pain Rating Scale
- SF-12v2:
-
12-Item Short Form Health Survey
- THA:
-
Total hip arthroplasty
- TKA:
-
Total knee arthroplasty
- VAS:
-
Visual analog scale
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
References
The Arthritis Alliance of Canada, The Impact of Arthritis in Canada: Today and over the next 30 Years, 2011 http://www.arthritisalliance.ca/en/initiativesen/impact-of-arthritis.
Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Joint Surg Am. 2018;100:1455–60.
Canadian Institute for Health Information. Hip and knee replacements in Canada, 2017–2018: Canadian joint replacement registry annual report. Ottawa: CIHI; 2019.
Sutton JC III, Antoniou J, Epure LM, et al. Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major-complication and readmission rates. J Bone Joint Surg Am. 2016;98:1419–28.
Aynardi M, Post Z, Ong A, et al. Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSSJ. 2014;10:252–5.
Bertin KC. Minimally invasive outpatient total hip arthroplasty: a financial analysis. Clin Orthop Relat Res. 2005;435:154–63.
Lovald ST, Ong KL, Malkani AL, et al. Complications, mortality, and costs for outpatient and short-stay total knee arthroplasty patients in comparison to standard-stay patients. J Arthroplast. 2014;29(3):510–5.
Kolisek FR, McGrath MS, Jessup NM, et al. Comparison of outpatient versus inpatient total knee arthroplasty. Clin Orthop Relat Res. 2009;467(6):1438–42.
Petis SM, Howard JL, Lanting BA, et al. In-hospital cost analysis of total hip arthroplasty: does surgical approach matter? J Arthroplast. 2016;31:53–8.
Adverse Reaction Reporting and Health Product Safety Information Guide for Health Professionals. Health Canada, Report No: 110123 ISBN: 978–1–100-18845-4.
U.S. Food and Drug Administration (Last Updated 02/01/2016) What is a Serious Adverse event?, Retrieved from: http://www.fda.gov/safety/medwatch/howtoreport/ucm053087.htm.
Expert Working Group (Efficacy) of the International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH). "Guideline for Industry - Clinical safety data management: definitions and standards for expedited reporting". FDA Center for Drug Evaluation and Research. 2007.
Bellamy N, Buchanan WW, Goldsmith CH, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40.
Soderman P, Malchau H. Is the Harris hip score system useful to study the outcome of total hip replacement? Clin Orthop Relat Res. 2001;384:189–97.
Gandhi SK, Salmon JW, Zhao SZ, et al. Psychometric evaluation of the 12-item short-form health survey (SF-12) in osteoarthritis and rheumatoid arthritis clinical trials. Clin Ther. 2001;23(7):1080–98.
Fransen M, Edmonds J. Reliability and validity of the EuroQol in patients with osteoarthritis of the knee. Rheumatology (Oxford). 1999;38(9):807–13.
Cameron JI, Franche R-L, Cheung AM, et al. Lifestyle interference and emotional distress in family caregivers of advanced Cancer patients. Cancer. 2002;94(2):521–7.
Robinson BC. Validation of a caregiver strain index. J Gerontol. 1983;38(3):344–8.
Zelen M. A new design for randomized clinical trials. N Engl J Med. 1979;300:1242–5.
Bernatz JT, Tueting JL, Anderson PA. Thirty-day readmission rates in orthopedics: a systematic review and meta-analysis. PLoS One. 2015;10(4):e0123593.
Blackwelder WC. "proving the null hypothesis" in clinical trials. Control Clin Trials. 1982;3:345–53.
Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ. 2002;11(5):415–30.
Hoch JS, Rockx MA, Krahn AD. Using the net benefit regression framework to construct cost-effectiveness acceptability curves: an example using data from a trial of external loop recorders versus Holter monitoring for ambulatory monitoring of "community acquired" syncope. BMC Health Serv Res. 2006;6:68.
Arshi A, Leong NL, Wang C, et al. Outpatient total hip arthroplasty in the United States: a population-based comparative analysis of complication rates. J Am Acad Orthop Sur. 2019;27(2):61–7.
Basques BA, Tetreault MW, Della Valle CJ. Same-day discharge compared with inpatient hospitalization following hip and knee arthroplasty. J Bone Joint Surg Am. 2017;99:1969–77.
Courtney PM, Boniello AJ, Berger RA. Complications following outpatient total joint arthroplasty: an analysis of a national database. J Arthroplast. 2017;32:1426–30.
Lovecchio F, Alvi H, Sahota S, et al. Is outpatient arthroplasty as safe as fast-track inpatient arthroplasty? A propensity score matched analysis. J Arthroplast. 2016;31:5197–201.
Nelson SJ, Webb ML, Lukasiewicz AM, et al. Is outpatient total hip arthroplasty safe? J Arthroplast. 2017;32:1439–42.
Otero JE, Gholson JJ, Pugely AJ, et al. Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplast. 2016;31:2714–25.
Crawford DC, Li CS, Sprague S, et al. Clinical and cost implications of inpatient versus outpatient orthopedic surgeries: a systematic review of the published literature. Orthop Rev (Pavia). 2015;7:6177.
Gromov K, Jørgensen GC, Petersen PB, Kjaersgaard-Andersen P, et al. Complications and readmissions following outpatient total hip and knee arthroplasty: a prospective 2-center study with matched controls. Acta Orthop. 2019;90(3):281–5.
Hoffmann JD, Kusnezov NA, Dunn JC, et al. The shift to same-day outpatient joint arthroplasty: a systematic review. J Arthroplast. 2018;33:1265–74.
Pollock M, Somerville L, Firth A, et al. Outpatient total hip arthroplasty, total knee arthroplasty, and unicompartmental knee arthroplasty: a systematic review of the literature. JBJS Rev. 2016;4(12):1–15.
Goyal N, Chen AF, Padgett SE, et al. Otto Aufranc award: a multicenter, randomized study of outpatient versus inpatient total hip arthroplasty. Clin Orthop Relat Res. 2017;475:364–72.
Ponnusamy KE, Naseer Z, El Dafrawy MH, et al. Post-discharge care duration, charges and outcomes among Medicare patients after primary total hip and knee arthroplasty. J Bone Joint Surg Am. 2017;99(11):e55.
SooHoo NF, Farng E, Lieberman JR, et al. Factors that predict short-term complication rates after total hip arthroplasty. Clin Orthop Relat Res. 2010;468:2363–71.
Sanders GD, Neumann PJ, Basu A, et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–103.
Guidelines for the economic evaluation of health technologies: Canada. 4th ed. Ottawa: CADTH; 2017.
Primeau CA, Marsh JD, Birmingham TB, et al. The importance of costing perspective: an example evaluating the cost-effectiveness of a locking versus nonlocking plate in medial opening wedge high tibial osteotomy. Can J Surg. 2019;62(1):E14–6.
Acknowledgements
We would like to acknowledge the participating investigators and coordinators at the study sites for their efforts and contributions to this study.
Funding
This study is supported by the Opportunities Fund of the Academic Health Sciences Centre Alternative Funding Plan of the Academic Medical Organization of Southwestern Ontario. We also received funding from the Physicians’ Services Incorporated Foundation whom peer-reviewed the protocol. Neither funding source plays a role in how the study is conducted.
Author information
Authors and Affiliations
Contributions
BOZ assisted in the development of the protocol, contributed to participant recruitment and data collection and wrote this manuscript with the help of DMB, JDM and BAL. DMB provided expertise in the area of epidemiology and research methodology for the development of the protocol including the study design, modified Zelen consent model, determining the appropriate outcome measures, data analysis plan, sample size calculation and contributed to this manuscript. JDM provided expertise in the area of health economics for the development of the protocol including inclusion of appropriate cost collection tools, perspectives to be used, data analysis plan and contributed to this manuscript. BAL is the primary investigator, provided clinical expertise for the development of the protocol including background and rationale for the study, eligibility criteria, study design, determining the appropriate outcome measures and contributed to this manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Western Ontario Health Sciences Research Ethics Board on May 11, 2015 (REB Approval #106362) and by the Unity Health Toronto Research Ethics Board on January 16, 2019 (REB Approval #18–311) after undergoing full board review.
Written informed consent will be obtained from each participant prior to enrolling them in the study and again at the end of the study prior to use of the data. Participation is voluntary and participants will be free to refuse participation or to withdraw from the study at any time with no effect on their future care. Participants are also free to refuse the use of their data at the end of the study after they have been informed of the true nature of the study. Participants do not waive any legal right by signing the consent form.
Consent for publication
Not applicable.
Competing interests
BL is a consultant for and receives institutional support from Stryker, DePuy and Smith & Nephew. He is also a principal investigator for studies funded by the above-mentioned companies, including receiving funding from Stryker to run a study entitled “Cost-effectiveness and functional analysis of a rapid recovery protocol compared to the standard of care.”
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zomar, B.O., Marsh, J.D., Lanting, B.A. et al. A protocol for a randomized controlled trial investigating the safety and cost-effectiveness of outpatient total hip arthroplasty. BMC Musculoskelet Disord 21, 663 (2020). https://doi.org/10.1186/s12891-020-03699-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-03699-z