Abstract
Background
Even though surgical techniques and implants have evolved, periprosthetic joint infection (PJI) remains a serious complication leading to poor postoperative outcome and a high mortality. The literature is lacking in studies reporting the mortality of very elderly patients with periprosthetic joint infections, especially in cases when an intensive care unit (ICU) treatment was necessary. We therefore present the first study analyzing patients with an age 80 and higher suffering from a periprosthetic joint infection who had to be admitted to the ICU.
Methods
All patients aged 80 and higher who suffered from a PJI (acute and chronic) after THR or TKR and who have been admitted to the ICU have been included in this retrospective, observational, single-center study.
Results
A total of 57 patients met the inclusion criteria. The cohort consisted of 24 males and 33 females with a mean age of 84.49 (± 4.0) years. The mean SAPS II score was 27.05 (± 15.7), the mean CCI was 3.35 (± 2.28) and the most patient had an ASA score of 3 or higher. The PJI was located at the hip in 71.9% or at the knee in 24.6%. Two patients (3.5%) suffered from a PJI at both locations. Sixteen patients did not survive the ICU stay. Non-survivors showed significantly higher CCI (4.94 vs. 2.73; p = 0.02), higher SAPS II score (34.06 vs. 24.32; p = 0.03), significant more patients who underwent an invasive ventilation (132.7 vs. 28.1; p = 0.006) and significantly more patients who needed RRT (4.9% vs. 50%; p < 0.001). In multivariate analysis, RRT (odds ratio (OR) 15.4, CI 1.69–140.85; p = 0.015), invasive ventilation (OR 9.6, CI 1.28–71.9; p = 0.028) and CCI (OR 1.5, CI 1.004–2.12; p = 0.048) were independent risk factors for mortality.
Conclusion
Very elderly patients with PJI who needs to be admitted to the ICU are at risk to suffer from a poor outcome. Several risk factors including a chronic infection, high SAPS II Score, high CCI, invasive ventilation and RRT might be associated with a poor outcome.
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.
Similar content being viewed by others
Background
The term “silver tsunami” describes the progressively ageing population in developed countries and the huge socioeconomic shift that is expected to effect various clinical fields including the „rise and burden of hip and knee osteoarthritis “[1]. According to Kiadaliri et al. the number of prevalent osteoarthritis cases increased by 43% between 1990 and 2015. The number of knee osteoarthritis alone has doubled in prevalences since the mid-twentieth century [2]. Thus, the estimated prevalence of Total Hip (THR) and Total Knee Replacements (TKR) in the United States was 2,552,815 and 4,700,621 respectively in 2010. Out of these 640,740 (THR) and 1,087,400 (TKR) were at the age of 80 and higher [3].
Knee and hip arthroplasty are a succesful treatment for osteoarthritis in terms of pain relief, function recovery and enhancing life quality [4, 5]. Even though surgical techniques and implants have evolved, periprosthetic joint infection (PJI) remains a serious complication leading to poor postoperative outcome and a high mortality [6]. The incidence of PJI after total joint arthroplasty differs according to localization and type between 1 and 3% [7]. Up to now, there is no gold standard treatment for patients with PJI. In addition to the Musculoskeletal Infection Society (MSIS) criteria introduced by the American Academy of Orthopedic Surgeons (AAOS) in 2011 [8, 9], the concept of Trampuz and Zimmerli is well known in Europe [10, 11]. Furthermore, treatment of PJI often includes a prolonged hospital stay, multiple surgeries, prolonged antimicrobial treatment, protheses and medical supplies which can lead to a 24 times higher treatment cost [12, 13]. Several different risk factors have been described for PJI after Total Joint Arthroplasty including obesity, urinary tract infection, diabetes and rheumatoid arthritis [6]. However, the literature is conflicted when it comes to determine age as an independent risk factor. In developed countries the proportion of elderly patients admitted to the Intensive Care Unit (ICU) increased dramatically [14, 15]. The literature is lacking in studies reporting the mortality of very elderly patients with periprosthetic joint infections, especially in cases when an ICU treatment was necessary. We therefore present the first study analyzing patients with an age 80 and higher suffering from a periprosthetic joint infection who had to be admitted to the ICU.
Methods
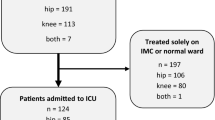
The study has been approved by the local Ethical Committee (No. of approval 18–6260-BR). From January 2012 and December 2016, all patients aged 80 and higher who suffered from a PJI (acute and chronic according to the definition as described by Li et al. [16]) after THR or TKR and who have been admitted to the ICU have been included in this retrospective, observational, single-center study. In defining periprosthetic joint infection all patients fullfilled criteria according to the European Bone and Joint Infection Society (EBJIS) and Musculoskeletal Infection Society (Table 1) [8, 9, 17]. The ICU consisted of 13-bed surgical intensive care unit in a Level 1 university and referral hospital for PJI in Germany. The ICU is accompanied by a stand-alone Intermediate Care Unit (IMC). The IMC ressourses and therapeutic options include an intensivist-led 24 h presence of a resident experienced in intensive care, monitoring corresponding to ICU-standard, non-invasive ventilation and continuous vasopressor-administration. Therefore, most surgical patients suffering PJI at risk or not stable enough for normal ward are admitted to the IMC. Severity of illness were assessed using the Simplified Acute Physiology Score II (SAPS II) [18], the American Society of Anaesthesiologists Score (ASA) [19] and the Charlson Comorbidity Index (CCI) [20].
Statistical analysis
Data were analyzed using SPSS version 21.0 (SSPS Inc., Chicago, IL) and Excel version 16.16.7 (Microsoft Corporation, Redmond, WA, USA). Univariate analysis was performed to compare demographics, surgical characteristics, and intensive care treatment. For categorical variables, frequency counts were computed and presented along with their percentages. For continuous variables, means were computed and presented along with their range. Mann Whitney U-test or Student’s T-Test were used, as appropriate. Statistical significance was set at p < 0.05. Multivariate analysis (binary logistic) was performed using the four most significant parameters in univariate analysis to determine independent risk factors for mortality.
Results
A total of 57 patients met the inclusion criteria. The cohort consisted of 24 males and 33 females with a mean age of 84.49 (± 4.0) years. The mean SAPS II score was 27.05 (± 15.7), the mean CCI was 3.35 (± 2.28) and the most patient had an ASA score of 3 or higher. The PJI was located at the hip in 71.9% or at the knee in 24.6%. Two patients (3.5%) suffered from a PJI at both locations. Most patients suffered from a chronic infection (86%) and underwent a planned surgical intervention (50.9%). The results are summarized in Tables 2, 3, 4.
Sixteen patients did not survive the ICU stay. In univariate analysis, non-survivors showed significantly higher CCI (4.94 vs. 2.73; p = 0.02), higher SAPS II score (34.06 vs. 24.32; p = 0.03), significant more patients who underwent an invasive ventilation (132.7 vs. 28.1; p = 0.006) and significantly more patients who needed renal replacement therapy (RRT) (4.9% vs. 50%; p < 0.001). Results are summarized in Table 5. In multivariate analysis, RRT (odds ratio (OR) 15.4, CI 1.69–140.85; p = 0.015), invasive ventilation (OR 9.6, CI 1.28–71.9; p = 0.028) and CCI (OR 1.5, CI 1.004–2.12; p = 0.048) were independent risk factors for mortality (Table 6).
Discussion
This study presents the first study ever to analyze the outcome of octagenarions in the setting of PJI and ICU treatment. PJI is a devastating complication resulting in severe pain, functional impairment and high mortality [21]. Furthermore, the estimated costs for infection revision is expected to be as high as $ 1.62 billion in the United States alone [22]. A validated risk score to assess and predict PJI does not exist. However, several risk factors have been discussed in the setting of PJI. Zuh et al. reported in their systematic review that body mass index, diabetes mellitus, corticosteroid therapy; hypoalbuminaemia, rheumatoid arthritis, blood transfusion, presence of a wound drain, wound dehiscence, superficial surgical site infection, coagulopathy, malignancy, immunodepression, National Nosocomial Infections Surveillance (NNIS) score ≥ 2, prolonged operative time and previous surgery are potential risk factors for PJI [23].
Even though most of these factors were not analyzed in detail in our study the vast majority of our patients had an ASA score of 3 and higher. Maaloum et al. reported a mortality rate of 20% in their retrospective case series analyzing 41 patients (mean age: 71.8 ± 9.4 years) suffering from a PJI admitted to the ICU. They could show as well that a high SAPS II score and a high ASA score is associated with a high mortality rate [24]. We also observed a significantly higher CCI in non-survivors compared to patients who have survived (4.94 ± 2.14 vs. 2.73 ± 2.04; p = 0.02). The proportion of patients requiring a RRT (50% vs. 4.9%; p < 0001) or invasive ventilation (56% vs. 20%; p = 0.006) was significantly higher in the non-survivor group in our study. These findings have been reported by several studies [25] and the same trends were observed by Maaloum et al. with more patients requiring RRT (50% vs, 15%; p = 0.05) or mechanical ventilation (88% vs. 76%; p = 0.66) in the non-survivor group [24].
The literature is conflicted with respect to determine age as an independent risk factor on survival in elderly patients. Martin-Loeches et al. reported in their prospective multicenter study that septic patients aged 80 and over have a higher hospital mortality compared to patients younger than 80 [14]. However, Flaatten et al. could show that the Clinical Frailty Scale is inversely associated with the 30-day survival. While 76% of the patients classified as “fit” were estimated to survive at 30 days following ICU admission only 59% of the patients who were classified as “frail” were estimated to survive the 30-day follow-up [26]. Our results also suggest that age per se has a smaller impact on survival than other factors such as the CCI, SAPS II and RRT [26, 27].
We observed a significantly higher rate of patients transferred from another ICU (31% vs. 5%; p = 0.006) in the non-survivor group. This might be explained by a delayed therapy, especially in cases when the septic prothesis has not been removed in the transferring hospital or the adequate antibiotic treatment has not been started. We did not analyze the surgical treatment delay in patients who have been transferred to our ICU. Nevertheless, previous studies have shown that an immediate treatment within the first hours is associated with a reduction in hospital mortality in very old patients [14, 28].
Treatment of very elderly patients admitted to the ICU is complex and represents an ongoing challenge for surgeons and intensive care specialists. Even though systematic ICU admissions of elderly patients failed to reduce the mortality [29] an appropriate and systematic approach with precise predictions models are needed for this patient group [30, 31].
Limitations
This study has several limitations: It is an observational, non-comperative, single-center cohort study in a retrospective setting, and therefore we may have missed data points and there is potential for bias or residual confounding from factors we did not measure. The available literature is lacking in comparible studies. Furthermore, there is a huge variety in the definition of acute and periprosthetic joint infections in the literature ranging from 4 up to 12 weeks. Therefore, conclusion based on our results should be drawn carefully.
However, this study is the first ever to report and analyze risk factors on survival in very elderly patients with PJI admitted to the ICU. More studies are warranted to better understand risk factors on mortality rates and offer these special patients the best possible treatment.
Conclusion
Very elderly patients with PJI who needs to be admitted to the ICU are at risk to suffer from a poor outcome. Several risk factors including a chronic infection, high SAPS II Score, high CCI, invasive ventilation and RRT might be associated with a poor outcome. Health care providers should inform these patients accordingly. The literature is lacking in studies analyzing this particular group of patients and further research is needed. Prospective multi-center cohort trials and comparative clinical trials represent a key area of opportunity for future studies.
Availability of data and materials
The data used and analyzed during the current study are available in anonymized form from the corresponding author on reasonable request.
Abbreviations
- AAOS:
-
American academy of orthopedic surgeons
- ASA:
-
American society of anaesthesiologists score
- CCI:
-
Charlson comorbidity index
- EBJIS:
-
European bone and joint infection society
- ICU:
-
Intensive care unit
- IMC:
-
Intermediate care unit
- MSIS:
-
Musculoskeletal infection society
- NNIS:
-
National nosocomial infections surveillance
- OR:
-
Odds ratio
- PJI:
-
Periprosthetic joint infection
- RRT:
-
Renal replacement therapy
- SAPS II:
-
Simplified acute physiology score II
- THR:
-
Total hip replacement
- TKR:
-
Total knee replacement
References
Kiadaliri AA, et al. High and rising burden of hip and knee osteoarthritis in the Nordic region, 1990-2015. Acta Orthop. 2018;89(2):177–83.
Wallace IJ, et al. Knee osteoarthritis has doubled in prevalence since the mid-20th century. Proc Natl Acad Sci U S A. 2017;114(35):9332–6.
Maradit Kremers H, et al. Prevalence of Total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97(17):1386–97.
Oleske DM, et al. Electronic health databases for epidemiological research on joint replacements: considerations when making cross-national comparisons. Ann Epidemiol. 2014;24(9):660–5.
Kurtz S, et al. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89(4):780–5.
Kong L, et al. Risk factors for periprosthetic joint infection following primary total hip or knee arthroplasty: a meta-analysis. Int Wound J. 2017;14(3):529–36.
Darouiche RO. Device-associated infections: a macroproblem that starts with microadherence. Clin Infect Dis. 2001;33(9):1567–72.
Parvizi J, et al. New definition for periprosthetic joint infection: from the workgroup of the musculoskeletal infection society. Clin Orthop Relat Res. 2011;469(11):2992–4.
Parvizi J, et al. The 2018 definition of periprosthetic hip and knee infection: an evidence-based and validated criteria. J Arthroplasty. 2018;33(5):1309–1314.e2.
Zimmerli W, Trampuz A, Ochsner PE. Prosthetic-joint infections. N Engl J Med. 2004;351(16):1645–54.
Trampuz A, Zimmerli W. Prosthetic joint infections: update in diagnosis and treatment. Swiss Med Wkly. 2005;135(17–18):243–51.
Alp E, et al. Incidence and economic burden of prosthetic joint infections in a university hospital: a report from a middle-income country. J Infect Public Health. 2016;9(4):494–8.
Haenle M, et al. Economic impact of infected total knee arthroplasty. ScientificWorldJournal. 2012;2012:196515.
Martin-Loeches I, et al. Risk factors for mortality in elderly and very elderly critically ill patients with sepsis: a prospective, observational, multicenter cohort study. Ann Intensive Care. 2019;9(1):26.
Nielsson MS, et al. Mortality in elderly ICU patients: a cohort study. Acta Anaesthesiol Scand. 2014;58(1):19–26.
Li C, Renz N, Trampuz A. Management of Periprosthetic joint infection. Hip Pelvis. 2018;30(3):138–46.
Ochsner, P., et al., Infections of the musculoskeletal system : basic principles, prevention, diagnosis and treatment. 2014: Grandvaux Swiss orthopaedics in-house-publisher 2014.
Le Gall JR, Lemeshow S, Saulnier F. A new simplified acute physiology score (SAPS II) based on a European/north American multicenter study. JAMA. 1993;270(24):2957–63.
Keats AS. The ASA classification of physical status--a recapitulation. Anesthesiology. 1978;49(4):233–6.
Charlson M, et al. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51.
Kunutsor SK, et al. Systematic review of risk prediction scores for surgical site infection or periprosthetic joint infection following joint arthroplasty. Epidemiol Infect. 2017;145(9):1738–49.
Haddad FS, Ngu A, Negus JJ. Prosthetic joint infections and cost analysis? Adv Exp Med Biol. 2017;971:93–100.
Zhu Y, et al. Risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. J Hosp Infect. 2015;89(2):82–9.
Maaloum Y, et al. Clinical spectrum and outcome of critically ill patients suffering from prosthetic joint infections. Infection. 2013;41(2):493–501.
Lai CC, et al. The outcomes and prognostic factors of patients requiring prolonged mechanical ventilation. Sci Rep. 2016;6:28034.
Flaatten H, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017;43(12):1820–8.
Boumendil A, et al. Variability of intensive care admission decisions for the very elderly. PLoS One. 2012;7(4):e34387.
Ferrer R, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med. 2014;42(8):1749–55.
Venkatesan P. Mortality in elderly patients with a systematic ICU admission programme. Lancet Respir Med. 2017;5(12):928.
Flaatten H, et al. The status of intensive care medicine research and a future agenda for very old patients in the ICU. Intensive Care Med. 2017;43(9):1319–28.
Kizilarslanoglu MC, et al. Is frailty a prognostic factor for critically ill elderly patients? Aging Clin Exp Res. 2017;29(2):247–55.
Acknowledgments
Not Applicable.
Funding
We acknowledge support by the DFG Open Access Publication Funds of the Ruhr-Universität Bochum.
Author information
Authors and Affiliations
Contributions
Study concept: UH, CW, EY, TAS. Study design: EY, AP, HB, SF. Data acquisition: UH, AP. Data analysis and interpretation: EY, UH, AP, CW, HB, TAS. Statistical analysis: UH, AP, EY. Manuscript editing: EY, HB, SF. Manuscript review: UH, CW, TAS. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has been approved by the local Ethical Committee of the Ruhr-University Bochum (No. of approval 18–6260-BR). Due to the retrospective nature of this study there was no need for consent to participate.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yilmaz, E., Poell, A., Baecker, H. et al. Poor outcome of octogenarians admitted to ICU due to periprosthetic joint infections: a retrospective cohort study. BMC Musculoskelet Disord 21, 304 (2020). https://doi.org/10.1186/s12891-020-03331-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-020-03331-0