Abstract
Background
Atrophic nonunion of femoral shaft fracture after intramedullary (IM) nailing is uncommon. The treatment for femoral shaft aseptic atrophic non-union remained controversial. The aim of this study was to compare the surgical results between exchanging reamed nailing (ERN) and augmentative antirotational plating (AAP) for femoral shaft aseptic atrophic nonunion.
Methods
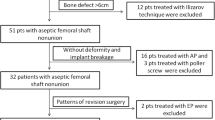
We retrospectively reviewed the patients with femoral shaft nonunion between the year of 2014 and 2015. The patients with nonunion after plate osteosynthesis, septic nonunion, hypertrophic nonunion, additional surgery during revision surgery were excluded. All the patients were followed up at least 12 months.
Results
Overall, the union rate after revision surgery was 70.8%. The union rate was significantly higher in the AAP group than in the ERN group. Operating time was also significantly shorter in the AAP group. Regarding the location of nonunion, the union rate was comparable between groups for isthmic nonunions. However, for non-isthmic nonunions, the union rate was significantly higher and operating time was significantly shorter in the AAP group.
Conclusion
AAP showed an overall higher union rate for management of femoral shaft aseptic atrophic nonunion compared with ERN. Especially for non-isthmic femoral shaft atrophic nonunions, AAP provided a significantly higher union rate and significantly shorter operating time.
Similar content being viewed by others
Background
Femoral shaft fracture is a common injury resulting from high-energy trauma, such as high-speed motor vehicle accidents and falls. A fractured femoral shaft always requires surgery to improve the patient’s short- and long-term outcomes. To date, closed reduction with intramedullary (IM) nailing is the treatment of choice for management of closed femoral shaft fracture owing to its high union rate and satisfactory surgical outcomes [1,2,3,4,5,6,7]. Despite the advantages of IM nailing for femoral shaft fracture, several complications still exist, including aseptic nonunion [6, 7].
Femoral shaft aseptic nonunion after IM nailing is considered to be rare, but recent studies suggest that the nonunion rate could range from 1.1 to 14% [5,6,7,8]. Either surgical or nonsurgical treatment has been recommended to stimulate the healing process and achieve fracture union in the literature [9,10,11]. Among different surgical interventions, exchanging reamed nailing (ERN) and augmentative antirotational plating (AAP) are the 2 primary recommended interventions for management of femoral shaft aseptic nonunion.
The choice of revision surgery for femoral shaft aseptic nonunion depends on the characteristics of the nonunion itself. Aseptic hypertrophic nonunion may result from inadequate fixation stability, thus requiring additional surgical procedures to provide a more stable environment for fracture union. In this circumstance, either ERN or AAP in revision surgery could result in a satisfactory union rate [12, 13]. On the other hand, loss of bone viability after fracture may result in aseptic atrophic nonunion. Although AAP with bone grafting seems more suitable theoretically than ERN in this circumstance, there is no consensuses on which surgical intervention is superior [13,14,15,16].
The purpose of this retrospective study was to determinate the optimal treatment for femoral shaft atrophic nonunion. We compare the surgical results between ERN and AAP in revision surgery for this type of nonunion after IM nailing at a single institution. In addition, we also attempted to identify an appropriate treatment based on the location of nonunion.
Methods
In the current study, we reviewed the medical records of patients at our institution between July 2004 and December 2015. The inclusion criterion was patients who underwent revision surgery for aseptic atrophic nonunion after IM nailing for management of femoral shaft fracture. Patients who previously underwent other osteosynthesis surgeries, such as plate osteosynthesis surgery, as initial management for femoral shaft fracture were excluded from the study. Moreover, patients who were suspected of having subclinical septic nonunion, underwent limb lengthening procedures during revision surgery, or had additional pathologic fracture were also excluded. In addition, in order to narrow and specify the results of the current study, patients who had nonunion classified as hypertrophic were also excluded. The medical record reviewing process was approved by our Institutional Review Board (No. 201600790B0) and processed by a single investigator (L. P.-J.).
To standardize the collection of data, we adapted several well-accepted criteria for nonunion, including septic or aseptic nonunion, type of nonunion, and anatomical location of nonunion. First, nonunion was defined as (1) a patient with persistent pain at the fracture site at least 6 months after the primary osteosynthesis surgery; (2) a fracture without complete healing at 6 months on radiographic examination; or (3) a lack of progressive healing for 3 consecutive months on radiographic follow-up [17].
Second, the current retrospective study aimed to review the outcomes of treatment for femoral shaft nonunion without infection; therefore, patients who had femoral shaft septic nonunion were excluded from the study. Diagnosis of septic nonunion was based on intraoperative tissue biopsy from a specimen obtained from non-united ends of the femoral shaft. There were 3 sets of tissue biopsies for each nonunion during surgery, and patients were enrolled in the study if all results were negative for bacterial growth.
Third, the criteria for nonunion were consistent with previous studies [18]. Hypertrophic nonunion referred to a fracture line persisting beyond the expected time for union, with callus in variable amounts about the fracture site on radiographic examination. On the contrary, atrophic nonunion referred to a fracture line persisting beyond the expected time for union, with no demonstrable callus on radiographic examination.
Last, the anatomical definition of the femoral shaft was defined according to the Arbeitsgemeinschaftfür Osteosynthesefragen (AO) classification, which refers to the area from the lower edge of the lesser trochanter to the upper border of the trans-epicondylar width of the knee. The anatomical location of femoral shaft nonunion was further divided into isthmic and non-isthmic [19].
The surgical techniques of ERN and AAP followed the descriptions in previous literature [20,21,22,23]. In the ERN group, the former IM nail was removed through a previous surgical wound. Then, the femoral medulla was prepared using a reaming technique (Fig. 1). We chose a new nail that was 1 to 2 mm larger than the previous nail, according to the size of the femur. In addition, all locking screws were placed in a static position. During the study period, there were 3 different antegrade femoral nails available at our institution (2004–2010: Russell-Taylor femoral interlocking nail; Smith & Nephew, Memphis, TN; 2010–2014: M/DN nail; Zimmer-Biomet, Warsaw, IN; since 2014: King Bo femur interlocking nail; Syntec Scientific Co, Changhwa, Taiwan). The choices of applied femoral interlocking nail during each period were based on the introduction policy in our hospital. No additional bone grafts were applied over the nonunion site.
In the AAP group, the former IM nail was left in place, whether or not the nail was broken. A new incision, usually 10 to 12 cm in length, was made over the nonunion site. After debridement, the interposed tissue between the nonunited ends was decorticated until bleeding, and a broad dynamic compression plate (DCP; DePuy Synthes, Johnson & Johnson, Raynham, MA) was applied (Fig. 2). A plate with appropriate length was chosen and fixation was achieved with compression cortical screws through near-all-cortex purchases just next to and passing by the IM nail. Autologous cancellous bone graft was harvested from the iliac crest and implanted over the nonunion site after decortication in all cases.
A 38-year-old woman who had a motor vehicle accident. a Left femoral shaft fracture below the isthmus. b and c Twelve months after intramedullary nail fixation with atrophic nonunion. d Augmentative antirotational plating with a dynamic compression plate. e and f Solid union at 5 months after surgery
The primary outcome was bony union after surgery, with the endpoints of evaluation being either nonunion becoming united or any new surgical intervention being performed. Clinically, union was defined as the patient’s full-weight ambulation without pain or discomfort. Radiographically, union was defined as a continuous cortex in 3 of 4 cortices on anteroposterior and lateral radiographs.
Data were analyzed using SPSS version 18.0 statistical software (SPSS Inc., Chicago, IL). Nonparametric variables were compared using the Pearson chi-squared or Fisher exact test, while continuous variables were analyzed using the student t test. The level of significance was set at P ≤ 0.05.
Results
From July 2004 to December 2015, 138 patients underwent revision surgery for femoral shaft aseptic nonunion at our institution. Among the 138 patients, 42 who had aseptic hypertrophic nonunion were excluded. Therefore, 96 patients with femoral shaft aseptic atrophic nonunion were enrolled in this study, including 54 men and 42 women. Forty-eight patients (50%) underwent open reduction and fixation as the primary surgical intervention based on evidence of a surgical scar over the fracture site or cerclage wire on radiography. Among the 96 patients, 70 underwent revision osteosynthesis surgery with ERN and 26 with AAP. At the end of the follow-up period, bony union was observed in 68 cases (union rate, 70.8%). Demographic data are shown in Table 1; there were no significant differences among all variables between groups, regardless of the location of nonunion. The results of different femoral interlocking nail in revision osteosynthesis surgery with ERN was shown in Table 2, which revealed no significant difference in union rate (P = 0.66, chi-square analysis) and time to union (P = 0.89, ANOVA analysis).
The data showed a significantly higher union rate in the AAP group than in the ERN group (88.5% vs 64.3%; P = 0.021). Another advantage of revision surgery with AAP was also revealed with regard to operating time (AAP vs ERN: 128.4 vs 169.5 min; P = 0.0047). Time to union, however, showed no significant difference between groups (Table 3).
We further subdivided patients into 2 groups based on the anatomical location of nonunion, isthmic and non-isthmic (Table 4). In patients with isthmic nonunion, the union rate after revision surgery was 69.8%, and there was no significant difference between groups (AAP vs ERN: 84.6% vs 66%; P = 0.19). However, in patients with non-isthmic nonunion, the union rate was significantly higher in the AAP group than in the ERN group (92.3% vs 72.7%; P = 0.04; Table 3).
Discussion
The current study evaluated the outcomes of patients with femoral shaft aseptic atrophic nonunion after revision surgery with either AAP or ERN during a decade at a single institution. Based on the study results, revision surgery with AAP had a higher union rate and shorter operating time than ERN. Furthermore, the data regarding the anatomical location of nonunion showed an advantage in union rate for non-isthmic nonunions treated with AAP rather than ERN, but not for isthmic nonunions.
The use of AAP or ERN in revision surgery for femoral shaft nonunion has been reported in the literature. Both interventions have shown good to satisfactory outcomes [20,21,22,23,24,25], but few studies have compared the surgical outcomes between techniques. A 40-case series reported by Jhunjhunwala [14] showed that plating is an effective treatment for nonunion of diaphyseal femoral fractures after IM fixation with the nail in situ. At the same time, Ru et al. [26] published a series of 28 patients who underwent either ERN (11 patients) or AAP (17 patients) and reported that AAP achieved satisfactory clinical outcomes, shorter operating time, lower blood loss, and less trauma than ERN. Our results are basically consistent with these 2 studies. However, our study provides even more powerful evidence that AAP is more advantageous than ERN. First, only patients with femoral shaft aseptic fractures of atrophic type were enrolled in the study. Thus, the study results should be more convincing than previous studies, which investigated both hypertrophic and atrophic femoral shaft aseptic nonunions. Second, we included a large number of patients from a single institution. We performed a post-hoc power analysis using G*Power software version 3.1.9.2 (Franz Paul, University Kiel, Germany) and found that at a significance level of 0.05 and with a total sample size of 96, we had 99% power to detect the difference in union rate.
Another issue to be addressed is which type of revision technique to use based on the anatomical location of nonunion. Previous studies have shown a trend toward using ERN for isthmic nonunions and AAP for non-isthmic nonunions [27]. ERN for femoral shaft nonunion was a generally agreed-upon method because of its advantages including a simple technique, internal bone grafting from reaming, better cosmetic result, and promising union rate [15, 16, 28,29,30,31]. Especially for isthmic nonunions, a nail that is 1 to 2 mm larger in diameter can fit the isthmus well during the revision surgery, thus increasing the bending stiffness. However, for non-isthmic nonunions, a new and larger nail might not fit the medulla well, and residual torsional instability might remain. Yang et al. [27] reviewed 41 patients who had non-isthmic nonunion after femoral shaft fracture who underwent ERN as the revision surgery; a 22% union failure rate was observed in their study. Park et al. reported an 18-case series of non-isthmic femoral shaft nonunions in which AAP showed a better union rate than ERN [25]. In our study, we found that the union rates for AAP and ERN were comparable for femoral shaft aseptic atrophic nonunions located at the isthmic region. However, there were advantages in union rate and operating time for non-isthmic nonunions treated with AAP rather than ERN.
Which type of plate to use during AAP for femoral shaft aseptic atrophic nonunion remains a controversial issue. A multicenter, retrospective study from Ru et al. [32], with a total of 180 cases, revealed that plating with autologous bone grafting has a 100% union rate. However, the authors expressed the results of the plating group with 2 different implants (a locked compression plate and DCP), and autologous bone graft was used for all nonunion patterns, irrespective of being hypertrophic or atrophic. In our study, only one DCP was used in all cases, and the mechanism of augmentation was such that the DCP provided antirotational strength by rigid fixation. We found that through radical decortication at the nonunited ends, adequate autologous bone grafting, and adding absolute stability by applying a DCP, satisfactory surgical outcomes were achieved.
Despite careful review of the medical records, there were limitations of the current study. First, it was a retrospective study over a 12-year period, with several orthopedic surgeons involved. The disease coding system has matured in recent few years, which might have caused data collection bias among cases in the earlier years. Also, the actual number of patients may be higher than the presented data. Second, we used clinical symptoms and serial radiographic follow-up to determine femoral shaft nonunion during the study period. The actual incidence of femoral shaft nonunion might be higher than the presented data with more-sensitive imaging examination, such as computed tomography. Third, AAP for femoral shaft nonunion has been performed more frequently in recent years; therefore, the number of cases in the AAP group was lower than that in the ERN group. Further studies should recruit more patients in both groups for better statistical outcomes. However, a major strength of this study was the standardized surgical techniques with uniform implants in both groups at a single institution. In addition, the quality of data analysis was high because the data were collected and analyzed by an independent examiner with no interest in the patients’ treatment (L.P.J.).
Conclusions
In conclusion, both ERN and AAP for femoral shaft atrophic nonunion were effective, but AAP showed an overall higher union rate. Especially for non-isthmic femoral shaft atrophic nonunions, AAP provided a considerably better union rate and shorter time to union.
Abbreviations
- AAP:
-
Augmentative antirotational plate
- ERN:
-
Exchanging reamed nail
- IM:
-
Intramedullary
References
Deepak MK, Jain K, Rajamanya KA, et al. Functional outcome of diaphyseal fractures of femur managed by closed intramedullary interlocking nailing in adults. Ann Afr Med. 2012;11:52–7.
Ricci WM, Bellabarba C, Evanoff B, et al. Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma. 2001;15:161–9.
Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg. 2009;17:296–305.
Winquist RA, Hansen ST Jr, Clawson DK. Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Joint Surg Am. 1984;66:529–39.
Wolinsky PR, McCarty E, Shyr Y, et al. Reamed intramedullary nailing of the femur: 551 cases. J Trauma. 1999;46:392–9.
Karadimas EJ, Papadimitriou G, Theodoratos G, et al. The effectiveness of the antegrade reamed technique: the experience and complications from 415 traumatic femoral shaft fractures. Strategies Trauma Limb Reconstr. 2009;4:113–21.
Umer M, Niazi AK, Hussain D, et al. Treatment of acute fractures of the femoral shaft with reamed intramedullary interlocking AO nails. J Pak Med Assoc. 2004;54:423–7.
Pihlajamäki HK, Salminen ST, Böstman OM. The treatment of nonunions following intramedullary nailing of femoral shaft fractures. J Orthop Trauma. 2002;16:394–402.
Alkhawashki HM. Shock wave therapy of fracture nonunion. Injury. 2015;46:2248–52.
Guimarães JA, Duarte ME, Fernandes MB, et al. The effect of autologous concentrated bone-marrow grafting on the healing of femoral shaft non-unions after locked intramedullary nailing. Injury. 2014;45(Suppl 5):S7–S13.
Nozaka K, Shimada Y, Miyakoshi N, et al. Combined effect of teriparatide and low-intensity pulsed ultrasound for nonunion: a case report. BMC Res Notes. 2014;7:317.
Yu CW, Wu CC, Chen WJ. Aseptic nonunion of a femoral shaft treated using exchange nailing Chang gung. Med J. 2002;25:591–8.
Somford MP, van den Bekerom MP, Kloen P. Operative treatment for femoral shaft nonunions, a systematic review of the literature. Strategies Trauma Limb Reconstr. 2013;8:77–88.
Jhunjhunwala HR, Dhawale AA. Is augmentation plating an effective treatment for non-union of femoral shaft fractures with nail in situ? Eur J Trauma Emerg Surg. 2016;42:339–43.
Maimaitiyiming A, Amat A, Rehei A, et al. Treatment of the femoral shaft nonunion with double plate fixation and bone grafting: a case series of 14 patients. Injury. 2015;46:1102–7.
Lin CJ, Chiang CC, Wu PK, et al. Effectiveness of plate augmentation for femoral shaft nonunion after nailing. J Chin Med Assoc. 2012;75:396–401.
Tay Cleveland KB. Delayed union and nonunion of fractures. In: Canale ST, Beaty JH, eds. Canale & Beaty: Campbell’s Operative Orthopaedics. Version 12. Philadelphia: Mosby; 2013: chapter 59.
Frölke JP, Patka P. Definition and classification of fracture non-unions. Injury. 2007;38(Suppl 2):S19–22.
Su XY, Zhao JX, Zhao Z, et al. Three-dimensional analysis of the characteristics of the femoral canal isthmus: an anatomical study. Biomed Res Int. 2015;2015:459612.
Wu CC. Exchange nailing for aseptic nonunion of femoral shaft: a retrospective cohort study for effect of reaming size. J Trauma. 2007;63:859–65.
Wu CC, Chen WJ. Treatment of femoral shaft aseptic nonunions: comparison between closed and open bone-grafting techniques. J Trauma. 1997;43:112–6.
Ueng SW, Chao EK, Lee SS, et al. Augmentative plate fixation for the management of femoral nonunion after intramedullary nailing. J Trauma. 1997;43:640–4.
Ueng SW, Shih CH. Augmentative plate fixation for the management of femoral nonunion with broken interlocking nail. J Trauma. 1998;45:747–52.
Hierholzer C, Glowalla C, Herrler M, et al. Reamed intramedullary exchange nailing: treatment of choice of aseptic femoral shaft nonunion. J Orthop Surg Res. 2014;9:88.
Park J, Kim SG, Yoon HK, et al. The treatment of nonisthmal femoral shaft nonunions with IM nail exchange versus augmentation plating. J Orthop Trauma. 2010;24:89–94.
Ru I, Cang H, Hu C, et al. Comparison of two surgical methods for aseptic nonunions of femoral shaft orthopaedic surgery [in Chinese]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2013;27:25–9.
Yang KH, Kim JR, Park J. Nonisthmal femoral shaft nonunion as a risk factor for exchange nailing failure. J Trauma Acute Care Surg. 2012;72:E60–4.
Furlong AJ, Giannoudis PV, DeBoer P, et al. Exchange nailing for femoral shaft aseptic non-union. Injury. 1999;30:245–9.
Hak DJ, Lee SS, Goulet JA. Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma. 2000;14:178–82.
Oh JK, Bae JH, Oh CW, et al. Treatment of femoral and tibial diaphyseal nonunions using reamed intramedullary nailing without bone graft. Injury. 2008;39:952–9.
Shroeder JE, Mosheiff R, Khoury A, et al. The outcome of closed, intramedullary exchange nailing with reamed insertion in the treatment of femoral shaft nonunions. J Orthop Trauma. 2009;23:653–7.
Ru JY, Niu YF, Cong Y, et al. Exchanging reamed nailing versus augmentative compression plating with autogenous bone grafting for aseptic femoral shaft nonunion: a retrospective cohort study. Acta Orthop Traumatol Turc. 2015;49:668–75.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
Author information
Authors and Affiliations
Contributions
Conceptualization: PJL, YHY and SWNU; Investigation: PJL, YH and YCC; Writing: PJL and YHY; Writing -Review and Editing: WLY; Supervision: SWNU. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
-
1.
The study protocol was approved by the Institutional Review Board (No. 201600790B0) of Chang Gung Memorial Hospital.
-
2.
The consent obtained from study participants was written.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lai, PJ., Hsu, YH., Chou, YC. et al. Augmentative antirotational plating provided a significantly higher union rate than exchanging reamed nailing in treatment for femoral shaft aseptic atrophic nonunion - retrospective cohort study. BMC Musculoskelet Disord 20, 127 (2019). https://doi.org/10.1186/s12891-019-2514-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-019-2514-3