Abstract
Background
Axial spondyloarthritis (ax-SpA) is a chronic inflammatory disease of the spine causing pain, stiffness, loss in physical function, and fatigue. Therefore, the physical and psychological burden of having this chronic disease can reduce the quality of life. We aimed to explore the relationship between demographic- and disease-related variables and health-related quality of life (HRQoL) in patients with ax-SpA.
Methods
Demographic- and disease-related, HRQoL-related and treatment data were collected. Disease measures included the Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), the BAS Functional Index (BASFI), the BAS Global (BAS-G) score, the Maastricht Ankylosing Spondylitis Enthesitis Score (MASES), the Health Assessment Questionnaire (HAQ) and co-morbidity. HRQoL was assessed using the SF-36 and the utility measures SF-6D and 15D. Variables associated with HRQoL were identified in unadjusted and adjusted analyses.
Results
We examined 380 patients with ax-SpA (67% men) with a mean age of 46 years. Among them, 86% reported exercising >1 h per week. Mean values were as follows: BASDAI, 3.17; MASES, 3.19; BASFI, 2.71; BAS-G. 3.88; and HAQ, 0.56. The percentage of current users of NSAIDs was 44%, and of DMARDs 23%. In multivariate analyses, exercising 1–3 h per week (B = 2.73, p = 0.022) and exercising >3 h per week (B = 2.71, p = 0.020), lower HAQ scores (B = −4.61, p = 0.001), lower BASFI scores (B = −1.05, p = 0.010) and lower BAS-G scores (B = −0.91, p = 0.001) were independently associated with higher SF-36-PCS scores, whereas modest alcohol consumption (B = 4.63, p = 0.018) and a lower BAS-G score (B = −1.73, p < 0.001) were independently associated with higher SF-36-MCS scores. Exercising 1–3 h per week (B = 0.032, p = 0.004) and exercising >3 h per week (B = 0.036, p = 0.001), lower HAQ scores (B = −0.051, p < 0.001), lower BAS-G scores (B = −0.010, p < 0.001) and co-morbidity (B = −0.014, p = 0.004) were independently associated with higher 15D scores. Finally, exercising 1–3 h per week (B = 0.045, p = 0.001) and exercising > 3 h per week (B = 0.053, p < 0.001), lower HAQ scores (B = −0.054, p = 0.001) and lower BAS-G scores (B = −0.020, p < 0.001) were associated with higher SF-6D scores.
Conclusions
In patients with ax-SpA, a low level of physical activity, impaired physical function and impaired general well-being were independently and consistently associated with a decreased HRQoL across all applied measures.
Similar content being viewed by others
Background
Axial spondyloarthritis (Ax-SpA) is a chronic, systemic inflammatory rheumatic disease affecting the axial skeleton. Its inflammatory disease processes can also involve peripheral joints, entheses and internal organs [1, 2]. Most frequently, the disorder presents with an insidious onset of back pain in early adulthood, and typically causes fatigue, stiffness and loss in physical function [2, 3]. The psychological burden of having such a chronic disease in addition to the somatic symptoms can have a major impact on the health-related quality of life (HRQoL) in patients with ax-SpA, both for patients with ankylosing spondylitis (AS) and non-radiographically determined ax-SpA, even at a young age [4,5,6,7]. HRQoL is a subjective and multidimensional concept and can be defined as an individual’s experience of their general health state, such as physical, social and mental well-being [8].
Data from the literature indicate no differences in HRQoL between patients with AS and non-radiographically determined ax-SpA [9]. Furthermore, patients with ax-SpA have reported HRQoL scores that are similar to other inflammatory diseases such as psoriasis and inflammatory bowel disease [10, 11]. However, patients with ax-SpA report lower HRQoL than do healthy controls [3, 12], and women with the disease report a lower HRQoL than do men [2, 13, 14]. Decreased HRQoL in patients with ax-SpA is associated with fatigue [15], increased disease activity, decreased daily activity and exercise [16,17,18], pain, and adverse psychological factors such as body image disturbance, anxiety and depression [6, 19].
HRQoL measurements can be used for economic evaluation (cost–utility analysis), and several generic utility instruments (e.g., 15D, SF-6D and EQ5D) [20, 21] have been developed. The utility measures can also be used to calculate quality-adjusted life years (QALYs) [20, 21]. Furthermore, HRQoL can be assessed using other generic HRQoL measures such as the well-known SF-36 [22, 23].
There is sparse knowledge on the associations between demographic- and disease-related variables and HRQoL using utility measures in patients with ax-SpA, especially after the introduction of new and more targeted medications [24]. Therefore, the aim of this study was to explore the relationships between demographic- and disease-related variables and HRQoL in patients with ax-SpA, using the utility measures 15D and SF-6D and the generic HRQoL measure SF-36.
Methods
Patient recruitment
Patients with ax-SpA included in this study were recruited consecutively from two outpatient rheumatology clinics, one located in the eastern part of Norway (Martina Hansens Hospital, MHH) and the other in the southern part (Sorlandet Hospital, SSHF), which also have been described previously [25]. The patients had to be 18 years or older and needed to meet the Assessment of Spondyloarthritis International Society (ASAS) criteria for ax-SpA [26].
Data collection
A broad spectrum of demographic, disease- and treatment-related data was collected using physical examinations, laboratory tests, interviews and questionnaires [25]. Demographic data included age, gender, education level, work status, physical exercise, body mass index (BMI), smoking and alcohol consumption. Disease duration was defined as the time between the date fulfilling the ASAS criteria for ax-SpA and the date for inclusion in the study, and human leucocyte antigen (HLA)-B27 status was registered. Disease activity was assessed using the Bath Ankylosing Spondylitis Activity Index (BASDAI), the Maastricht Ankylosing Spondylitis Enthesitis Score (MASES) and C-reactive protein (CRP) level. Physical function was assessed by the Bath Ankylosing Spondylitis Functional Index (BASFI) and the Health Assessment Questionnaire (HAQ) [27]. Data on the Bath Ankylosing Spondylitis Patient Global Score (BAS-G) and morning stiffness were also collected. Any additional current medications including the use of non-steroidal anti-inflammatory drugs (NSAIDs), synthetic disease-modifying anti-rheumatic drugs (DMARDs), biological DMARDs and prednisolone were also recorded. Data on co-morbidities (yes/no) (heart diseases, pulmonary diseases; neurological, endocrine, haematological, gastro-intestinal, urogenital, other rheumatology diseases, mental disorders and cancers) were collected, and we computed a summed score to reflect co-morbidity. This score has also been used in other studies [25, 28, 29].
HRQoL was assessed using both the SF-36 and 15D tools, which also has been described previously [30]. The former is a self-reported and generic questionnaire, including eight domains: general health, bodily pain, physical function, role limitations (physical), mental health, vitality, social function and role limitations (emotional). The eight domains can be combined into a physical and mental sum scale that reflects physical and mental health. The physical component summary (PCS) and the mental component summary (MCS) scales were also used in this study. Regression analyses were performed to impute missing values in accordance with the instruction by the developer of the questionnaire [22, 23]. The SF-36 scales were scored according to published scoring procedures, and each scale was expressed using values from 0 to 100, with 100 representing excellent health [22, 23, 31, 32].
From the SF-36 score we also generated the utility measure SF-6D [21]. This is based on 11 questions from the SF-36 and includes six dimensions, each with four to six levels. The SF-6D utility scores range from 0.29 to 1.00, with 1.00 indicating “full health”. The Norwegian standard SF-36 version 1.00 was used to derive the SF-6D. Regression analyses were performed to impute missing values in accordance with instructions published by the developer of the questionnaire [21, 22]. The SF-6D questionnaire has been validated for its psychometric properties in other studies in several countries [21].
The 15D questionnaire is a generic, multidimensional, standardized evaluation tool of HRQoL that can be used primarily as a single index measure, but also as a profile utility measure, which has been described previously [28]. It describes the patient’s health status, assessing 15 dimensions: mobility, vision, hearing, breathing, sleeping, eating, speech, elimination, usual activities, mental function, discomfort and symptoms, depression, distress, vitality and sexual activity [20]. Each dimension comprises one question with five response categories. A single utility index score is obtained by incorporating population-based preference weights to the dimensions [33, 34]. The utility scores fall between 0.0 (being dead) and 1.00 (no problems on any dimension). Regression analyses were performed to impute missing values in accordance with the guidelines published by the developer of the questionnaire [20]. The questionnaire has been validated thoroughly for psychometric properties in other studies in several countries [20, 33, 34].
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics (IBM Corp., Armonk, NY, USA (version 22)). Continuous variables are presented as the mean and standard deviation (SD, in parentheses) and categorical variables as numbers and proportions (%). Chi-squared tests and Student’s t tests were used to compare differences between subgroups. To further examine the differences in SF-36 scores between our patients and norm-based scores, we calculated the effect size, calculated by subtracting the mean SF-36 scores in the patients from the mean SF-36 scores in the general population and then dividing by the SD for the general population [35]. We applied Cohen’s standards for effect size values as: small effect 0.2; medium effect 0.5; and large effect 0.8 [36].
Multiple linear regression analysis (general linear model (GLM) in SPSS) was used to examine the adjusted association between demographic- and disease-related variables and HRQoL (SF-36-PCS, SF-36-MCS, 15D and SF-6D scores). The independent variables in the multiple analyses were chosen based on univariate associations with HRQoL, clinical experience and factors associated with HRQoL in previous studies [6, 15, 37]. In the final multivariate model, we included the demographic variables, disease activity (assessed by BASDAI and MASES scores), health status (assessed by HAQ, BASFI and BAS-G scores), damage (assessed by BASMI score), co-morbidity and treatment centre as independent variables. Treatment, disease duration and morning stiffness were also tested in the models as independent variables; however, the same patterns persisted when exploring these associations with HRQoL as dependent variables, so were excluded. The final tested variables are listed in Table 3. For robustness, we also tested the models by backward multiple regression analyses. The level of significance was set at p < 0.05.
Ethical and legal aspects
The study was approved by the Regional Committee for Medical Research Ethics (REK # 4.2007.2152).
Results
Demographic- and disease-related characteristics
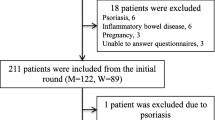
In total, 389 patients with ax-SpA were included in the study. Among these, 380 gave valid responses to the main HRQoL measure SF-36, and comprised the final sample. The only significant difference between the non-responders (n = 9) and responders to SF-36 was age (57.7 (SD 7.1) vs. 45.5 (12.0) years (p = 0.001).
When comparing demographic variables listed in Table 1 between the two centres, MHH (n = 252) and SSHF (n = 128), a statistically significant difference was identified for duration of education >13 years (60% vs. 49%; p = 0.038). Concerning disease-related variables, patients from MHH had better outcomes compared with SSHF in terms of BASDAI (2.9 (2.1) vs. 3.7 (2.1), p = 0.001); BASFI (2.5 (2.2) vs. 3.0 (2.3), p = 0.045); BAS-G (3.6 (2.5) vs. 4.4 (2.6), p = 0.009); and MASES (2.4 (2.90) vs. 4.90 (4.66), p < 0.001). Patients from MHH currently used more biological DMARD treatment than those from SSHF (30% vs. 9%, p < 0.001). For the remaining variables in Table 1, there were no significant differences between the centres. For the analysis, we pooled the patient data and adjusted for the two centres in multivariate analyses.
The mean age for the 380 patients was 45.8 (12.0) years; 67% were men; 75% were married or cohabiting; 51% reported exercising >3 h per week and 35% 1–3 h per week. Mean outcome values were as follows: BASDAI 3.17 (2.11); MASES 3.19 (3.75); BASFI 2.71 (2.23); BAS-G 3.88 (2.57); and HAQ 0.56 (0.49). Current users of NSAIDs comprised 44% of the sample versus 23% for biological DMARDs, and 90% were HLA-B27 positive. When comparing women and men with ax-SpA (Table 1), women had a lower BMI (25.5 (4.7) vs. 27.5 (4.5) kg/m2; p < 0.001) and lower alcohol consumption (1–6 glasses per week (67% vs. 71%), more than 7 glasses per week (7% vs. 13%) p = 0.012). Women reported higher MASES (4.42 (3.85) vs. 2.57 (3.53), p < 0.001), lower BASMI (2.03 (1.60) vs. 2.38 (2.19), p = 0.013) and higher HAQ scores (0.64 (0.53) vs. 0.52 (0.47), p = 0.034). For the other variables listed in Table 1, no statistically significant differences were found between men and women.
HRQoL in patients with ax-SpA
When comparing HRQoL between the MHH and SSHF centres, patients from MHH reported higher scores for the SF-36 domains: vitality (49.5 (20.2) vs. 44.3 (20.0), p = 0.019); bodily pain (51.0 (20.0) vs. 43.6 (20.9), p = 0.001), physical role limitations (46.7 (41.8) vs. 34.9 (35.5), p = 0.014); SF-36-PCS (40.6 (9.1) vs. 37.7 (10.0), p = 0.006); and SF-6D (0.67 (0.10) vs. 0.64 (0.10), p = 0.003).
When comparing HRQoL between women and men (Table 2), women reported significantly lower scores for the SF-36 domains of bodily pain (45.3 (19.8) vs. 50.1 (20.5), p = 0.025) and physical role limitations (36.5 (39.8) vs. 46.5 (41.7), p = 0.024). However, when comparing the SF-36 scores in patients with ax-SpA and published norm-based SF-36 reference data for the general population [35], the patients reported significantly lower scores (p < 0.001) for all eight SF-36 dimensions. The differences in effect size for the SF-36 dimensions were as follows: mental health −0.20; vitality −0.63; bodily pain −0.90; general health −0.98; social function −0.49; physical function −0.63; physical role −0.89; and emotional role −0.38.
Adjusted associations between demographic- and disease-related variables and HRQoL
In the multivariate analyses (Table 3), exercising 1–3 h per week (B = 2.73, p = 0.022) and exercising >3 h per week (B = 2.71, p = 0.020), lower HAQ scores (B = −4.61, p = 0.001), lower BASFI scores (B = −1.05, p = 0.010) and lower BAS-G scores (B = −0.91, p = 0.001) were independently associated with higher SF-36-PCS values. Modest alcohol consumption (B = 4.63, p = 0.019) and lower BAS-G scores (B = −1.73, p < 0.001) were independently associated with higher SF-36-MCS. Exercising 1–3 h per week (B = 0.032, p = 0.004) and exercising >3 h per week (B = 0.036, p = 0.001), lower HAQ scores (B = −0.051, p < 0.001), lower BAS-G scores (B = −0.010, p < 0.001) and co-morbidity (B = −0.014, p = 0.004) were independently associated with a higher 15D score. Finally, exercising 1–3 h per week (B = 0.045, p = 0.001) and exercising >3 h per week (B = 0.053, p < 0.001), lower HAQ scores (B = −0.054, p = 0.001) and lower BAS-G scores (B = −0.020, p < 0.001) were associated with higher SF-6D scores. The demographic- and disease-related variables included in the multiple analyses explained 57.1% of the variance in SF-36-PCS, 21.5% in SF-26-MCS, 60.2% in the 15D scores and 56.9% in the SF-6D scores. The same results were seen when the multivariate model was run backwards (data not shown).
Discussion
When exploring the associations between demographic- and disease-related variables and HRQoL in patients with ax-SpA, our main finding was that low levels of exercise, impaired physical function (HAQ scores) and impaired general disease-associated well-being (BAS-G scores) were consistently and independently associated with decreased HRQoL across different relevant measures. Interestingly, in the adjusted analysis, apart from exercise intensity, no significant associations were found between demographic variables and the HRQoL measures SF-36-PCS, SF-36-MCS, 15D and SF-6D.
Our patients with ax-SpA reported lower HRQoL (SF-36 scores) compared with norm-based SF-36 reference scores in Norway [35], with the effect size ranging from −0.20 (mental health) to −0.98 (general health). The effect sizes indicate a substantial burden on HRQoL in the patient group, especially within the physical SF-36 domains. Our patients’ SF-36 scores were similar to the scores of Alkan et al. (2013) [15] who assessed HRQoL in Turkish patients with ax-SpA, highlighting the burden of this disease for such patients.
Minor statistically significant differences between female and male patients were only found for some demographic factors (BMI and alcohol consumption), some disease-related variables (swollen joints, entheses score, physical function and skeletal damage score) and some HRQoL domains (SF-36 bodily pain and physical role limitations; Tables 1 and 2). This suggests that the overall burden and the perception of ax-SpA are similar rather than different between genders. In previous studies, women with ax-SpA reported lower HRQoL values than men [13, 14], as well as more pain and more physical consequences of pain [13, 14]. Our data are consistent with those reports as our female patients with ax-SpA reported more bodily pain and reported reduced physical role limitations on the HRQoL measure SF-36.
In patients with ax-SpA, pharmacological anti-inflammatory treatment with NSAIDs and anti-tumour necrosis factor (TNF)-α treatment have been shown to improve physical function and quality of life [38, 39]. The percentage of ax-SpA patients in our study on NSAIDS was 44%, and users of biological DMARDs comprised 23%. This may explain the rather low level of disease activity seen in several measures reflecting this (e.g., BASDAI scores) in our study.
Exercise intensity was identified as being significantly associated with HRQoL across the different measures. Along with targeted treatment, exercise and rehabilitation therapy are cornerstones in the management of ax-SpA, including patients with AS [38,39,40,41]. Systematic workouts such as water exercises and exercises for increasing flexibility, muscle strength and cardio-respiratory fitness in ordinary clinical care have been shown to be beneficial [17, 40]. Good physical function implies coping in terms of daily activities and living, which further implies that the patients with ax-SpA can live nearly ordinary lives despite their chronic illness. Exercise is an important part of the holistic approach in treatment and care of this patient type [17, 40].
Co-morbidity was only associated with the 15D measure and not with the other HRQoL measures. Because the items included in this questionnaire are more concrete than those included in the other questionnaires, they may capture the disease-related limitations caused by ax-SpA more specifically [20,21,22,23]. Furthermore, the items addressed in the 15D questionnaires might be considered easier to respond to [20, 22], which is also our clinical experience [28]. Another explanation for the lack of association between co-morbidity and HRQoL might be the low number of co-morbidities in our patients, which seemed to be lower than in previous studies [24].
Back pain is a characteristic symptom in patients with ax-SpA [3]. Pain was only measured by the SF-36 as bodily pain along with physical function measures that might be affected. When we compared the SF-36 bodily pain score with norm-based scores, the effect size revealed a substantial difference between the two groups [35]. These comparisons underline the pain problem in patients with ax-SpA, although it is not site specific. Other HRQoL studies in patients with ax-SpA have also included a visual analogue scale (VAS) [15, 42], and a more specific pain measure might have revealed more nuanced and other findings. On the other hand, the consequence of pain in terms of reduced functioning was extensively covered by the other patient-reported measures in our study.
To our knowledge, this is the first study measuring HRQoL using the utility measures 15D and SF-6D in patients with ax-SpA. Interestingly, in the multivariate models shown in Table 3, the two utility measures—easier to use than the more comprehensive SF-36—performed as well as the SF-36-PCS expressed as the variance (R2 ) and compared better with the SF-36-MCS outcome. This might be interpreted as a test of concurrent validity for the two utility measures [43]. Furthermore, the relatively high variances in HRQoL (except for SF-36-MCS) explained by the demographic- and disease-related variables included in the multiple/adjusted comparisons might also indicate that the independent variables chosen for the analyses (those that are mostly collected in ordinary clinical care) were suitable [37, 43]. On the other hand, there is a question as to whether there were too many independent/explanation variables in the multiple analyses or whether there were overlaps between the questions included in the measures in the independent and dependent variables in the multiple regression model, such as the HAQ and SF-36-PCS measures [22, 23, 44]. The high validity of the utility measures, compared with SF-36 as the gold standard for the assessment of HRQoL, could be of importance, as only feasible HRQoL measures might have the potential to be used as part of the clinical standard in routine clinical care.
The disease-related independent variables that remained as significant associations with HRQoL in the adjusted analyses were all self-reported health or symptom measures. In their conceptual model, Wilson and Cleary linked clinical variables with HRQoL [45]. Their model shows how measures can be thought of as existing on a continuum of increasing biological (e.g., objective ax-SpA disease measures), social and psychological complexity. In this model, HRQoL is influenced by self-reported symptoms of functional status, along with characteristics of the individual and the environment, and not biological and other objective health and disease measures [45]. This seems to have been the case in our study as well.
Methodological considerations
The strengths of this study were that all the participants were recruited consecutively from two geographically restricted areas and the numbers were sufficient for robust analyses. Further, apart from age, there were few exclusion criteria and there were no differences between the patients included in the study and those who did not want to participate. At the time the data were collected, patients at MHH used significantly more biological DMARDS than did those at SSHF, which might explain some of the differences in self-reported health status. However, in the adjusted analyses, the centres did not turn out to be significantly associated with dependent variables. Therefore, pooling of the patients from the two areas was justified, as there were only small differences between them. Another strength of our study is that we used several validated patient-reported questionnaires and outcomes to cover the patients’ perspectives [20,21,22, 27].
A major limitation of our study was the cross-sectional study design, which does not permit any causal interpretations. In this regard, our results should be interpreted with caution as we only found associations between dependent and independent variables. Interestingly, when the adjusted models were run backwards, the results remained the same, indicating that our findings are likely robust.
Conclusions
In patients with ax-SpA, low physical activity (exercising <1 h per week), impaired physical function (higher HAQ scores) and impaired general ax-SpA disease well-being outcomes (higher BAS-G scores) were independently and consistently associated with decreased HRQoL across several measures. This indicates that the two utility measures (15D and SF-6D) reflect and capture HRQoL in patients with ax-SpA to the same extent as the SF-36. Our study has confirmed that ax-SpA negatively influences HRQoL and suggests that physical exercise is important as a specific treatment strategy to maintain and improve HRQoL in patients with ax-SpA.
Abbreviations
- AS:
-
Ankylosing spondylitis
- ax-SpA:
-
axial spondyloarthritis
- BASDAI:
-
Bath Ankylosing Spondylitis Activity Index
- BASFI:
-
Bath Ankylosing Spondylitis Functional Index
- BAS-G:
-
Bath Ankylosing Spondylitis Patient Global Score
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- DMARDs:
-
Disease-modifying anti-rheumatic drugs
- GLM:
-
General linear model
- HAQ:
-
Health Assessment Questionnaire
- HRQoL:
-
Health-related quality of life
- MASES:
-
Maastricht Ankylosing Spondylitis Enthesitis Score
- MCS:
-
Mental component summary
- MHH:
-
Martina Hansens Hospital
- NSAIDs:
-
Non-steroidal anti-inflammatory drugs
- PCS:
-
Physical component summary
- QALYs:
-
Quality-adjusted life years
- REK:
-
Norwegian Regional Committee for Medical Research Ethics
- SSHF:
-
Sørlandet Hospital
References
Bal S, Bal K, Turan Y, Deniz G, Gürgan A, Berkit I, Şendur Ö. Sexual functions in ankylosing spondylitis. Rheumatol Int. 2011;31(7):889–94.
Webers C, Essers I, Ramiro S, Stolwijk C, Landewe R, van der Heijde D, van den Bosch F, Dougados M, van Tubergen A. Gender-attributable differences in outcome of ankylosing spondylitis: long-term results from the outcome in Ankylosing Spondylitis international study. Rheumatology (Oxford). 2016;55(3):419–28.
Dagfinrud H, Mengshoel AM, Hagen KB, Loge JH, Kvien TK. Health status of patients with ankylosing spondylitis: a comparison with the general population. AnnRheumDis. 2004;63(12):1605–10.
Healey EL, Haywood KL, Jordan KP, Garratt AM, Ryan S, Packham JC. Ankylosing spondylitis and its impact on sexual relationships. Rheumatology (Oxford, England). 2009;48(11):1378–81.
Østensen M. New insights into sexual functioning and fertility in rheumatic diseases. Best Practice Research Clinical Rheumatology. 2004;18(2):219–32.
Kotsis K, Voulgari PV, Drosos AA, Carvalho AF, Hyphantis T. Health-related quality of life in patients with ankylosing spondylitis: a comprehensive review. Expert Rev Pharmacoecon Outcomes Res. 2014;14(6):857–72.
Yang X, Fan D, Xia Q, Wang M, Zhang X, Li X, Cai G, Wang L, Xin L, Xu S, et al. The health-related quality of life of ankylosing spondylitis patients assessed by SF-36: a systematic review and meta-analysis. Qual Life Res. 2016;25(11):2711–23.
Spilker B: Quality of life and pharmacoeconomics in clinical trials. 1996.
Kiltz U, Baraliakos X, Karakostas P, Igelmann M, Kalthoff L, Klink C, Krause D, Schmitz-Bortz E, Florecke M, Bollow M, et al. Do patients with non-radiographic axial spondylarthritis differ from patients with ankylosing spondylitis? Arthritis Care Res (Hoboken). 2012;64(9):1415–22.
Perez Alamino R, Maldonado Cocco JA, Citera G, Arturi P, Vazquez-Mellado J, Sampaio-Barros PD, Flores D, Burgos-Vargas R, Santos H, Chavez-Corrales JE, et al. Differential features between primary ankylosing spondylitis and spondylitis associated with psoriasis and inflammatory bowel disease. J Rheumatol. 2011;38(8):1656–60.
Kreis S, Molto A, Bailly F, Dadoun S, Fabre S, Rein C, Hudry C, Zenasni F, Rozenberg S, Pertuiset E, et al. Relationship between optimism and quality of life in patients with two chronic rheumatic diseases: axial spondyloarthritis and chronic low back pain: a cross sectional study of 288 patients. Health Qual Life Outcomes. 2015;13:78.
Salaffi F, Carotti M, Gasparini S, Intorcia M, Grassi W. The health-related quality of life in rheumatoid arthritis, ankylosing spondylitis, and psoriatic arthritis: a comparison with a selected sample of healthy people. Health Qual Life Outcomes. 2009;7:25.
Tournadre A, Pereira B, Lhoste A, Dubost JJ, Ristori JM, Claudepierre P, Dougados M, Soubrier M. Differences between women and men with recent-onset axial spondyloarthritis: results from a prospective multicenter French cohort. Arthritis Care Res (Hoboken). 2013;65(9):1482–9.
de Carvalho HM, Bortoluzzo AB, Goncalves CR, da Silva JA, Ximenes AC, Bertolo MB, Ribeiro SL, Keiserman M, Menin R, Skare TL, et al. Gender characterization in a large series of Brazilian patients with spondyloarthritis. Clin Rheumatol. 2012;31(4):687–95.
Alkan BM, Fidan F, Erten S, Aksekili H, Alemdar A, Eroglu E, Ardicoglu O, Tosun A. Fatigue and correlation with disease-specific variables, spinal mobility measures, and health-related quality of life in ankylosing spondylitis. Mod Rheumatol. 2013;23(6):1101–7.
O'Dwyer T, O'Shea F, Wilson F. Decreased health-related physical fitness in adults with ankylosing spondylitis: a cross-sectional controlled study. Physiotherapy. 2016;102(2):202-9.
O'Dwyer T, O'Shea F, Wilson F. Decreased physical activity and cardiorespiratory fitness in adults with ankylosing spondylitis: a cross-sectional controlled study. Rheumatol Int. 2015;35(11):1863–72.
Demontis A, Trainito S, Del Felice A, Masiero S. Favorable effect of rehabilitation on balance in ankylosing spondylitis: a quasi-randomized controlled clinical trial. Rheumatol Int. 2016;36(3):333-9.
Shen B, Zhang A, Liu J, Da Z, Xu X, Liu H, Li L, Gu Z. Body image disturbance and quality of life in Chinese patients with ankylosing spondylitis. Psychol Psychother. 2014;87(3):324–37.
Sintonen H. The 15D instrument of health-related quality of life: properties and applications. Ann Med. 2001;33(5):328–36.
Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21(2):271–92.
Ware JE Jr, Snow KK, Kosinski MA, Gandek MS. SF-36 Health Survey Manual & Interpretation Guide. Boston Massachusetts: New England Medical Centre, The Health Institute; 1993.
Ware JE Jr, Kosinski MA, Keller SD. SF-36 physical and mental health summery scale: a User’s manual. Boston: Massachusetts: New England Medical Centre, The Health Institute; 1994.
Akkoc N, Direskeneli H, Erdem H, Gul A, Kabasakal Y, Kiraz S, Balkan Tezer D, Hacibedel B, Hamuryudan V. Direct and indirect costs associated with ankylosing spondylitis and related disease activity scores in Turkey. Rheumatol Int. 2015;35(9):1473–8.
Berg KH, Rohde G, Proven A, Almas E, Benestad E, Ostensen M, Haugeberg G. Exploring the relationship between demographic and disease-related variables and perceived effect of health status on sexual activity in patients with axial spondyloarthritis: associations found only with non-disease variables. Scand J Rheumatol. 2017;15:1–7.
Rudwaleit M, van der Heijde D, Landewe R, Listing J, Akkoc N, Brandt J, Braun J, Chou CT, Collantes-Estevez E, Dougados M, et al. The development of assessment of SpondyloArthritis international society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis. 2009;68(6):777–83.
Pincus T, Summey JA, Soraci SA Jr, Wallston KA, Hummon NP. Assessment of patient satisfaction in activities of daily living using a modified Stanford health assessment questionnaire. Arthritis Rheum. 1983;26(11):1346–53.
Rohde G, Moum T, Haugeberg G. Comparing 15D and SF-6D performance in fragility wrist and hip fracture patients in a two-year follow-up case-control study. Value Health. 2012;15(8):1100–7.
Rohde G, Haugeberg G, Mengshoel AM, Moum T, Wahl AK. Two-year changes in quality of life in elderly patients with low-energy hip fractures. A case-control study. BMC Musculoskelet Disord. 2010;11:226.
Rohde G, Berg KH, Prøven A, Haugeberg G. Exploring the relationship between demographic and disease related variables and health-related quality of life in patients with axial Spondyloarthritis. Qual Life Res. 2015;24(10):1074. (Suplement 1 Abstract presented at 22nd Annual Conference od the International Society for Quality if Life Research).
Kvien TK, Kaasa S, Smedstad LM. Performance of the Norwegian SF-36 health survey in patients with rheumatoid arthritis. II. A comparison of the SF-36 with disease-specific measures. J Clin Epidemiol. 1998;51(11):1077–86.
Loge JH, Kaasa S, Hjermstad MJ, Kvien TK. Translation and performance of the Norwegian SF-36 health survey in patients with rheumatoid arthritis. I. Data quality, scaling assumptions, reliability, and construct validity. J Clin Epidemiol. 1998;51(11):1069–76.
Stavem K. Reliability, validity and responsiveness of two multiattribute utility measures in patients with chronic obstructive pulmonary disease. Qua lLife Res. 1999;8(1–2):45–54.
Stavem K, Froland SS, Hellum KB. Comparison of preference-based utilities of the 15D, EQ-5D and SF-6D in patients with HIV/AIDS. Qual Life Res. 2005;14(4):971–80.
Hougen HC. Survey of living Conditionc 2002, cross - sectional survey (Samordnet levek†rsunders›kelse 2002 - tverrsnittsunders›kelsen): dokumentasjonsrapport, vol. 2004/22. Oslo: Statistics Norway (Statistisk sentralbyr†, Avdeling for personstatistikk/Seksjon for intervjuunders›kelse); 2004.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, N. J: Laurence Erlbaum; 1988.
Altman DG. Practical statistics for medical research. London. New York: Chapman and Hall; 2006.
Zochling J, Sieper J, van der Heijde D, Braun J. Development of a core set of domains for data collection in cohorts of patients with ankylosing spondylitis receiving anti-tumor necrosis factor-alpha therapy. J Rheumatol. 2008;35(6):1079–82.
Zochling J, van der Heijde D, Dougados M, Braun J. Current evidence for the management of ankylosing spondylitis: a systematic literature review for the ASAS/EULAR management recommendations in ankylosing spondylitis. Ann Rheum Dis. 2006;65(4):423–32.
Eppeland SG, Diamantopoulos AP, Soldal DM, Haugeberg G. Short term in-patient rehabilitation in axial spondyloarthritis - the results of a 2-week program performed in daily clinical practice. BMC Research Notes. 2013;6:185.
Braun J, van den Berg R, Baraliakos X, Boehm H, Burgos-Vargas R, Collantes-Estevez E, Dagfinrud H, Dijkmans B, Dougados M, Emery P, et al. 2010 update of the ASAS/EULAR recommendations for the management of ankylosing spondylitis. Ann Rheum Dis. 2011;70(6):896–904.
Hyphantis T, Kotsis K, Tsifetaki N, Creed F, Drosos A, Carvalho A, Voulgari P. The relationship between depressive symptoms, illness perceptions and quality of life in ankylosing spondylitis in comparison to rheumatoid arthritis. J Int Leag Assoc Rheumatol. 2013;32(5):635–44.
Fayers PM, Machin D. Quality of life: the assessment, analysis and interpretation of patient-reported outcomes. Chichester: John Wiley; 2007.
Pincus T, Callahan LF, Brooks RH, Fuchs HA, Olsen NJ, Kaye JJ. Self-report questionnaire scores in rheumatoid arthritis compared with traditional physical, radiographic, and laboratory measures. Ann Intern Med. 1989;110(4):259–66.
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;273(1):59–65.
Acknowledgements
We appreciate the expert technical assistance and help with data collection provided by the nurses at SSHF and MHH. We also thank statistician Are Hugo Pripp at the Unit for Biostatistics and Epidemiology, Oslo University Hospital for help with the statistics.
Funding
The study was funded by a research grant from Health Southern Norway Regional Trust and partly by Sorlandet Hospital and Martina Hansens Hospital.
Availability of data and materials
The data are stored on secure research computer servers at Sorlandet Hospital, in accordance with Norwegian regulations for research. The data are available on request from authorized individuals.
Author information
Authors and Affiliations
Contributions
GR initiated this paper as part of a larger study of patients with ax-SpA, analysed the data and wrote the manuscript. GH was the principal investigator for the study. AP was responsible for data collection at MHH. All co-authors contributed to the content of the paper and critiqued revisions. GR, KHB, AP and GH approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study was approved by the Regional Committee for Medical Research Ethics (REK # 4.2007.2152). All the participants gave written consent to participate in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Rohde, G., Berg, K.H., Prøven, A. et al. The relationship between demographic- and disease-related variables and health-related quality of life in patients with axial spondyloarthritis. BMC Musculoskelet Disord 18, 328 (2017). https://doi.org/10.1186/s12891-017-1693-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-017-1693-z