Abstract
Background
Tibiotalocalcaneal arthrodesis (TTCA) using intramedullary nails is a salvage procedure for many diseases in the ankle and subtalar joint. Despite “newly described intramedullary nails” with specific anatomical shapes there still remain major complications regarding this procedure. The following study presents a modified biomechanical test setup for investigations of the hindfoot.
Methods
Nine fresh-frozen specimens from below the human knee were anaysed using the Hindfoot Arthrodesis Nail (Synthes) instrument. Quasi-static biomechanical testing was performed for internal/external rotation, varus/valgus and dorsal/plantar flexion using a modified established setup (physiological load entrance point, sledge at lever arm to apply pure moments). Additionally, a 3D optical measurement system was added to allow determination of interbony movements.
Results
The mean torsional range of motion (ROM) calculated from the actuator data of a material testing machine was 10.12° (SD 0.6) compared to 10° (SD 2.83) as measured with the Optotrak® system (between tibia and calcaneus). The Optotrak showed 40 % more rotation in the talocrural joint.
Mean varus/valgus ROM from the material testing flexion machine was seen to be 5.65° (SD 1.84) in comparison to 2.82° (SD 0.46) measured with the Optotrak. The subtalar joint showed a 70 % higher movement when compared to the talocrural joint.
Mean ROM in the flexion test was 5.3° (SD 1.45) for the material testing machine and 2.1° (SD 0.39) for the Optotrak. The movement in the talocrural joint was 3 times higher compared to the subtalar joint.
Conclusion
The modified test setup presented here for the hindfoot allows a physiological biomechanical loading. Moreover, a detailed characterisation of the bone-implant constructs is possible.
Similar content being viewed by others
Background
Tibiotalocalcaneal arthrodesis (TTCA) using an intramedullary nail is a salvage procedure for many diseases involving the talocrural and subtalar joint. Since the first report of arthrodesis with retrograde femoral nails, new generations of intramedullary nails have been designed in regard to the specific anatomy of the ankle.
Modifications, especially those regarding the development of a lateral bend in the distal part of the intramedullary nail, led to more stability and therefore less non-union rates because of the nail’s course, going through the calcaneus instead of the sustentaculum tali. In addition, with the reconstruction of the physiological hindfoot valgus, the simulation of a more conventional gait pattern was possible [1, 2]. In their biomechanical study, Mann et al. showed the importance of the course of the calcaneal screw from posterior to anterior [3]. These results could be confirmed by Means et al. [4]. But still there are major complications; especially the non-union of the upper ankle joint and/or subtalar joint are major problems, which follow this procedure (Fig. 1) [5–8].
a Non-union of the subtalar joint after tibiotalocalcaneal arthrodesis by intramedullary nail with successful arthrodesis of the ankle joint. (68 year old male patient, 18 months after arthrodesis due to osteoarthritis and infection after pilon-fracture b) Complete failure with nail loosening and non-union of the ankle joint and the subtalar joint. (58 old male patient, 18 months after tibiotalocalcaneal arthrodesis due to varus osteoarthritis of the ankle and pes cavovarus correction)
It is common sense, that instability, especially torsional and shear stress, has negative impact on bone healing. In case of the hindfoot arthrodesis three bones and two joints are involved, which can cause instability und thus promote a non-union. Therefore, comparing overall construct stability is insufficient, attentions has to be directed to the stability of the talocrural and subtalar joint separately.
Actual biomechanical setups are able to compare the complete bone-implant- constructs only, without offering any differentiation of talocrural and subtalar joint movement. An established biomechanical method [9–11] was therefore modified and enhanced to address this disadvantage. Furthermore, the load entry point on the construct was adapted to mimic more physiological conditions. Additionally, a 3D motion tracking system was added to evaluate movements between all joint sections (tibia, talus, calcaneus) individually.
Methods
Specimens
Nine fresh-frozen human specimens from below the knee taken from our Institute of Anatomy were used for this study (five female, four male donors). Median age of the donors was 85.3 years (range: 77–95 years), four right and five left tibiae were available. The specimens were stored at -18C and thawed at room temperature for 24 h before testing.
For screening of pre-existing bony pathologies and implant size estimation, conventional radiographs in two planes (antero-posterior and lateral) were obtained. Additional bone mineral density of the cancellous bone in the calcaneus was measured by quantitative computed tomography (Somatom Definition, Siemens, Erlangen, Germany).
The specimens were prepared by removing all soft-tissue except for the stabilizing ligaments at the ankle such as the distal syndesmotic complex, the interosseous membrane, collateral ligaments and the capsule of the ankle and subtalar joints. The joint surfaces of the ankle and subtalar joints were left intact following former biomechanical studies [9, 12]. The forefoot was amputated at the Chopart’s joint. In contrast to the study of Klos et al. the fibula was not resected, in order to prevent additional instability [9]. Tibia and fibula were transected 30 cm above the ankle joint.
Implant
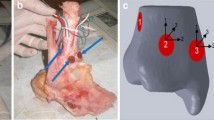
For this study we used the Hindfoot Arthrodesis Nail (HAN, Depuy Synthes, West Chester, PA, USA) made of titanium alloy (Ti6Al7Nb). The HAN-nail shows a valgus bend of 12° distally. Nail locking was performed using two screws in the calcaneus, one screw in the talus and two screws in the tibia (Fig. 2). The nail used in this study had a length of 240 mm and a diameter of 10 mm (following x-ray measurement).
Implantation
An experienced orthopaedic surgeon, following the manufacturers’ guidelines and using the adequate tools under c-arm control, performed implantation.
In contrast to the intraoperative procedure, the joint cartilage was not removed to ensure a standardized procedure.
Biomechanical testing
The test setup used in this study was based on the publications of Mückley et al. and Klos et al. [9, 10]. They used an upside down positioning of the specimen with force application via a 80 mm lever arm using a connecting rod for varus/valgus and flexion testing, for torsional testing force was applied directly to the embedding [9].
For mechanical testing a material testing machine (Instron 8874, Instron, High Wycombe, Bucks, United Kingdom) was used. We modified the test setup in two main aspects:
First, we included a ball-bearing rail guide (sledge) with negligible friction to the new lever arm instead of the connecting rod described by Mückley et al. and Klos et al. [11, 12]. The sledge was connected to the testing machine actuator with a type of cardanic suspension, which allowed small rotational movements in all directions. This refined suspension ensured a constant length of the lever arm of 80 mm in every position during varus/valgus and dorsi-/plantarflexion. In these motion planes, the sledge minimized shear stress on the specimen and allowed a more anatomical and especially standardized loading condition (Fig. 3a). The length of the lever arm was chosen following the work of Klos et al. [9, 12]. Embedding the tuber calcanei on a marked position (at the base plate) and using a cross-laser for the alignment of the specimens on the machine table ensured standardization of the lever arm length to 80 mm. Secondly, the load entry point was moved to the tuber of the calcaneus (from the anterior processes of the calcaneus as described by Mückley et al. and Klos et al.) [9, 11, 12] to simulate a physiologic loading of the construct, according to a normal heel strike during the gait pattern (Fig. 3b) [13–15]. A physiologic load entry point is from special interest for torsional loading and the comparison of intramedullary implants. Due to the varying nail entry point torsional stability depends on the relation of nail and load entry point. An especially unstable situation can be imagined, when nail and load entry point are identical.
a Modification of the load application by adding a ball-bearing rail guide (sledge) at the suspension to exclude shear stress and to apply loads with a constant lever arm; b Shift of the load entry point to the tuber of the calcaneus to simulate physiological conditions. In contrast Klos et al. [7, 8] applied the load in extension of the tibia shaft axis
Before embedding, all screw holes and the subtalar joint were covered using modelling clay to prevent any influence on the biomechanical properties, especially artificial fusion of the subtalar joint due to misplaced bone cement and infiltration of the cement into the medullary canal. First the calcaneus was embedded using Technovit (Technovit 3040 Heraeus Kulzer GmbH, Wernheim, Germany) and a special casing to allow a radiological view on the calcaneus. Afterwards, the tibia and fibula were embedded, verifying the adjustment and positioning by a cross-line laser. To exclude shear stress, the proximal embedding was performed on the testing machine.
Finally, a 3D optical motion measurement system was attached to the specimens (Fig. 4; Optotrak Certus, NDI Europe GmbH, Radolfzell, Germany). Four active marker triplets were used: one at the tibial shaft, one at the talus, one at the embedding of the calcaneus and one at the machine table (global reference coordinate system). The NDI software (First Principles Version 2, NDI Europe GmbH, Radolfzell, Germany) allowed calculation of all relative movements within the standardized coordinate systems. Data were recorded using a frequency of 25 Hz. The accuracy of the NDI measurement of translational motions was within ±0.03 mm and had a resolution of 0.01 mm; rotational accuracy was 0.0757 ± 0.121° [16].
Test setup for dorsi-/plantarflexion (left) with markers on machine table, tibia, talus and calcaneus embedding. First Principles display (right) showing x-axis in red, y-axis in green and z-axis in blue. a global coordinate system and coordinate system of the Instron machine table; b tibia; c talus; d calcaneus. The black dots represent reference points to create the coordinate systems
All biomechanical tests were performed in load-control mode, machine data (time, cycle, angle, moment, axial displacement, force) were recorded at a rate of 64 Hz. The forces and resulting moments were selected due to former publications [9–11, 17]. Biomechanical testing was performed according to the following protocol:
-
quasi-static tests (20 cycles) in
-
o dorsi-/plantarflexion (±62.5 N equal to ±5 Nm) at 0.5 Hz
-
o varus/valgus (±62.5 N equal to ±5 Nm) at 0.5 Hz
-
o torsion in external-/internal rotation (±5 Nm) at 1°/sec
Analysis
After 10 cycles of loading (to exclude setting behaviour) 10 cycles of mechanical loading have been applied to the specimens. For these 10 cycles the range of motion and neutral zone has been determined for every specimen, for further evaluation a mean value has been calculated for every specimen.
The general setup motion can be easily described in terms of range of motion (ROM) and neutral zone (NZ) [18–21]. The neutral zone is defined as that region where motion is possible without any loading. Both parameters were determined for all quasi-static tests from the machine data plotting every singe cycle in Excel (Microsoft Corporation, Version 14, Redmond WA, USA) and measuring manually (Fig. 5). From the optical measurement system, the ROM was differentiated, and rotational motion was calculated between tibia and calcaneus (TIB-CAL), tibia and talus (TIB-TAL), talus and calcaneus (TAL-CAL). These results have mathematically the relation TIB-CAL = TIB-TAL + TAL-CAL. The results from the optical measurement system mathematically could not be transferred to the machine data, especially not for varus/valgus and flexion, due to the lever arm the extent of machine actuator movement is much higher then the movement in the bone-implant-construct.
Rotation about the x-axis represents varus/valgus movements, rotation about the y-axis dorsi-/plantarflexion, and rotation about the z-axis internal-/external rotation.
For statistical analysis ROM values from the Instron were compared to the Optotrak results (TIB-CAL) using the Wilcoxon signed-rank test for depended samples was used. The same procedure was used for statistical comparison within the Optotrak results.
Results
Torsion
The mean range of motion calculated from the material testing machine data for internal and external rotation was 10.12° (SD 0.6). In comparison, the torsional range of motion as measured with the Optotrak system between tibia and calcaneus was 10° (SD 2.83). This difference was statistically not significant (p = 0.463). With the use of Optotrak, we were also able to determine the movements between tibia-talus and talus-calcaneus and found a 40 % significant higher rotation in the talocrural joint (p = 0.028; Table 1). In contrast, the machine data allowed us to calculate a neutral zone of 1.85° (Fig. 6).
Varus/valgus
The mean range of motion from the machine data observed here was 5.65° (SD 1.84) compared to 2.82° (SD 0.46) as measured using the Optotrak. This difference was statistically significant with p = 0.028. The subtalar joint showed a 70 % significant higher movement compared to the talocrural joint for varus/valgus bending (p = 0.028, Fig. 7).
Range of motion in degrees for varus/valgus and flexion from machine data (green) and Optotrak (blue). TIB-CAL is the range of motion of the whole construct – measured between tibia and calcaneus. TIB-TAL is the movement in the upper ankle joint (tibia – talus) and TAL-CAL in the subtalar joint (talus – calcaneus)
Dorsal/plantar flexion
The mean range of motion for the flexion test was 5.3° (SD 1.45) seen from the material testing machine and 2.1° (SD 0.39) as seen from the Optotrak. This difference was statistically significant with p = 0.046. We found approximately a 3-times significant higher movement in the talocrural joint compared to the subtalar joint (p = 0.028, Fig. 7).
For varus/valgus and flexion data, the material testing machine data enabled determination of values in the neutral zone (Fig.6).
Discussion
TTCA using intramedullary nails is an established salvage procedure. Unfortunately, it happens quite often that non-union complications of the upper ankle joint and/or the subtalar joint occur.
Therefore, biomechanical testing and the development of new fixation methods and designs are of significant interest also for TTCA. Starting with femoral nails for TTCA, new generations of intramedullary nails have been developed again and again.
Biomechanical testing of the new developed implants was conducted in several test setups ranging from static to cyclic loading, but all of them mainly using machine data for mechanical characterization [3, 4, 22–25]. Fragomen et al. investigated the Ilizarov external fixator and an intramedullary nail regarding micro motions. Therefore they used a passive marker optical measurement system above and under the osteotomy gap, but only a two dimensional evaluation was possible [26].
With our modifications of the test setup developed by Mückley et al., we were able to exclude shear stress on the construct and ensure a constant lever arm and consequently a standardized application of constant moments/forces to the construct [10, 11]. The additional use of the 3D motion measurement system allows the detection of movements between the involved bones with high precision. Utilizing a combination of material testing machine data and the Optotrak system, it is possible to characterize the ROM from both, the neutral zone (taken from the machine data) and the interbony movements (taken from the Optotrak system). This is possible by matching the load data of the machine with the motion data of the Optotrak.
For the HAN we found the talocrural joint prone to torsional stress as well as dorsiflexion and plantarflexion, whereas the subtalar joint is more prone to varus/valgus stress. Comparing the range of motion results from the machine and the optical system, we found no significant differences for torsional loading. In contrast, we found statistically significant differences for varus/valgus and dorsal/plantar flexion. These differences result from the test setup with using a lever arm for these loading scenarios. Therefore, the values from the machine are significant higher compared with the values from the optical measurement system looking at pure bony movements. The results of the neutral zone are only determined from the machine data and therefore, include the instability of implant and of the fixture.
Further important features of today’s intramedullary hindfoot nails are locking and compression mechanisms. Biomechanical studies have demonstrated that a higher stability can be attained when a combination with these fixation methods is employed [10, 11].
Using the presented setup biomechanical investigations of the hindfoot can be performed very sophisticated. The optical measurement system allows the differentiation of the involved joints (tibio-talar and talo-calcanear) combined with the machine data, that allow gathering information of the neutral zone and the whole construct. Overall, the setup allows detecting weak points of implants or effects of operative procedures. The test setup is not limited to hindfoot arthrodesis and intramedullary nails. With slight modifications implants/operations concerning the ankle joint or the subtalar joint and the effect to the other joint can be investigated.
Using the results strategies/developments can be performed to optimize implants or procedures to improve the management of hindfoot pathologies. Moreover, modifications to the implants themselves may allow a further reduction of the complication rates by increasing the stability of the TTCA construct.
This study also has limitations: using biomechanical testing without any soft tissue/muscle/tendon simulation is a basic method to compare mechanical characteristics of bone implant interfaces and limited cofounders. Additionally, the cartilage in talocrural and the subtalar joint has not been removed. This allowed us a very standardized approach resulting in a relative unstable situation. Another limitation is the independence of the optical and machine data, this does us not allow to calculate neutral zone values from the optical dataset.
Conclusion
The modified test setup for the hindfoot presented here promotes a more physiological and biomechanical loading. This offers – together with the 3D optical measuring system – a more standardized testing, above all for difficult cases, and also allows a detailed characterisation of the bone-implant constructs. Utilizing this, new implants and surgical techniques at the hindfoot can be compared with the current state of affairs; implant developments can be followed and, where necessary, their complications reduced.
Abbreviations
HAN, hindfoot arthrodesis nail; NZ, neutral zone; ROM, range of motion; SD, standard deviation; TTCA, tibiotalocalcaneal arthrodesis
References
Grass R, Rammelt S, Heineck J, Zwipp H. Hindfoot arthrodesis resulting from retrograde medullary pinning. Orthopade. 2005;34(12):1238–44. doi:10.1007/s00132-005-0865-y.
Thomas RL, Sathe V, Habib SI. The use of intramedullary nails in tibiotalocalcaneal arthrodesis. J Am Acad Orthop Surg. 2012;20(1):1–7. doi:10.5435/JAAOS-20-01-001.
Mann MR, Parks BG, Pak SS, Miller SD. Tibiotalocalcaneal arthrodesis: a biomechanical analysis of the rotational stability of the Biomet Ankle Arthrodesis Nail. Foot Ankle Int. 2001;22(9):731–3.
Means KR, Parks BG, Nguyen A, Schon LC. Intramedullary nail fixation with posterior-to-anterior compared to transverse distal screw placement for tibiotalocalcaneal arthrodesis: a biomechanical investigation. Foot Ankle Int. 2006;27(12):1137–42.
Budnar VM, Hepple S, Harries WG, Livingstone JA, Winson I. Tibiotalocalcaneal arthrodesis with a curved, interlocking, intramedullary nail. Foot Ankle Int. 2010;31(12):1085–92. doi:10.3113/FAI.2010.1085.
Devries JG, Philbin TM, Hyer CF. Retrograde intramedullary nail arthrodesis for avascular necrosis of the talus. Foot Ankle Int. 2010;31(11):965–72. doi:10.3113/FAI.2010.0965.
Haaker R, Kohja EY, Wojciechowski M, Gruber G. Tibio-talo-calcaneal arthrodesis by a retrograde intramedullary nail. Ortop Traumatol Rehabil. 2010;12(3):245–9.
Rammelt S, Pyrc J, Agren PH, Hartsock LA, Cronier P, Friscia DA, et al. Tibiotalocalcaneal fusion using the hindfoot arthrodesis nail: a multicenter study. Foot Ankle Int. 2013;34(9):1245–55. doi:10.1177/1071100713487526.
Klos K, Wahnert D, Gueorguiev B, Schwieger K, Hofmann GO, Windolf M, et al. Development of a technique for cement augmentation of nailed tibiotalocalcaneal arthrodesis constructs. Clin Biomech. 2010;25(6):576–81. doi:10.1016/j.clinbiomech.2010.03.006.
Muckley T, Eichorn S, Hoffmeier K, von Oldenburg G, Speitling A, Hoffmann GO, et al. Biomechanical evaluation of primary stiffness of tibiotalocalcaneal fusion with intramedullary nails. Foot Ankle Int. 2007;28(2):224–31. doi:10.3113/FAI.2007.0224.
Muckley T, Hoffmeier K, Klos K, Petrovitch A, von Oldenburg G, Hofmann GO. Angle-stable and compressed angle-stable locking for tibiotalocalcaneal arthrodesis with retrograde intramedullary nails. Biomechanical evaluation. J Bone Joint Surg Am. 2008;90(3):620–7. doi:10.2106/JBJS.G.00010.
Klos K, Gueorguiev B, Schwieger K, Frober R, Brodt S, Hofmann GO, et al. Comparison of calcaneal fixation of a retrograde intramedullary nail with a fixed-angle spiral blade versus a fixed-angle screw. Foot Ankle Int. 2009;30(12):1212–8. doi:10.3113/FAI.2009.1212.
Haraguchi N, Armiger RS, Myerson MS, Campbell JT, Chao EY. Prediction of three-dimensional contact stress and ligament tension in the ankle during stance determined from computational modeling. Foot Ankle Int. 2009;30(2):177–85. doi:10.3113/FAI.2009.0177.
Jenkyn TR, Anas K, Nichol A. Foot segment kinematics during normal walking using a multisegment model of the foot and ankle complex. J Biomech Eng. 2009;131(3):034504. doi:10.1115/1.2907750.
Prachgosin T, Chong DY, Leelasamran W, Smithmaitrie P, Chatpun S. Medial longitudinal arch biomechanics evaluation during gait in subjects with flexible flatfoot. Acta Bioeng Biomech. 2015;17(4):121–30.
Schulze M, Hartensuer R, Gehweiler D, Holscher U, Raschke MJ, Vordemvenne T. Evaluation of a robot-assisted testing system for multisegmental spine specimens. J Biomech. 2012;45(8):1457–62. doi:10.1016/j.jbiomech.2012.02.013.
Santangelo JR, Glisson RR, Garras DN, Easley ME. Tibiotalocalcaneal arthrodesis: a biomechanical comparision of multiplanar external fixation with intramedullary fixation. Foot Ankle Int. 2008;29(9):936–41. doi:10.3113/FAI.2008.0936.
Attal R, Maestri V, Doshi HK, Onder U, Smekal V, Blauth M, et al. The influence of distal locking on the need for fibular plating in intramedullary nailing of distal metaphyseal tibiofibular fractures. Bone Joint J. 2014;96-B(3):385–9. doi:10.1302/0301-620X.96B3.32185.
Dailey HL, Daly CJ, Galbraith JG, Cronin M, Harty JA. The Flexible Axial Stimulation (FAST) intramedullary nail provides interfragmentary micromotion and enhanced torsional stability. Clin Biomech. 2013;28(5):579–85. doi:10.1016/j.clinbiomech.2013.04.006.
Wahnert D, Hoffmeier KL, von Oldenburg G, Frober R, Hofmann GO, Muckley T. Internal fixation of type-C distal femoral fractures in osteoporotic bone. J Bone Joint Surg Am. 2010;92(6):1442–52. doi:10.2106/JBJS.H.01722.
Wahnert D, Stolarczyk Y, Hoffmeier KL, Raschke MJ, Hofmann GO, Muckley T. Long-term stability of angle-stable versus conventional locked intramedullary nails in distal tibia fractures. BMC Musculoskelet Disord. 2013;14:66. doi:10.1186/1471-2474-14-66.
Alfahd U, Roth SE, Stephen D, Whyne CM. Biomechanical comparison of intramedullary nail and blade plate fixation for tibiotalocalcaneal arthrodesis. J Orthop Trauma. 2005;19(10):703–8.
Bennett GL, Cameron B, Njus G, Saunders M, Kay DB. Tibiotalocalcaneal arthrodesis: a biomechanical assessment of stability. Foot Ankle Int. 2005;26(7):530–6.
Berend ME, Glisson RR, Nunley JA. A biomechanical comparison of intramedullary nail and crossed lag screw fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int. 1997;18(10):639–43.
Chiodo CP, Acevedo JI, Sammarco VJ, Parks BG, Boucher HR, Myerson MS, et al. Intramedullary rod fixation compared with blade-plate-and-screw fixation for tibiotalocalcaneal arthrodesis: a biomechanical investigation. J Bone Joint Surg Am. 2003;85-A(12):2425–8.
Fragomen AT, Meyers KN, Davis N, Shu H, Wright T, Rozbruch SR. A biomechanical comparison of micromotion after ankle fusion using 2 fixation techniques: intramedullary arthrodesis nail or Ilizarov external fixator. Foot Ankle Int. 2008;29(3):334–41. doi:10.3113/FAI.2008.0334.
Acknowledgements
Funding
This study was supported by Small Bone Innovations Inc. (SBI, 1380 S. Pennsylvania Avenue, Morrisville, PA 19067). The Company delivered all of their implants, paid for the specimens used and for the implants of the competitor. Additionally, financial support for laboratory expenses was given.
Availability of data and materials
All the data supporting your findings is contained within the manuscript.
Authors’ contributions
We confirm that all authors read and approved the final version of the manuscript. JE substantially designed the study and carried out data interpretation and drafting the manuscript. MS was responsible for the test setup's design and conception, as well as data analysis. DG undertook data acquisition, data interpretation and manuscript revision. ML also surveyed data acquisition and evaluation. MJR overtook data interpretation and critical manuscript revision. DW was responsible for data evaluation, statistics and manuscript drafting. SO supported instrumentation, design of the study and drafting of the manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable, this is a biomechanical study.
Ethics approval and consent to participate
The local institute of anatomy provided the specimens used in this study. The local Ethical Committee (Ethikkommission der Ärztekammer Westfalen-Lippe und der Medizinischen Fakultät der Westfälischen Wilhelms-Universität) stated before, that biomechanical studies using specimens from body donors do not need an approval.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Evers, J., Schulze, M., Gehweiler, D. et al. A modified and enhanced test setup for biomechanical investigations of the hindfoot, for example in tibiotalocalcaneal arthrodesis. BMC Musculoskelet Disord 17, 318 (2016). https://doi.org/10.1186/s12891-016-1177-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-016-1177-6