Abstract
Asthma, influenced by genetic, environmental, and social factors is leading to poor outcomes and preventable mortality due to inadequate care and limited access to effective treatments. This study aimed to analyze self-reported asthma prevalence in Turkey, focusing on its determinants, such as individual factors, lifestyle, socioeconomic status, and healthcare access.
This study conducts a secondary analysis of the 2019 Turkiye Health Survey (THS), employing a nationally representative cross-sectional design by the Turkish Statistical Institute. The sampling utilized a stratified, two-stage cluster sampling method, with data from 16,976 adults (aged 15 years and older) analyzed for asthma determinants. The independent variables are categorized into four domains: individual factors, lifestyle assessment, socioeconomic factors, and access to the healthcare services.
The prevalence of asthma is 9.8%, varying significantly across demographics. Higher asthma rates are observed among older, divorced/widowed individuals, those with communication difficulties, and obese individuals. Cost-related unmet healthcare needs and appointment scheduling delays increase asthma risk. Logistic regression models identified age, marital status, obesity, education level, and healthcare access as significant predictors of asthma.
This study underscores the multifaceted determinants of asthma in Turkey, highlighting the necessity for targeted interventions addressing individual, lifestyle, socioeconomic, and healthcare access factors.
Similar content being viewed by others
Introduction
Asthma is a widespread chronic respiratory condition that significantly impacts global health, affecting a substantial portion of the population, ranging from 1% to 29% across various countries [1]. This disease imposes a considerable burden, leading to premature mortality and reduced quality of life. It contributes significantly to disability-adjusted life years (DALYs) reduction, accounting for approximately one-fifth of all losses related to chronic respiratory diseases and ranking 34th in global disease burden assessments [2].
In different regions of Turkey, adult asthma studies, mainly using the European Community Respiratory Health Survey (ECRHS), reported asthma prevalence ranging from 1.2% to 9.4% and asthma-like symptom prevalence between 9.8% and 27.3%. The multicenter PARFAIT study by the Thoracic Society revealed a nationwide asthma prevalance of 7.1% in males and 9.0% in females [3, 4].
Despite the lack of standardized definitions of asthma, diagnostic criteria (such as spirometry) that can be used in all countries, and the lack of consensus between surveillance programs and questionnaires that have led to imprecise estimates of the incidence, prevalence, and burden of the disease, there is strong evidence that the incidence of asthma has increased significantly over the past 50 years. Despite the global political commitment, progress in reducing the burden of asthma has been insufficient, particularly in low-income countries [5].
Asthma is a complex condition influenced by genetic, environmental, and social factors. Social determinants of health (SDHs) encompass various aspects, such as early childhood development, education, gender, working conditions, income, social status, environment, lifestyle, and access to healthcare [6]. Disruption in these areas leads to health disparities, especially in respiratory diseases, compared to others [7]. Studies highlight low socioeconomic status (SES) and poverty-related factors as strongly linked to asthma development and poor outcomes, such as lung function decline and exacerbations. Preventable asthma mortality and severe attacks often result from inadequate care and limited access to effective treatments due to a lack of government support and policies [5, 7, 8].
Understanding asthma's inequalities requires a multifaceted approach, considering a range of risk factors across different levels. The World Health Organization's conceptual framework on Social Determinants of Health illustrates how socioeconomic and political contexts (e.g., government, policies, and cultures) influence structural determinants (e.g., social class, education, income) and subsequently impact individual behaviors (e.g., obesity, smoking) and healthcare access [8]. While some studies in Turkey have focused on asthma-related factors, national research linking asthma to lifestyle, social determinants, and healthcare access is lacking [3]. Addressing these gaps is essential for developing effective strategies to mitigate the impact of asthma and improve public health outcomes in Turkey.
This study aimed to analyze the prevalence of self-reported asthma in Turkey and its determinants, such as individual factors, lifestyle, socioeconomic status, and healthcare access. It also addresses gaps in national research by investigating the link between asthma and lifestyle choices, social determinants, and healthcare accessibility in the country.
Methods
Study design and setting
The Turkish Statistical Institute (TurkStat) conducted the 2019 Turkiye Health Survey (THS), a cross-sectional study, between September and December 2019. For national representation, the sampling of surveys utilizes a stratified, two-stage cluster sampling method based on the "Address-Based Registry System". The THS 2019 included 17,084 adult individuals (aged 15 years and older) across Turkiye. The study methodology excluded individuals residing in dormitories, prisons, hospitals, nursing homes, small villages or hamlets.
The microdata set of the 2019 Health Survey was officially requested and obtained from TurkStat to develop a model to explore the determinants of asthma in Turkey [9, 10]. After the data cleaning process, we included 16,976 individuals aged 15 years and older in our analyses.
The dependent variable of this study was any positive answer to the question “During the past 12 months, have you had asthma (allergic asthma included)?”
The study employed a four-domain approach to analyze independent variables influencing asthma prevalance. Individual factors were evaluated by age, marital status, and difficulties in Turkish communication. Lifestyle assessment was used to assess the presence of obesity (measured via body mass index), and activity levels were categorized as inactive, minimally active, and highly active using MET calculations and smoking. Socioeconomic factors included education, employment status, and access to public health insurance. Healthcare service accessibility is assessed by cost-related unmet healthcare needs, delays experienced in accessing healthcare within the past 12 months due to lengthy appointment scheduling, and delays encountered in healthcare access within the past year due to transportation or distance constraints.
Detailed descriptions of each independent variable can be found on the metadata of the Turkiye Health Survey page of the Turkish Statistical Institute [9, 10]. Additionally, an appendix table titled "The Survey Questions and Categorization of Related Variables" has been added for easier reference.
Ethical approval
The principles of the Declaration of Helsinki were followed, meaning that the survey results were published at an aggregate level and that the anonymity of the interviewed individuals and households was fully secured. Before interpreting the results, the researchers obtained the consent of the Ethical Board from the School of Medicine at Ege University.
Statistical analyses
We evaluated the associations between independent variables and asthma using chi-square analysis. The data are presented as numbers and percentages. Variables that were significant according to Pearson's chi-square tests were considered independent variables in multivariate logistic regression models. We employed four logistic regression models in the analyses and calculated odds ratios (ORs) and 95% confidence intervals (CIs). Hosmer and Lemeshow's test yielded a probe value of more than 0.05 for all four models. For all analyses, the p value was considered to be < 0.05. We performed the analysis using the Statistical Package for Social Sciences (SPSS) version 26.
Results
The participants in the study group had an average age of 44.0±17.7 years, 33.9% of whom were younger than 35 years. The percentage of women was 54.6%, and 68.6% of the respondents were married.
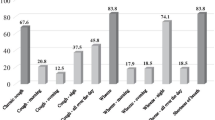
A minority of the group (3.1%) reported challenges in native language communication. Furthermore, 15.0% were unemployed, while 32.8% identified as homemakers. Notably, 15.4% indicated experiencing cost-related unmet healthcare needs (Table 1). The overall asthma prevalance was 9.8%. However, the prevalence of asthma varies significantly across individuals, lifestyles, and socioeconomic factors. Specifically, we observed higher asthma rates among women (12.7%), divorced or widowed individuals (19.3%), and those facing communication difficulties in Turkey (21.6%). Moreover, obese individuals (21.5%), inactive individuals (11.6%), those with less than 5 years of education (14.9%), and those covered by public health insurance (10.0%) exhibited elevated asthma prevalence. Moreover, asthma prevalence was notably greater among homemakers (14.3%), individuals with the lowest income (13.0%), and those with high levels of cost-related unmet needs (14.9%). Notably, delays due to lengthy appointment scheduling (11.9%) and delays due to distance or transportation constraints (14.9%) were statistically significant (Table 1).
Four multivariate models were constructed to assess the influence of individual characteristics, lifestyle factors, socioeconomic determinants, and access to the healthcare system. As new variables were added to each model, Nagelkerke's R-squared values increased.
In the first model assessing individual characteristics, it was found that older age increased the risk of asthma, and among the divorced/widowed individuals, there was a 1.6-fold (95% CI: 1.3-2.1) increase in risk, while those experiencing difficulty in communication in Turkish showed a 1.6-fold (95% CI: 1.3-2.0) increase in risk(Table 2).
In Model 2, which was developed by adding lifestyle factors, there was no change in the impact of individual characteristics; additionally, both obesity and activity were observed to increase the risk of asthma.
Model 3, which included socioeconomic variables, showed that the effects of individual characteristics and obesity persisted, but contrary to univariate analyses, only low education levels and the lowest income group increased the risk of asthma. The risk of asthma disappeared for minimal activities in Model 3 (Table 2).
The addition of variables related to access to healthcare services in Model 4 did not alter the effects of the variables in the previous three models except for the effect of lowest income. The risk of asthma increased by 1.6-fold (95% CI: 1.4-1.8) due to cost-related unmet healthcare needs and by 1.2-fold (95% CI: 1.1-1.4) among those experiencing delays due to lengthy appointment scheduling. A slight decrease in the impact of gender was observed after adding socioeconomic and access to healthcare variables. A similar effect was observed for difficulty in communication in Turkish(Table 2).
Discussion
This study pioneers the investigation of the combined influence of individual characteristics, lifestyle factors, socioeconomic determinants, and healthcare accessibility on asthma within a population that is representative of Turkey. Studies on asthma or its prevalence in Turkey are primarily hospital-based, resulting in a wide range of prevalence rates [3, 4, 11,12,13,14,15].Our study relies on self-reported asthma and is not based on a specific phenotype; we did not encounter a similar study representing both rural and urban areas across Turkey. Nevertheless, our findings align with both population-based studies conducted in specific regions of Turkey and are even more robust than those of other studies [4, 16,17,18]and within the range of global prevalence estimates of ever-existing asthma derived from 220 population-based studies [16]. The multivariate models used in our analysis allowed us to assess the independent contributions of various factors to asthma risk while controlling for potential confounders. Interestingly, we observed that the impacts of individual characteristics, lifestyle factors, and socioeconomic factors remained consistent across the different models, highlighting their robust associations with asthma outcomes.
Individual factors are among the most frequently studied determinants affecting asthma prevalance in the literature. In our study, both univariate and multivariate analyses consistently showed a greater prevalance of asthma among women, older individuals, specifically divorced or widowed individuals, and those experiencing difficulties in communication in Turkey in all four models.
In this study, the prevalence of asthma in Turkey increased with age, particularly among individuals aged 45 years and older. Global research as well as some national research indicates a rise in adult asthma prevalance across age groups, notably from young adults through middle age [11,12,13]. The SNAPSHOT study, which was conducted in five Middle Eastern countries, including Turkey, and two population-based studies, which were conducted in two of the provinces of Turkey, support this trend of increasing asthma prevalance with age, as observed in our study [15, 17]. This outcome could be explained by the degenerative alterations in the respiratory system associated with aging, as well as the coexistence of chronic pulmonary conditions in the elderly population. Physiologic and immunologic changes in aging populations complicate asthma diagnosis and management. Factors such as nonadherence, tobacco use, inhaler difficulties, and corticosteroid-related side effects contribute to decreased disease control across age groups [18, 19].
In accordance with national and international research, our study revealed a higher rate of asthma in women [4, 13, 15,16,17, 20, 21]. There are varying results from different countries regarding the impact of marital status on asthma prevalance. While one study found no association between relationship status and asthma [22], a study from India reported a greater prevalance of asthma among divorced or widowed individuals [23]. In our study, the elevated asthma rates among divorced or widowed individuals may be attributed to factors such as a greater proportion of divorced/widowed women of older age and lower income levels. Furthermore, stress, either independently or leading to unhealthy eating habits, could also contribute to the increased frequency of asthma in our study.
We observed a greater prevalence of asthma among individuals facing difficulties in native language communication. This finding suggests a potential causal relationship between language barriers and asthma prevalence. Notably, significant racial and ethnic disparities regarding asthma morbidity, prevalence, mortality rates, and responses to medications have been reported in the literature [20, 24], which aligns with the findings of our study. However, it is important to note that Turkey's census categories do not explicitly define racial and ethnic groups. Despite Turkish being the primary language of instruction in educational institutions, a considerable portion of the population speaks Kurdish (14%) and Arabic (2%), with the rest belonging to other language groups [21]. A study conducted in Turkey shed light on the challenges encountered by individuals lacking proficiency in the official language when accessing healthcare. These challenges include limited access to health information, strained patient-provider relationships, delays in seeking medical care, reliance on others for healthcare access, low adherence to treatment regimens, dissatisfaction with healthcare services, and difficulties exercising healthcare right [25].
Although a relationship between both obesity and physical activity with asthma was found in the univariate analysis, minimal physical activity was not found to be associated with asthma in Models 3 and 4. The literature has shown that obesity is associated not only with the development of asthma but also with asthma-related limitations in activities such as sports, indicating its role in the manifestation of asthma [26,27,28]. Given the increasing trend of obesity in Turkey [29, 30], it is crucial to enhance preventive and therapeutic services related to obesity in healthcare [30, 31] Following the inclusion of socioeconomic and healthcare access variables in the model, the removal of minimal physical activity as a risk factor suggests that even the addition of walking paths in socioeconomically disadvantaged areas could be beneficial for the control of asthma [31].
Our study findings indicate that the prevalence of asthma is highest among former smokers, with nonsmokers showing a greater frequency of asthma than regular or occasional smokers. This observation raises several important questions. First, it underscores the complex relationship between smoking status and asthma development, highlighting the need for a nuanced understanding of these associations [32]. Second, smoking cessation may not immediately alleviate the risk of asthma, as evidenced by the elevated asthma rates among former smokers [33, 34]. These complexities underscore the necessity for further research to elucidate the mechanisms underlying the observed patterns and to inform targeted interventions for asthma prevention and management. The cross-sectional nature of our study adds a layer of complexity to accurately interpreting cause–effect relationships. Similarly, a previous cross-sectional study in Turkey indicated a lower smoking prevalence among people with asthma than among the general population, potentially contributing to these findings [34]. Furthermore, factors beyond smoking, especially in allergic and elderly populations, play a role in the complex dynamics of asthma development. The prevalence of asthma associated with smoking seems to mirror that of the general population, yet asthma management tends to be more challenging and severe in active smokers [33]. These factors highlight the need for personalized approaches to asthma management, taking into account individual risk factors and lifestyle choices. However, further research is needed to better understand the relationship between smoking and asthma development in different populations.
In the literature, socioeconomic status has often been assessed either independently as education or in some studies as a combination of education and income. In this research, the effects of four different SES variables were evaluated both individually and collectively.
According to the univariate analyses, all socioeconomic status (SES) variables, such as education, insurance coverage, income, and employment, were found to be associated with asthma. However, in the multiple regression analyses, among these SES variables, the lowest income level group and lower education were identified as risk factors for asthma in Turkey, while employment appeared to act as a protective factor.
Education has consistently been found to be significantly associated with asthma in both univariate and multivariate analyses, consistent with the findings of numerous national and international studies [23, 24, 35, 36]. Education is not only crucial for asthma onset but also plays a significant role in asthma management [35, 37]. Its stability over time, unlike occupation and income, can vary throughout life, which can explain its continued impact across all models, particularly due to its influence on health literacy, which is a key determinant of treatment adherence.
While conflicting results due to confounding factors exist, an expanding body of research indicates a link between low income and increased asthma prevalence, and exacerbations [35, 36, 38]. In our study, although the lowest income level was significant in Model 3, this association disappeared when healthcare access variables were considered.
Additionally, the absence of a discernible impact of having health insurance in the multivariate analyses could be attributed to several factors. One possible explanation is the comprehensive coverage provided by universal health insurance in Turkey, which may have minimized the differences between insured and uninsured individuals regarding access to healthcare services related to asthma. These findings suggest that healthcare access could serve as a mediator between insurance, income, and asthma outcomes, highlighting the intricate interplay of socioeconomic factors in health outcome [8, 36].
In our study, we observed a significant disparity in access to healthcare services for asthma patients, particularly concerning cost-related issues and appointment unavailability. This finding is crucial for understanding the challenges in controlling asthma as a disease. Asthma imposes substantial financial burdens due to the high costs associated with diagnosis, treatment, and ongoing care, including expensive medications and specialized services [39, 40]. Research indicates that individuals with uncontrolled asthma experience higher rates of hospitalization and medication prescriptions, leading to increased healthcare costs for asthma-related and general healthcare needs. These disparities are observed globally, even in countries with universally funded healthcare systems [41,42,43].
Despite Turkey's relatively high health insurance coverage, access barriers related to cost persist. Analysis of global health expenditure data reveals a decline in Turkey's healthcare spending as a percentage of GDP, leading to heightened private healthcare expenses, mainly driven by out-of-pocket payments and private health insurance. This trend intensifies the financial burden on individuals seeking healthcare services [42]. Furthermore, the rapid expansion of healthcare privatization in recent years has resulted in a considerable migration of specialized services from the public to private sectors in Turkey, with poor patient satisfaction outcomes in the public sector [43]. Therefore, addressing healthcare access for asthma patients, starting from preventive services, is crucial and should be carefully addressed in healthcare policies.
This study was conducted not based on a specific asthma survey but rather by utilizing a single question related to asthma from a study aiming to identify health issues in Turkey. Limitations of this study include its reliance on self-reported asthma rather than clinical diagnosis, which may introduce recall bias and misclassification. Additionally, the study's cross-sectional design limits the ability to establish causal relationships between variables. The use of self-reported data also raises concerns about the accuracy and consistency of responses, particularly regarding sensitive topics such as smoking and income. Furthermore, the study did not differentiate between asthma phenotypes or severity levels, which could have provided more nuanced insights into the relationship between individual characteristics and asthma outcomes. There might be other unmeasured confounding factors that were not accounted for in the study, such as environmental and occupational factors, genetic predisposition, and exposure to allergens.
This study highlights the intricate effects of individual characteristics, lifestyle factors, socioeconomic factors, and healthcare accessibility on asthma prevalence in Turkey. Turkish women, older individuals, particularly divorced or widowed people, and those with communication challenges showed a greater prevalence of asthma. Tailored interventions focusing on behavioral changes and enhanced primary care services are crucial, especially for elderly people with asthma. Overall, our findings underscore the need for targeted interventions addressing language barriers in healthcare to improve asthma management and healthcare outcomes among linguistically diverse populations. The efficacy of intensive pulmonary rehabilitation programs, incorporating exercise training, dietary adjustments, and psychological support, has been demonstrated in improving the management of obese individuals with poorly controlled asthma, underscoring the value of such interventions in enhancing asthma control, physical health, and exercise performance.
Although initially related to asthma, minimal physical activity was not a significant risk factor in later models, suggesting that even basic exercise interventions can benefit asthma control, especially in disadvantaged areas. Smoking patterns underscore the need for personalized approaches and further research into smoking's impact on asthma. Education consistently influenced asthma prevalence, while low income was identified as a risk factor in Turkey. Employment acted protectively. The limited impact of health insurance suggests the importance of addressing healthcare access barriers through policy interventions. Despite high health insurance coverage, access barriers related to cost and appointment unavailability persist. Robust policies targeting preventive services and equitable access to specialized care are crucial, given the decline in healthcare spending and the growing private healthcare sector.
In conclusion, a comprehensive approach involving individualized interventions, lifestyle modifications, targeted healthcare policies addressing socioeconomic barriers, and equitable.
Availability of data and materials
This study is not a clinical trial. The data that support the findings of this study are available from the Turkish Statistical Institute, but restrictions apply to the availability of these data, which were used under license for the current study and are not publicly available. However, the data are available from the authors upon reasonable request and with the permission of the Turkish Statistical Institute.
Contact person for the study’s data request: aslidavas@gmail.com
The website where the data can be purchased: https://data.tuik.gov.tr/Kategori/GetKategori?p=Health-and-Social-Protection--101
References
Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention Updates . 2023. https://ginasthma.org/reports/.
The Global Asthma Report 2022. Int J Tuberc Lung Dis. 2022;26(1):1–104. https://doi.org/10.5588/ijtld.22.1010.
Kurt E, Metintas S, Basyigit I, Bulut I, Coskun E, Dabak S, et al. Prevalence and Risk Factors of Allergies in Turkey (PARFAIT): results of a multicentre cross-sectional study in adults. Eur Respir J. 2009;33(4):724–33. https://doi.org/10.1183/09031936.00082207.
Çelik GE, Soyer Ö, Aydın Ö. Astım Tanı ve Tedavi Rehberi 2020 Güncellemesi. Ankara: Buluş Matbaa; Available from: https://www.toraks.org.tr.
Merhej T, Zein JG. Epidemiology of Asthma: Prevalence and Burden of Disease. 2023. 3–23. https://doi.org/10.1007/978-3-031-32259-4_1/.
Trivedi M, Pappalardo AA, Udoko M, Garg A, Phipatanakul W, Szefler SJ, et al. Social determinants of health in asthma through the life course. J Allergy Clin Immunol Pract. 2022;10(4):953–61. https://doi.org/10.1016/j.jaip.2021.12.032.
Perez MF, Coutinho MT. An overview of health disparities in asthma. Yale J Biol Med. 2021;94(3):497–507.
Sullivan K, Thakur N. Structural and social determinants of health in asthma in developed economies: a scoping review of literature published between 2014 and 2019. Curr Allergy Asthma Rep. 2020;20(2):5. https://doi.org/10.1007/s11882-020-0899-6.
TURKSTAT. Metadata of Turkey Health Survey. 2019. Cited 2023 Nov 25. Available from: https://data.tuik.gov.tr/Kategori/GetKategori?p=saglik-ve-sosyal-koruma-101&dil=2.
TURKSTAT. Turkey Health Survey, 2019 . https://data.tuik.gov.tr/Bulten/Index?p=Turkey-Health-Survey-2019-33661.
Yildiz F, Mungan D, Gemicioglu B, Yorgancioglu A, Dursun B, Oner Erkekol F, et al. Asthma phenotypes in Turkey: a multicenter cross-sectional study in adult asthmatics PHENOTURK study. Clin Respir J. 2017;11(2):210–23. https://doi.org/10.1111/crj.12326.
Kılıç M, Yalçınkaya G. The frequency of asthma and allergy symptoms in adults and its related factors. Anatol J Fam Med. 2023;6(2):93–9. https://doi.org/10.5505/anatoljfm.2023.85619.
Celik GE, Aydin O, Gokmen D, Koycu Buhari G, Celebi Sozener Z, Gemicioglu B, et al. Picturing asthma in Turkey: results from the Turkish adult asthma registry. J Asthma. 2023;60(11):1973–86. https://doi.org/10.1080/02770903.2023.2206902.
Daloğlu GÖ, Fişekçi Sibel Evyapan, Göksel Fatma Kıter, Zencir Mehmet, Başer Sevin. Denizli il merkezindeki 20–49 yaş grubu erişkinlerde astım semptom prevalansı ve etkileyen risk faktörleri. Toraks Derg. 2006;7:151–6.
Hamzaçebi̇ H, Ünsal M, Kayhan S, Bi̇lgi̇n S, Ercan S, Hastalıkları Hastanesi G, et al. Prevalence of asthma and respiratory symptoms by age, gender and smoking behaviour in Samsun, North Anatolia Turkey. Vol. 54, Tüberküloz ve Toraks Dergisi. 2006.
Song P, Adeloye D, Salim H, Dos Santos JP, Campbell H, Sheikh A, et al. Global, regional, and national prevalence of asthma in 2019: a systematic analysis and modelling study. J Glob Health. 2022;29(12):04052. https://doi.org/10.7189/jogh.12.04052.
Tarraf H, Aydin O, Mungan D, Albader M, Mahboub B, Doble A, et al. Prevalence of asthma among the adult general population of five Middle Eastern countries: results of the SNAPSHOT program. BMC Pulm Med. 2018;18(1):68. https://doi.org/10.1186/s12890-018-0621-9.
Ponte EV, Lima A, Almeida PCA, de Jesus JPV, Lima VB, Scichilone N, et al. Age is associated with asthma phenotypes. Respirology. 2017;22(8):1558–63. https://doi.org/10.1111/resp.13102.
Dharmage SC, Perret JL, Custovic A. Epidemiology of asthma in children and adults. Front Pediatr. 2019;18:7. https://doi.org/10.3389/fped.2019.00246.
Cunningham J. Socioeconomic status and self-reported asthma in Indigenous and non-Indigenous Australian adults aged 18–64 years: analysis of national survey data. Int J Equity Health. 2010;9(1):18. https://doi.org/10.1186/1475-9276-9-18.
Koc I, Hancioglu A, Cavlin A. Demographic Differentials and Demographic Integration of Turkish and Kurdish Populations in Turkey. Popul Res Policy Rev. 2008;27(4):447–57.
Cazzoletti L, Zanolin ME, Antonicelli L, Battaglia S, Bono R, Corsico A, et al. Relationship status and respiratory diseases: an analysis on a general population sample. In: Epidemiology. Eur Respir Soc; 2021: PA3514. https://doi.org/10.1183/13993003.congress-2021.PA3514.
Agrawal S, Pearce N, Ebrahim S. Prevalence and risk factors for self-reported asthma in an adult Indian population: a cross-sectional survey. Int J Tuberc Lung Dis. 2013;17(2):275–82. https://doi.org/10.5588/ijtld.12.0438.
Drake KA, Galanter JM, Burchard EG. Race, ethnicity and social class and the complex etiologies of asthma. Pharmacogenomics. 2008;9(4):453–62. https://doi.org/10.2217/14622416.9.4.453.
Bayram T, Sakarya S. Oppression and internalized oppression as an emerging theme in accessing healthcare: findings from a qualitative study assessing first-language related barriers among the Kurds in Turkey. Int J Equity Health. 2023;22(1):6. https://doi.org/10.1186/s12939-022-01824-z.
Dixon AE, Que LG. Obesity and asthma. Semin Respir Crit Care Med. 2022;43(05):662–74. https://doi.org/10.1055/s-0042-1742384.
Peters U, Dixon AE, Forno E. Obesity and asthma. J Allergy Clin Immunol. 2018;141(4):1169–79. https://doi.org/10.1016/j.jaci.2018.02.004.
Yücel ÜÖ, Çalış AG. The relationship between general and abdominal obesity, nutrition and respiratory functions in adult asthmatics. J Asthma. 2023;60(6):1183–90. https://doi.org/10.1080/02770903.2022.2137038.
Yumuk VD. Prevalence of obesity in Turkey. Obes Rev. 2005;6(1):9–10. https://doi.org/10.1111/j.1467-789X.2005.00172.x.
Sözmen K, Unal B, Capewell S, Critchley J, O’Flaherty M. Estimating diabetes prevalence in Turkey in 2025 with and without possible interventions to reduce obesity and smoking prevalence, using a modelling approach. Int J Public Health. 2015;60(S1):13–21. https://doi.org/10.1007/s00038-014-0622-2.
McLoughlin RF, Clark VL, Urroz PD, Gibson PG, McDonald VM. Increasing physical activity in severe asthma: a systematic review and meta-analysis. Eur Respir J. 2022;60(6):2200546. https://doi.org/10.1183/13993003.00546-2022.
Bellou V, Gogali A, Kostikas K. Asthma and tobacco smoking. J Pers Med. 2022;12(8):1231. https://doi.org/10.3390/jpm12081231.
Kamga A, Rochefort-Morel C, Le Guen Y, Ouksel H, Pipet A, Leroyer C. Asthma and smoking: a review. Respir Med Res. 2022;82:100916. https://doi.org/10.1016/j.resmer.2022.100916.
Yildiz F, Dursun AB, Disçi R. Prevalence of asthmatic smokers: Turkish experience ( PASTE Study). Clin Respir J. 2014;8(3):350–6. https://doi.org/10.1111/crj.12326.
Bacon SL, Bouchard A, Loucks EB, Lavoie KL. Individual-level socioeconomic status is associated with worse asthma morbidity in patients with asthma. Respir Res. 2009;10(1):125. https://doi.org/10.1186/1465-9921-10-125.
Grant T, Croce E, Matsui EC. Asthma and the social determinants of health. Ann Allergy Asthma Immunol. 2022;128(1):5–11. https://doi.org/10.1016/j.anai.2021.10.002.
Ilmarinen P, Stridsman C, Bashir M, Tuomisto LE, Vähätalo I, Goksör E, et al. Level of education and asthma control in adult-onset asthma. J Asthma. 2022;59(4):840–9.
Cardet JC, Louisias M, King TS, Castro M, Codispoti CD, Dunn R, et al. Income is an independent risk factor for worse asthma outcomes. J Allergy Clin Immunol. 2018;141(2):754–760.e3. https://doi.org/10.1016/j.jaci.2017.04.036.
Sekerel BE, Turktas H, Bavbek S, Oksuz E, Malhan S. Economic burden of pediatric asthma in turkey: a cost of illness study from payer perspective. Turkish Thorac J. 2020;21(4):248–54. https://doi.org/10.5152/TurkThoracJ.2019.19025.
Wilke T, Timmermann H, Mueller S, Hardtstock F, Unmuessig V, Welte RR, et al. Association between asthma control and healthcare costs: Results from a German linked data study. Heal Serv Manag Res. 2023;36(1):42–50. https://doi.org/10.1177/09514848221100749.
Redmond C, Akinoso-Imran AQ, Heaney LG, Sheikh A, Kee F, Busby J. Socioeconomic disparities in asthma health care utilization, exacerbations, and mortality: a systematic review and meta-analysis. J Allergy Clin Immunol. 2022;149(5):1617–27. https://doi.org/10.1016/j.jaci.2021.10.007.
Polin Katherine, YıldırımHasan Hüseyin WR. Health Systems in Action Insight for Türkiye. 2022. Available from: https://iris.who.int/bitstream/handle/10665/362347/9789289059213-eng.pdf?sequence=1https://iris.who.int/bitstream/handle/10665/362347/9789289059213-eng.pdf?sequence=1.
Yılmaz V. Exploring patient experiences of the internal market for healthcare provision in Turkey: publicness under pressure. J Soc Policy. 2021;50(3):588–605. https://doi.org/10.1017/S0047279420000343.
Acknowledgments
Not applicable
Funding
We did not utilize any financial resources.
Author information
Authors and Affiliations
Contributions
Aslı Davas played a key role in the data acquisition and performed the secondary analyses of the national sample. Asli Davas and Meltem Çiçeklioğlu contributed to the interpretation of the results and provided critical intellectual input throughout the research process. Both authors were actively involved in drafting and revising the manuscript, ensuring its intellectual content and accuracy. All the authors read and approved the final manuscript.
Authors' information (optional)
No information provided.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The principles of the Declaration of Helsinki were followed, meaning that the survey results were published at an aggregate level and that the anonymity of the interviewed individuals and households was fully secured. Before interpreting the results, the researchers obtained the consent of the Ethical Board of the School of Medicine, Ege University.
This study is not an experimental study; it is a secondary analysis of the 2019 Turkey Health Survey (THS), a cross-sectional study conducted between September and December 2019 by the Turkish Statistical Institute (TurkStat). The consent of the participants was obtained from the Turkish Statistical Institute. The declaration of the Turkish Statistical Institute regarding metadata and publication as well as Institutional Quality Check Reports can be accessed on the bottom right side of the webpage under metaveri segment: https://data.tuik.gov.tr/Bulten/Index?p=Turkey-Health-Survey-2019-33661
Consent to participation
Informed consent was obtained in writing from all individuals aged 15 and above who participated in this study. The consent forms are archived by the Turkish Statistical Institute. Face-to-face interviews were conducted by trained interviewers. All participants in the sample group were literate. This is not an experimental study, and therefore, additional human ethics and consent declarations are not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Davas, A., Çiçeklioğlu, M. Understanding the determinants of self-reported asthma in Turkey: insights from national data on individual, lifestyle, socioeconomic, and healthcare access factors. BMC Pulm Med 24, 349 (2024). https://doi.org/10.1186/s12890-024-03159-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03159-7