Abstract
Background
For patients with congenital heart disease-related pulmonary arterial hypertension (CHD-PAH), cardiopulmonary exercise testing (CPET) can reflect cardiopulmonary reserve function. However, CPET may not be readily accessible for patients with high-risk conditions or limited mobility due to disability. Echocardiography, on the other hand, serves as a widely available diagnostic tool for all CHD-PAH patients. This study was aimed to identify the parameters of echocardiography that could serve as indicators of cardiopulmonary function and exercise capacity.
Methods
A cohort of 70 patients contributed a total of 110 paired echocardiogram and CPET results to this study, with 1 year interval for repeated examinations. Echocardiography and exercise testing were conducted following standardized procedures, and the data were collected together with clinically relevant indicators for subsequent statistical analysis. Demographic comparisons were performed using t-tests and chi-square tests. Univariate and multivariate analyses were conducted to identify potential predictors of peak oxygen uptake (peak VO2) and the carbon dioxide ventilation equivalent slope (VE/VCO2 slope). Receiver operating characteristic (ROC) analysis was used to assess the performance of the parameters.
Results
The ratio of tricuspid annular plane systolic excursion to pulmonary artery systolic pressure (TAPSE/PASP) was found to be the only independent indicator significantly associated with both peak VO2 and VE/VCO2 slope (both p < 0.05). Additionally, left ventricular ejection fraction (LVEF) and right ventricular fractional area change (FAC) were independently correlated with the VE/VCO2 slope (both p < 0.05). TAPSE/PASP showed the highest area under the ROC curve (AUC) for predicting both a peak VO2 ≤ 15 mL/kg/min and a VE/VCO2 slope ≥ 36 (AUC = 0.91, AUC = 0.90, respectively). The sensitivity and specificity of TAPSE/PASP at the optimal threshold exceeded 0.85 for both parameters.
Conclusions
TAPSE/PASP may be a feasible echocardiographic indicator for evaluating exercise tolerance.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Background
Congenital heart disease-related pulmonary arterial hypertension (CHD-PAH) is a life-threatening chronic condition typically arising from intracardiac or extracardiac shunts, leading to both volume and pressure overload. It often results in diminished exercise tolerance [1, 2]. Regular assessment of activity levels is recommended for individuals with CHD-PAH [1]. Cardiopulmonary exercise test (CPET) is a noninvasive procedure capable of objectively assessing cardiopulmonary reserve function and exercise tolerance. It offers valuable insights into exercise capacity, gas exchange dynamics during exercise, ventilator efficiency, and cardiac function. Besides, CPET also aids in developing exercise regimens and holds prognostic value for CHD-PAH patients [3,4,5,6,7,8]. Early studies have identified peak oxygen uptake (peak VO2) and the carbon dioxide ventilation equivalent slope (VE/VCO2 slope) from CPET as univariate biomarkers with prognostic implications in this population [6, 9]. In addition, according to the European Society of Cardiology and the European Respiratory Society (ESC/ERS) guidelines for risk stratification in PAH patients, a peak VO2 ≤ 15 ml/kg/min or VE/VCO2 slope ≥ 36 is considered an intermediate-high risk determinant for prognosis [10]. However, CPET may not be feasible for all PAH patients, particularly those with contraindications or limited mobility due to disability. Hence, there is a pressing need for safer and simpler diagnostic modalities to assess the severity and exercise capacity of PAH patients.
Echocardiography, known for its safety, simplicity, and cost-effectiveness, is recommended as the primary screening tool for initial assessment and follow-up in patients with CHD-PAH [1, 10]. Several echocardiographic parameters have been identified to correlate with exercise capacity and demonstrate prognostic significance in PAH patients [11,12,13].
In view of these findings, our aim was to identify an echocardiographic parameter capable of reflecting exercise capacity in patients with CHD-PAH.
Methods
Patients
The study included patients who met the following criteria from October 2021 to April 2023 at Guangdong Provincial People’s Hospital. Inclusion criteria comprised individuals who were (1) aged ≥ 18 years, (2) diagnosed with hemodynamic criteria consistent with PAH as per catheterization, including mean pulmonary arterial pressure > 20 mmHg, pulmonary arterial wedge pressure ≤ 15 mmHg, and pulmonary vascular resistance > 2 Wood units, in accordance with the 2022 ESC/ERS pulmonary hypertension guidelines, and clinically classified as having CHD-PAH, and (3) underwent echocardiography, 6-minute walk distance (6MWD), and CPET within 48 h. Patients with any of the following conditions were excluded: (1) other forms of pulmonary hypertension, (2) refusal to provide informed consent. After one year of enrollment, patients were recalled for repeat examinations.
Echocardiography
Routine echocardiographic measurements were performed with patients positioned in the left lateral decubitus position using commercially available echocardiography systems (Philips EPIQ 7 C, Philips CV x, or Philips iE Elite). Images from three consecutive beats were digitally stored for offline analysis (QLAB 13.0, Philips Andover, MA). Various parameters including left ventricular ejection fraction (LVEF), right atrial area (RAA), tricuspid annular plane systolic excursion (TAPSE), right ventricular free wall thickness (RVWT), peak systolic velocity of the tricuspid annulus (S’), right ventricular fractional area change (FAC), echocardiography-estimated pulmonary arterial mean pressure (ePAMP), and echocardiography-estimated pulmonary arterial systolic pressure (ePASP) were measured based on current guidelines [14]. Among them, ePASP was calculated using the tricuspid regurgitation jet velocity, combined with an estimate of right atrial pressure derived from inferior vena cava diameter and respiratory changes. Echocardiography-estimated pulmonary arterial diastolic pressure (ePADP) was estimated from the velocity of the end-diastolic pulmonary regurgitant jet, also combined with the estimated right atrial pressure. The formula for calculating ePAMP is: ePAMP = 1/3(ePASP) + 2/3(ePADP). Additionally, right atrial and right ventricular two-dimensional speckle tracking imaging parameters were analyzed. Images of 4-chamber apical views focused on the right ventricle were obtained with a sector narrowing of 30°-60° and an acquisition frequency of 60–90 images per second [15]. Right atrial strain during the reservoir phase (RASr) and right ventricular free wall longitudinal strain (RVFWLS) were included in the study.
Cardiopulmonary exercise testing
CPET was performed using the Alfred Schiller AG CS-200 cardiopulmonary exercise testing system. Following strict multistage calibration, patients underwent symptom-limiting maximal exercise tests on a bicycle ergometer (Ergoselect, Ergoline 900, Germany), with SpO2 monitored using a fingertip pulse oximeter (Heal Force, PC-60C1, China). The Ramp protocol was adopted, and patients were encouraged to exert maximal effort in the absence of discomfort. Expected values for each parameter were referenced from the Wasserman formula. Recorded CPET parameters included peak oxygen uptake (peakVO2), carbon dioxide output (VCO2), minute ventilation (VE), and VE/VCO2 slope. The anaerobic threshold was determined using the V-slope method.
Six-minute walk test
All patients underwent a non-encouraged 6-minute walk test in a 30-meter-long corridor under the same environmental conditions. Throughout the test, participants’ heart rate and oxygen saturation were monitored every minute, with blood pressure measured at the beginning and end of the test. Upon completion of the 6 min, the walk distance was recorded, and participants completed the Borg Dyspnea and Fatigue Scale questionnaires.
Statistical analysis
Data analysis was conducted using EmpowerStats (www.empowerstats.com, X&Y Solutions, Inc., Boston, MA) and R software version 4.1.1 (http://www.r-project.org). Continuous variables following a normal distribution were expressed as mean ± standard deviation, while categorical variables were expressed as numbers and proportions. Chi-square tests were used for group comparisons of categorical variables. Student’s t-tests were used for normally distributed continuous variables. Kruskal‒Wallis test was applied for skewed continuous variables. Indicators with a p value < 0.05 were included in multivariate analysis, progressively eliminated via forward stepwise regression. Variables with a p value < 0.05 in the multivariate analysis were incorporated into receiver operating characteristic (ROC) curve analysis, and the area under the curve (AUC) was calculated. The optimal predictive threshold was determined, and sensitivity and specificity of each index for predicting intermediate-high risk, as stratified by CPET according to the 2022 ESC/ERS pulmonary hypertension guidelines, were calculated.
Results
Baseline characteristics
A total of 70 patients were diagnosed with CHD-PAH, among whom 40 underwent two sets of echocardiography and CPET within a one-year interval. Finally, they contributed 110 paired echocardiogram and CPET results. Baseline characteristics of the overall population are presented in Table 1. Patients had a mean age of 35 ± 8 years, with the majority of female (87%), and the majority falling into World Health Organization functional class (WHO-FC) I-II (96%). Only the distributions of WHO-FC were significantly different between the subgroups (both p < 0.01).
Compared to individuals with a peak VO2 > 15 ml/kg/min, those with a peak VO2 ≤ 15 ml/kg/min demonstrated lower SpO2 and shorter 6MWD (p = 0.001, p < 0.001, respectively). Similarly, patients with a VE/VCO2 slope ≥ 36 exhibited lower SpO2 and shorter 6MWD (p < 0.001, p < 0.001, respectively). Within the subgroup with a peak VO2 ≤ 15 ml/kg/min, RAA, RVWT, S’, ePASP, and RVFWLS were higher (all p < 0.001), while FAC, TAPSE/PASP, and RASr were lower (all p < 0.001). Conversely, in the subgroup with a VE/VCO2 slope ≥ 36, RAA, RVWT, ePAMP, ePASP, and RVFWLS were higher (all p < 0.01), while FAC and TAPSE/PASP were lower (both p < 0.001).
Correlation analysis
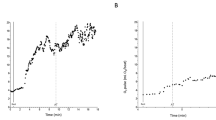
The results of univariate and multivariate analyses of the predictive factors for peak VO2 and VE/VCO2 slope are presented in Tables 2 and 3, respectively. Figure 1 depicts the linear correlation analysis between the echocardiographic parameters and the main CPET results in the overall population. According to our multivariate analysis, only TAPSE/PASP was independently associated with peak VO2 (β = 5.72, p = 0.019). In the multivariate analysis of the VE/VCO2 slope, LVEF, FAC, and TAPSE/PASP were found to be independently predictive factors (β = -0.48, p = 0.022; β = -0.65, p < 0.001; β = -23.29, p = 0.024, respectively). LVEF weakly correlated with VE/VCO2 slope, with the correlation coefficient of 0.20. Among the echocardiographic parameters assessed in our study, only TAPSE/PASP demonstrated independent and moderate linear correlation with both peak VO2 and VE/VCO2 slope.
Linear correlation analysis between echocardiography parameters and the main results of the cardiopulmonary exercise testing
(a) Relationship between peak VO2 and TAPSE/PASP. (b) Relationship between VE/VCO2 slope and TAPSE/PASP. (c) Relationship between VE/VCO2 slope and FAC. (d) Relationship between VE/VCO2 slope and LVEF. Abbreviations: TAPSE/PASP, the ratio of tricuspid annular plane systolic excursion and systolic pulmonary arterial pressure; FAC, fractional area change; LVEF, left ventricular ejection fraction
ROC analysis
Figure 2; Table 4 shows the results of the ROC analysis for the overall population regarding the selected parameters in relation to peak VO2 and VE/VCO2 slope values. TAPSE/PASP exhibited the highest AUC for predicting both a peak VO2 result of ≤ 15 mL/kg/min and a VE/VCO2 slope result of ≥ 36 (AUC = 0.91, AUC = 0.90, respectively). Additionally, the optimal threshold for TAPSE/PASP to predict a peak VO2 result of ≤ 15 mL/kg/min was determined to be 0.26 mm/mmHg, with a sensitivity and specificity of 0.88 and 0.88, respectively. Similarly, to predict a VE/VCO2 slope ≥ 36, the cutoff for TAPSE/PASP was 0.23 mm/mmHg, with a sensitivity of 0.85 and specificity of 0.91. The AUC for the other two parameters, LVEF and FAC, which were independently associated with VE/VCO2 slope, were 0.46 and 0.70, respectively.
Receiver Operating Characteristic curves for predicting peak VO2 ≤ 15 mL/kg/min and VE/VCO2 slope ≥ 36. (a) ROC curve depicting the performance of TAPSE/PASP in predicting peak VO2 ≤ 15 mL/kg/min. (b) ROC curves illustrating the predictive capabilities of TAPSE/PASP, FAC, and LVEF for VE/VCO2 slope ≥ 36. Abbreviations: TAPSE/PASP, the ratio of tricuspid annular plane systolic excursion and systolic pulmonary arterial pressure; FAC, fractional area change
Discussion
The findings of our study revealed a significant correlation between TAPSE/PASP and exercise capacity, as indicated by peak VO2 and VE/VCO2 slope during CPET in patients with PAH. TAPSE/PASP exhibited excellent performance, with higher AUC, sensitivity, and specificity in distinguishing intermediate-high risk patients, as stratified by CPET according to ESC/ERS pulmonary hypertension guidelines. To the best of our knowledge, this is the first study to compare the relationship between TAPSE/PASP and CPET in a PAH population.
Previous studies have suggested that various echocardiographic parameters, including right ventricular global longitudinal strain, RVFWLS, FAC, TAPSE, S’, and RAA, could classify PAH patients based on peak VO2 or VE/VCO2 slope [13]. Besides, Sljivic et al. have also demonstrated that the right ventricular global longitudinal strain and 3-dimensional right ventricle ejection fraction are strongly associated with exercise capacity in patients with heart failure and a reduced ejection fraction (HFrEF) [16]. Additionally, Liu et al. reported that right ventricular peak systolic strain might aid in classifying PAH patients according to exercise testing risk stratification cut-offs [12]. These studies suggest that right ventricular function parameters obtained via echocardiography may reflect cardiopulmonary reserve function and exercise capacity. However, our study revealed that among several commonly used echocardiographic parameters of right ventricular function, only TAPSE/PASP was independently and concurrently associated with both peak VO2 and VE/VCO2 slope after multivariate analysis. While FAC was moderately correlated with VE/VCO2 slope and demonstrated some ability to distinguish CHD-PAH patients at intermediate-high risk, LVEF exhibited weak correlation and poor classification ability, with an AUC of only 0.46 in the overall population. This aligns with previous findings suggesting that VE/VCO2 slope was strongly related to right ventricular function but poorly and even not related to left ventricular function [17,18,19].
As a direct indicator of exercise ability, 6MWD appeared to be less correlated with CPET than TAPSE/PASP. This could be attributed to the influence of various factors, including objective factors such as sex, age, height, weight, comorbidities, as well as subjective factors such as the learning curve and motivation [10].
Two-dimensional speckle tracking echocardiographic parameters, such as RASr and RVFWLS, did not emerge as independent influencing factors in our study. One potential explanation could be their linear correlation with TAPSE/PASP, which in turn exhibited a robust correlation with peak VO2 and VE/VCO2 slope.
Furthermore, the ROC analysis results in our study, including AUC, sensitivity, and specificity, highlighted the superiority of TAPSE/PASP over other parameters in predicting both peak VO2 ≤ 15 mL/kg/min and VE/VCO2 slope ≥ 36.
In patients with CHD-PAH, inadequate control of volume and pressure overload can lead to three-layer remodeling of distal precapillary pulmonary vessels, including uncontrolled growth of endothelial cells, smooth muscle cells, and fibroblasts, as well as infiltration of inflammatory cells, [20, 21] accompanied by an increase in pulmonary vascular resistance, resulting in right heart dysfunction and right ventricular-pulmonary artery uncoupling [22]. Damage to the pulmonary vascular bed can cause pulmonary ventilation-perfusion mismatch, manifested as an elevated VE/VCO2 slope in CPET. [23], while decreased exercise tolerance due to right heart dysfunction is reflected in a reduced peak VO2 [23]. Therefore, a right ventricle-pulmonary arterial coupling index may be associated with ventilatory inefficiency and maximal oxygen uptake.
TAPSE/PASP, initially proposed by Guazzi et al. in patients with left heart disease and Group 2 PH, [24] has been the most widely recognized and recommended noninvasive right ventricle-pulmonary arterial coupling index currently [10, 25, 26]. However, limited research has evaluated the correlation between this parameter and cardiopulmonary exercise ability. Legris et al. suggested a strong association between TAPSE/PASP and peak VO2 in patients with HFrEF [18]. In our study, TAPSE/PASP demonstrated a strong correlation with CPET values, reflecting cardiopulmonary function and exercise capacity, and efficiently classified patients at intermediate-high risk based on CPET parameters of ESC/ERS risk stratification. These findings suggest that TAPSE/PASP may provide additional information about exercise tolerance in disease assessment, clinical treatment, and follow-up for CHD-PAH patients, especially for high-risk patients unable to complete CPET.
This study had several limitations. It was conducted in a single center and requires validation in additional locations. The majority of patients in our study were WHO class I-II, limiting the generalizability of the results to patients with WHO class III-IV. Besides, patients with respiratory diseases that may impair ventilation reserve function were not excluded, potentially affecting CPET results. Additionally, longitudinal data were not included in this study, warranting further exploration of the consistency between TAPSE/PASP and changes in cardiopulmonary exercise.
Conclusions
TAPSE/PASP were strongly associated with exercise capacity and exhibited the best classification ability, as evidenced by the highest AUC, sensitivity, and specificity, making it effective in distinguishing PAH patients with impaired aerobic performance and heightened risk stratification. Therefore, TAPSE/PASP holds considerable potential for facilitating a convenient and safe evaluation of exercise tolerance in patients with CHD-PAH.
Data availability
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CHD-PAH:
-
Congenital heart disease-related pulmonary arterial hypertension
- CPET:
-
Cardiopulmonary exercise test
- peak VO2 :
-
Peak oxygen uptake
- VE/VCO2 slope:
-
Carbon dioxide ventilation equivalent slope
- ESC/ERS:
-
European Society of Cardiology and the European Respiratory Society
- PAH:
-
Pulmonary arterial hypertension
- 6MWD:
-
6-minute walk distance
- LVEF:
-
Left ventricular ejection fraction
- RAA:
-
Right atrial area
- TAPSE:
-
Tricuspid annular plane systolic excursion
- RVWT:
-
Right ventricular free wall thickness
- S’:
-
Peak systolic velocity of the tricuspid annulus
- FAC:
-
Fractional area change
- ePAMP:
-
Echocardiography-estimated pulmonary arterial mean pressure
- ePASP:
-
Echocardiography-estimated pulmonary arterial systolic pressure
- PADP:
-
Pulmonary arterial diastolic pressure
- RASr:
-
Right atrial strain during the reservoir phase
- RVFWLS:
-
Right ventricular free wall longitudinal strain
- peakVO2 :
-
Peak oxygen uptake
- VCO2 :
-
Carbon dioxide output
- VE:
-
Minute ventilation
- VE/VCO2 slope:
-
The carbon dioxide ventilation equivalent slope
- ROC:
-
Receiver operating characteristic
- AUC:
-
Area under the receiver operating characteristic curve
- WHO-FC:
-
World Health Organization functional class
- TAPSE/PASP:
-
The ratio of tricuspid annular plane systolic excursion to pulmonary artery systolic pressure
- HFrEF:
-
Heart failure and reduced ejection fraction
References
Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, et al. 2018 AHA/ACC Guideline for the management of adults with congenital heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. Circulation. 2019;139(14):e698–800.
Brida M, Gatzoulis MA. Pulmonary arterial hypertension in adult congenital heart disease. Heart. 2018;104(19):1568–74.
Diller GP, Dimopoulos K, Okonko D, Li W, Babu-Narayan SV, Broberg CS, et al. Exercise intolerance in adult congenital heart disease: comparative severity, correlates, and prognostic implication. Circulation. 2005;112(6):828–35.
Wensel R, Opitz CF, Anker SD, Winkler J, Höffken G, Kleber FX, et al. Assessment of survival in patients with primary pulmonary hypertension: importance of cardiopulmonary exercise testing. Circulation. 2002;106(3):319–24.
Blumberg FC, Arzt M, Lange T, Schroll S, Pfeifer M, Wensel R. Impact of right ventricular reserve on exercise capacity and survival in patients with pulmonary hypertension. Eur J Heart Fail. 2013;15(7):771–5.
Arena R, Lavie CJ, Milani RV, Myers J, Guazzi M. Cardiopulmonary exercise testing in patients with pulmonary arterial hypertension: an evidence-based review. J Heart Lung Transpl. 2010;29(2):159–73.
Wensel R, Francis DP, Meyer FJ, Opitz CF, Bruch L, Halank M, et al. Incremental prognostic value of cardiopulmonary exercise testing and resting haemodynamics in pulmonary arterial hypertension. Int J Cardiol. 2013;167(4):1193–8.
Araújo CG, Herdy AH, Stein R. Maximum oxygen consumption measurement: valuable biological marker in health and in sickness. Arq Bras Cardiol. 2013;100(4):e51–3.
Inuzuka R, Diller GP, Borgia F, Benson L, Tay EL, Alonso-Gonzalez R, et al. Comprehensive use of cardiopulmonary exercise testing identifies adults with congenital heart disease at increased mortality risk in the medium term. Circulation. 2012;125(2):250–9.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger R, Brida M et al. 2022 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Respir J. 2023; 61(1).
Farmakis IT, Demerouti E, Karyofyllis P, Karatasakis G, Stratinaki M, Tsiapras D et al. Echocardiography in Pulmonary arterial hypertension: is it time to reconsider its Prognostic Utility? J Clin Med. 2021; 10(13).
Liu BY, Wu WC, Zeng QX, Liu ZH, Niu LL, Tian Y, et al. Two-dimensional speckle tracking echocardiography assessed right ventricular function and exercise capacity in pre-capillary pulmonary hypertension. Int J Cardiovasc Imaging. 2019;35(8):1499–508.
Rehman MB, Garcia R, Christiaens L, Larrieu-Ardilouze E, Howard LS, Nihoyannopoulos P. Power of resting echocardiographic measurements to classify pulmonary hypertension patients according to European society of cardiology exercise testing risk stratification cut-offs. Int J Cardiol. 2018;257:291–7.
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23(7):685–713.
Sugimoto T, Dulgheru R, Bernard A, Ilardi F, Contu L, Addetia K, et al. Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging. 2017;18(8):833–40.
Sljivic A, Pavlovic KM, Bukumiric Z, Celic V. Association between right ventricle two- and three-dimensional echocardiography and exercise capacity in patients with reduced left ventricular ejection fraction. PLoS ONE. 2018;13(6):e0199439.
Rehman MB, Howard LS, Christiaens LP, Gill D, Gibbs J, Nihoyannopoulos P. Resting right ventricular function is associated with exercise performance in PAH, but not in CTEPH. Eur Heart J Cardiovasc Imaging. 2018;19(2):185–92.
Legris V, Thibault B, Dupuis J, White M, Asgar AW, Fortier A, et al. Right ventricular function and its coupling to pulmonary circulation predicts exercise tolerance in systolic heart failure. ESC Heart Fail. 2022;9(1):450–64.
Methvin AB, Owens AT, Emmi AG, Allen M, Wiegers SE, Dries DL, et al. Ventilatory inefficiency reflects right ventricular dysfunction in systolic heart failure. Chest. 2011;139(3):617–25.
Wagenvoort CA. The pathology of primary pulmonary hypertension. J Pathol. 1970;101(4):Pi.
Price LC, Wort SJ, Perros F, Dorfmüller P, Huertas A, Montani D, et al. Inflammation in pulmonary arterial hypertension. Chest. 2012;141(1):210–21.
Vonk NA, Chin KM, Haddad F, Hassoun PM, Hemnes AR, Hopkins SR et al. Pathophysiology of the right ventricle and of the pulmonary circulation in pulmonary hypertension: an update. Eur Respir J. 2019; 53(1).
Dumitrescu D, Sitbon O, Weatherald J, Howard LS. Exertional dyspnoea in pulmonary arterial hypertension. Eur Respir Rev. 2017; 26(145).
Guazzi M, Bandera F, Pelissero G, Castelvecchio S, Menicanti L, Ghio S, et al. Tricuspid annular plane systolic excursion and pulmonary arterial systolic pressure relationship in heart failure: an index of right ventricular contractile function and prognosis. Am J Physiol Heart Circ Physiol. 2013;305(9):H1373–81.
Fauvel C, Raitiere O, Boucly A, De Groote P, Renard S, Bertona J, et al. Interest of TAPSE/sPAP ratio for noninvasive pulmonary arterial hypertension risk assessment. J Heart Lung Transplantation. 2022;41(12):1761–72.
Guazzi M. Use of TAPSE/PASP ratio in pulmonary arterial hypertension: an easy shortcut in a congested road. Int J Cardiol. 2018;266:242–4.
Acknowledgements
The authors would like to thank all the patients involved for their support and cooperation.
Funding
This study was supported by the National Natural Science Foundation of China (82371963), Guangdong Basic and Applied Basic Research Foundation (2021A1515012232 and 2021A1515011366) and the NSFC lauching fund of the Guangdong Provincial People’s Hospital (8197070830, 8207070477, and 82270211), Guangdong Medical Science and Technology Research Foundation (B2023010), and Guangzhou Basic and Applied Basic Research Special Youth Doctoral “Setting Sail” Project (2024A04J5038).
Author information
Authors and Affiliations
Contributions
Each author of this study has made significant contributions. H.F. and C.Z. conceptualized and guided the study. L.Y., D.L., T.H. and H.F. drafted and revised the manuscript. G.Z. conducted the CPET on patients. L.Y., T.H. and X.L. acquired the echocardiography images. L.Y. and D.L. conducted the statistical analysis. The published version of the manuscript has been read and approved by all the authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of Guangdong Provincial People’s Hospital (NO. KY-Q-2022-353-02). All the procedure are followed by the guidelines of Helsinki. All patients in this study signed informed consent forms.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, L., Luo, D., Huang, T. et al. Echocardiographic assessment for cardiopulmonary function in patients with congenital heart disease-related pulmonary arterial hypertension. BMC Pulm Med 24, 306 (2024). https://doi.org/10.1186/s12890-024-03113-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03113-7