Abstract
Background
Remimazolam is safe and effective for moderate sedation during flexible bronchoscopy, but its safety and efficacy during endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) remains undetermined. The REST trial (NCT06275594) will be a prospective randomized study of remimazolam in patients undergoing EBUS-TBNA with conscious sedation. The primary aim is to evaluate whether remimazolam is safe and effective for moderate sedation during EBUS-TBNA compared to real-world midazolam and on-label midazolam.
Methods
The REST trial will recruit 330 patients from four university hospitals with mediastinal lesions suspected of being lung cancer who are eligible for EBUS-TBNA under moderate sedation. The participants will be randomized into groups using remimazolam, real-world midazolam, and on-label midazolam (US prescribing information dosage) to perform EBUS-TBNA for procedural sedation. The primary endpoint will be procedural success using composite measures.
Discussion
The REST trial will prospectively evaluate the efficacy and safety of remimazolam during EBUS-TBNA under moderate sedation. It will provide information for optimizing sedation modalities and contribute to practical benefits in patients undergoing EBUS-TBNA.
Trial registration
ClinicalTrials.gov (NCT06275594). Prospectively registered on 15 February 2024.
Similar content being viewed by others
Background
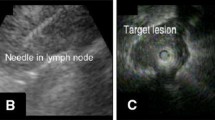
Real-time endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA), developed for examining mediastinal lymph nodes, uses an ultrasonic probe at the end of a conventional flexible bronchoscope. Compared to a flexible bronchoscope, it has a greater diameter and requires repeat needle aspiration from mediastinal lymph nodes. Thus EBUS-TBNA is a relatively longer procedure than flexible bronchoscopy [1, 2].
Systematic EBUS-TBNA includes sampling suspected lymph nodes based on imaging studies and routine sampling of stations 4R, 4L and 7 (if the short axis ≥ 8 mm). The SCORE study showed that compared to positron emission tomography guided targeted EBUS, a systematic EBUS procedure followed by esophageal investigation using the same EBUS bronchoscope (EUS-B), increases the sensitivity for detecting mediastinal nodal metastasis in lung cancer patients by 9% [3]. Given that the EBUS scope has a greater diameter and more stations need to be sampled during systematic EBUS-TBNA staging, appropriate sedation is essential.
Midazolam (onset of action 3–5 min) is an important agent for moderate sedation; however, the active metabolite of midazolam has an elimination half-life of 1.8–6.4 h, which can prolong post-procedural sedation. Propofol is a potent intravenous sedative with a very short onset of action (15–40 s) and a very short half-life, allowing rapid recovery. However, it requires constant monitoring due to potential respiratory depression or hypotension without antidote medication [4, 5].
Remimazolam is a novel benzodiazepine used for intravenous sedation. It has an ultra-short duration of action. It has been successfully used in procedural sedation and general anesthesia with fast onset and recovery times, high procedure success rates, and acceptable adverse profiles [5, 6]. Therefore, the benefits of remimazolam derived from its fast onset and recovery times warrant further examination in a prospective, controlled study. To date, no studies have evaluated the effectiveness and safety of remimazolam during EBUS-TBNA. The REST trial will evaluate whether remimazolam provides benefits in performing EBUS-TBNA compared to real-world midazolam, or on-label midazolam.
Methods/design
Study design and inclusion criteria
The REST trial will be a multicenter, open label, randomized clinical trial that will enroll patients undergoing EBUS-TBNA under conscious sedation to evaluate the efficacy and safety of remimazolam compared to real-world midazolam or on-label midazolam (Fig. 1). After providing informed consent, participants will be recruited from four institutions across South Korea: Yeungnam University Hospital, Asan Medical Center, Pusan National University Yangsan Hospital, and Chungbuk National University Hospital. The study will recruit participants from 1 April 2024 until 1 February 2025. Participants will be followed until 1 month after the procedure.
All consecutive patients over 18 years of age who are candidates for EBUS-TBNA due to suspected malignancy, with saturation pulse oximetry (SpO2) ≥ 90% in ambient air or with no more than 2 L/min oxygen support are eligible for enrollment. The exclusion criteria are patients undergoing simultaneous radial EBUS or electromagnetic navigation bronchoscopy; American Society of Anesthesiologists (ASA) score 4 or higher; Mallampati score 4; body mass index (BMI) < 18.4 or > 30.0; known allergic reaction to benzodiazepines, flumazenil, opioids, naloxone, or a medical condition affected by these agents; EBUS-TBNA performed outside the bronchoscopy unit; chronic kidney disease requiring dialysis; and patients with a current active acute infection or uncontrolled chronic inflammatory lung disease.
Randomization, data collection, and management
After providing informed consent, participants will be randomized centrally 1:1:1 to the remimazolam, real-world midazolam, or on-label midazolam arms after stratification by study site, age ≥ 60 vs. < 60 years, and BMI (> 23 vs. ≤ 23 kg/m2).
Randomization will be performed using a web-based electronic case report form (eCRF) created by Procuratio®. The assignment process will not involve the attending physicians. However, this study will be an open label study, so physicians will know what sedatives the patients are given. The enrolled participants will be evaluated for baseline characteristics, procedural profile, pathological results, and cough using a procedural convenience survey after study enrollment. The data to be collected are listed in Table 1. Complication profiles will be observed and recorded for up to 1 month after the procedure.
A web-based eCRF created by Procuratio® will be used to gather data. The eCRFs will be collected at the time of study enrollment and at a follow-up outpatient visit within 1 month after the procedure. The web-based eCRF will anonymize and secure all data. The enrollment procedure began in April 2024 with the goal of being completed by February 2025. The last round of data collection and follow-up is expected to be completed in March 2025.
Sedative, and procedural protocols
Before bronchoscopy, the oropharynx will be sprayed 10 times (10 mg/puff) with 10% lidocaine spray solution. Using a bronchoscope, 1% lidocaine solution will be administered to the vocal cords, mid-trachea, and both major bronchi. Additional lidocaine will be administered if requested by the bronchoscopist. The patient will be given oxygen at 5 L/min via nasal cannula.
An initial dose of 25–50 µg fentanyl and a single intravenous dose of 5.0 mg remimazolam (ASA I-II) or 2.5 mg remimazolam (ASA III) will be administered in the remimazolam arm. For the real-world midazolam arm, 2–3 mg midazolam will be administered with a maximum dose 7.5 mg. For on-label midazolam, 1.75 mg (< 60 years old and healthy) or 1.0 mg (≥ 60 years old or debilitated/chronically ill) midazolam will be administered to a maximum dose of 7.5 mg. The detailed sedation protocols are presented in Table 2.
Bronchoscopy will be started when an adequate sedation Modified Observer’s Assessment of Alertness/Sedation Scale (MOAA/S ≤ 3) score is achieved. If sedation is insufficient after the first dose of trial medication, patients can receive a maximum of five additional remimazolam doses in any 15 min window or a maximum of three additional doses of midazolam in any 12 min window in the real-world and on label midazolam arms at intervals of ≥ 2 min. Top-up doses of fentanyl (25–50 μg) at intervals of ≥ 5 min are permitted in all three arms, until adequate analgesia is achieved or a maximum of 200 μg has been administered. If there is still insufficient sedation to start the procedure, treatment failure is declared and rescue sedation is administered using drugs from the treatment group under the supervision of a respiratory physician without anesthesia personnel. During the procedure, all patients will be monitored via electrocardiogram, noninvasive blood pressure, oxygen saturation, and respiratory rate every 5 min. EBUS-TBNA procedures will be performed using the Olympus (BF-UC260FW) or EB‐1970UK (Pentax) by pulmonologists with at least 5 years of experience with EBUS-TBNA. The operator’s biopsy method will be respected without clear regulations and EBUS profiles will be recorded, including lymph node biopsy results by station, final diagnosis, and complication.
Sample size calculation
In the REST trial, expected procedural success of remimazolam group was 80%, those of real-world midazolam (control 1) was 60%, and those of on-label midazolam (control 2) was 40% [4, 7]. Therefore, two sided multiple comparison analysis was planned to test whether the procedural success rate of remimazolam group was significantly different from the two midazolam group. We accepted the 0.025 significance level under Bonferroni correction for multiple comparison. The sample size of each groups was 96 and the corresponding powers of each of the tests were 0.8. Based on an assumed 10% drop-out rate of patients after randomization, we aim to include a total of 330 patients.
Assessment of study outcomes
The primary objective is to compare the procedural success with remimazolam, real-world midazolam, or on-label midazolam using a composite measure. Secondary endpoints include the times until the procedure is started and the patient is fully alert after the procedure and the total procedure and recovery times. The requirement for flumazenil and total fentanyl dose are included. A cough visual analogue scale (VAS) and procedure convenience VAS measured by the patient, physicians performing the procedures, and nurses in the bronchoscopy room are also included. For safety, the vital signs will be recorded. All participants will be followed-up 1 month after the procedure to evaluate the presence of complications. The detailed definitions of the outcomes are presented in Table 3.
Ethics approval
The REST trial will be conducted in accordance with the principles of Good Clinical Practice and the tenets of the Declaration of Helsinki. The Institutional Review Board of each participating institution have already approved the study protocol: Yeungnam University Hospital (YUMC 2023–12–017), Asan Medical Center (S2023–2655), Pusan National University Yangsan Hospital (11–2023–024), and Chungbuk National University Hospital (2023–11–003–003). Informed consent will be obtained from all participants. The study is registered at ClinicalTrials.gov (NCT06275594).
Trial status
REST Trial is ongoing now. Enrollment began in April 2024 and is currently in progress with the aim of completing enrollment by March 2025. Final collection of data and formal analysis is planned at mid-2025.
Discussion
Proper sedation plays a crucial role in EBUS-TBNA procedures. It ensures patient comfort, reduces anxiety, and minimizes movement during the procedure, which is important for both the accuracy and safety of the biopsy. Furthermore, it can affect the overall patient experience. Patients who receive adequate sedation often report less discomfort, have less recall of the procedure, and show a greater willingness to undergo the procedure again if needed [8]. Various sedatives can be used for EBUS-TBNA to ensure patient comfort and procedure efficacy. Sedatives and opioids are frequently combined to achieve optimal sedation and analgesia. Commonly used sedatives include midazolam, ketamine, and propofol. Midazolam, commonly used for its anxiolytic and amnesic effects, is often administered in combination with fentanyl for EBUS-TBNA procedures. However, it has some disadvantages; while effective as a sedative, its onset may be delayed and its duration may be extended beyond the desired therapeutic window [9]. This is particularly evident in the elderly or patients with hepatic dysfunction, in whom the pharmacokinetics of midazolam are altered, leading to reduced metabolic clearance and consequently prolonged drug action. Such pharmacodynamic variability necessitates cautious administration and vigilant monitoring to mitigate the risks associated with protracted sedative effects [10].
Remimazolam is a recently developed ultra-short-acting benzodiazepine sedative [11]. Recent meta-analyses and studies have reported its usefulness for procedural sedation [12]. Its safety and effectiveness at providing sedation during bronchoscopy has been studied [4, 13]. Its unusual metabolism results in a quick onset and brief duration of effect [14]. In clinical trials, it has been found to offer efficient sedation with a superior profile to midazolam during bronchoscopy [4]. It achieves sleepiness rapidly without causing major changes in hemodynamic stability. It has also been linked to the reduced occurrence of bradycardia or hypotension compared to dexmedetomidine [15]. Compared to conventional bronchoscopy, EBUS-TBNA takes longer and involves direct contact with and irritation of the airway. Therefore, ensuring proper sedation is crucial. However, despite the advantage of the action time of remimazolam, no research has examined it in EBUS-TBNA.
Maintaining appropriate sedation during procedures is difficult, particularly when trying to maintain it at a moderate level. Without proper sedation, performing procedures becomes challenging, and more midazolam than the recommended dose may be used. In a recent study that compared the efficacy of remimazolam with midazolam dosed according to real-world medical practice and on-label prescribing information, remimazolam had similar effects to real-world midazolam for some parameters and was comparable to on-label midazolam in others [16]. In this trial, we will compare remimazolam with two different midazolam dosages to enhance its practical applicability in actual clinical environments.
The study participants will be drawn from four tertiary hospitals in South Korea, with minimal limitations on procedure settings. The study will standardize the method of local anesthesia and oxygen supply, while maintaining flexibility in other procedural areas to accommodate the specific situations at each hospital. Given that the study will involve three distinct cohorts within each facility, the results should be particularly applicable to real-world data.
The major limitation of this study is its open-label design, which lacks blinding and can introduce bias and affect the interpretation of results. To minimize observer bias and ensure objectivity in an open-label study, the cough visual analogue scale (VAS) and procedure convenience VAS will be obtained from clinicians, nurses, and patients. In addition, other evaluation criteria will be standardized and clearly defined.
In conclusion, the REST trial will be a unique, investigator-initiated trial that aims to identify the efficacy and safety of remimazolam in performing EBUS-TBNA, particularly in procedural sedation in adults outside the operating room. This study should determine the efficacy of remimazolam compared to midazolam and improve our understanding of this sedative for use in EBUS-TBNA. The trial will provide important information on the optimal usage of sedatives for EBUS-TBNA. The study outcomes will also be instructive for designing future comparative studies of EBUS-TBNA.
Availability of data and materials
The datasets generated and analyzed during the current study will be available from the corresponding author on reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
Body mass index
- EBUS-TBNA:
-
Endobronchial ultrasound-guided transbronchial needle aspiration
- eCRF:
-
Electronic case report form
- MOAA/S:
-
Modified Observer’s Assessment of Alertness/Sedation Scale
- VAS:
-
Visual analogue scale
References
Yasufuku K, Pierre A, Darling G, de Perrot M, Waddell T, Johnston M, da Cunha Santos G, Geddie W, Boerner S, Le LW, et al. A prospective controlled trial of endobronchial ultrasound-guided transbronchial needle aspiration compared with mediastinoscopy for mediastinal lymph node staging of lung cancer. J Thorac Cardiovasc Surg. 2011;142(6):1393-1400 e1391.
Kinsey CM, Arenberg DA. Endobronchial ultrasound-guided transbronchial needle aspiration for non-small cell lung cancer staging. Am J Respir Crit Care Med. 2014;189(6):640–9.
Crombag LMM, Dooms C, Stigt JA, Tournoy KG, Schuurbiers OCJ, Ninaber MK, Buikhuisen WA, Hashemi SMS, Bonta PI, Korevaar DA, et al. Systematic and combined endosonographic staging of lung cancer (SCORE study). Eur Respir J. 2019;53(2):1800800.
Pastis NJ, Yarmus LB, Schippers F, Ostroff R, Chen A, Akulian J, Wahidi M, Shojaee S, Tanner NT, Callahan SP, et al. Safety and Efficacy of Remimazolam Compared With Placebo and Midazolam for Moderate Sedation During Bronchoscopy. Chest. 2019;155(1):137–46.
Kim KM. Remimazolam: pharmacological characteristics and clinical applications in anesthesiology. Anesth Pain Med (Seoul). 2022;17(1):1–11.
Hu Q, Liu X, Wen C, Li D, Lei X. Remimazolam: An Updated Review of a New Sedative and Anaesthetic. Drug Des Devel Ther. 2022;16:3957–74.
Chow S-C, Shao J, Wang H. Sample size calculations in clinical research. 2nd ed. Boca Raton: Chapman & Hall/CRC; 2008.
Karewicz A, Faber K, Karon K, Januszewska K, Ryl J, Korczynski P, Gorska K, Dabrowska M, Krenke R. Evaluation of patients’ satisfaction with bronchoscopy procedure. PLoS ONE. 2022;17(10): e0274377.
Conway A, Chang K, Mafeld S, Sutherland J. Midazolam for sedation before procedures in adults and children: a systematic review update. Syst Rev. 2021;10(1):69.
Practice Guidelines for Moderate Procedural Sedation and Analgesia 2018: A Report by the American Society of Anesthesiologists Task Force on Moderate Procedural Sedation and Analgesia, the American Association of Oral and Maxillofacial Surgeons, American College of Radiology, American Dental Association, American Society of Dentist Anesthesiologists, and Society of Interventional Radiology. Anesthesiology. 2018;128(3):437–79.
Kilpatrick GJ, McIntyre MS, Cox RF, Stafford JA, Pacofsky GJ, Lovell GG, Wiard RP, Feldman PL, Collins H, Waszczak BL, et al. CNS 7056: a novel ultra-short-acting Benzodiazepine. Anesthesiology. 2007;107(1):60–6.
Jhuang BJ, Yeh BH, Huang YT, Lai PC. Efficacy and Safety of Remimazolam for Procedural Sedation: A Meta-Analysis of Randomized Controlled Trials With Trial Sequential Analysis. Front Med (Lausanne). 2021;8: 641866.
Kim SH, Cho JY, Kim M, Chung JM, Yang J, Seong C, Kim EG, Seok JW, Shin YM, Lee KM, et al. Safety and efficacy of remimazolam compared with midazolam during bronchoscopy: a single-center, randomized controlled study. Sci Rep. 2023;13(1):20498.
Schuttler J, Eisenried A, Lerch M, Fechner J, Jeleazcov C, Ihmsen H. Pharmacokinetics and Pharmacodynamics of Remimazolam (CNS 7056) after Continuous Infusion in Healthy Male Volunteers: Part I. Pharmacokinetics and Clinical Pharmacodynamics Anesthesiology. 2020;132(4):636–51.
Hu B, Zhang M, Wu Z, Zhang X, Zou X, Tan L, Song T, Li X. Comparison of Remimazolam Tosilate and Etomidate on Hemodynamics in Cardiac Surgery: A Randomised Controlled Trial. Drug Des Devel Ther. 2023;17:381–8.
Dao VA, Schippers F, Stohr T. Efficacy of remimazolam versus midazolam for procedural sedation: post hoc integrated analyses of three phase 3 clinical trials. Endosc Int Open. 2022;10(4):E378–85.
Acknowledgements
None.
Funding
This research was supported by Korean Association for the Study of Targeted Therapy (KASTT) affiliated with Korean Association for Lung Cancer (KASTT-20230211).
KASTT reviewed study protocol, and permitted study progress.
Author information
Authors and Affiliations
Contributions
All authors qualify for authorship under the ICMJE Recommendations (https://www.icmje.org). HYS, KSH, WJ, and JHA contributed to the concept and design of the study, manuscript preparation, revision, and final approval of the manuscript. HYS, KSH, SMM, JGJ, SHK, JYC, BY, SK, CMC, WJ and JHA contributed to critical revisions, and final approval of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The REST trial will be conducted in accordance with the principles of Good Clinical Practice and the tenets of the Declaration of Helsinki. The Institutional Review Board of each participating institution have already approved the study protocol: Yeungnam University Hospital (YUMC 2023–12–017), Asan Medical Center (S2023–2655), Pusan National University Yangsan Hospital (11–2023–024), and Chungbuk National University Hospital (2023–11–003–003). Informed consent will be obtained from all participants. The study is registered at ClinicalTrials.gov (NCT06275594).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Seol, H.Y., Hong, K.S., Jang, J.G. et al. A prospective, open-label, randomized clinical trial to evaluate the efficacy and safety of remimazolam in patients undergoing EBUS-TBNA: REST trial design. BMC Pulm Med 24, 243 (2024). https://doi.org/10.1186/s12890-024-03067-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03067-w