Abstract
Background
The relationship between risk factors of common postoperative complications after pulmonary resection, such as air leakage, atelectasis, and arrhythmia, and patient characteristics, including nutritional status or perioperative factors, has not been sufficiently elucidated.
Methods
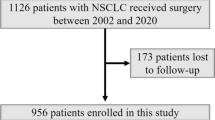
One thousand one hundred thirty-nine non-small cell lung cancer patients who underwent pulmonary resection were retrospectively analyzed for risk factors of common postoperative complications.
Results
In a multivariate analysis, male sex (P = 0.01), age ≥ 65 years (P < 0.01), coexistence of chronic obstructive pulmonary disease (COPD) (P < 0.01), upper lobe (P < 0.01), surgery time ≥ 155 min (P < 0.01), and presence of lymphatic invasion (P = 0.01) were significant factors for postoperative complication. Male sex (P < 0.01), age ≥ 65 years (P = 0.02), body mass index (BMI) < 21.68 (P < 0.01), coexistence of COPD (P = 0.02), and surgery time ≥ 155 min (P = 0.01) were significant factors for severe postoperative complication. Male sex (P = 0.01), BMI < 21.68 (P < 0.01), thoracoscopic surgery (P < 0.01), and surgery time ≥ 155 min (P < 0.01) were significant risk factors for postoperative air leakage. Coexistence of COPD (P = 0.01) and coexistence of asthma (P < 0.01) were significant risk factors for postoperative atelectasis. Prognostic nutrition index (PNI) < 45.52 (P < 0.01), lobectomy or extended resection more than lobectomy (P = 0.01), and surgery time ≥ 155 min (P < 0.01) were significant risk factors for postoperative arrhythmia.
Conclusion
Low BMI, thoracoscopic surgery, and longer surgery time were significant risk factors for postoperative air leakage. Coexistence of COPD and coexistence of asthma were significant risk factors for postoperative atelectasis. PNI, surgery time, and surgical procedure were revealed as risk factors of postoperative arrhythmia. Patients with these factors should be monitored for postoperative complication.
Trial registration
The Institutional Review Board of Kanazawa Medical University approved the protocol of this retrospective study (approval number: I392), and written informed consent was obtained from all patients.
Similar content being viewed by others
Background
The incidence of postoperative complications associated with pulmonary resection for non-small cell lung cancer (NSCLC) was reported to be 9–37% [1,2,3]. Furthermore, the incidence of postoperative complications associated with lobectomy was 10–50% and was higher in older patients [4]. Several postoperative complications might occur after pulmonary resection, and air leakage, pneumonia, atelectasis, and arrhythmia are considered common complications. In these reports, the incidence of postoperative pulmonary complications after pulmonary resection was 6–30%. Age, smoking history, and chronic obstructive pulmonary disease (COPD) are considered significant risk factors for postoperative pulmonary complications [5,6,7,8,9].
In our previous study, we reported that the coexistence of asthma, neutrophil-to-lymphocyte ratio (NLR), and pulmonary lobe were significant risk factors for postoperative complications [10]. Recently, low body mass index (BMI) and nutritional status, such as prognostic nutrition index (PNI), have been demonstrated as risk factors of postoperative pulmonary complications [11,12,13]. Furthermore, Charlson comorbidity index (CCI), surgical procedure, and surgery time were showed as risk factors of postoperative complications [14]. However, the relationship between risk factors of common postoperative complications, such as air leakage, atelectasis, and arrhythmia, after pulmonary resection and patient characteristics, including nutritional status, or perioperative factors have not been adequately elucidated.
In the present study, we retrospectively analyzed the risk factors of postoperative complications in NSCLC patients who underwent pulmonary resection, including risk factors of common postoperative complications.
Methods
Patients
One thousand one hundred thirty-nine NSCLC patients who underwent pulmonary resection at Kanazawa Medical University between January 2002 and December 2021 were enrolled in this retrospective study.
Data collected were sex, age, smoking history, BMI, comorbidity, CCI, carcinoembryonic antigen (CEA) levels, PNI, NLR, cancer inflammation prognostic index (CIPI), and pulmonary lobe involvement in lung cancer. Smoking history was assessed using the Brinkman Index, which is calculated by multiplying the number of cigarettes smoked per day by the number of years the subject has been smoking [15]. CCI was calculated by score according to the comorbidity grade [16]. Furthermore, comorbidity was divided into six categories: atrial fibrillation, pectoris angina, interstitial lung disease (ILD), COPD, asthma, and diabetes mellitus. PNI was calculated by combining serum albumin levels with the total peripheral lymphocyte count in peripheral blood [17]. NLR was defined as the ratio of neutrophil-to-lymphocyte count, and CIPI was calculated as CEA (ng/ml) × NLR [18, 19].
Surgical factors
Data collected were surgical approach, surgery time, and surgical procedure. The surgical approach was divided into three categories: robotic-assisted thoracic surgery (RATS), video-assisted thoracic surgery (VATS), and open thoracotomy. We decided to undertake RATS and VATS as the thoracoscopic surgery. The surgical procedure was divided into seven categories: wedge resection, segmentectomy, lobectomy, sleeve lobectomy, lobectomy combined with segmentectomy, lobectomy combined with chest wall resection, bilobectomy, and pneumonectomy.
Pathological factors
Data on lymphatic invasion, vascular invasion, differentiation, histological type, and pathological stage were collected.
Postoperative complications
Postoperative complications were categorized into five grades according to the Clavien–Dindo classification system: grade I, II, IIIa, IIIb, IVa, IVb, and V. The suffix “d” (for “disability”) was used to denote any postoperative impairment [20]. Severe complications were defined as grade IIIa or more. Furthermore, we also divided postoperative complications into nine categories for the multivariate analysis of risk factors: air leakage, arrhythmia, atelectasis, pneumonia, chylothorax, home oxygen therapy, cerebral infarction, empyema or pleuritis, and surgical site infection.
Statistical analyses
Qualitative variables are expressed as absolute numbers and percentages, and quantitative data are expressed as medians and ranges. The cutoff values for factors associated with postoperative complications were calculated using receiver operating characteristic (ROC) curve analysis, and risk analyses were performed using these cutoff values. The univariate and multivariate analysis of the risk factors for the postoperative complications, including severe postoperative complication and each postoperative complications, were performed by logistic regression analysis Multivariate analysis was performed for the factors that showed significant differences in univariate analysis. All statistical analyses were two-sided and statistical significance was set at P < 0.05. Statistical analyses were performed using JMP software v14 (SAS Institute Inc., Cary, NC, USA).
Results
Patients’ characteristics
The clinicopathological characteristics of the 1139 patients are shown in Table 1. There were 701 men, and the median age was 70.7 years. Median Brinkman Index was 600 and median BMI was 22.71. In total, 682 patients had comorbidities, including 28 patients with atrial fibrillation, 91 with angina pectoris, 41 with ILD, 399 with COPD, 38 with asthma, and 169 with diabetes mellitus. Median CEA concentration was 3.4 ng/ml, median PNI was 49.8, NLR was 2.22, and median CIPI was 7.92. The pulmonary lobes resected for NSCLC included the right upper lobe in 344 patients, right middle lobe in 69, right lower lobe in 271, left upper lobe in 267, and left lower lobe in 188.
Surgical factors
RATS was performed in 62 patients, VATS in 398, and open thoracotomy in 679. With regards to the surgical procedures, wedge resection was performed in 190 patients, segmentectomy in 115, lobectomy in 756, sleeve lobectomy in 8, lobectomy combined with segmentectomy in 8, lobectomy with chest wall resection in 13, bilobectomy in 20, and pneumonectomy in 29. The median surgery time was 169 min.
Pathological factors
The histological types were as follows: adenocarcinoma in 839 patients, squamous cell carcinoma in 224, large cell neuroendocrine carcinoma in 30, adenosquamous cell carcinoma in 17, pleomorphic carcinoma in 16, carcinoid in 7, and large-cell carcinoma in 6. Lymphatic invasion was present in 391 patients and vascular invasion in 491. Differentiation was categorized as G1 in 36 patients, G2 in 570, G3 in 168, and G4 in 35. The pathological stages were: stage 0 in 64 patients, IA in 605, IB in 202, IIA in 46, IIB in 112, IIIA in 94, IIIB in 4, IV in 8, yield to treatment (y) IA in 8, and yIIA in 1.
Postoperative complications
Postoperative complications were observed in 327 patients (28.7%). Clavien–Dindo grade I complications were noted in 2 patients, grade II in 129, grade IIIa in 183, grade IIIb in 12, and grade V in 1. Major postoperative complications included air leakage in 141 patients, arrhythmia in 64, pneumonia in 36, and atelectasis in 32. Minor postoperative complications were chylothorax in nine patients, home oxygen therapy in seven, cerebral infarction in six, empyema or pleuritis in six, surgical site infection in six, and broncho-pleural fistula in three.
Cutoff values calculated from ROC curves
The cutoff values of factors associated with postoperative complications were calculated by ROC curve analysis. The following cutoff values were determined: age, 65 years; BMI, 21.68; PNI, 45.52; CIPI, 7.25; CIPI, 14.59; and surgery time, 155 min.
Univariate and multivariate analyses
The relationship between patient characteristics and postoperative complications was analyzed (Table 2). The following were significant factors for postoperative complications in the univariate analysis: male sex (P < 0.01), age ≥ 65 years (P < 0.01), Brinkman index ≥ 600 (P < 0.01), coexistence of COPD (P < 0.01), PNI < 45.52 (P < 0.01), CIPI > 7.25 (P = 0.01), upper lobe (P < 0.01), lobectomy or extended resection more than lobectomy (P < 0.01), surgery time ≥ 155 min (P < 0.01), non-adenocarcinoma (P < 0.01), presence of lymphatic invasion (P < 0.01), presence of vascular invasion (P = 0.02), and presence of grade 3/4 differentiation (P < 0.01). Male sex (P = 0.01), age ≥ 65 years (P < 0.01), coexistence of COPD (P < 0.01), upper lobe (P < 0.01), surgery time ≥ 155 min (P < 0.01), and presence of lymphatic invasion (P = 0.01) were significant factors for postoperative complication in the multivariate analysis. The relationship between patient characteristics and severe postoperative complication was analyzed (Table 3). The following were significant factors for severe postoperative complication in the univariate analysis: male sex (P < 0.01), age ≥ 65 years (P = 0.04), Brinkman index ≥ 600 (P < 0.01), BMI < 21.68 (P < 0.01), coexistence of COPD (P < 0.01), CIPI > 7.25 (P < 0.01), lobectomy or extended resection more than lobectomy (P = 0.01), surgery time ≥ 155 min (P < 0.01), non-adenocarcinoma (P = 0.02), presence of lymphatic invasion (P = 0.01), and presence of grade 3/4 differentiation (P = 0.01). Male sex (P < 0.01), age ≥ 65 years (P = 0.02), BMI < 21.68 (P < 0.01), coexistence of COPD (P = 0.02), and surgery time ≥ 155 min (P = 0.01) were significant factors for severe postoperative complication in the multivariate analysis.
Risk factors of each postoperative complication
The significant risk factors of each postoperative complication by multivariate analysis are shown in Table 4. Male sex (P < 0.01), age ≥ 65 years (P = 0.03), Brinkman index ≥ 600 (P = 0.02), BMI < 21.68 (P < 0.01), coexistence of COPD (P < 0.01), CIPI > 7.25 (P = 0.01), thoracoscopic surgery (P = 0.01), and surgery time ≥ 155 min (P = 0.04) were significant risk factors for postoperative air leakage in the univariate analysis (data not shown). However, male sex (P = 0.01), BMI < 21.68 (P < 0.01), thoracoscopic surgery (P < 0.01), and surgery time ≥ 155 min (P < 0.01) were significant risk factors for postoperative air leakage in the multivariate analysis.
PNI < 45.52 (P < 0.01), thoracoscopic surgery (P = 0.01), lobectomy or extended resection more than lobectomy (P < 0.01), surgery time ≥ 155 min (P < 0.01), non-adenocarcinoma (P < 0.01), presence of lymphatic invasion (P = 0.03), presence of vascular invasion (P = 0.01), presence of grade 3/4 differentiation (P = 0.02), and pathological stage ≥ II (P = 0.03) were significant factors for postoperative arrhythmia in the univariate analysis (data not shown). In the multivariate analysis, PNI < 45.52 (P < 0.01), lobectomy or extended resection more than lobectomy (P = 0.01), and surgery time ≥ 155 min (P < 0.01) were significant risk factors for postoperative arrhythmia.
Coexistence of COPD (P < 0.01), coexistence of asthma (P < 0.01), and upper lobe (P = 0.04) were significant factors for postoperative atelectasis in the univariate analysis (data not shown). However, coexistence of COPD (P = 0.01) and coexistence of asthma (P < 0.01) were the only significant risk factors for postoperative atelectasis in the multivariate analysis.
While male sex (P < 0.01), Brinkman index ≥ 600 (P < 0.01), coexistence of COPD (P < 0.01), and non-adenocarcinoma (P = 0.03) were significant factors for postoperative pneumonia in the univariate analysis (data not shown), there were no significant risk factors for postoperative pneumonia in the multivariate analysis.
Although we analyzed the risk factors of chylothorax, home oxygen therapy, cerebral infarction, empyema or pleuritis and surgical site infection, significant risk factors could not be identified.
Discussion
We analyzed risk factors of postoperative complication for NSCLC patients who underwent pulmonary resection, including risk factors of common postoperative complications. Male sex, high age, coexistence of COPD, upper lobe, longer surgery time, and presence of lymphatic invasion were significant factors for postoperative complication. Furthermore, male sex, high age, low BMI, coexistence of COPD, and longer surgery time were significant factors for severe postoperative complication. Age, comorbidity, smoking history, surgical approach, and type of surgical procedure have previously been showed as risk factors for postoperative complication in NSCLC patients who have undergone pulmonary resection [4, 6, 7, 14, 21, 22]. In addition, upper lobe location and surgery time were revealed as risk factors for postoperative complication in this study. The pulmonary lobe of the tumor, including the right upper lobe, right lower lobe, and left upper lobe, was a significant risk factor for postoperative complication in our previous study [10]. Furthermore, longer surgery time has been reported as a risk factor of postoperative complication for lung cancer patients who underwent pulmonary lobectomy [23]. Male sex, high age, coexistence of COPD, and longer surgery time were revealed as risk factors of both postoperative complication and severe postoperative complication in this study; hence, patients with these factors should be especially monitored for postoperative complication, and the effort to shorten the surgery time should be important.
High age and low BMI have been demonstrated as risk factors of postoperative pulmonary complication [12, 13]. Male sex, low BMI, thoracoscopic surgery, and longer surgery time were significant risk factors for postoperative air leakage, and coexistence of COPD and coexistence of asthma were significant risk factors for postoperative atelectasis, while there was no significant risk factor of postoperative pneumonia identified in this study. In a previous study, male sex and thoracoscopic surgery were revealed as risk factors of postoperative air leakage, and the presence of asthma was showed as a risk factor of postoperative atelectasis or pneumonia [24]. Although risk factors of postoperative pneumonia were not revealed in current study, smoking status tended to be a risk factor of postoperative pneumonia and then the careful follow-up should be necessary.
Although surgical procedure has previously been reported as a risk factor of postoperative arrhythmia [24], PNI and surgery time, in addition to surgical procedure, were revealed as risk factors of postoperative arrhythmia in this study. Nutritional status has not been reported as a risk factor of postoperative arrhythmia for NSCLC patients who have undergone pulmonary resection, and further studies are needed. Longer surgery time might induce autonomic denervation and stress-mediated neurohumoral mechanisms resulting postoperative arrythmia. Surgical procedure, such as lobectomy or extended resection more than lobectomy, might induce a large load to the right heart system and cause arrhythmia by reducing pulmonary vasculature.
The utility of sublobar resection for early-stage NSCLC was recently revealed [25,26,27]. Although sublobar resection is associated with less postoperative complications than lobectomy in these reports, there were no significant differences in risk of postoperative complications among surgical procedures in this study. Postoperative complications by surgical procedures might be significant differences in patient populations such as the elderly or with emphysematous lungs, and the future studies should be needed.
Although chylothorax and cerebral infarction are crucial postoperative complications for NSCLC patients who have undergone pulmonary resection, it might be difficult to statistically determine the risk factors of these postoperative complications because of the small numbers of patients with such complications, as in this study.
This study had several limitations. First, it was a retrospective study, and it potentially involved unobserved cofounding and selection biases. Second, the study was performed at a single institution, and the study population was small. The small representation of atrial fibrillation or asthma or interstitial lung disease in this study might be limited the effect to risk on postoperative complications including postoperative severe complications and each postoperative complication. Third, the possibility cannot be ruled out that there were cases that were not included in this study due to insufficient data, resulting in selection bias.
Conclusions
We analyzed risk factors of postoperative complication for NSCLC patients who underwent pulmonary resection, including risk factors of common postoperative complications. Male sex, high age, coexistence of COPD, and longer surgery time were revealed as risk factors of both postoperative complication and severe postoperative complication in this study. For each postoperative complication, male sex, low BMI, thoracoscopic surgery, and longer surgery time were significant risk factors for postoperative air leakage, while coexistence of COPD and coexistence of asthma were significant risk factors for postoperative atelectasis, and PNI, surgery time, and surgical procedure were revealed as risk factors of postoperative arrhythmia. There was no significant risk factor of postoperative pneumonia. Patients with these factors should be carefully monitored for each postoperative complication.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to [our institutional restrictions e.g., them containing information that could compromise research participant privacy/consent], but are available from the corresponding author on reasonable request.
Abbreviations
- NSCLC:
-
Non-small cell lung cancer
- COPD:
-
Chronic obstructive pulmonary disease
- NLR:
-
Neutrophil-to-lymphocyte ratio
- BMI:
-
Body mass index
- PNI:
-
Prognostic nutrition index
- CCI:
-
Charlson comorbidity index
- CEA:
-
Carcinoembryonic antigen
- CIPI:
-
Cancer inflammation prognostic index
- ILD:
-
Interstitial lung disease
- RATS:
-
Robotic-assisted thoracic surgery
- VATS:
-
Video-assisted thoracic surgery
- ROC:
-
Receiver operating characteristic
References
Rueth NM, Andrade RS. IS VATS lobectomy better: perioperatively, biologically and oncologically? Ann Thorac Surg. 2010;89:S2107–11.
Boffa DJ, Allen MS, Grab JD, Gaissert HA, Harpole DH, Wright CD. Data from the Society of thoracic surgeons General thoracic surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg. 2008;135:247–54.
Allen MS, Darling GE, Pechet TTV, Mitchell JD, Herndon IIJE, Landreneau RJ, et al. Morbidity and mortality of major pulmonary resections in patients with early-stage lung cancer: initial results of the randomized, prospective ACOSOG Z0030 trial. Ann Thoac Surg. 2006;81:1013–20.
Berry MF, Hanna J, Tong BC, Burfeind WR, Harpole DH, D’Amico TA, et al. Risk factors for morbidity after lobectomy for lung cancer in eldery patients. Ann Thorac Surg. 2009;88:1093–9.
Jung R, He S, Dai H, lin F, Ge W, Tao G, et al. Incidence and risk factors of postoperative pulmonary complications after thoracic surgery for early non-small cell lung cancer. Int j Clin Exp Med. 2018;11(1):285–94.
Agostini P, Lugg ST, Adams K, Smith T, Kalkat MS, Rajesh PB, et al. Risk factors and short-term outcomes of postoperative pulmonary complications after VATS lobectomy. J Cardiothorac Surg. 2018;13:28.
Lee JY, Jin SM, Lee CH, Lee BJ, Kang CH, Yim JJ, et al. Risk factors of postoperative pneumonia after lung cancer surgery. J Korean Med Sci. 2011;26:979–84.
Agostini P, Cieslik H, Rathinam S, Bishay E, Kalkat MS, Rajesh PB, et al. Postoperative pulmonary complications following thoracic surgery: are there any modifiable risk factors? Thorax. 2010;65:815–8.
Stolz AJ, Schutzner J, Lischke R, Simonek J, Harustiak T, Pafko P. Predictors of atelectasis after pulmonary lobectomy. Surg Today. 2008;38:987–92.
Motono N, Ishikawa M, Iwai S, Yamagata A, Iijima Y, Uramoto H. Analysis of risk factors for postoperative complications in non-small cell lung cancer: comparison with the Japanese National Clinical Database risk calculator. BMC Surg. 2022;22:180.
Park S, Joo H, Yang M, Kim JA, Kim JK, Park SJ. The prognostic nutritional index and postoperative complications after curative lung cancer resection: a retrospective cohort study. J Thorac Cardiovasc Surg. 2020;160:276–85.
Lee SC, Lee JG, Lee SH, Kim EY, Chang J, Kim DJ, et al. Prediction of postoperative pulmonary complications using preoperative controlling nutritional status (CONUT) score in patients with resectable non-small cell lung cancer. Sci Rep. 2020;10:12385.
Benker M, Citak N, Neuer T, Opitz I, Inci I. Impact of preoperative comorbidities on postoperative complication rate and outcome in surgically resected non-small cell lung cancer patients. Gen Thorac Cardiovasc Surg. 2022;70:248–56.
Pei G, Zhou S, Han Y, Liu Z, Xu S. Risk factors for postoperative complications after lung resection for non-small cell lung cancer in elderly patients at a single institution in China. J Thorac Dis. 2014;6:1230–8.
Brinkman GL, Coates EO. The effect of bronchitis, smoking, and occupation on ventilation. Am Rev Respir Dis 1963;87: 684 – 93.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Choric Dis. 1987;40:373–83.
Qiu C, Qu X, Shen X, Zheng C, Zhu L, Meng L, et al. Evaluation of Prognostic Nutritional Index in patients undergoing radical surgery with Nonsmall Cell Lung Cancer. Nutr Cancer. 2015;67:741–7.
Zahorec R. Ratio of neutrophil to lymphocyte counts - rapid and simple parameter of systemic inflammation and stress in critically ill. Bratisl Lek Listy. 2001;102:5–14.
You JF, Hsu YJ, Chern YJ, Cheng CC, Jong BK, Liao CK, et al. Preoperative cancer inflammation prognostic index as a superior predictor of short- and long-term outcomes in patients with stage I-III colorectal cancer after curative surgery. Cancers. 2022;14:6232.
Katayama H, Kurokawa Y, Nakamura K, Ito H, Kanemitsu Y, Masuda N, et al. Extended Clavien-Dindo classifcation of surgical complications: Japan Clinical Oncology Group postoperative complications criteria. Surg Today. 2016;46:668–85.
Kozower BD, Sheng S, O’Brien SM, Liptay MJ, Lau CL, Jones DR, et al. STS database risk models: predictors of mortality and major morbidity for lung cancer resection. Ann Thorac Surg. 2010;90:875–83.
Yang R, Wu Y, Yao L, Xu J, Zhang S, Du C, et al. Risk factors of postoperative pulmonary complications after minimally invasive anatomic resection for lung cancer. Ther Clin Risk Manag. 2019;15:223–31.
Angelis P, Tan KS, Chudgar NP, Dycoco J, Adusumilli PS, Bains MS, et al. Operative time is associated with postoperative complications after pulmonary lobectomy. Ann Surg. 2023;278:e1259–1266.
Motono N, Ishikawa M, Iwai S, Yamagata A, Iijima Y, Uramoto H. Individualization of risk factors for postoperative complication after lung cancer surgery: a retrospective study. BMC Surg. 2021;21:311.
Saji H, Okada M, Tsuboi M, Nakajima R, Suzuki K, Aokage K, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (JCOG0802/WJOG4607L): a multicentre, open-label, phase 3, randomized, controlled, non-inferior trial. Lancet. 2022;399:1607–17.
Tsutani Y, Tsubokawa N, Ito M, Misumi K, Hanaki H, Miyata Y, et al. Postoperative complications and prognosis after lobar resection versus sublobar resection in elderly patients with clinical stage I non-small-cell lung cancer. Eur J Cardiothorac Surg. 2018;53:366–71.
Miura K, Ide S, Minamisawa M, Mishima S, Matsuoka S, Eguchi T, et al. Sublobar resection or lobectomy and postoperative respiratory complications in emphysematous lungs. Eur J Cardiothorac Surg. 2024;65:ezae061.
Acknowledgements
We thank H. Nikki March, PhD, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Funding
This study has not been funded.
Author information
Authors and Affiliations
Contributions
N. M. performed the research, collected and analyzed the data and wrote the paper. T.M., M.I., S. I., and Y.I. contributed to sample collection. H. U. contributed to supervision of this study and revision of the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The present study was conducted in accordance with the amended Declaration of Helsinki. The Institutional Review Boards of Kanazawa Medical University approved the protocol (approval number: I392), and written informed consent was obtained from all of the patients.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Motono, N., Mizoguchi, T., Ishikawa, M. et al. Analysis of risk factors of postoperative complication for non-small cell lung cancer. BMC Pulm Med 24, 333 (2024). https://doi.org/10.1186/s12890-024-03054-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03054-1