Abstract
Background
Patients with congenital myopathies may experience respiratory involvement, resulting in restrictive ventilatory dysfunction and respiratory failure. Pulmonary hypertension (PH) associated with this condition has never been reported in congenital ryanodine receptor type 1(RYR1)-related myopathy.
Case presentation
A 47-year-old woman was admitted with progressively exacerbated chest tightness and difficulty in neck flexion. She was born prematurely at week 28. Her bilateral lower extremities were edematous and muscle strength was grade IV−. Arterial blood gas analysis revealed hypoventilation syndrome and type II respiratory failure, while lung function test showed restrictive ventilation dysfunction, which were both worse in the supine position. PH was confirmed by right heart catheterization (RHC), without evidence of left heart disease, congenital heart disease, or pulmonary artery obstruction. Polysomnography indicated nocturnal hypoventilation. The ultrasound revealed reduced mobility of bilateral diaphragm. The level of creatine kinase was mildly elevated. Magnetic resonance imaging showed myositis of bilateral thigh muscle. Muscle biopsy of the left biceps brachii suggested muscle malnutrition and congenital muscle disease. Gene testing revealed a missense mutation in the RYR1 gene (exon33 c.C4816T). Finally, she was diagnosed with RYR1-related myopathy and received long-term non-invasive ventilation (NIV) treatment. Her symptoms and cardiopulmonary function have been greatly improved after 10 months.
Conclusions
We report a case of RYR1-related myopathy exhibiting hypoventilation syndrome, type II respiratory failure and PH associated with restrictive ventilator dysfunction. Pulmonologists should keep congenital myopathies in mind in the differential diagnosis of type II respiratory failure, especially in patients with short stature and muscle weakness.
Similar content being viewed by others
Background
Congenital myopathies, a group of rare inherited muscle diseases characterized by abnormalities in the structure of muscle fibers, vary in their clinical presentation, histopathology, and genetic causes [1]. Common clinical features of congenital myopathies include dysmorphic facial features secondary to muscle weakness, abnormal extrinsic eye movements, spinal malformation, malignant hyperthermia, and cardiac or respiratory involvement [1, 2]. Respiratory failure with or without hypercapnia may occur when the diaphragm and other respiratory muscles are affected, resulting in serious complications or even death [2,3,4]. However, congenital myopathies can be easily misdiagnosed in clinical practice. The main histopathological types of those with respiratory insufficiency include core myopathy, myotubular myopathy, autosomal centronuclear myopathy, congenital fiber-type disproportion myopathy, and myosin storage myopathy [2, 3]. Common genes associated with respiratory involvement include α-skeletal actin (ACTA1), nebulin (NEB), selenoprotein 1 (SEPN1), slow α-tropomyosin (TPM3), and ryanodine receptor type 1 (RYR1) [1].
Pulmonary hypertension (PH) is a pathophysiological disorder defined by a mean pulmonary arterial pressure (mPAP) > 20 mmHg at rest according to the latest guidelines. PH is divided into five groups based on etiology including chronic respiratory diseases and/or hypoxia [5]. Some patients may experience hypoventilation syndrome and exhibit hypoxemia with or without hypercapnia, which is defined as type II or type I respiratory failure, respectively. One of the causes of hypoventilation is restrictive lung diseases, a common manifestation of congenital myopathies affecting the respiratory muscles [3]. RYR1-related myopathies are the most prevalent group of congenital myopathies and have multiple clinical phenotypes, such as symmetric proximal muscle weakness, significant respiratory involvement, King Denborough syndrome, arrhythmias, malignant hyperthermia and so on [6,7,8]. Up to now, PH has never been reported in cases of congenital RYR1-related myopathy, which should be considered as a potential indirect cause in the differential diagnosis of respiratory dysfunction.
Here we report a female patient with RYR1-related myopathy who exhibited type II respiratory failure and PH associated with restrictive ventilatory dysfunction.
Case presentation
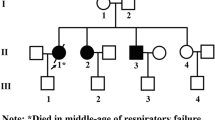
A 47-year-old woman was admitted to our hospital with progressively exacerbated chest tightness after activity and echocardiographic suspicion of PH. Her body weight was 50 kg with the height of 150 cm. She was born prematurely at week 28. The patient had no similar family history, but her younger brother was also small and slight in stature. Her chest computed tomography (CT) five years ago showed no significant abnormalities. Four months before this admission, she experienced aggravating dyspnea. Lung function test indicated severe restrictive ventilation dysfunction and reduced diffusion capacity [forced expiratory volume in one second (FEV1) 36%pred, forced vital capacity (FVC) 34%pred, FEV1/FVC 111%, single-breath carbon monoxide diffusing capacity of the lungs (DLCO SB) 47%pred] (Table 1). Re-performed chest CT showed linear opacities, consolidation and nodules. Echocardiography was unavailable at that time. After antibiotics treatment, the symptom of dyspnea was improved while edema in both lower limbs gradually appeared. Meanwhile, she was diagnosed with hypertension (180/100 mmHg at highest) and received antihypertensive agents. Echocardiography two months ago showed mitral and tricuspid regurgitation, which may indicate underlying PH without obvious changes in the structure of the heart. Venous thromboembolism was excluded after CT pulmonary angiography and ultrasonography of the lower extremity veins. However, she had an enlarged main pulmonary artery of 34 mm in diameter. Symptomatic and supportive treatment did not bring significant improvement. One month ago, she was hospitalized again due to aggravated symptoms. The echocardiography indicated massive tricuspid regurgitation, mild right cardiac enlargement and suspicion of PH with an estimated pulmonary arterial systolic pressure (sPAP) of 76 mmHg, lack of signs of left heart disease. Arterial blood gas analysis (ABG) showed a partial pressure of carbon dioxide (PaCO2) of 60 mmHg and a partial pressure of oxygen (PaO2) of 57 mmHg. She received antibiotics, expectorants, bronchodilator and symptomatic treatment. The edema reduced but the chest tightness did not show significant improvement.
On admission, the patient presented with cyanosis and difficulty in neck flexion. She was afebrile, with a respiratory rate of 20 breaths per minute and a blood pressure of 122/75 mmHg. Heart rate was 109 beats per minute with a loud pulmonic component of the second heart sound. Her bilateral lower extremities were moderately edematous and muscle strength was mildly decreased in grade IV−, which defined as being able to engage in activities against light resistance. The admission electrocardiogram showed sinus tachycardia, right axis deviation, and negative T waves in leads V1-V3. The patient presented with hypoventilation, type II respiratory failure and a special phenomenon of hypoxia in the supine position. ABG while breathing room air revealed a PaO2 of 38 mmHg in the supine position, but 52 mmHg in the sitting position (Table 1). Lung function test indicated that the residual volume of single breath (RV-SB) was 1.42 L and total lung capacity of single breath (TLC-SB) was 2.39 L. The DLCO/alveolar ventilation (VA) was 1.45 mmol/min/kPa/L, which was 82.4% of the predicted value. Supine FEV1, FVC, FEV1/FVC ratio and the percentage they occupied of the predicted value measurements were all lower than the sitting measurements (Table 1). Lower extremity ultrasound and echocardiography were repeated with similar results to previous examinations. D-dimer in plasma was 1.23 mg/L. Ventilation-perfusion scan was performed and excluded pulmonary embolism, while the simultaneous chest CT indicated scattered patchy and linear shadows in bilateral lungs, and an elevation of the right diaphragm (Fig. 1). RHC indicated that the mPAP was 38 mmHg, pulmonary arterial wedge pressure was 7 mmHg, cardiac output was 4.99 L/min, and pulmonary vascular resistance was 6.21 Wood’s Unit. It revealed severe precapillary pulmonary hypertension, and concurrent acute vasoreactivity testing was negative. Advanced right heart contrast echocardiography showed no shunts. It was less likely to be PH associated with left heart disease, congenital heart disease, or chronic pulmonary artery obstruction. The cause of PH was more likely chronic lung diseases and/or hypoxia. Combining the supine hypoxia phenomenon and restrictive ventilation dysfunction, diaphragmatic ultrasound examination was performed and then revealed reduced mobility of bilateral diaphragm. Specifically, the left diaphragm showed an excursion of 1.0 cm both during quiet breathing and at maximum inspiration, with a diaphragmatic thickening fraction of 26%. On the right side, the diaphragm had an excursion of 1.7 cm during quiet breathing and 1.8 cm at maximum inspiration, with a diaphragmatic thickening fraction of 14%. The red blood cell count, hemoglobin and hematocrit on admission were 5.71 × 1012/L, 109 g/L and 44.2%, respectively. In conjunction with anemia-related testing, iron-deficiency anemia was considered and treated. Polysomnography indicated that the patient experienced hypoventilation during nocturnal sleep, with a hypopnea index of 119.6 times per hour. The longest duration of hypopnea lasted 63 s, and the average blood oxygen saturation (SO2) during sleep was only 73% (Table 1). Hypoventilation syndrome was definitively diagnosed.
Chest computed tomography of the patient. A-C lung window; D-I mediastinal window. Chest computed tomography on admission indicated scattered patchy and linear shadows in bilateral lungs. An elevation of the right diaphragm can be seen in Fig. C, F and G. Figure H and I showed the sagittal views of the right and left diaphragm at the same level, respectively
Except for weak positive for anti-TIF1γ antibody and antinuclear antibody (1:80), other immune-related antibody spectra were negative. The creatine kinase (CK) was mildly elevated with a value of 394 U/L. Magnetic resonance imaging (MRI) showed bilateral thigh muscle changed consistent with myositis (Fig. 2). According to the consultation of the rheumatologist, the muscle biopsy was performed on the left biceps brachii and revealed the pathological features of central core disease (Fig. 3).
Thigh magnetic resonance imaging of the patient. Magnetic resonance imaging showed bilateral thigh muscle changed consistent with myositis (multiple muscle atrophy and patchy slighted high signal in fat saturated sequence) mainly involved the adductor magnus and sartorius (arrows). A T1-weighted non-fat saturated coronal image; B T2-weighted non-fat saturated coronal image; C synthetic T2-weighted non-fat saturated axial image; D synthetic T2-weighted fat saturated axial image
The pathological features of patient with RYR1 gene mutation. A and B. H&E and MGT staining × 10: the central core of muscle fiber light stained with surrounded by purple circle; C and D PAS and ORO staining × 10: no accumulation of glycogen and lipid in muscle fibers; E and F. NADH-TR and COX staining × 10: the deficiency or light staining of NADH-TR and cytochrome C oxidase in centrally located of muscle fibers
Thus, we conducted genetic susceptibility gene whole exome sequencing, using the blood sample. The sequencing revealed a missense mutation in the RYR1 gene (exon33 c.C4816T), which was associated with congenital myopathies. Taking all factors into consideration, the patient was diagnosed with RYR1-related myopathy. We initiated non-invasive ventilation (NIV) therapy (Spontaneous-Timed mode, inspiratory positive airway pressure was 14cmH2O, expiratory positive airway pressure was 4cmH2O, respiratory rate was 14 breaths per minute) to improve her ventilation, while closely monitoring her symptoms, breathing pattern and SO2. We used an in-laboratory overnight polysomnogram to titrate NIV in this patient. An oral-nasal mask was chosen for NIV. After regularly using non-invasive positive pressure ventilation at night, her chest tightness and cough significantly improved, so did her exercise tolerance and heart function. In addition to oral diuretics and long-term NIV therapy, we recommended home rehabilitation exercises upon discharge.
After 10 months, she no longer experienced chest tightness or shortness of breath and her muscle strength was better. ABG while breathing room air indicated a higher PaO2 of 68 mmHg and a lower PaCO2 of 52 mmHg in the supine position. The lung function test suggested an improvement in ventilation function compared to before (Table 1). Repeated echocardiography showed mild tricuspid regurgitation, with a sPAP of 32 mmHg. The red blood cell count, hemoglobin and hematocrit were 4.00 × 1012/L, 121 g/L and 36.6%, respectively. Repeated polysomnography indicated improved hypoventilation during nocturnal sleep, with a hypopnea index of only 1.2 times per hour. The longest duration of hypopnea decreased to 51 s, and the average SO2 during sleep rose to 96%. We recommended the patient to continue home NIV treatment and rehabilitation, and have regular outpatient follow-up visits.
Discussion and conclusion
To our knowledge, this is the first report describing a case with RYR1-related myopathy presented with hypoventilation syndrome, type II respiratory failure, and PH associated with restrictive ventilator dysfunction. Respiratory muscles, especially the diaphragm, were involved in the congenital myopathy caused by missense mutation in the RYR1 gene. It impaired the patient's ventilation function and caused hypoventilation syndrome, leading to chronic hypoxemia and hypercapnia, which processed to respiratory failure and resulted in the development of PH eventually.
As for the differential diagnosis process of PH, her medical history, echocardiography and RHC indicated low possibility of PH associated with left or congenital heart disease. The D-dimer test is widely recognized as a valuable biomarker that can rule out venous thromboembolism without the need for costly and time-consuming imaging tests. An approximately fourfold increase in the normal cut-off value of D-dimer in the plasma is associated with a significantly higher risk of pulmonary embolism [9]. This patient had a mild elevated D-dimer and further ventilation-perfusion scan ruled out pulmonary embolism. Meanwhile, her lung function test indicated restrictive ventilation dysfunction. The polysomnography indicated hypoventilation syndrome, while ABG revealed hypercapnia and hypoxemia. There was no evidence for connective tissue disease, HIV infection, portal hypertension or any other possible diseases leading to PH. Thus, we considered that PH was associated with hypoventilation in this patient, which was caused by respiratory muscle dysfunction resulting from myopathy.
PH due to hypoventilation is usually seen in sleep-related breathing disorders [10, 11]. Patients with sleep-related hypoventilation syndromes are often accompanied by hypercapnia and hypoxemia, about half of whom also present with PH and their functional impairment can be improved by NIV [10,11,12]. Hypoxic and hypercapnic vasoconstriction may play an important pathological role in the reversibility of PH. Meanwhile, sympathetic activation and the elevated viscosity of the blood could also increase the pulmonary vascular resistance, leading to an increase in pulmonary artery pressure [10, 11]. Experiments in rats also found that the PH and increased hematocrit linked to sleep-disordered breathing were a result of chronic intermittent hypercapnic hypoxia [13]. Similar mechanisms may be potentially involved in the development of PH in this patient. Her polysomnography indicated hypoventilation syndrome and ABG revealed hypercapnia and hypoxemia, secondary pulmonary vasoconstriction may explain her reversible PH after NIV. In addition, her follow-up blood routine test showed a decrease in red blood cell count and hematocrit, which may indicate the reduced blood viscosity indirectly. NIV improved her hypoventilation, ultimately improving her cardiopulmonary function.
Congenital myopathies describe a collection of diseases that vary in clinical, histological, and genetic characteristics, primarily impacting muscles. Clinical features, muscle imaging and biopsy, and genetic testing are necessary in the diagnosis [1,2,3]. The pathogenic genes mainly include dynamin 2 (DNM2), myotubularin (MTM1), ACTA1, slow skeletal β-cardiac myosin (MYH7), titin (TTN), NEB, SEPN1, β-tropomyosin (TPM2), TPM3, amphiphysin 2 (BIN1) and RYR1 [1, 2]. Hypotonia and muscle weakness are the main clinical features [2]. Meanwhile, approximately 64.1% of the individuals exhibited varying degrees of respiratory impairment, with about half of them necessitating nocturnal NIV as a result of respiratory failure [4]. Since diaphragm weakness is one of the main features of myopathy, evaluating diaphragmatic dysfunction is of great importance in these patients. Ultrasonography is a quick and simple method that can be done at the bedside, which showed a strong relationship with the standard respiratory tests commonly used in clinical settings [14]. In the differential diagnosis of respiratory failure, the clinician should pay attention to the patient's medical history and clinical manifestations not only limit to respiratory system, without overlooking some rare but possible causes. Meanwhile, critical examinations such as diaphragmatic ultrasound should be considered in the diagnostic process. Reports of PH indirectly caused by congenital myopathies are relatively rare. PH impacts the quality of life for patients and can be fatal in some circumstances. Therefore, the etiological treatment is crucial for improving the prognosis [5].
Notably, in addition to congenital myopathies, certain diseases can also present with muscle weakness. The differential diagnosis includes neurologic, rheumatologic, endocrine, genetic, medication- or toxin-related, and infectious etiologies [15, 16]. Different neurologic causes can manifest as signs of involvement of either upper or lower motor neurons, or both, with variable patterns of onset and involvement of muscles [15,16,17,18]. Creatine kinase levels are generally normal and do not necessitate a muscle biopsy. Weakness caused by inflammatory muscle diseases, with acute or subacute course, mainly affects the proximal muscles. Creatine kinase levels can be moderately or severely elevated, and muscle biopsies commonly show inflammatory infiltration. Patients often experience skin rashes, dysphagia, or other indications of immune system involvement [15, 16, 19]. Endocrine etiologies mainly include adrenal insufficiency, hyperthyroidism, hypothyroidism, Cushing's syndrome and secondary hyperparathyroidism. They also mainly involve the proximal muscles and are accompanied by manifestations of the primary disease [15, 16, 20]. When patients have a history of exposure to drugs (e.g. fluoroquinolones, glucocorticoids, or statins), toxins (e.g. heavy metals, alcohol, or certain recreational drugs), or infections (e.g. viruses or parasites), muscle weakness should be considered as possibly related to these factors after excluding other possible reasons [16, 21,22,23]. As for genetic causes, most diseases primarily involve proximal muscles. Their patterns of onset often progress gradually. Patients usually have congenital abnormalities in other organs, like the brain, heart, ocular region, skeletal system and so on. Creatine kinase levels are variable, while muscle biopsies often indicate nonspecific myopathic changes, mainly including muscle fiber atrophy, degeneration, and regeneration [15, 16]. When patients exhibit the aforementioned characteristics, it is necessary to consider the possibility of genetic etiologies and to perform genetic testing.
RYR1-related myopathy is acknowledged as the most common core myopathy among the congenital myopathies and linked to a broad spectrum of diseases [6, 24]. Although fatigue and weakness were key symptoms of interest among participants with RYR1-related myopathy, 2.4% of patients also reported respiratory difficulties [25]. A retrospective cross-sectional study also revealed that 6.8% of patients with RYR1-related myopathy had neonatal respiratory involvement and required nocturnal NIV therapy [4]. Muscle biopsy is crucial for diagnosis. Its primary histological subtypes encompass central core disease, multiminicore disease, core-rod myopathy, centronuclear myopathy, and congenital fiber-type disproportion. Regardless of the pathological type, there will be varying degrees of impact of respiratory function, resulting in pulmonary-related complications [6, 26]. A recent study summarized the respiratory features of centronuclear myopathy included RYR1-mutated individuals, and found that supine respiratory function measurements of patients were overall lower than sitting measurements [27]. The present case experienced aggravating dyspnea, hypoxia and worse respiratory function in supine position, and hypoventilation during sleep, which were consistent with the characteristics of the disease. Other suggestive clinical features include muscle weakness, hypotonia, myalgia, ophthalmoplegia, bulbar involvement, dysphagia, orthopedic deformities and malignant hyperthermia [6, 24]. The levels of serum CK are often normal or only mildly elevated [2, 7]. When patients exhibit the above characteristics, pulmonologists should consider the possibility of congenital myopathy.
In addition to clinical and histopathologic features, imaging examinations also have diagnostic significance. RYR1-related myopathy mainly involves muscle atrophy and intramuscular fatty infiltration [6, 28]. Muscle MRI or ultrasound can detect the patterns of muscle involvement or preservation, while the former is more commonly used and accurate in clinical practice [2, 6, 7]. The mainly involved muscles in the lower limbs include adductor magnus, sartorius, vastus lateralis, vastus intermedius, and vastus medialis, while the rectus femoris, adductor longus, and gracilis are not significantly affected [6]. An effective modified T1-weighted MRI-based algorithm has been proposed to identify and quantify fatty infiltration in patients with RYR1-related myopathy [28]. Electromyography (EMG) is less useful in diagnosis given that it can either show normal results or indicate findings similar to myopathy or other neuromuscular disorders in most cases [2]. Thigh MRI of this patient indicated irregular morphology of the bilateral muscles, multiple muscle atrophy, multiple patchy slighted high signals in fat saturated sequence, and blurred fat gaps between muscles. The main muscles involved were the adductor magnus and sartorius, while the adductor longus and gracilis were relatively spared, which consistent with the pattern of muscle involvement and preservation in RYR1-related myopathy. Gene testing contributes to the determination of diagnosis and the technology of next-generation sequencing (NGS) makes it more efficient and convenient to use in clinical settings [2, 6].
Main therapies being developed for RYR1-related myopathy include drugs that counteract the harmful effects of stress on the cellular environment and the modifications of RYR1 after protein synthesis, and drugs that directly target RYR1 or regulate the proteins that influence its functionality [6, 29,30,31]. Further randomized controlled trials are needed to determine approved therapeutic medications. Moreover, patients with congenital myopathies who presented with nocturnal hypoventilation can benefited from NIV [1,2,3]. At the same time, we should pay attention to the fact that the presence of sialorrhea and neurobehavioral impairment, and absence of respiratory symptoms can affect negatively of NIV adaptation [32].
There are also some limitations of this report. The patient refused to undergo a follow-up RHC. Thus, we cannot obtain a complete comparison of her hemodynamic parameters after treatment. However, other non-invasive evaluations, such as echocardiography, indeed revealed an improvement in her cardiopulmonary function. Additionally, the underlying mechanisms of PH in this patient cannot be confirmed, further animal experiments will be needed to validate current hypotheses in the future.
In conclusion, we report the first case with RYR1-related myopathy who exhibited hypoventilation syndrome, type II respiratory failure, and PH associated with restrictive ventilator dysfunction to the best of our knowledge. When patients exhibit characteristics of muscle weakness, pulmonologists should consider the possibility of myopathies including congenital myopathies. Imaging examinations, muscle biopsy and genetic testing are useful in the differential diagnosis. Meanwhile, attention should be paid to PH related to hypoventilation in clinical practice. NIV is effective and well tolerated in these patients.
Availability of data and materials
The data that support this case report are available from the corresponding author on reasonable request.
Abbreviations
- RYR1 :
-
Ryanodine receptor type 1
- PH:
-
Pulmonary hypertension
- RHC:
-
Right heart catheterization
- NIV:
-
Non-invasive ventilation
- ACTA1 :
-
α-skeletal actin
- NEB :
-
Nebulin
- SEPN1 :
-
Selenoprotein 1
- TPM3 :
-
Slow α-tropomyosin
- mPAP:
-
Mean pulmonary arterial pressure
- CT:
-
Computed tomography
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- RV-SB:
-
Residual volume of single breath
- TLC-SB:
-
Total lung capacity of single breath
- DLCO SB:
-
Single-breath carbon monoxide diffusing capacity of the lungs
- VA:
-
Alveolar ventilation
- sPAP:
-
Pulmonary arterial systolic pressure
- PaCO2 :
-
Partial pressure of carbon dioxide in arterial blood
- PaO2 :
-
Partial pressure of oxygen in arterial blood
- SO2 :
-
Blood oxygen saturation
- FiO2 :
-
Fraction of inspiration oxygen
- PFR:
-
PaO2/FiO2 ratio
- ABG:
-
Arterial blood gas analysis
- SO2 :
-
Blood oxygen saturation
- CK:
-
Creatine kinase
- MRI:
-
Magnetic resonance imaging
- DNM2 :
-
Dynamin 2
- MTM1 :
-
Myotubularin
- MYH7 :
-
Slow skeletal β-cardiac myosin
- TTN :
-
Titin
- TPM2 :
-
β-Tropomyosin
- BIN1 :
-
Amphiphysin 2
- EMG:
-
Electromyography
- NGS:
-
Next-generation sequencing
References
Claeys KG. Congenital myopathies: an update. Dev Med Child Neurol. 2019;62(3):297–302. https://doi.org/10.1111/dmcn.14365.
Cassandrini D, Trovato R, Rubegni A, Lenzi S, Fiorillo C, Baldacci J, Minetti C, Astrea G, Bruno C, Santorelli FM. Congenital myopathies: clinical phenotypes and new diagnostic tools. Ital J Pediatr. 2017;43(1):101. https://doi.org/10.1186/s13052-017-0419-z.
Gilbreath HR, Castro D, Iannaccone ST. Congenital Myopathies and Muscular Dystrophies. Neurol Clin. 2014;32(3):689–703. https://doi.org/10.1016/j.ncl.2014.04.006.
Colombo I, Scoto M, Manzur AY, Robb SA, Maggi L, Gowda V, Cullup T, Yau M, Phadke R, Sewry C, et al. Congenital myopathies: Natural history of a large pediatric cohort. Neurology. 2015;84(1):28–35. https://doi.org/10.1212/WNL.0000000000001110.
Humbert M, Kovacs G, Hoeper MM, Badagliacca R, Berger RMF, Brida M, Carlsen J, Coats AJS, Escribano-Subias P, Ferrari P, et al. 2022 ESC/ERS Guidelines for the diagnosis and treatment of pulmonary hypertension. Eur Heart J. 2022;43(38):3618–731. https://doi.org/10.1093/eurheartj/ehac237.
Lawal TA, Todd JJ, Meilleur KG. Ryanodine Receptor 1-Related Myopathies: Diagnostic and Therapeutic Approaches. Neurotherapeutics. 2018;15(4):885–99. https://doi.org/10.1007/s13311-018-00677-1.
Zhou H, Jungbluth H, Sewry CA, Feng L, Bertini E, Bushby K, Straub V, Roper H, Rose MR, Brockington M, et al. Molecular mechanisms and phenotypic variation in RYR1-related congenital myopathies. Brain. 2007;130(8):2024–36. https://doi.org/10.1093/brain/awm096.
Hayakawa I, Abe Y, Ono H, Kubota M. Severe congenital RYR1-associated myopathy complicated with atrial tachycardia and sinus node dysfunction: a case report. Ital J Pediatr. 2019;45(1):165. https://doi.org/10.1186/s13052-019-0756-1.
Sikora-Skrabaka M, Skrabaka D, Ruggeri P, Caramori G, Skoczyński S, Barczyk A. D-dimer value in the diagnosis of pulmonary embolism—may it exclude only? J Thorac Dis. 2019;11(3):664–72. https://doi.org/10.21037/jtd.2019.02.88.
Naeije R. Pulmonary hypertension in hypoventilation syndromes. Eur Respir J. 2013;43(1):12–5. https://doi.org/10.1183/09031936.00185213.
Adir Y, Humbert M, Chaouat A. Sleep-related breathing disorders and pulmonary hypertension. Eur Respir J. 2021;57(1):2002258. https://doi.org/10.1183/13993003.02258-2020.
Held M, Walthelm J, Baron S, Roth C, Jany B. Functional impact of pulmonary hypertension due to hypoventilation and changes under noninvasive ventilation. Eur Respir J. 2013;43(1):156–65. https://doi.org/10.1183/09031936.00147712.
McGuire M, Bradford A. Chronic intermittent hypercapnic hypoxia increases pulmonary arterial pressure and haematocrit in rats. Eur Respir J. 2001;18(2):279–85.
Ruggeri P, Lo Monaco L, Musumeci O, Tavilla G, Gaeta M, Caramori G, Toscano A. Ultrasound assessment of diaphragm function in patients with late-onset Pompe disease. Neurol Sci. 2020;41(8):2175–84. https://doi.org/10.1007/s10072-020-04316-6.
Saguil A. Evaluation of the patient with muscle weakness. Am Fam Physician. 2005;71(7):1327–36.
Larson ST, Wilbur J. Muscle Weakness in Adults: Evaluation and Differential Diagnosis. Am Fam Physician. 2020;101(2):95–108.
Hülsbrink R, Hashemolhosseini S. Lambert-Eaton myasthenic syndrome – Diagnosis, pathogenesis and therapy. Clin Neurophysiol. 2014;125(12):2328–36. https://doi.org/10.1016/j.clinph.2014.06.031.
Juel VC, Massey JM. Myasthenia gravis. Orphanet Journal of Rare Diseases. 2007; 2(1). https://doi.org/10.1186/1750-1172-2-44.
Dalakas MC, Longo DL. Inflammatory Muscle Diseases. N Engl J Med. 2015;372(18):1734–47. https://doi.org/10.1056/NEJMra1402225.
Singer PA, Cooper DS, Levy EG, Ladenson PW, Braverman LE, Daniels G, Greenspan FS, McDougall IR, Nikolai TF. Treatment guidelines for patients with hyperthyroidism and hypothyroidism. Standards of Care Committee, American Thyroid Association. JAMA. 1995;273(10):808–12.
Klopstock T. Drug-induced myopathies. Curr Opin Neurol. 2008;21(5):590–5. https://doi.org/10.1097/WCO.0b013e32830e2774.
Thompson PD, Panza G, Zaleski A, Taylor B. Statin-Associated Side Effects. J Am Coll Cardiol. 2016;67(20):2395–410. https://doi.org/10.1016/j.jacc.2016.02.071.
Simon L, Jolley SE, Molina PE. Alcoholic Myopathy: Pathophysiologic Mechanisms and Clinical Implications. Alcohol Res. 2017;38(2):207–17.
Ogasawara M, Nishino I. A review of core myopathy: central core disease, multiminicore disease, dusty core disease, and core-rod myopathy. Neuromuscul Disord. 2021;31(10):968–77. https://doi.org/10.1016/j.nmd.2021.08.015.
Capella-Peris C, Cosgrove MM, Chrismer IC, Razaqyar MS, Elliott JS, Kuo A, Emile-Backer M, Meilleur KG. Understanding Symptoms in RYR1-Related Myopathies: A Mixed-Methods Analysis Based on Participants’ Experience. The Patient - Patient-Centered Outcomes Research. 2020;13(4):423–34. https://doi.org/10.1007/s40271-020-00418-7.
Lawal TA, Todd JJ, Witherspoon JW, Bönnemann CG, Dowling JJ, Hamilton SL, Meilleur KG, Dirksen RT. Ryanodine receptor 1-related disorders: an historical perspective and proposal for a unified nomenclature. Skelet Muscle. 2020;10(1):32. https://doi.org/10.1186/s13395-020-00243-4.
Bouma S, Cobben N, Bouman K, Gaytant M, van de Biggelaar R, van Doorn J, Reumers SFI, Voet NBM, Doorduin J, Erasmus CE, et al. Respiratory features of centronuclear myopathy in the Netherlands. Neuromuscul Disord. 2023;33(7):580–8. https://doi.org/10.1016/j.nmd.2023.06.003.
Lawal TA, Patankar A, Todd JJ, Razaqyar MS, Chrismer IC, Zhang X, Waite MR, Jain MS, Emile-Backer M, Witherspoon JW, et al. Ryanodine Receptor 1-Related Myopathies: Quantification of Intramuscular Fatty Infiltration from T1-Weighted MRI. Journal of Neuromuscular Diseases. 2021;8(4):657–68. https://doi.org/10.3233/jnd-200549.
Todd JJ, Lawal TA, Witherspoon JW, Chrismer IC, Razaqyar MS, Punjabi M, Elliott JS, Tounkara F, Kuo A, Shelton MO, et al. Randomized controlled trial of N-acetylcysteine therapy for RYR1-related myopathies. Neurology. 2020;94(13):e1434–44. https://doi.org/10.1212/wnl.0000000000008872.
Lee CS, Hanna AD, Wang H, Dagnino-Acosta A, Joshi AD, Knoblauch M, Xia Y, Georgiou DK, Xu J, Long C, et al. A chemical chaperone improves muscle function in mice with a RyR1 mutation. Nat Commun. 2017;8(1):14659. https://doi.org/10.1038/ncomms14659.
Dowling JJ, Lawlor MW, Dirksen RT. Triadopathies: An Emerging Class of Skeletal Muscle Diseases. Neurotherapeutics. 2014;11(4):773–85. https://doi.org/10.1007/s13311-014-0300-3.
Russo M, Bonanno C, Profazio C, La Foresta S, Faraone C, Lizio A, Vita GL, Sframeli M, Aricò I, Ruggeri P, et al. Which are the factors influencing NIV adaptation and tolerance in ALS patients? Neurol Sci. 2020;42(3):1023–9. https://doi.org/10.1007/s10072-020-04624-x.
Acknowledgements
The authors would like to thank the patient’s daughter for her cooperation with the follow-up.
Funding
Funding was provided by National High Level Hospital Clinical Research Funding and Elite Medical Professionals Project of China-Japan Friendship Hospital (No. ZRJY2021-QM11).
Author information
Authors and Affiliations
Contributions
S.Z and Z.Z had the conception and design of the study. Y.C, S.Z and X.L prepared all the data from the patient and wrote the original draft. W.X, C.W and Z.Z critically revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki and the policy of the Ethics Committee.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and accompanying clinical data.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, Y., Zhang, S., Lu, X. et al. Unusual cause of muscle weakness, type II respiratory failure and pulmonary hypertension: a case report of ryanodine receptor type 1(RYR1)-related myopathy. BMC Pulm Med 24, 194 (2024). https://doi.org/10.1186/s12890-024-03016-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-03016-7