Abstract
Background
Sedation during flexible bronchoscopy (FB) should maintain an adequate respiratory drive, ensure maximum comfort for the patient, and warrant that the objectives of the procedure are achieved. Nevertheless, the optimal sedation method for FB has yet to be established. This study aimed to compare the standard recommended combination of midazolam-fentanyl (MF) with that of dexmedetomidine-ketamine (DK) for patient sedation during FB.
Methods
Patients subjected to FB were randomly assigned to a DK (n = 25) and an MF group (n = 25). The primary outcome was the rate of critical desaturation events (arterial oxygen saturation < 80% with nasal oxygen supply 2 L/min). Secondary outcomes included sedation depth, hemodynamic complications, adverse events, and patient and bronchoscopist satisfaction.
Results
The incidence rates of critical desaturation events were similar between the two groups (DK: 12% vs. MF: 28%, p = 0.289). DK achieved deeper maximum sedation levels (higher Ramsay - lower Riker scale; p < 0.001) and was associated with longer recovery times (p < 0.001). Both groups had comparable rates of hemodynamic and other complications. Patient satisfaction was similar between the two groups, but bronchoscopist satisfaction was higher with the DK combination (p = 0.033).
Conclusion
DK demonstrated a good safety profile in patients subjected to FB and achieved more profound sedation and better bronchoscopist satisfaction than the standard MF combination without increasing the rate of adverse events.
Similar content being viewed by others
Background
Flexible bronchoscopy (FB) is widely used for diagnostic and therapeutic lung interventions. Sedation is routinely administered during the procedure to reduce patient discomfort and facilitate the achievement of the clinical objectives [1]. Since FB is a typically brief process, the ideal agent should ensure deep sedation with preservation of the respiratory drive and minimal side effects [2]. Conventional medications include benzodiazepines (e.g., midazolam), opioids (e.g., fentanyl), and propofol, but all have the disadvantage of potentially significant suppression of the respiratory center [2,3,4,5]. Some experts have recently suggested that the evidence supporting the use of the midazolam-fentanyl (MF) combination during FB is weak to moderate [3, 5], while others have even advised against the use of opioids [6].
Dexmedetomidine is a selective α-2 receptor agonist with mild sedative, anxiolytic, and antisialagogue properties [7]. The agent does not affect the respiratory drive but can cause significant hemodynamic instability, mainly bradycardia and hypotension [7, 8]. Several studies have explored the role of dexmedetomidine in FB [9,10,11,12,13,14,15,16,17,18,19]; some of these trials reported a reduced rate of desaturation events compared to the conventional sedatives [9, 11, 13], while others found a higher incidence of hemodynamic adverse events and less satisfactory patient and bronchoscopist experiences [9, 12, 14, 16, 17].
Ketamine is an N-methyl D-aspartate receptor antagonist with anesthetic and powerful analgesic properties [20]. Its adverse events include excessive salivation and agitation on recovery, but the agent offers additional benefits, such as bronchodilation and cardiovascular stimulation (tachycardia, increased blood pressure, increased cardiac output) by enhancing the release of catecholamines [20]. When dexmedetomidine and ketamine are combined, their unfavorable effects may be counterbalanced, resulting in satisfactory sedation with favorable respiratory and hemodynamic profiles [21, 22]. The dexmedetomidine-ketamine (DK) combination has been studied in children [21, 23, 24] and adults requiring sedation for various invasive procedures [19, 22, 25]. The DK combination has also been evaluated as an adjunct to MF [19] and, recently, as a stand-alone regimen [26] in individuals undergoing FB.
The aim of this study was to evaluate further the DK and the standard MF combination in adults undergoing FB in terms of sedation quality, respiratory and hemodynamic profiles, and patient and bronchoscopist satisfaction. We hypothesized that the DK combination would be at least non-inferior to the MF regimen regarding major desaturation events.
Methods
Study design and population
This randomized controlled trial of adult patients (age > 18 years) scheduled for FB was conducted between September 2019 and May 2020 at the Respiratory Medicine Department of Athens Naval Hospital, Greece.
Exclusion criteria included: known or suspected allergy to any of the study drugs, renal impairment (serum creatinine > 2 mg/dL), hepatic impairment (liver enzymes > 2 times the upper limit of normal), seizure disorders, history of psychosis or bipolar disorder, hemodynamic instability (heart rate - HR < 50 bpm or systolic blood pressure - SBP < 90 mmHg), and critically ill patients. The study protocol was approved by the Ethics Committee of Athens Naval Hospital (act number 296/13.08.2019), and written informed consent was obtained from all participants.
Protocol
Demographic data and medical history were reviewed at the presentation, and the vital signs (including the modified Medical Research Council Dyspnea Scale) were assessed.
Fiberoptic and EBUS bronchoscopes were used depending on the target planning of the procedure. EBUS can produce greater discomfort to the patient and can be more demanding for the proceduralist, so an adjusted model was used to score bronchoscopist satisfaction with the different sedation methods.
Eligible patients were then randomly assigned to two groups:
-
1.
DK group: Dexmedetomidine solution of 1 µg/kg dissolved in 60 ml saline was administered over 15 min before the procedure was initiated, followed by a maintenance dose of 0.5 µg/kg/h (continuous infusion). After the first 15 min, a bolus dose of 50 mg ketamine dissolved in 10 ml saline was given. A bolus dose of 0.5 µg/kg after at least 20 min as an one-time administration and an increase of 0.1 µg/kg/h in the infusion rate of dexmedetomidine was considered when necessary to optimize the level of sedation.
-
2.
MF group: Midazolam was dissolved at the ratio of 1 mg/2 ml saline. We used a premedication dosage of 2 mg midazolam for anxiolysis 15 min before administering the induction dose, while registering vitals and preparing for bronchoscope insertion. Next, an induction dose of 5 mg bolus midazolam was administered and after 3–5 min the bronchoscope was inserted. Bolus doses of 1 mg midazolam at a minimum of 5–7 min intervals were administered as needed in order to obtain the desired sedation depth. Administration of fentanyl was given at a solution of 100 µg fentanyl / 10 ml saline; administered at 50 µg doses. First dose was administered at the induction phase, and up to 2 more bolus doses administered at 20-minute intervals in between and titrated as needed to obtain the desired sedation depth.
The depth of sedation was quantified at the onset of drug infusion using the Observer’s Assessment of Alertness/Sedation scale; a maximum score of 3 was considered optimal for starting FB [27]. Bolus doses of dexmedetomidine (DK group) and midazolam (MF group) were administered when necessary to maintain the same target score. Riker and Ramsay scale scores were also measured for the purposes of comparing sedation scales in regards to outcomes as a possible secondary endpoint. An anesthesiologist was present throughout the procedure to oversee and monitor the sedation protocol. Only the anesthesiologist and the nurse of the bronchoscopy suite were aware of the sedation regimen. The attending pulmonologist remained blind regarding the sedation protocol until the completion of the bronchoscopist satisfaction questionnaire (see below).
Lidocaine gel was placed at the nostril of entry before the procedure, and lidocaine (4 ml of 2% solution) was sprayed under direct vision through the bronchoscope for vocal cord anesthesia before entering the larynx. All participants were initially premedicated with 2 mg of midazolam 20 min before commencing the procedure for anxiolysis and perioperative amnesia. They also received oxygen at 2 L/min via nasal cannula and 0.9%.
NaCl i.v. at 8 ml/h throughout the procedure. Continuous monitoring included electrocardiography, oxygen saturation (SpO2), and automated non-invasive blood pressure recordings.
Outcomes
The total dose of the administered sedatives (including boluses) was recorded for each patient. The duration of the procedure (duration of FB) and recovery (measured from the time of bronchoscope withdrawal until the time the patient was evaluated as ready for discharge) were also noted.
The depth of sedation was evaluated using the Ramsay sedation scale [28] and the Riker sedation-agitation scale [29]. Both tools provide quantitative measurements in the maximum and minimum sedation-agitation range during the procedure. Higher Ramsay and lower Riker scores signify deeper sedation levels [28, 29].
Cough rate and intensity were evaluated according to a previously published questionnaire [30] including Likert-scale [36] items, as follows: 1 = no cough before or during the procedure; 2 = cough before FB without interruption of the procedure; 3 = cough during the procedure which demands more than one interruptions; 4 = persistent cough with more than three (frequent) procedural interruptions; 5 = persistent cough with frequent procedural interruptions and residual cough for more than two hours post-procedure. The rates of adverse events, including desaturations (SpO2 < 80%), blood pressure instability (determined by having a > 20% fluctuation of pre-operative mean arterial pressure) and significant bleeding (determined as bleeding on bronchoscopy site needing chemical intervention, wedging, mechanical ventilation or surgical intervention) were recorded.
Bronchoscopist satisfaction was measured with a Likert-scale tool answering the question “How satisfied are you with both the ease and outcome of the procedure” as follows: 1 = not satisfied at all; 2 = somewhat satisfied; 3 = more satisfied with the procedural outcome; 4 = mostly satisfied with the outcome and somewhat with procedural ease; 5 = exceptionally satisfied with both procedural outcome and ease.
Patient satisfaction [31] was evaluated by the following questions: (1) I was satisfied with the sedation administered for the procedure, (2) I felt pain and/or discomfort beyond my tolerance during the procedure, (3) I believe my needs were met during the procedure (4) I felt pain and discomfort after the procedure, (5) I would be willing to undergo a second procedure if the first did not yield adequate results. The responses were measured in a Likert scale format with values 1 = strongly disagree; 2 = disagree; 3 = neither agree nor disagree; 4 = agree; 5 = strongly agree. The questionnaire was given in printed form at discharge, and the responses were collected by telephone call the day after the procedure.
Sample size estimation and statistical analyses
The primary endpoint of the study was the occurrence of major desaturation events (i.e., SpO2 < 80% with nasal oxygen supply 2 L/min, duration >/= 15 s). Assuming a desaturation rate of 20 ± 5%, we calculated a lower critical number of 25 patients per group to prove non-inferiority within the above limits of the primary endpoint, with a p-value of < 0.05 and 85% power.
Continuous variables are presented as mean ± SD with median and range and compared with the Student’s t or Mann-Whitney U test, as appropriate. Categorical variables are given as number of cases (%) and compared with the chi-square or Fisher’s exact test. Multivariable linear regression analysis was applied to reveal the predictors of bronchoscopist satisfaction (log-transformed score). A p-value of < 0.05 was considered significant in all instances. Statistical analysis was conducted with the SPSS version 28 (IBM Corp., Armonk, NY).
Results
A total of 73 patients were screened for eligibility during the study period. Of them, 15 did not fulfill the inclusion criteria, and 4 did not consent to participate in the study. The remaining 54 patients were randomly allocated to the two study groups. The DK group noted two sedation protocol violations (the attending anesthesiologist changed to a different drug). In the MF group, the procedure was interrupted in one patient due to severe bleeding, while one participant refused to answer the patient satisfaction questionnaire. Therefore, the final study population included 50 patients, 25 in each group. Their demographic and clinical characteristics are shown in Table 1. A study flow is presented in Fig. 1.
Indications for bronchoscopy for the MF and DK group included: pulmonary nodule 5 (20%) and 15 (60%), mass 9 (36%) and 5 (20%), consolidation 9 (36%) and 6 (24%), and lymph node enlargement 3 (12%) and 0 (0%), respectively. A simple fiberoptic bronchoscope was used in 19 (76%) of the MF group patients and in 14 (56%) of those of the DK group (p = 0.232). An endobronchial ultrasound (EBUS) bronchoscope was used in 6 (24%) patients of the MF group and 11 (44%) of the DK group.
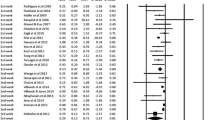
The study outcomes are presented in Table 2 and in Figs. 2 and 3. The DK combination achieved deeper sedation levels at the phase of maximum sedation compared to the MF regimen (Table 2). During that phase, most patients in the DK group were well beyond the optimal sedation level (i.e., they were more sedated) (Fig. 2). Sedation characteristics during the minimum sedation phase were comparable between the two groups (Table 2; Fig. 2). DK combination was associated with longer procedure and recovery duration (Table 2). The DK group scored marginally lower on the cough scale (p = 0.064). The rate of critical desaturation events was 28% in the MF and 12% in the DK group (p = 0.289). The rate of other complications also did not differ (Table 2). One female patient in the DK group presented urinary loss during the procedure without prior medical history of incontinence.
Bronchoscopist satisfaction was higher in the DK group (4.4 ± 0.9; median 5, range 2–5) compared to the MF group (3.7 ± 1.2; median 4, range 2–5; p = 0.033) (Fig. 3). The DK combination and the lack of complications during the procedure emerged as significant and independent determinants of bronchoscopist satisfaction (Table 3). Multivariable regression analysis showed a statistically significant value of p = 0.018 for the DK combination adjusted effect, while a value of p = 0.596 for EBUS usage in regards to bronchoscopist satisfaction, which suggests that EBUS usage did not affect bronchoscopist satisfaction. Patient satisfaction levels were comparable between the DK (23.3 ± 2.5; median 24, range 14–25) and the MF group (22.9 ± 2.3; median 23, range 15–25; P = 0.282) (Fig. 3).
Discussion
In this single-center, randomized controlled trial, we explored the safety and efficacy of the DK combination compared to a standard MF regimen in adults undergoing FB. Our findings suggest that DK can achieve deep sedation with adequate respiratory and hemodynamic profiles, reasonable patient comfort, and high bronchoscopist satisfaction. Major desaturation events occurred at a similar frequency in the two study groups, thus confirming the non-inferiority of the DK combination, in line with the study hypothesis. However, the time required for recovery was significantly longer in the DK group, which might limit the widespread application of the DK combination, especially in the case of busy bronchoscopic laboratories.
Dexmedetomidine, as opposed to conventional sedatives and opioids, has the advantage of preserving the respiratory drive, a critical objective of conscious sedation during bronchoscopy [1, 2]. However, the drug may cause hemodynamic instability (i.e., bradycardia and hypotension), which may significantly affect the success of the interventional procedure [8]. Indeed, previous studies in adults have confirmed that dexmedetomidine was associated with more hemodynamic adverse events leading to less satisfactory doctor experiences [9, 12, 14, 16, 17]. Ketamine, on the other hand, despite its well-known adverse effects, causes cardiovascular stimulation, which may counterbalance the effects of dexmedetomidine [21]. In addition, ketamine is a potent analgesic that could act complementary to dexmedetomidine to increase patient comfort [21, 22]; its bronchodilatory effect and the ability to preserve the respiratory drive at low doses [20] may offer additional benefits in patients undergoing FB [1].
An earlier randomized-controlled trial has explored the utility of DK combination as an adjunct to MF regimen in adults undergoing FB [19]. Atkins et al. [19] have shown that, patients in the MF-DK group (n = 25) achieved lower serum midazolam and fentanyl levels than those (n = 25) who received only the MF combination. Patient and bronchoscopist satisfaction scores and time of desaturations (SpO2 < 90%) were comparable between the two groups. It is worth noting that the relative decrease in minute ventilation was greater in the MF group [19]. Although the design and the objectives of the above study were different from ours (DK as adjuvant therapy [19] versus DK as a stand-alone regimen in our study), its findings are in line with ours; in patients undergoing FB, since the DK combination can achieve satisfactory conscious sedation without significant respiratory or hemodynamic adverse events.
The DK combination has also been studied in children [21, 23, 24] and adults [22, 25] undergoing invasive procedures other than FB. Similar to our study, those trials have proven the safety and efficacy of the DK combination in terms of sedation quality, respiratory and hemodynamic complications, and patient and doctor satisfaction. However, the time required to obtain the appropriate level of sedation and the duration of recovery was generally longer than those observed with the conventional regimens. Thus, it has been recently suggested that the DK combination may be more suitable for high-risk patients who require hemodynamic and respiratory stability during non-urgent invasive procedures [25].
Airway interventions like bronchoscopy have specific requirements related to cough, gag reflex, and patient agitation due to discomfort [1]. In this regard, the DK combination performed optimally in our study, which may explain the higher bronchoscopist satisfaction in the DK group. The deeper sedation level most likely facilitated the attending bronchoscopist and allowed for a more focused and thorough procedure; Additionally, the significantly longer duration of FB in the DK group further supports the above hypothesis. Future studies should explore this aspect by taking into account the qualitative characteristics of bronchoscopist and anesthesiologist satisfaction in regards to the intervention type (FB, EBUS, etc.) and the particularities of each patient, as a personalized approach.
Major desaturation events occurred with statistically similar frequencies in the two study groups, albeit their rate was slightly lower with the DK combination. Although this result supports the non-inferiority of the DK regimen, it does not indicate that DK may be more suitable for high-risk respiratory patients [21]. A recent study that investigated the role of dexmedetomidine in awake fiberoptic intubation for the management of difficult airway reported a markedly decreased muscle tone compared to fentanyl and ketamine [32], suggesting that this may be the principal mechanism of dexmedetomidine-induced respiratory depression. This is a different mechanism to the central respiratory depression caused by benzodiazepines and opiates. Reduced muscle tone respiratory depression can be less impactful to certain patient populations like Parkinson’s disease patients, and can be usually dealt with a jaw thrust maneuver, which we successfully used in our cases as well. Riker scale score and Ramsay scale measurement analysis did not offer any additional insight, but the data might prove to be useful for a cross-examination of different scales for procedural sedation in regards to patient and bronchoscopist satisfaction in future meta-analysis.
Notably, the DK combination might prove more suitable for patients with Parkinson’s disease, in whom respiratory-related disease incidences are pervasive [33]. While benzodiazepines can aggravate Parkinson’s symptoms [34], dexmedetomidine and ketamine have been shown to ameliorate dyskinesia and improve the respiratory mechanics in such patients [35, 36].
Our study has limitations. The sample size, although proper to prove non-inferiority, was small and did not offer enough power to evaluate further the apparent benefits of the DK regimen (e.g., in terms of cough and major desaturation events) or to detect uncommon complications in either treatment arm. Second, our study was only partially blinded; although the pulmonologist was unaware of the sedation protocol, the attending anesthesiologist and the laboratory nurse had access to the type of sedation. Third, the study sample was rather inhomogeneous, including patients with various respiratory diseases and different procedural goals. Fourth, we have no data on the exact number of midazolam/fentanyl bolus doses used in the MF group, and no data for the patients for whom an increase in the infusion rate of dexmedetomidine was required in the DK group. Finally, it is possible that the midazolam premedication offered a synergistic action with dexmedetomidine and ketamine. Nevertheless, the sedation protocol remained consistent across all participants. Combining DK with an anxiolytic dose of midazolam may prove even more effective for demanding bronchoscopic procedures, omitting the use of fentanyl to maximize sedation while minimizing impact on respiratory function. Future studies, with better design and larger sample sizes, should also determine the appropriate dosage of DK combination and explore its benefits over the conventional sedation regimens for specific patient populations (e.g., high-risk respiratory patients, patients with Parkinson’s disease, patients on opiate withdrawal or with contraindications to opiates, etc.).
In conclusion, our study showed that the administration of a DK combination during FB achieved conscious sedation, stable respiratory and hemodynamic profiles, and patient comfort comparable to those of the classical MF regimen. Although the time required for recovery was longer in the DK group, the deeper but uncomplicated sedation allowed for a more focused and thorough procedure, thus resulting in significantly higher bronchoscopist satisfaction. The DK combination may be considered a viable and promising alternative to standard sedation regimens in adult patients undergoing FB.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Du Rand IA, Blaikley J, Booton R, Chaudhuri N, Gupta V, Khalid S, et al. Summary of the British Thoracic Society guideline for diagnostic fexible bronchoscopy in adults. Thorax. 2013;68(8):786–7.
Hong KS, Choi EY, Park DA, Park J. Safety and Efficacy of the Moderate Sedation during Flexible Bronchoscopic Procedure: a systematic review and Meta-analysis of Randomized controlled trials. Med (Baltim). 2015. https://doi.org/10.1097/MD.000000000000145910.1097/MD.0000000000001459.
Strohleit D, Galetin T, Kosse N, Lopez-Pastorini A, Stoelben E. Guidelines on analgosedation, monitoring, and recovery time for flexible bronchoscopy: a systematic review. BMC Pulm Med. 2021. https://doi.org/10.1186/s12890-021-01532-4.
Dreher M, Ekkernkamp E, Storre JH, Kabitz HJ, Windisch W. Sedation during flexible bronchoscopy in patients with pre-existing respiratory failure: Midazolam versus Midazolam plus Alfentanil. Respiration. 2010. https://doi.org/10.1159/000267227.
Mohan A, Madan K, Hadda V, et al. Guidelines for diagnostic flexible bronchoscopy in adults: Joint Indian Chest Society/National College of chest physicians (I)/Indian association for bronchology recommendations. Lung India. 2019. https://doi.org/10.4103/lungindia.lungindia_108_19.
Hautmann H, Eberhardt R, Heine R, et al. Empfehlung Zur Sedierung in Der Flexiblen Bronchoskopie [Recommendations for sedation during flexible bronchoscopy]. Pneumologie. 2011. https://doi.org/10.1055/s-0031-1291395.
Mantz J, Josserand J, Hamada S. Dexmedetomidine: new insights. Eur J Anaesthesiol. 2011. https://doi.org/10.1097/EJA.0b013e32833e266d.
Chang ET, Certal V, Song SA, et al. Dexmedetomidine versus propofol during drug-induced sleep endoscopy and sedation: a systematic review. Sleep Breath. 2017. https://doi.org/10.1007/s11325-017-1465-x.
Ryu JH, Lee SW, Lee JH, Lee EH, Do SH, Kim CS. Randomized double-blind study of remifentanil and dexmedetomidine for flexible bronchoscopy. Br J Anaesth. 2012. https://doi.org/10.1093/bja/aer400.
Zhang H, Fang B, Zhou W. The efficacy of dexmedetomidine-remifentanil versus dexmedetomidine-propofol in children undergoing flexible bronchoscopy: a retrospective trial. Med (Baltim). 2017. https://doi.org/10.1097/MD.0000000000005815.
Yuan F, Fu H, Yang P, et al. Dexmedetomidine-fentanyl versus propofol-fentanyl in flexible bronchoscopy: a randomized study. Exp Ther Med. 2016. https://doi.org/10.3892/etm.2016.3274.
Lin TY, Huang YC, Kuo CH, et al. Dexmedetomidine sedation for endobronchial ultrasound-guided transbronchial needle aspiration, a randomised controlled trial. ERJ Open Res. 2020. https://doi.org/10.1183/23120541.00064-2020.
St-Pierre P, Tanoubi I, Verdonck O, et al. Dexmedetomidine Versus Remifentanil for Monitored Anesthesia Care during Endobronchial Ultrasound-guided transbronchial needle aspiration: a Randomized Controlled Trial. Anesth Analg. 2019. https://doi.org/10.1213/ANE.0000000000003633.
Kumari R, Jain K, Agarwal R, Dhooria S, Sehgal IS, Aggarwal AN. Fixed dexmedetomidine infusion versus fixed-dose midazolam bolus as primary sedative for maintaining intra-procedural sedation during endobronchial ultrasound-guided transbronchial needle aspiration: a double blind randomized controlled trial. Expert Rev Respir Med. 2021. https://doi.org/10.1080/17476348.2021.1918000.
Kim J, Choi SM, Park YS, et al. Dexmedetomidine versus midazolam for sedation during endobronchial ultrasound-guided transbronchial needle aspiration: a randomised controlled trial. Eur J Anaesthesiol. 2021. https://doi.org/10.1097/EJA.0000000000001370.
Goneppanavar U, Magazine R, Periyadka Janardhana B, Krishna Achar S. Intravenous dexmedetomidine provides Superior Patient Comfort and Tolerance compared to intravenous midazolam in patients undergoing flexible bronchoscopy. Pulm Med. 2015. https://doi.org/10.1155/2015/727530.
Liao W, Ma G, Su QG, Fang Y, Gu BC, Zou XM. Dexmedetomidine versus midazolam for conscious sedation in postoperative patients undergoing flexible bronchoscopy: a randomized study. J Int Med Res. 2012. https://doi.org/10.1177/147323001204000415.
Pertzov B, Krasulya B, Azem K, et al. Dexmedetomidine versus propofol sedation in flexible bronchoscopy: a randomized controlled trial. BMC Pulm Med. 2022. https://doi.org/10.1186/s12890-022-01880-9.
Atkins JH, Haas AR, Sterman DH, Vachani A, Mandel JE. A randomized, placebo-controlled, concealed allocation comparison of respiratory depression during bronchoscopy with dexmedetomidine-ketamine as an adjunct to fentanyl-midazolam sedation. Transl Perioper Pain Med. 2016;1(1):24–31.
Zanos P, Moaddel R, Morris PJ et al. Ketamine and Ketamine Metabolite Pharmacology: Insights into Therapeutic Mechanisms [published correction appears in Pharmacol Rev. 2018;70(4):879]. Pharmacol Rev. 2018; https://doi.org/10.1124/pr.117.015198.
Tobias JD. Dexmedetomidine and ketamine: an effective alternative for procedural sedation? Pediatr Crit Care Med. 2012. https://doi.org/10.1097/PCC.0b013e318238b81c.
Singh A, Iyer KV, Maitra S, et al. Ketamine and dexmedetomidine (Keto-dex) or ketamine and propofol (Keto-fol) for procedural sedation during endoscopic retrograde cholangiopancreatography: which is safer? A randomized clinical trial. Indian J Gastroenterol. 2022. https://doi.org/10.1007/s12664-022-01291-y.
Tosun Z, Akin A, Guler G, Esmaoglu A, Boyaci A. Dexmedetomidine-ketamine and propofol-ketamine combinations for anesthesia in spontaneously breathing pediatric patients undergoing cardiac catheterization. J Cardiothorac Vasc Anesth. 2006. https://doi.org/10.1053/j.jvca.2005.07.018.
Koruk S, Mizrak A, Gul R, Kilic E, Yendi F, Oner U. Dexmedetomidine-ketamine and midazolam-ketamine combinations for sedation in pediatric patients undergoing extracorporeal shock wave lithotripsy: a randomized prospective study. J Anesth. 2010. https://doi.org/10.1007/s00540-010-1023-1.
Grégoire C, De Kock M, Henrie J, et al. Procedural Sedation with Dexmedetomidine in Combination with ketamine in the Emergency Department. J Emerg Med. 2022. https://doi.org/10.1016/j.jemermed.2022.01.017.
Chernik DA, Gillings D, Laine H, et al. Validity and reliability of the Observer’s Assessment of Alertness/Sedation scale: study with intravenous midazolam. J Clin Psychopharmacol. 1990;10(4):244–51.
Ramsay MA, Savege TM, Simpson BR, Goodwin R. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974. https://doi.org/10.1136/bmj.2.5920.656.
Riker RR, Picard JT, Fraser GL. Prospective evaluation of the sedation-agitation scale for adult critically ill patients. Crit Care Med. 1999;27:1325–9.
Kobayashi F, Saraya T, Oda M, et al. Novel predictive factors for patient discomfort and severe cough during bronchoscopy: a prospective questionnaire analysis. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0240485.
Chanthong P, Abrishami A, Wong J, Herrera F, Chung F. Systematic review of questionnaires measuring patient satisfaction in ambulatory anesthesia. Anesthesiology. 2009. https://doi.org/10.1097/ALN.0b013e31819db079.
Verma AK, Verma S, Barik AK, Kanaujia V, Arya S. Intubating conditions and hemodynamic changes during awake fiberoptic intubation using fentanyl with ketamine versus dexmedetomidine for anticipated difficult airway: a randomized clinical trial. Braz J Anesthesiol. 2021. https://doi.org/10.1016/j.bjane.2021.01.005.
Shaibdat NS, Ahmad N, Azmin S, Ibrahim NM. Causes, factors, and complications associated with hospital admissions among patients with Parkinson’s disease. Front Neurol. 2023. https://doi.org/10.3389/fneur.2023.1136858.
Gaztanaga W, Sarno M, Margolesky J, et al. Do Benzodiazepines Impair Motor and nonmotor symptoms in a sample of Parkinson’s Disease patients? Cureus. 2021. https://doi.org/10.7759/cureus.13220.
Nakajima T, Suzuki Y, Miyaue N. Successful management of Parkinson’s Disease Dyskinesia during Local Anesthesia with Dexmedetomidine. Cureus. 2021. https://doi.org/10.7759/cureus.13739.
Ye T, Bartlett MJ, Sherman SJ, Falk T, Cowen SL. Spectral signatures of L-DOPA-induced dyskinesia depend on L-DOPA dose and are suppressed by ketamine. Exp Neurol. 2021. https://doi.org/10.1016/j.expneurol.2021.113670.
Likert R. A technique for the measurement of attitudes. Archives Psychol. 1932.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
AF, NZ and CM collected the data and performed the procedure. SF performed the statistical analysis. AF and SF wrote the manuscript. KK and VG revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Subjects have given their written informed consent. The study protocol has been approved by the Athens Naval Hospital Scientific and Ethics Review Board (act number 296/13.08.2019). Clinical trial registration number and date: ClinicalTrials.gov Identifier NCT06185127, date 29/12/2023, link https://clinicaltrials.gov/study/NCT06185127?term=NCT06185127&rank=1.
Consent for publication
Not applicable.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Apostolos, F., Nikolaos, Z., Charalampos, M. et al. Dexmedetomidine-ketamine combination versus fentanyl-midazolam for patient sedation during flexible bronchoscopy: a prospective, single-blind, randomized controlled trial. BMC Pulm Med 24, 301 (2024). https://doi.org/10.1186/s12890-024-02988-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-02988-w