Abstract
Background
Safely implementing transbronchial lung cryobiopsy (TBLC) in patients with interstitial lung disease (ILD) requires accurate navigation. Traditional fluoroscopy falls short in reducing the risk of post-procedure pneumothorax. The potential of electromagnetic navigation bronchoscopy (ENB) as a more precise navigation method warrants further exploration.
Methods
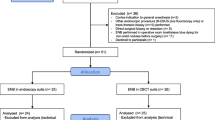
A prospective cohort study was conducted on ILD patients undergoing TBLC. Patients were assigned either fluoroscopy or ENB for cryoprobe positioning. Navigation accuracy was evaluated using cone beam computed tomography (CBCT) images as the standard. Safety and diagnostic yield were also observed.
Results
Seventeen patients underwent TBLC, with 10 guided by fluoroscopy and seven by ENB. Fluoroscopy-guided cryoprobe navigation required more adjustments [9/15 (60%) v.s. 1/9 (11%), p = 0.018] for subsequent TBLC compared to ENB, as confirmed by CBCT images. Clinical characteristics, post-procedure complications, and biopsy specimen size showed no significant differences between the groups. Fourteen patients obtained a pathological diagnosis, and 15 received a multidisciplinary discussion (MDD) diagnosis. In the fluoroscopy group, three patients failed to obtain a pathological diagnosis, and two failed to obtain an MDD diagnosis.
Conclusions
ENB demonstrates significantly superior accuracy in TBLC navigation compared to traditional fluoroscopy when CBCT images are used as a reference. Further studies are necessary to determine the value of ENB in TBLC navigation for ILD patients.
Similar content being viewed by others
Introduction
Transbronchial lung cryobiopsy (TBLC) is increasingly applied in the diagnosis of interstitial lung disease (ILD), and it has been considered an alternative to surgical lung biopsy (SLB), which was once considered the gold standard for the pathological diagnosis of ILD [1]. The safety of TBLC has been proved in many studies, but its main complications remain airway bleeding and pneumothorax [2,3,4,5]. Therefore, navigation is required during the TBLC procedure to determine whether the cryoprobe is positioned properly to avoid proximity to the great vessels and pleura. Among various navigation methods, fluoroscopy is the earliest and most commonly used [6, 7]. The application of fluoroscopy during TBLC is also recommended in the CHEST Guideline and Expert Panel Report [8]. However, previous studies have shown that fluoroscopy navigated TBLC has a high incidence of pneumothorax complications [9].
Therefore, other navigation methods that can reduce the risk of complications of TBLC are gradually being explored, among which cone beam computed tomography (CBCT)-navigated TBLC can significantly reduce the incidence of post-procedure pneumothorax and airway bleeding [3, 10, 11]. However, the scarcity of CBCT equipment and radiation exposure limits its wide application in TBLC navigation. Electromagnetic Navigation Bronchoscopy (ENB) is a relatively new technique for bronchoscopy navigation. It utilizes reconstructed virtual three-dimensional images of the tracheobronchial tree derived from high-resolution chest imaging. The process involves setting navigation goals and planning paths within a specific system, such as superDimension™, facilitating the accurate location of lesions and performing biopsies using a position sensor during bronchoscopy within a specific electromagnetic field [12]. ENB has been extensively applied in the biopsy of suspected tumor lesions in the peripheral lung [13]. The National Comprehensive Cancer Network guidelines have recommended using ENB for biopsy in peripheral pulmonary nodule lesions for definitive diagnosis [14]. Previous studies have shown that ENB navigated TBLC can significantly improve the diagnostic yield of small pulmonary nodules with good safety profile [15]. However, there has been only one previous single-arm study of ENB navigated TBLC in the diagnosis of ILD, and the results showed that ENB navigation for TBLC could bring a high diagnostic yield (11/13, 85%) [16]. Therefore, it is necessary to further illuminate the advantages of ENB navigated TBLC in the diagnosis of ILD.
Therefore, this pilot prospectively comparative study was conducted to explore the accuracy of ENB compared to conventional fluoroscopy in TBLC navigation in patients with ILD.
Material and methods
Patients
A total of 17 patients participated in the study, all of whom were admitted to the Department of Pulmonary and Critical Care Medicine, China-Japan Friendship Hospital due to ILD between January 1st, 2020 and December 31st, 2022. All patients completed hematological examinations, pulmonary function tests, and high-resolution computed tomography (HRCT) after admission and were evaluated by ILD and respiratory intervention specialists. Further TBLC was recommended by the multidisciplinary team (MDT) to confirm the diagnosis of patients when the following inclusion criteria were met: > 18 years of age; a diagnosis of ILD could not be established after integration of clinical features; forced vital capacity (FVC) > 50%; and diffusing capacity of the lung for carbon monoxide (DLCO) > 35%. Patients who met the following criteria were excluded: acute exacerbation in the past 30 days, bleeding diathesis, anticoagulant therapy, current use of anti-platelet drugs, pulmonary hypertension, respiratory failure, liver or kidney dysfunction, cardiac insufficiency, and platelet count < 50 × 109/L. The site for the lung biopsy is determined through MDT discussion and is typically chosen to target the most prominent lesion site. For diffuse lesions, there is a preference for sampling from the lower lobes. Additionally, the approach includes consideration for sampling multiple segments or lobes, depending on an assessment by an interventional pulmonology specialist. This assessment will evaluate the likelihood of successful sampling and weigh the potential risks involved. This study was approved by the Ethics Committee of the China-Japan Friendship Hospital (2017-25-1), and written informed consent was obtained from all patients.
Procedures
Patients received either the fluoroscopy navigation group or the ENB group prior to the TBLC procedure were included. TBLC was performed through an endotracheal tube or rigid bronchoscopy under general anesthesia in a hybrid CBCT operation room. For patients in the ENB group. A compact disc of the HRCT scan within 1 week was created for the superDimension™ navigation system (ver. 7.0, Medtronic Inc.).
The cryoprobe positioning of TBLC was divided into two steps. The first step was to determine the initial position of cryoprobe through fluoroscopy or ENB, and then a CBCT scan was performed to confirm whether the cryoprobe position was appropriate. Cryoprobes from ERBE, Solingen, Germany were used in both groups (1.9 mm or 2.4 mm cryoprobe). In the fluoroscopy navigation group, the cryoprobe was advanced as far as possible into the target bronchial segment through the bronchoscopy working channel. Fluoroscopy was then used to navigate the cryoprobe so that the tip of the cryoprobe was 1 to 2 cm from the visceral pleura. In the ENB group, an electromagnetic board was placed on the back of the patient. At first, a portion of the tip of the Extended Working Channel (EWC) would be cut off to allow the 1.9 mm cryoprobe to pass through. A position sensor was then introduced into the airways at the tip of the navigation probe through EWC. With the electromagnetic field generated, the position of the sensor was calculated in real time and merged with the previously created 3D reconstruction of the patient. The sensor was then navigated to the target site in the electromagnetic field according to the predefined biopsy mark. Once the sensor position is determined, remove the sensor and place the cryoprobe through the EWC. After cryoprobe placement by fluoroscopy navigation or ENB, the CBCT imaging (Artis Zee III ceiling, Siemens AG, Munich, Germany) was performed. The cryoprobe position within the lung parenchyma and its relationship to other thoracic structures was assessed using three-dimensional CT images acquired in the axial, coronal, and sagittal planes. If the cryoprobe position was not ideal, it would be adjusted according to CBCT images, and the final biopsy position would be determined, which was generally about 1-2 cm away from visceral pleura.
Cryobiopsy (6–8 s for the 1.9 mm cryoprobe and 4–6 s for the 2.4 mm cryoprobe) was [17] performed after cryoprobe positioning, using carbon dioxide as the cryogen. Pre-positioned bronchial blockers (CRE balloon; Boston Scientific Microvasive, Natick, MA, USA) were immediately filled (0.5–1 atm) after each biopsy to stop bleeding. To check for acute pneumothorax, CBCT imaging or X-rays were operated following the procedure. Four levels of severity were assigned to bleeding [18]: Grade 0, no bleeding; Grade 1, mild bleeding (suction is needed for clearance, but no other endoscopic procedures are required); Grade 2, moderate bleeding (endoscopic procedures such as bronchial occlusion-collapse or ice-cold saline instillations are necessary); Grade 3, severe bleeding (the patient is hemodynamically unstable or has respiratory instability and may need to undergo surgical tamponade or blood transfusions). The flow of TBLC for patients in the ENB group is shown in Fig. 1. TBLC sites, number of cryoprobe adjustments, number and size of specimens, and complications were recorded.
The flow of navigation and TBLC procedure for patients in the ENB group. A portion of the Extended Working Channel (EWC) tip would be cut off to allow passage of the 1.9 mm cryoprobe (A). The electromagnetic navigation probe with a position sensor at the tip was placed through EWC (B). In the electromagnetic field, used the navigation probe to guide the flexible bronchoscope, and the EWC placed in the working channel to the pre-set biopsy site (C). Once navigation is complete, withdraw the navigation probe and position the cryoprobe through the EWC into the target biopsy site (D). After cryoprobe placement, CBCT scanning was performed to determine if the cryoprobe position was ideal (E). TBLC was performed to obtain lung tissue specimens after confirming that the cryoprobe was in the proper position (F)
All pathological diagnosis were made by experienced pulmonary pathologists. A second pathologist was consulted in complex cases, and discrepancies were resolved by consensus. The multidisciplinary discussion (MDD) diagnosis was the final clinical diagnosis and was made through discussions among MDT members. There were pulmonary and critical care medicine physicians, radiologists, pathologists, and rheumatologists on the MDT.
Statistics
Continuous variables were reported as median within the interquartile range (IQR), considering the small sample size of this study. The Mann–Whitney test was used for continuous variables. Categorical variables are presented directly or reported with frequency (percentage). The Fisher exact tests were conducted to compare binary and categorical variables. The statistical analyses were performed with SPSS statistics software (version 25.0; SPSS Inc., Chicago, IL).
Results
Of the 17 enrolled patients who underwent TBLC, 10 underwent biopsy with fluoroscopy navigation and 7 with ENB. Demographic characteristics, clinical manifestations, and procedure-concerned laboratory tests of the patients are shown in Table 1. There were no significant differences in clinical characteristics between the fluoroscopy and ENB groups.
Patients were re-navigated when biopsies were performed in different pulmonary lobes, and a total of 24 navigations were performed in the 17 enrolled patients, 15 navigations in 10 patients using fluoroscopy, and 9 navigations in 7 patients using ENB. The comparison of the biopsy/navigation site, the number of cryoprobe adjustments based on CBCT images, specimen parameters, and procedure-related complications between the two groups is shown in Table 2. There was no significant difference in biopsy/navigation position between the two groups, but cryoprobes in the fluoroscopy group required more adjustments [9/15(60%) v.s. 1/9(11%), p = 0.018)] after CBCT confirmed position than those in the ENB group. There was no difference in specimen size and post-procedure complications between the two groups of patients.
The specific imaging findings, pathological and multidisciplinary discussion diagnosis of the two groups are shown in Table 3. A total of 14 patients had a pathological diagnosis, and 15 patients had an MDD diagnosis. Non-specific interstitial pneumonia (NSIP) was the most common imaging manifestation in both groups. NSIP was also the most common pathological diagnosis in both groups. In the fluoroscopy group, three patients could not obtain a definite pathological diagnosis, while in the ENB group, all patients obtained a pathological diagnosis. After MDD, one patient in the fluoroscopy group was diagnosed with unclassifiable interstitial lung disease (uILD), two patients with an indeterminate diagnosis, while all patients in the ENB group had a final clinical diagnosis.
Discussion
TBLC can lead to good pathologic and multidisciplinary discussion diagnostic yield of ILD, but the risk of pneumothorax and airway bleeding is a limiting factor for its application [2,3,4,5]. Therefore, accurate navigation is an essential prerequisite for the development of TBLC. Based on the CBCT image as the standard, this study further clarified the application value of ENB in TBLC navigation in patients with ILD by comparing the accuracy of fluoroscopy navigation and ENB.
The biopsy target of TBLC in ILD should not be too close to the pleura or the great vessels to avoid pneumothorax and remarkable airway bleeding [19]. The incidence of pneumothorax in patients with ILD undergoing TBLC without navigation was up to 20.9%, so subsequent studies demonstrated the value of fluoroscopy, radial endobronchial ultrasound (radial-EBUS), CBCT, and ENB in TBLC navigation in this group of patients [3, 16, 20,21,22,23]. Given the simplicity and breadth of the application of fluoroscopy equipment, the CHEST Guideline and Expert Panel Report promoted the routine use of fluoroscopy for TBLC in ILD patients [8]. However, whether fluoroscopy navigation could reduce the risk of pneumothorax is still controversial [9, 20, 21]. Radial-EBUS can identify the large vessels in the biopsy field, thus reducing the risk of airway bleeding. Still, the risk of pneumothorax in TBLC using radial-EBUS navigation is high (15%) due to poor judgment of pleural distance [22, 23]. Our team has previously demonstrated the value of CBCT in TBLC through a larger cohort, especially in reducing pneumothorax complications (1.9%) [3]. It is suggested that CBCT navigation may be the safest method for TBLC navigation. However, CBCT has not been widely used in ILD centers. In addition to our team’s previous study, there was only one report on the use of CBCT in TBLC navigation in ILD patients [10], suggesting that accurate and widely used navigation methods should continue to be found.
Many previous studies have confirmed the advantages of ENB in cryobiopsy of peripheral lung lesions, especially pulmonary nodules [13, 24]. It is reasonable to believe the application value of this combination in diagnosing ILD. Kronborg-White et al. conducted a pilot study of ENB as a TBLC navigation tool in diagnosing ILD at multiple European centers [16]. The study used the superDimentation™ system and enrolled 13 patients. With 1.7 mm or 1.9 mm cryoprobe, three patients (23%) developed pneumothorax, one patient (8%) developed mild bleeding, six patients (46%) developed moderate bleeding after TBLC and 11 patients (85%) were finally diagnosed. In our study, the superDimentation™ system was also used. All TBLC in the ENB group used 1.9 mm cryoprobes. With the help of CBCT, no patient developed post-procedure pneumothorax, and there were 11 cases (46% of all navigations) of mild bleeding and 1 case (4% of all navigations) of moderate bleeding. Fourteen of the 17 patients had a pathological diagnosis by TBLC, and 15 had MDD diagnosis, of which 1 had a diagnosis of uILD. The main objective of this study is to observe the accuracy of ENB in TBLC navigation compared with that of fluoroscopy. The results showed that cryoprobe navigation by fluoroscopy required more adjustments than ENB when CBCT images were used as the gold standard for cryoprobe positioning. The results also suggested that ENB has the potential to be comparable to CBCT.
However, ENB presents certain drawbacks in clinical applications. Firstly, ENB is not a truly real-time navigation system; its accuracy is compromised by factors such as patient respiratory movements, localization discrepancies, and short-term variations in pulmonary lesions. To address these issues, patients in this study had completed HRCT within 1 week prior to undergoing TBLC and utilized the most recent imaging for ENB navigation. The majority of ILDs are chronic inflammatory and fibrotic lesions with minimal short-term change. Moreover, CBCT, a true real-time navigation system, was used to calibrate ENB’s accuracy in this study. There was only one cryoprobe adjustment (1 out of 11 biopsies) for TBLC with ENB, suggesting that ENB, despite not being a real-time system, is highly accurate and valuable for further application in diagnosing ILD. If a patient has limited lesions and there is concern that ENB may not accurately access the lesion specimen, the addition of radial-EBUS may be considered to aid navigation. This combined navigation approach has been utilized for biopsy of small peripheral pulmonary nodules and merits further investigation for its value in TBLC for patients with ILD [17, 25, 26]. Secondly, the consumables associated with ENB are expensive, costing more than those for other navigation methods such as fluoroscopy and CBCT. Yet, if ENB reduces the risk of complications associated with biopsy, it may reduce actual healthcare expenditures, so further practical cost-effective studies are needed. Moreover, future developments may introduce more affordable consumables, potentially expanding ENB’s application scenarios. In conclusion, while the current application of ENB in TBLC remains limited, it holds special value in certain scenarios, such as offering a non-radiative option for pregnant patients with ILD who require lung biopsy, which has been previously reported [27, 28]. Pregnant patients were not included in this study, necessitating further research to explore ENB’s potential benefits for this patient group.
There are also some limitations to our study. First, the sample size of the study was very small, which might lead to random error. Although the results showed a significant difference in the accuracy of ENB versus fluoroscopy navigation, the reliability of the results may be low. Second, the decision to use CBCT as the benchmark for navigation accuracy is open to debate, given the scarcity of studies on CBCT’s application in guiding TBLC in ILD patients. Our study’s approach—incorporating CBCT for corrective measures alongside ENB versus fluoroscopy—might have limited our ability to accurately determine the actual complication rates and diagnostic effectiveness of ENB or fluoroscopy-guided TBLC. Future research involving larger cohorts and multi-center trials without CBCT correction for ENB-guided TBLC, is essential to more definitively ascertain ENB’s efficacy in TBLC navigation for ILD patients.
Conclusions
We performed the first comparison of the accuracy of ENB and fluoroscopy in TBLC navigation in patients with ILD in a prospective pilot trial. When CBCT images were used as reference, TBLC navigation with ENB was significantly more accurate than traditional fluoroscopy. Further studies are still required to explore the application prospect of ENB in TBLC navigation in patients with ILD.
Availability of data and materials
The data that support the findings of this study are available from Dr. GZ and Dr. HD. These data were used under license for the current study, so these data are not publicly available. However, the data are available from the authors upon reasonable request and with permission from corresponding authors.
Abbreviations
- CBCT:
-
Cone beam computed tomography
- DLCO:
-
Diffusing capacity of the lung for carbon monoxide
- ENB:
-
Electromagnetic navigation bronchoscopy
- EWC:
-
Extended Working Channel
- FVC:
-
Forced vital capacity
- HRCT:
-
High-resolution computed tomography
- IQR:
-
Interquartile range
- ILD:
-
Interstitial lung disease
- MDD:
-
Multidisciplinary discussion
- MDT:
-
Multidisciplinary team
- NSIP:
-
Non-specific interstitial pneumonia
- radial-EBUS:
-
Radial endobronchial ultrasound
- SLB:
-
Surgical lung biopsy
- TBLC:
-
Transbronchial lung cryobiopsy
- uILD:
-
Unclassifiable interstitial lung disease
References
Korevaar DA, Colella S, Fally M, Camuset J, Colby TV, Hagmeyer L, Hetzel J, Maldonado F, Morais A, Ravaglia C, et al. European Respiratory Society guidelines on transbronchial lung cryobiopsy in the diagnosis of interstitial lung diseases. Eur Respir J. 2022;60(5).
Cooley J, Balestra R, Aragaki-Nakahodo AA, Caudell Stamper DN, Sriprasart T, Swank Z, Baughman RP, Benzaquen S. Safety of performing transbronchial lung cryobiopsy on hospitalized patients with interstitial lung disease. Respir Med. 2018;140:71–6.
Zhou G, Ren Y, Li J, Yang T, Su N, Zhao L, Wang D, Li Y, Tian Z, Liu R, et al. Safety and diagnostic efficacy of cone beam computed tomography-guided transbronchial cryobiopsy for interstitial lung disease: a cohort study. Eur Respir J. 2020;56(2).
Troy LK, Grainge C, Corte TJ, Williamson JP, Vallely MP, Cooper WA, Mahar A, Myers JL, Lai S, Mulyadi E, et al. Diagnostic accuracy of transbronchial lung cryobiopsy for interstitial lung disease diagnosis (COLDICE): a prospective, comparative study. Lancet Respir Med. 2020;8(2):171–81.
Kheir F, Uribe Becerra JP, Bissell B, Ghazipura M, Herman D, Hon SM, Hossain T, Khor YH, Knight SL, Kreuter M, et al. Transbronchial lung Cryobiopsy in patients with interstitial lung disease: a systematic review. Ann Am Thorac Soc. 2022;19(7):1193–202.
Fruchter O, Fridel L, Rosengarten D, Raviv Y, Rosanov V, Kramer MR. Transbronchial cryo-biopsy in lung transplantation patients: first report. Respirology. 2013;18(4):669–73.
Colella S, Haentschel M, Shah P, Poletti V, Hetzel J. Transbronchial lung Cryobiopsy in interstitial lung diseases: best practice. Respiration. 2018;95(6):383–91.
Maldonado F, Danoff SK, Wells AU, Colby TV, Ryu JH, Liberman M, Wahidi MM, Frazer L, Hetzel J, Rickman OB, et al. Transbronchial Cryobiopsy for the diagnosis of interstitial lung diseases: CHEST guideline and expert panel report. Chest. 2020;157(4):1030–42.
Sriprasart T, Aragaki A, Baughman R, Wikenheiser-Brokamp K, Khanna G, Tanase D, Kirschner M, Benzaquen S. A single US Center experience of Transbronchial lung Cryobiopsy for diagnosing interstitial lung disease with a 2-scope technique. J Bronchology Interv Pulmonol. 2017;24(2):131–5.
Benn BS, Romero AO, Bawaadam H, Ivanick N, Lum M, Krishna G. Cone beam CT guidance improves Transbronchial lung Cryobiopsy safety. Lung. 2021;199(5):485–92.
Chen LC, Yang SM, Malwade S, Chang HC, Chang LK, Chung WY, Ko JC, Yu CJ. Cone-beam computed-tomography-derived augmented fluoroscopy-guided biopsy for peripheral pulmonary nodules in a hybrid operating room: a case series. Diagnostics (Basel). 2023;13(6).
Leong S, Ju H, Marshall H, Bowman R, Yang I, Ree AM, Saxon C, Fong KM. Electromagnetic navigation bronchoscopy: a descriptive analysis. J Thorac Dis. 2012;4(2):173–85.
Mehta AC, Hood KL, Schwarz Y, Solomon SB. The evolutional history of electromagnetic navigation bronchoscopy: state of the art. Chest. 2018;154(4):935–47.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, Bruno DS, Chang JY, Chirieac LR, D’Amico TA, et al. Non-small cell lung Cancer, version 3.2022, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw. 2022;20(5):497–530.
Taton O, Bondue B, Gevenois PA, Remmelink M, Leduc D. Diagnostic yield of combined pulmonary Cryobiopsies and electromagnetic navigation in small pulmonary nodules. Pulm Med. 2018;2018:6032974.
Kronborg-white S, Bendstrup E, Gori L, Luzzi V, Madsen LB, Poletti V, Rasmussen TR, Trigiani M, Vezzosi S, Tomassetti S. A pilot study on the use of the super dimension navigation system for optimal cryobiopsy location in interstitial lung disease diagnostics. Pulmonology. 2023;29(2):119–23.
Jiang S, Liu X, Chen J, Ma H, Xie F, Sun J. A pilot study of the ultrathin cryoprobe in the diagnosis of peripheral pulmonary ground-glass opacity lesions. Transl Lung Cancer Res. 2020;9(5):1963–73.
Ravaglia C, Bonifazi M, Wells AU, Tomassetti S, Gurioli C, Piciucchi S, Dubini A, Tantalocco P, Sanna S, Negri E, et al. Safety and diagnostic yield of Transbronchial lung Cryobiopsy in diffuse parenchymal lung diseases: a comparative study versus video-assisted thoracoscopic lung biopsy and a systematic review of the literature. Respiration. 2016;91(3):215–27.
Barisione E, Salio M, Romagnoli M, Praticò A, Bargagli E, Corbetta L. Competence in transbronchial cryobiopsy. Panminerva Med. 2019;61(3):290–7.
Dhooria S, Mehta RM, Srinivasan A, Madan K, Sehgal IS, Pattabhiraman V, Yadav P, Sivaramakrishnan M, Mohan A, Bal A, et al. The safety and efficacy of different methods for obtaining transbronchial lung cryobiopsy in diffuse lung diseases. Clin Respir J. 2018;12(4):1711–20.
Harari S, Cereda F, Pane F, Cavazza A, Papanikolaou N, Pelosi G, Scarioni M, Uslenghi E, Zompatori M, Caminati A. Lung Cryobiopsy for the diagnosis of interstitial lung diseases: a series contribution to a debated procedure. Medicina (Kaunas). 2019;55(9).
Inomata M, Kuse N, Awano N, Tone M, Yoshimura H, Jo T, Minami J, Takada K, Muto Y, Fujimoto K, et al. Utility of radial endobronchial ultrasonography combined with transbronchial lung cryobiopsy in patients with diffuse parenchymal lung diseases: a multicentre prospective study. BMJ Open Respir Res. 2021;8(1).
Li X, Pan J, Ma Y, Ren Y, Gao BL. Diagnosis of diffuse parenchymal lung diseases using transbronchial cryobiopsy guided by endobronchial ultrasound compared to clinicoradiological diagnosis. Quant Imaging Med Surg. 2022;12(2):1139–48.
Cicenia J, Avasarala SK, Gildea TR. Navigational bronchoscopy: a guide through history, current use, and developing technology. J Thorac Dis. 2020;12(6):3263–71.
Ozgul G, Cetinkaya E, Ozgul MA, Abul Y, Gencoglu A, Kamiloglu E, Gul S, Dincer HE. Efficacy and safety of electromagnetic navigation bronchoscopy with or without radial endobronchial ultrasound for peripheral lung lesions. Endosc Ultrasound. 2016;5(3):189–95.
Ma L, Fang Y, Zhang T, Xue P, Bo L, Liu W, Fu E. Comparison in efficacy and safety of forceps biopsy for peripheral lung lesions guided by endobronchial ultrasound-guided sheath (EBUS-GS) and electromagnetic navigation bronchoscopy combined with EBUS (ENB-EBUS). Am J Transl Res. 2020;12(8):4604–11.
Ie S, Alper B, Szerlip HM. Respiratory bronchiolitis: an unusual cause of pulmonary infiltrates in a pregnant woman. Am J Med Sci. 2000;320(3):219–21.
Lee YJ, Kim YS. Cryptogenic organizing pneumonia associated with pregnancy: a case report. World J Clin Cases. 2022;10(6):1946–51.
Acknowledgements
The authors thank colleagues from Department of Pulmonary and Critical Care Medicine and Department of Rheumatology, China-Japan Friendship Hospital for their assistance in diagnosis and management of patients.
Funding
This study was supported by National Key Research and Development Program of China (2021YFC2500700) and Special Project of Clinical and Translational Medicine, Chinese Academy of Medical Sciences (2021-I2M-C&T-B-088). The research was designed, conducted, and analyzed by the authors independently of the funding sources. The research was designed, conducted, and analyzed by the authors independently of the funding sources.
Author information
Authors and Affiliations
Contributions
SW, GZ and HD conceived of the study. SW, JY and GZ participated in the design of the study and coordination. SL, JG and YR participated in the enrolment of the cases. LZ and ML participated in multidisciplinary discussion of enrolled cases. DW, YL, ZT and WL participated in the procedure of TBLC. SW and GZ performed the statistical analysis. SW drafted the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the China-Japan Friendship Hospital (2017-25-1), and written informed consent was obtained from all patients. This study was performed in accordance with the Declaration of Helsinki.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, S., Yang, J., Luo, S. et al. The accuracy of electromagnetic navigation bronchoscopy compared to fluoroscopy in navigation of transbronchial lung cryobiopsy in patients with interstitial lung disease. BMC Pulm Med 24, 108 (2024). https://doi.org/10.1186/s12890-024-02925-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-02925-x