Abstract
Background
This study assessed hospitalisation frequency and related clinical outcomes among adult Aboriginal Australians with bronchiectasis over a ten-year study period.
Method
This retrospective study included patients aged ≥ 18 years diagnosed with bronchiectasis between 2011 and 2020 in the Top End, Northern Territory of Australia. Hospital admissions restricted to respiratory conditions (International Classification of Diseases (ICD) code J) and relevant clinical parameters were assessed and compared between those with and without hospital admissions.
Results
Of the 459 patients diagnosed to have bronchiectasis, 398 (87%) recorded at least one respiratory related (ICD-J code) hospitalisation during the 10-year window. In comparison to patients with a recorded hospitalisation against those without—hospitalised patients were older (median 57 vs 53 years), predominantly females (54 vs 46%), had lower body mass index (23 vs 26 kg/m2) and had greater concurrent presence of chronic obstructive pulmonary disease (COPD) (88 vs 47%), including demonstrating lower spirometry values (forced vital capacity (FVC) and forced expiratory volume in 1 s (FEV1) (median FVC 49 vs 63% & FEV1 36 vs 55% respectively)). The total hospitalisations accounted for 3,123 admissions (median 4 per patient (IQR 2, 10)), at a median rate of 1 /year (IQR 0.5, 2.2) with a median length of 3 days (IQR 1, 6). Bronchiectasis along with COPD with lower respiratory tract infection (ICD code-J44) was the most common primary diagnosis code, accounting for 56% of presentations and 46% of days in hospital, which was also higher for patients using inhaled corticosteroids (81 vs 52%, p = 0.007). A total of 114 (29%) patients were recorded to have had an ICU admission, with a higher rate, including longer hospital stay among those patients with bronchiectasis and respiratory failure related presentations (32/35, 91%). In multivariate regression model, concurrent presence of COPD or asthma alongside bronchiectasis was associated with shorter times between subsequent hospitalisations (-423 days, p = 0.007 & -119 days, p = 0.02 respectively).
Conclusion
Hospitalisation rates among adult Aboriginal Australians with bronchiectasis are high. Future interventions are required to explore avenues to reduce the overall morbidity associated with bronchiectasis among Aboriginal Australians.
Similar content being viewed by others
Background
Bronchiectasis is a chronic pulmonary condition characterised by a cycle of recurrent lower respiratory tract infections and airway inflammation giving rise to frequent hospitalisations and reduced quality of life [1, 2]. Globally, there is emerging evidence in the literature to suggest that presence of bronchiectasis is associated with a significant degree of hospitalisations and high mortality rates [3,4,5,6]. However, these global studies portray bronchiectasis as largely a disease of the elderly [7,8,9]. In the First Nations Indigenous people’s context, for the majority bronchiectasis is a lifelong disease, or at best an early adulthood to middle-age disease [10,11,12,13] (from here on “Indigenous” is used to refer to global First nations populations, while “Aboriginal Australian” is used to specifically refer to Australia’s’ First Nations people). In the paediatric Aboriginal Australian population, bronchiectasis incidence is one among the highest in the world [14, 15], and the prevalence remains significantly higher among Aboriginal Australians compared to non-Aboriginal Australian adults [16], as well as among global Indigenous populations, as observed among the New Zealand’s First Nations Indigenous Māori and Pacific Islander populations compared to New Zealand’s non-Indigenous population [17, 18].
Presence of bronchiectasis can lead to a greater number of hospitalisations and associated mortality both as direct results of bronchiectasis exacerbations per se or as an indirect contributor to other comorbidities [19,20,21,22,23]. Among both Aboriginal Australians and among Indigenous populations worldwide the prevalence of multimorbidity is high [24,25,26,27]. Indeed, concurrent presence of bronchiectasis and chronic obstructive pulmonary disease (COPD) has been reported in up to 50% of adult Aboriginal Australians [28,29,30,31,32,33]. Furthermore, hospitalisation frequency related to bronchiectasis, and bronchiectasis specific mortality rates appear to be significantly higher among Indigenous patients than their non-Indigenous counterparts [34,35,36,37]. However, although a higher hospitalisation frequency amongst Indigenous patients with bronchiectasis has been described in the existing literature, there is little data regarding other pertinent factors such as principal reasons for hospital presentation, length of hospital stays, utilisation of intensive care unit (ICU) or mechanical ventilation and therapeutic interventions, in particular use of inhaled pharmacotherapy. In the recent past, a significant prevalence of chronic respiratory disorders, including bronchiectasis among adult Aboriginal Australians in the Northern Territory (NT) of Australia has begun to be elucidated [10, 24]. Hence, it is timely to investigate in greater detail hospital presentations and related outcomes among adult Aboriginal Australians with bronchiectasis. Therefore, this study sets forth to describe the demographics, relevant clinical parameters, frequency and reason for hospitalisations, length of stay, treatment details, utilisation of ICU and ventilation in an adult Aboriginal Australian cohort diagnosed to have bronchiectasis over a ten-year period (2011–2020) in the Top End Health Service (TEHS) region of the NT of Australia.
Methods
Study setting and study population
This study was conducted at the respiratory and sleep division based at the Royal Darwin Hospital (RDH), a university affiliated tertiary care teaching hospital and Darwin Respiratory and Sleep Health, Darwin Private Hospital, within the TEHS, NT region of Australia. The TEHS region within the NT covers approximately 35% or 475,338 km2 of the total area of the NT and contains an estimated adult population (≥ 18 years) of 129,000 people, representing almost 80% of the total NT adult population [38, 39]. In the TEHS, 22% of the adult population are Aboriginal Australians, of whom approximately 77% reside in remote or very remote communities as defined by the Australian Statistical Geographic Standard Level 4 or Level 5 [40].
Ethics
This study was approved by the Human Research Ethics governance/committee of the TEHS, NT and Menzies School of Health Research (Reference: HREC; 2019–3547). The authors acknowledge the rights of Australian Aboriginal people involved in this study, and as such conducted and reported according to strengthening and reporting of health research involving Aboriginal people [41], including consultations with institute Aboriginal representatives. Individual patient consent was not required, as it was a retrospective study and no active interventions were undertaken and the need for individual consent was waived by the Human Research Ethics governance/committee of the TEHS, NT and Menzies School of Health Research.
Study participants
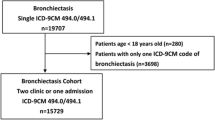
This study is a part of a larger project examining various aspects of bronchiectasis disease profiles among the adult Aboriginal Australian population residing in the TEHS health district region of the NT of Australia, which is inclusive of all adult Australian Aboriginal patients aged ≥ 18 years identified to have bronchiectasis via chest Computed tomography (CT) scan between 2011 and 2020. Hospital admission data for this period (1 Jan 2011 – 31 Dec 2020) was assessed across the three hospitals in the TEHS regions (RDH, Katherine District Hospital and Gove District Hospital) (Fig. 1).
Clinical data examined
Demographics, residence locality, smoking status, concurrent medical co-morbidities, including other non- bronchiectasis respiratory conditions, spirometry parameters (Forced expiratory volume in 1 s (FEV1), Forced vital capacity (FVC) & FEV1/FVC) when available and chest CT scan results for location of bronchiectasis were recorded. Hospital admissions restricted to those being respiratory related (International Classification of Diseases (ICD) code J and sub class) were included for analysis. Principal diagnosis, frequency, length of hospital stay and time between hospitalisations were assessed. Hospitalisation rate was defined as the number of hospitalisations divided by the time from the date of the first recorded hospitalisation within the study period until either the end of the study period, or death – whichever occurred first. ICU visits and mechanical ventilation data were collected at the person level and not broken down per visit. Further details on methods and study design are available form a recent report from our centre [16].
Statistical analysis
Continuous data were displayed as median (interquartile range (IQR)) and categorical data as number (%). Differences in demographic and clinical variables between hospitalised and non-hospitalised patients were tested via quantile regression (continuous parameters) or logistic regression (categorical parameters). Differences in the proportion of patients with each specific ICD code, the proportion of total visits with that code, and the median length of stay per code between patients using and not using ICS were tested via logistic and quantile regressions respectively. Univariate and multivariate mixed regression models were used to test the effect of demographic and clinical parameters on total time spent in hospital, and median length of time between hospitalisations for patients who recorded at least two hospitalisations, reporting results as beta (95% confidence interval (CI)). Stepwise regression was utilised to define the model for the multivariate regressions. Parameters for which the entire cohort did not have complete data (BMI, lung function parameters and smoking status) were excluded from the model, while age, sex and remote/urban residence were forced inclusions, with other parameters excluded at a threshold of p > 0.1. A second model incorporated all parameters with forced inclusion of age, sex and remote/urban residence, and is displayed in Supplement 1. Romano-Wolff correction was utilised for multiple hypothesis adjustment, with 150 bootstrap replications. All analysis was conducted in STATA IC 15 (College Station, Texas).
Results
Hospital admission data
Of the 459 patients included in this database, 398 patients (87%) recorded at least one respiratory related hospitalisation during the 10-year study window until 31 December 2020, and 229 (50.1%) recorded at least one admission within the last year (median rate 1 (IQR 0, 2)) (Table 1). Two patients recorded over 100 hospitalisations during the study window, potentially skewing the results and thus were removed from further analysis. Patients who recorded a hospital admission showed similar age, gender, remoteness, BMI and smoking status distribution as those without any hospital admissions (Table 1). However, patients with a hospital admission had reduced FEV1 (36% predicted (IQR 27, 48.5) vs. 55% predicted (IQR 51, 63)). The prevalence of comorbid COPD was higher in the hospitalised group (88 vs. 48%, p = 0.029), however there was no difference in the prevalence of other comorbidities. Inhaled pharmacotherapy, including ICS prescriptions were recorded at almost twice the rate among the hospitalised patient group compared to the non-hospitalised patients (p = 0.029).
Length of hospital admission data
A total of 3,123 hospital admissions were available to be assessed, with patients recording a median 4 (IQR 2, 10) admissions over the study period. The length of time from patients first admission until the end of the study period or death was a median 5.4 years (IQR 3.2, 8.1), resulting in an overall median hospital admission rate of 1 /year (IQR 0.5, 2.2). The median length of individual hospital admissions was 3 days (IQR 1, 6), with 390 (12.5%) same day separations and 162 (5.2%) of greater than two weeks duration. In total, patients with at least one hospital admission spent a median 21 days (IQR 9, 52) in hospital across the study period. At least two hospitalisations were recorded for 327/396 (82%) patients. Of the 2,727 hospital admissions among these patients 926 (34%) occurred within 30 days of a prior hospitalisation, 349 (12.8%) within 30–60 days from a prior hospitalisation and the remaining 1,452 (53.3%) more than 60 days after.
Respiratory related hospital admission as per ICD separation codes
Hospital admissions coded J44 (COPD with lower respiratory tract infection) were the most common, with 69.2% of patients recording at least one J44 visit (Table 2) (the description of individual ICD codes is detailed in supplementary file 2). Furthermore, J44 visits accounted for 55.7% of hospital presentations and 46% of total days in hospital. Pneumonia related visits (J15) and those related to respiratory failure (J96) however were associated with the longest stays in hospital per visit (J15, median 6 days (IQR 3, 10.5) and J96, median 7 days (IQR 4, 12)).
Hospital admission and Inhaled pharmacotherapy use data
Among the patients with at least one hospital admission, 232 (58.6%) had recorded use of ICS. Among these 188/232 (81%) recorded at least one J44 related hospitalisation, a greater proportion than among those patients not using ICS 86/164 (52.4%) (RW p-value = 0.007). There were no differences in the proportion of patients presenting with other codes, the total number of presentations for any codes, nor the length of time spent in hospital between ICS and non-ICS use.
ICU admission data
Of the 396 patients with a hospital admission, 114 (28.8%) had at least one ICU admission, among whom the median total number of hours spent in ICU was 128 h (IQR 68, 236) (Supplementary file 3). A greater proportion of patients with a J96 code recorded an ICU admission (91.4%) compared to any other code. Patients who recorded at least one J85 (median 440 h (IQR 7, 652)) or J96 (median 215 h (IQR 106, 278.5)) hospital admission recorded more hours in ICU than other patients. Mechanical ventilation was recorded for 32 patients (8.1%), for whom the median total number of hours on ventilation was 48.5 h (IQR 30.5, 145.5). Almost half (43%) of patients with a J96 code recorded mechanical ventilation.
Regression analysis
In univariate regression models each 10% decrease in FEV1 was associated with a 6.33-day (95% CI 3.43, 9.23) increase in total time spent in hospital, while each 10% decrease in FVC was associated with a 6-day (95% CI 2.89, 9.12) increase. Comorbid COPD (19-days (95% CI 10.13, 27.87)), asthma (13-days (95% CI 6.18, 19.82)), and heart failure (23-days (95% CI 12.33, 33.67)) were each associated with increases in the total number of days spent in hospital (Table 3).
In the multivariate model, comorbid COPD (12.88-days (95% CI 2.28, 23.48)), HTN (10.13-days (95% CI 3.32, 16.94)) and heart failure (15.36-days (95% CI 4.40, 26.32)) were the factors associated with increased time in hospital (Table 4). Statistical significance for all associations however was attenuated following Romano-Wolff correction.
Regression analysis for patients with two or more hospital admissions
At least two hospitalisations were recorded for 327/396 (82%) patients. In univariate mixed regression models, there was reduced length of time between hospitalisations among patients with comorbid COPD (-475.9 days (95% CI -649.31, -302.5)), asthma (-129.22 days (95% CI -229.09, -29.35)), and with right lower lobe involvement (-154.79 days (95% CI -249.15, -60.42)), (Table 4). In the multivariate model, comorbid COPD (-423.37 days (95% CI -598.65, -2242.09)) and asthma (-118.83 days (95% CI -222.06, -15.6)) remained associated with reduced interval between hospitalisations.
Discussion
In this study, 87% of bronchiectasis patients were noted to have had at least one respiratory related hospital admission during the 10-year study period, with 29% requiring ICU admission. Patients spent a median of 3 weeks in hospital, and 82% of patients had recurrent admissions. Patients who required hospitalisation appeared to be in poorer health than other patients as evidenced by a higher rate of comorbidities, lower lung function values and greater prescription rates of inhaled pharmacotherapy. Presence of COPD or asthma were associated with greater lengths of time spent in hospital, and shorter intervals between hospitalisations.
In the global non-Indigenous populations, hospital admission data and factors associated with mortality, including the economic burden secondary to bronchiectasis are well documented [3,4,5,6,7, 19,20,21,22,23]. Among the adult Indigenous population however, literature surrounding hospital admissions is sparse – despite a higher burden of chronic respiratory disease [10, 24]. On the backdrop of poorer socioeconomic environment, alongside geographic, social and systemic barriers to healthcare, Indigenous people typically display a greater degree of multimorbidity, which in turn may alter the way in which respiratory diseases manifest in comparison to their non-Indigenous counterparts [28, 31, 42,43,44,45,46,47,48].
The majority of patients (69.4%) had an admission secondary to COPD (J44), similar to what has been observed in previous reports [49]. Although, indeed it is difficult to ascertain if bronchiectasis is a primary or a secondary factor driving hospital admission rates in the presence of multi-respiratory morbidity, including concurrent presence of bronchiectasis and COPD among Aboriginal Australians [28], however, it is reasonable to speculate that the presence of bronchiectasis among patients with COPD would have perpetuated exacerbation rates and subsequent hospitalisations. Previous studies in other population settings have demonstrated worse outcomes when bronchiectasis co-exists with COPD, especially in the presence of a smoking history, alongside lower lung function parameters [3, 5]. Indeed, in the current cohort with hospitalisations, COPD was recorded in 88%, a smoking history in 85%, and median FVC & FEV1 of 49 & 36% predicted respectively. Furthermore, a 10% reduction in FEV1 was associated with a mean 5.3 day increase in the total number of days in hospital, although significance was attenuated on multiple hypotheses correction. Previous reports have shown that among adult Aboriginal Australians, lung function parameters are substantially lower compared to their Caucasian counterparts [50,51,52,53,54], thus, it may be indicative that presence of lower lung function parameters could be a predictor for increased length of hospital admissions among Indigenous patients more generally, including patients with bronchiectasis. Therefore, it is reasonable to speculate that improving lung function parameters with targeted interventions among Indigenous patients with respiratory disorders will reduce hospital admission rates and length of hospitalisation. Furthermore, Bronchiectasis and COPD overlap syndrome (BCOS) is increasingly recognized [55]. Although both these conditions share several similar clinical features, the management of these conditions differs; hence, in clinical practice, differentiating if COPD or bronchiectasis is the primary disorder, especially when inhaled pharmacotherapy is considered, is vital. In addition to classical clinical manifestations, chest CT scan finding will be of heightened value in differentiating which of these conditions is predominant [56].
Among patients with bronchiectasis, a lower BMI is reported to be an independent predictor of mortality [57]. In our study we observed BMI to be lower among patients with hospital admissions– though we did not test the effect of BMI on mortality specifically in this study. If a lower BMI among Aboriginal Australian patients would translate to poorer long-term outcomes is not known currently and only prospective studies will elucidate this aspect. However, it is noteworthy that the median BMI in the current cohort is lower than the BMI reported previously among non-Aboriginal Australian cohort with bronchiectasis [58].
It is vital to note that the majority of patients in this study resided in remote/rural localities (92%) (Fig. 1). Hence, during exacerbations of airway disease and when needing hospital admissions, patients are inevitably retrieved to secondary or tertiary care centres, therefore incurring substantial cost to the health system [59, 60]. Nevertheless, the economic burden of managing patients with bronchiectasis in this region is not exactly known, especially for adult Aboriginal Australian people residing in remote and rural communities [61]. However, a study from Brazil estimated R$28 million (approx. AUD 14 million) in a twelve-year period for an average hospital stay of 8.1 days [21]. It is reasonable to speculate the economic cost could be substantially higher in the Australian setting, especially when considering transporting patients from remote communities by air and relocating family and caregivers. Due to limited access to specialist health care in remote Aboriginal Australian communities the threshold to transfer to a tertiary institution during exacerbation of airway disease may be low. This may be the reason for observing only 12.5% of hospitalisations were recorded as a same day separation. Hence, it is apparent that addressing bronchiectasis and other respiratory diseases at the community and primary health care level, may be an avenue to prevent recurrent hospital admissions and associated health care utilisation and expenditure [62]. Moreover, patients are more likely to show adherence to treatment interventions for disease management with continuity of care at community and primary health care level.
Although currently literature portrays a high bronchiectasis disease burden and associated adverse health outcomes globally, innovative preventative or therapeutic interventions are negligible, other than the proven benefits of chest physiotherapy/airway clearance techniques and classic mucolytic/mucoactive agents [63, 64]. In this study we did not explore specific treatment interventions, either in the ambulatory setting or during acute hospital admissions that would have any influence on recurrent hospital admission rates or for the length of stay. However, among patients prescribed ICS, we observed a higher proportion had an admission related to ICD code J44 compared to patients with no ICS prescription. Utilisation of ICS among patients with bronchiectasis is controversial and may be detrimental [65]. Previous studies from our centre had reported higher use of ICS among Indigenous patients with bronchiectasis and to have a significant decline in lung function parameters with ICS [66, 67]. It is unclear if ICS is over prescribed due to concurrent presence of other airway diseases such as COPD and asthma in this cohort. However, prospective studies are needed to define if increased hospital rates are related to natural disease progression and recurrent exacerbation or if they are related to aftermath effects of ICS use [68].
This study has demonstrated that the bronchiectasis disease burden is substantial, as is its impact on hospital admission rates and overall poor outcomes among adult Aboriginal Australians. In the largely non-Aboriginal Australian bronchiectasis registry, 29% of patients recorded a respiratory hospitalisation in the last year [58], while in the current Aboriginal Australian cohort, 50% did so. Moreover, despite evidence in the literature dating back to the 1980’s to suggest hospital admission rates are substantially higher among Aboriginal Australian patients in comparison to their non-Aboriginal counterparts with bronchiectasis [69], hospital admission rates continue to remain substantially high in this population, as evident form our current study. Furthermore, there has been no substantial interventions to address this disparity in the last three decades [70]. Therefore, it is apparent that it is inevitable that the noted higher morbidity secondary to bronchiectasis is likely to continue to show a grim trend for the future, unless clinically and culturally appropriate interventions are implemented urgently to address the overall respiratory disease burden among adult Aboriginal Australians, so that, in particular, bronchiectasis does not continue to remain a neglected chronic lung disease among Aboriginal Australians for the foreseeable future [71].
Limitations
This study’s outcomes pertain to Aboriginal Australian people residing in the TEHS region of the NT of Australia and the results represented in this study cannot be generalised to the wider Aboriginal populations in Australia or for Indigenous people globally. We did not assess patients’ presentations to primary health care or at remote community health centres with exacerbation of their airway disease and interventions undertaken, as this was beyond the scope of this study. We also did not have data to represent therapeutic interventions during hospital admissions, which would have provided more insight for those patients with recurrent hospital admissions, especially if interventions such as chest physiotherapy/sputum clearance techniques were implemented. Moreover, with a higher presence of COPD in this population, it is uncertain if bronchiectasis is a primary or a secondary cause for hospital admissions. Furthermore, there may be a bias for those patients recorded to have no hospital admissions, as it is possible despite exacerbations of airway disease, due to remoteness and geographical isolations they did not present to hospital for admission and also spirometry data was not available in all patients. In addition, as this study was retrospective in nature, this would have introduced potential bias in the outcomes observed. Nonetheless, this is the first study to represent hospital admission data in an adult Aboriginal Australian cohort, in this region. The outcomes represented in this study may be an avenue for health organisations and stakeholders to implement strategies to address to close the respiratory health gap among adult Aboriginal Australians and Indigenous people globally.
Conclusion
This study has demonstrated that respiratory related hospital and ICU admission rates and frequency are alarmingly high among adult Aboriginal Australians secondary to bronchiectasis. Concurrent presence of asthma, COPD, heart failure and reduced lung function parameters are associated with more time spent during hospital admission. The majority of recurrent hospitalisations were observed in the presence of underlying COPD or asthma. Future interventions are required at primary/community health care level to prevent recurrent hospitalisations, ongoing further morbidity and mortality among adult Aboriginal Australians suffering from bronchiectasis.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- FVC:
-
Forced vital capacity
- FEV1 :
-
Forced expiratory volume in 1 s
- HTN:
-
Hypertension
- ICD:
-
International Classification of Diseases
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- NT:
-
Northern Territory
- RDH:
-
Royal Darwin hospital
- TEHS:
-
Top End Health Service
References
King PT. The pathophysiology of bronchiectasis. Int J Chron Obstruct Pulmon Dis. 2009;4:411–9.
Mäntylä J, Mazur W, Törölä T, Bergman P, Kauppi P. In bronchiectasis, poor physical capacity correlates with poor quality of life. Eur Clin Respir J. 2022; 9:1, 2095104. https://doi.org/10.1080/20018525.2022.2095104.
Choi H, Yang B, Kim YJ, et al. Increased mortality in patients with non cystic fibrosis bronchiectasis with respiratory comorbidities. Sci Rep. 2021;11(1):7126. https://doi.org/10.1038/s41598-021-86407-8.
Sin S, Yun SY, Kim JM, et al. Mortality risk and causes of death in patients with non-cystic fibrosis bronchiectasis. Respir Res. 2019;20:271. https://doi.org/10.1186/s12931-019-1243-3.
Goeminne PC, Nawrot TS, Ruttens D, Seys S, Dupont LJ. Mortality in non-cystic fibrosis bronchiectasis: A prospective cohort analysis. Respir Med. 2014;108(2):287–96.
McDonnell MJ, Aliberti S, Goeminne PC, et al. Comorbidities and the risk of mortality in patients with bronchiectasis: an international multicentre cohort study. Lancet Respir Med. 2016;4(12):969–79. https://doi.org/10.1016/S2213-2600(16)30320-4.
Quint JK, Millett ER, Joshi M, et al. Changes in the incidence, prevalence and mortality of bronchiectasis in the UK from 2004 to 2013: a population-based cohort study. Eur Respir J. 2016;47(1):186–93.
Ringshausen FC, Rademacher J, Pink I, et al. Increasing bronchiectasis prevalence in Germany, 2009–2017: a population-based cohort study. Eur Respir J. 2019;54(6):1900499. https://doi.org/10.1183/13993003.00499-2019.
Seitz AE, Olivier KN, Adjemian J, Holland SM, Prevots DR. Trends in bronchiectasis among medicare beneficiaries in the United States, 2000 to 2007. Chest. 2012;142(2):432–9.
Howarth T, Heraganahally SS, Heraganahally SS. Bronchiectasis among adult First Nations Indigenous people – A scoping review. Curr Respir Med Rev. 2023;19:36–51.
Schutz KL, Fancourt N, Chang AB, et al. Transition of pediatric patients with bronchiectasis to adult medical care in the Northern Territory: A retrospective chart audit. Front Pediatr. 2023;11:1184303. https://doi.org/10.3389/fped.2023.1184303.
McCallum GB, Oguoma VM, Versteegh LA, et al. Comparison of profiles of first nations and non-first nations children with bronchiectasis over two 5-year periods in the northern territory. Australia Chest. 2021;160(4):1200–10. https://doi.org/10.1016/j.chest.2021.04.057.
Barton J, Scott L, Maguire G. Bronchiectasis in the Kimberley region of Western Australia. Aust J Rural Health. 2018;26:238–44.
Chang AB, Grimwood K, Mulholland EK, Torzillo PJ; Working Group on Indigenous Paediatric Respiratory Health. Bronchiectasis in indigenous children in remote Australian communities. Med J Aust 2002;177:200–204.
Valery PC, Torzillo PJ, Mulholland K, et al. Hospital-based case-control study of bronchiectasis in indigenous children in Central Australia. Pediatr Infect Dis J. 2004;23:902–8.
Gibbs C, Howarth T, Ticoalu A, et al. Bronchiectasis among Indigenous adults in the Top End of the Northern Territory, 2011–2020: a retrospective cohort study. Med J Aust. 2024. https://doi.org/10.5694/mja2.52204.
Twiss J, Metcalfe R, Edwards E, Byrnes C. New Zealand national incidence of bronchiectasis ‘“too high”’ for a developed country. Arch Dis Child. 2005;90:737–40.
de Boer S, Lewis CA, Fergusson W, Ellyett K, Wilsher ML. Ethnicity, socioeconomic status and the severity and course of non-cystic fibrosis bronchiectasis. Int Med J. 2018;48:845–50.
Mateus SP, Ribeiro-Alves M, Salles REB, et al. Mortality and comorbidities in patients with bronchiectasis over a 3-year follow-up. Medicine (Baltimore). 2022;101(52): e32537. https://doi.org/10.1097/MD.0000000000032537.
Sciosciaa G, Alcaraz-Serranob V, Méndezc R, et al. Factors associated with one year mortality in hospitalised patients with exacerbated bronchiectasis. Arch Bronconeumol. 2022;58:773–7.
Biatobock DR, Paz M da SM, Olmedo DWV, Barlem ELD, Ramos DF. Bronchiectasis: morbidity and mortality in Brazil and its impact on hospitalization rates. Rev. Soc. cient. Parag. 2022;27(1):61–73.
Loebinger MR, Wells AU, Hansell DM, et al. Mortality in bronchiectasis: a long-term study assessing the factors influencing survival. Eur Respir J. 2009;34:843–9. https://doi.org/10.1183/09031936.00003709.
Phua HP, Lim WY, Ganesan G, et al. Epidemiology and economic burden of bronchiectasis requiring hospitalisation in Singapore. ERJ Open Res. 2021;7(4):00334–2021. https://doi.org/10.1183/23120541.00334-2021.
Howarth TP, Jersmann HPA, Majoni SW, et al. The ‘ABC’ of respiratory disorders among adult Indigenous people: asthma, bronchiectasis and COPD among Aboriginal Australians – a systematic review. BMJ Open Respir Res. 2023;10(1): e001738.
Ospina MB, Voaklander DC, Stickland MK. Prevalence of asthma and chronic obstructive pulmonary disease in Aboriginal and non-Aboriginal populations: a systematic review and meta-analysis of epidemiological studies. Can Respir J. 2012;19(6):355–60. https://doi.org/10.1155/2012/825107.
Ospina MB, Voaklander D, Senthilselvan A, et al. Incidence and prevalence of chronic obstructive pulmonary disease among aboriginal peoples in Alberta, Canada. PLoS ONE. 2015;10(4): e0123204. https://doi.org/10.1371/journal.pone.0123204.
Randall DA, Lujic S, Havard A, et al. Multimorbidity among Aboriginal people in New South Wales contributes significantly to their higher mortality. Med J Aust. 2018;209(1):19–23.
Kruavit A, Fox M, Pearson R, Heraganahally S. Chronic respiratory disease in the regional and remote population of the northern territory top end: a perspective from the specialist respiratory outreach service. Aust J Rural Health. 2017;25:275–84.
Heraganahally SS, Wasgewatta SL, McNamara K, et al. Chronic Obstructive Pulmonary Disease In Aboriginal Patients of The Northern Territory Of Australia: A Landscape Perspective. Int J Chron Obstruct Pulmon Dis. 2019;14:2205–17.
Heraganahally SS, Timothy TP, Sorger L. Chest computed tomography findings among adult Indigenous Australians in the Northern Territory of Australia. J Med Imaging Radiat Oncol. 2022;66(3): 337–344 2021. https://doi.org/10.1111/1754-9485.13295.
Mehra S, Chang AB, Lam CK, et al. Bronchiectasis among Australian Aboriginal and Non-Aboriginal patients in the regional and remote population of the Northern Territory of Australia. Rural Remote Health. 2021;21(2):6390. https://doi.org/10.22605/RRH6390.
Heraganahally SS, Wasgewatta SL, McNamara K, et al. Chronic obstructive pulmonary disease with and without bronchiectasis in Aboriginal Australians – a comparative study. Int Med J. 2020;50(12):1505–13. https://doi.org/10.1111/imj.14718.
Heraganahally SS, Howarth TP, Lloyd A, White E, Veale A, Ben Saad H. The Prevalence of Bronchodilator Responsiveness “Asthma” Among Adult Indigenous Australians Referred for Lung Function Testing in the Top End Northern Territory of Australia. J Asthma Allergy. 2022:15 1305–1319.
Roberts ME, Lowndes L, Milne DG, Wong CA. Socioeconomic deprivation, readmissions, mortality and acute exacerbations of bronchiectasis. Intern Med J. 2012;42:e129–36.
Bibby S, Milne R, Beasley R. Hospital admissions for non-cystic fibrosis bronchiectasis in New Zealand. N Z Med J. 2015;128:30–8.
Blackall SR, Hong JB, King P, et al. Bronchiectasis in indigenous and non-indigenous residents of Australia and New Zealand. Respirology. 2018;23(8):743–9. https://doi.org/10.1111/resp.13280.
Heraganahally SS, Ghimire RH, Howarth T, Kankanamalage OM, Palmer D, Falhammar H. Comparison and Outcomes of Emergency Department presentations with Respiratory disorders among Australian Indigenous and non-Indigenous Patients. BMC Emerg Med. 2022;22:11. https://doi.org/10.1186/s12873-022-00570-3.
The 2017–18 annual report for the Department of Health and the Health Services. Northern Territory Government 2018. Available from: Department of Health website: https://www.health.nt.gov.au. Accessed June 2023.
Australian Bureau of Statistics. INGP Indigenous Status and SEXP Sex by AGEP Age by SA3 (UR) [Census Table Builder]. (2021). Accessed June 2023.
Australian Bureau of Statistics. Australian Statistical Geography Standard (ASGS): Volume 5—Remoteness Structure, July 2011. ABS cat. no. 1270.0.55.005. Canberra: Australian Bureau of Statistics. 2013a.
National Health and Medical Research Council. Ethical conduct in research with Aboriginal and Torres Strait Islander Peoples and communities: Guidelines for researchers and stakeholders. Canberra: Commonwealth of Australia; 2018. [Available from URL: https://www.nhmrc.gov.au. Accessed June 2023].
Heraganahally SS, Silva SAMS, Howarth TP, Kangaharan N, Majoni SW. Comparison of clinical manifestation among Australian Indigenous and non- Indigenous patients presenting with pleural effusion. Int Med J. 2022;52(7):1232–41. https://doi.org/10.1111/imj.15310.
Seyedshahabedin MM, Howarth TP, Mo L, Biancardi E, Heraganahally SS. Flexible bronchoscopy indications and outcomes between Indigenous and non-Indigenous patients in the Northern Territory of Australia. Int Med J. 2022. https://doi.org/10.1111/imj.15865.
Heraganahally SS, Mortimer N, Howarth T, et al. Utility and outcomes among indigenous and non-indigenous patients requiring domiciliary oxygen therapy in the regional and rural Australian population. Aust J Rural Health. 2021;29(6):918–26. https://doi.org/10.1111/ajr.12782.
Sze DFL, Howarth TP, Lake CD, Ben Saad H, Heraganahally SS. Differences in the Spirometry Parameters Between Indigenous and Non-Indigenous Patients with COPD: A Matched Control Study. Int J Chron Obstruct Pulmon Dis. 2022;17:869–881.
Howarth TP, Saad HB, Perez AJ, Atos CB, White E, Heraganahally SS. Comparison of diffusing capacity of carbon monoxide (DLCO) and total lung capacity (TLC) between Indigenous Australians and Australian Caucasian adults. PLoS ONE. 2021;16(4): e0248900. https://doi.org/10.1371/journal.pone.0248900.
Heraganahally SS, Kruavit A, Oguoma VM, et al. Sleep apnoea among Australian Aboriginal and Non- Aboriginal patients in the Northern Territory of Australia– a comparative study. Sleep. 2020;43(3):zsz248. https://doi.org/10.1093/sleep/zsz248.
Mishra K, Fazal R, Howarth T, Mutai J, Doss AX, Heraganahally SS. Cystic lung disease in adult Indigenous Australians in the Northern Territory of Australia. J Med Imaging Radiat Oncol. 2023. https://doi.org/10.1111/1754-9485.13593.
Sánchez-Muñoz G, López de Andrés A, Jiménez-García R, et al. Time Trends in Hospital Admissions for Bronchiectasis: Analysis of the Spanish National Hospital Discharge Data (2004 to 2013). PLoS One. 2016;11(9):e0162282. https://doi.org/10.1371/journal.pone.0162282.
Heraganahally S, Howarth TP, White E, Ben SH. Implications of using the GLI-2012, GOLD and Australian COPD-X recommendations in assessing the severity of airflow limitation on spirometry among an Indigenous population with COPD: an Indigenous Australians perspective study. BMJ Open Respir Res. 2021;8: e001135. https://doi.org/10.1136/bmjresp-2021-001135.
Howarth T, Gahreman D, Ben Saad H, Ng L, Heraganahally SS. Correlation of spirometry indices to chest radiology in the diagnosis of chronic airway disease among regional and rural Indigenous Australians. Int Med J. 2023. https://doi.org/10.1111/imj.16023.
Heraganahally SS, Howarth T, Mo L, Sorger L, Ben SH. Critical analysis of spirometric patterns in correlation to chest computed tomography among adult Indigenous Australians with chronic airway diseases. Expert Rev Respir Med. 2021;15(9):1229–38. https://doi.org/10.1080/17476348.2021.1928496.
Heraganahally SS, Howarth T, Sorger L, Ben SH. Sex differences in pulmonary function parameters among Indigenous Australians with and without chronic airway disease. PLoSONE. 2022;17(2): e0263744. https://doi.org/10.1371/journal.pone.0263744.
Heraganahally SS, Howarth T, White E, et al. Lung function parameters among Australian Aboriginal “Apparently Healthy” Adults: an Australian Caucasian and Global Lung Function Initiative (GLI-2012) various ethnic norms comparative study. Expert Rev Respir Med. 2020;23:1–11. https://doi.org/10.1080/17476348.2021.1847649.
Sobala R, De Soyza A. Bronchiectasis and Chronic Obstructive Pulmonary Disease Overlap Syndrome. Clin Chest Med. 2022;43(1):61–70. https://doi.org/10.1016/j.ccm.2021.11.005.
Martinez-Garcia MA, Miravitlles M. Bronchiectasis in COPD patients: more than a comorbidity? Int J Chron Obstruct Pulmon Dis. 2017;12:1401–11. https://doi.org/10.2147/COPD.S132961.Erratum.In:IntJChronObstructPulmonDis.2019;14:245.
Lee JM, Lee SA, Han CH, et al. Body mass index as a predictor of mortality in bronchiectasis: A nationwide population-based study. Respir Med. 2021;180: 106370. https://doi.org/10.1016/j.rmed.2021.106370.
Visser SK, Bye PTP, Fox GJ, et al. Australian adults with bronchiectasis: The first report from the Australian Bronchiectasis Registry. Respir Med. 2019;155:97–103.
Heraganahally SS, Monsi E, Gadil E, Maze D, Lynch S. Catastrophic effects of using cannabis via bucket bong in Top End Northern Territory of Australia. Am J Trop Med Hyg. 2023;1–6. https://doi.org/10.4269/ajtmh.23-0393.
Pal A, Howarth TP, Rissel C, et al. COPD disease knowledge, self-awareness and reasons for hospital presentations among a predominately Indigenous Australian cohort – a study to explore preventable hospitalization. BMJ Open Resp Res. 2022;9: e001295. https://doi.org/10.1136/bmjresp-2022-001295.
Roberts JM, Goyal V, Kularatna S, et al. The economic burden of bronchiectasis: a systematic review. Chest. 2023. https://doi.org/10.1016/j.chest.2023.06.040.
Vigneault LP, Diendere E, Sohier-Poirier C, Hanna MA, Poirier A, St-Onge M. Acute health care among Indigenous patients in Canada: a scoping review. Int J Circumpolar Health. 2021;80:1. https://doi.org/10.1080/22423982.2021.1946324.
Huang H-Y, Chung F-T, Lin C-Y, et al. Influence of comorbidities and airway clearance on mortality and outcomes of patients with severe bronchiectasis exacerbations in Taiwan. Front Med. 2022;8: 812775. https://doi.org/10.3389/fmed.2021.812775.
Qi Q, Ailiyaer Y, Liu R, et al. Effect of N-acetylcysteine on exacerbations of bronchiectasis (BENE): a randomized controlled trial. Respir Res. 2019;20(1):73. https://doi.org/10.1186/s12931-019-1042-x.
Martínez-García MÁ, Oscullo G, García-Ortega A, Matera MG, Rogliani P, Cazzola M. Inhaled corticosteroids in adults with non-cystic fibrosis bronchiectasis: from bench to bedside. A Narrative Review Drugs. 2022;82(14):1453–68. https://doi.org/10.1007/s40265-022-01785-1.
Heraganahally S, Howarth TP, Issac S, et al. Exploring the appropriateness of prescribing practice of inhaled pharmacotherapy among Aboriginal Australians in the Top End Northern Territory of Australia: a retrospective cohort study. BMJ Open Resp Res. 2023;10: e001508. https://doi.org/10.1136/bmjresp-2022-001508.
Heraganahally SS, Ponneri TR, Howarth TP, Saad HB. The effects of inhaled airway directed pharmacotherapy on decline in lung function parameters among indigenous australian adults with and without underlying airway disease. Int J Chron Obstruct Pulmon Dis. 2021;16:2707–20.
Heraganahally SS, Ghataura AS, Er XY, Heraganahally S, Biancardi E. Excessive Dynamic Airway Collapse: A COPD/Asthma Mimic or a Treatment-emergent Consequence of Inhaled Corticosteroid Therapy: Case Series and Brief Literature Review. Clin Pulm Med. 2020;27:175–82.
Williams P, Gracey M, Smith P. Hospitalization of aboriginal and non-aboriginal patients for respiratory tract diseases in Western Australia, 1988–1993. Int J Epidemiol. 1997;26(4):797–805. https://doi.org/10.1093/ije/26.4.797.
Heerema J, Hug S, Bear N, Hill K. Characterising hospitalisation risk for chronic obstructive pulmonary disease exacerbations: Bedside and outpatient clinic assessments of easily measured variables. Chron Respir Dis. 2023;20:1–9.
Kolbe J, Wells AU. Bronchiectasis: A neglected cause of respiratory morbidity and mortality. Respirology. 1996;1(4):221–2.
Acknowledgements
We thank the Thoracic Society of Australia and New Zealand (TSANZ) research grant assessment committee members in recognising this research as a priority in addressing bronchiectasis disease burden among the adult Aboriginal Australians and supporting through the—Robert Pierce Grant-In-Aid for Indigenous Lung Health. We also thank Associate Professor Linda Ford—Indigenous Australian woman, a Mak Mak Marranunggu descendent from the Delissaville, Wagait Larrakia Aboriginal Land Trust and the Gurudju Aboriginal Land Trust in the Northern Territory for the support and facilitating Mrs Adriana Ticoalu from the Northern Institute, Faculty of Arts & Society, Charles Darwin University, Darwin, Northern Territory, Australia to assist with data collection for this study. We also extend our sincere apparition to Dr Shiidheshwar Ravichandran and Dr Davaadorj Erdenebayar for their help during this study.
Funding
This work was supported by the Thoracic Society of Australia and New Zealand (TSANZ) Robert Pierce Grant-In-Aid for Indigenous Lung Health. The TSANZ did not have any role in the study design, data collection, analysis, or interpretation.
Author information
Authors and Affiliations
Contributions
TH—conceptualisation, data curation, formal analysis, investigation, methodology, resources, software, validation, visualisation, writing & original draft, and writing & review & editing. CG & conceptualisation, data curation, formal analysis, methodology, resources, software, validation, visualisation, writing & original draft, and writing & review & editing.AA—conceptualisation, data curation, resources, software, validation, visualisation, writing & original draft, and writing & review & editing.SH—conceptualisation, data curation, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, visualisation, writing & original draft, and writing & review & editing and is the overall guarantor and accountable for the research work.
Authors’ information
Not applicable.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Human Research Ethics governance/committee of the Top End Health Service (TEHS), Northern Territory (NT) and Menzies School of Health Research (Reference: HREC; 2019–3547). Individual patient consent was not required, as it was a retrospective study and no active interventions were undertaken and the need for individual consent was waived by the Human Research Ethics governance/committee of the TEHS, NT and Menzies School of Health Research.
Consent for publication
Not applicable.
Competing interests
Nil.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Howarth, T., Gibbs, C., Heraganahally, S.S. et al. Hospital admission rates and related outcomes among adult Aboriginal australians with bronchiectasis – a ten-year retrospective cohort study. BMC Pulm Med 24, 118 (2024). https://doi.org/10.1186/s12890-024-02909-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-02909-x