Abstract
Background
While it is known that the overconsumption of ultra-processed foods (UPFs) is associated with a heightened risk of respiratory ailments, the specific effects of UPF intake on COPD remain unclear. This study was designed to explore the potential link between COPD and the consumption of UPFs among adult individuals in Iran.
Methods
In this hospital-based case-control study conducted at Alzahra University Hospital in Isfahan, Iran, we enrolled 84 patients newly diagnosed with COPD, along with 252 healthy controls matched for age and sex. COPD was defined based on the results of spirometry tests, specifically when the forced expiratory volume per second (FEV1) was less than 80% or the ratio of FEV1 to forced vital capacity (FVC) was less than 70%. To evaluate the dietary intake of the participants, we utilized a validated food frequency questionnaire (FFQ) consisting of 168 items. Additionally, we gathered data on potential confounding factors using a pre-tested questionnaire.
Results
The mean ages for the case and control groups were 57.07 and 55.05 years, respectively. Our study found no significant association between the intake of ultra-processed foods (UPFs) and the likelihood of COPD, with an odds ratio (OR: 0.78, 95% CI: 0.34–1.77). This lack of association persisted even after adjusting for factors such as energy intake, sex, and age (OR: 0.48; 95% CI: 0.19–1.21). Further controlling for potential confounders like body mass index (BMI), physical activity, and smoking status did not alter this finding (OR: 0.367; 95% CI: 0.123–1.1008, P = 0.074).
Conclusions
In our study, we observed no significant association between the intake of Ultra-Processed Foods (UPFs) and the odds of Chronic Obstructive Pulmonary Disease (COPD). This finding remained consistent even after adjusting for factors such as energy intake, sex, age, Body Mass Index (BMI), physical activity, and smoking status. Therefore, within the scope of our study, it appears that the consumption of UPFs does not significantly impact the likelihood of developing COPD. However, we recommend further research to deepen our understanding of the intricate relationship between dietary habits and respiratory health.
Similar content being viewed by others
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a significant global health concern. According to the Global Burden of Disease Study 2019, COPD accounted for a substantial number of deaths and disability-adjusted life years (DALYs) worldwide [1]. The study reported that in 2019, there were 212.3 million prevalent cases of COPD globally, with COPD accounting for 3.3 million deaths and 74.4 million DALYs [1]. Another study found that the total number of COPD cases increased by 39.5% from 1990 to 2017 [2].
The importance of diet in managing and preventing COPD has been increasingly recognized. A balanced diet rich in antioxidants and anti-inflammatory foods may help prevent and manage COPD [3, 4]. In particular, the consumption of ultra-processed foods has been linked to a higher risk of COPD [5]. These foods often contain high levels of added sugar, fat, and/or salt, but lack vitamins and fiber [6]. A study found that elevated consumption of ultra-processed food was associated with a higher risk of COPD, and this association was primarily mediated by glucose, inflammation, and lipids [5]. Conversely, substituting unprocessed or minimally processed food for ultra-processed food was associated with a decreased risk of COPD [5]. Therefore, maintaining a healthy diet and avoiding ultra-processed foods could play a crucial role in managing and preventing COPD. However, more research is needed to further understand these relationships and to develop dietary guidelines for individuals with COPD.
COPD is a leading cause of death, illness, and healthcare load worldwide [7], and is characterized by chronic bronchitis, small airway blockage, and emphysema, leading to chronic inflammation of the airways and pulmonary parenchyma with irreversible and progressive airflow restriction [7]. With 210 million COPD patients worldwide and projections to become the third leading cause of mortality by 2030 [8], understanding the factors contributing to COPD is of paramount importance.
While smoking is the most significant cause of COPD [9], but factors such as workplace pollution, environmental pollution and genetics are also important contributors in the pathogenesis of COPD [10]. Recent studies have underscored the significance of dietary habits in both the onset and progression of chronic diseases [11]. Recent studies have underscored the significance of dietary habits in both the onset and progression of chronic diseases, including COPD [12,13,14].
Over the past decades, diets in many countries have shifted towards a significant increase in the consumption of ultra-processed foods (UPFs) [15,16,17,18],which are high in additives, salt, free sugars, fats, preservatives, synthetic antioxidants [19]. but often lack important micronutrients, fiber, protein, and phytochemicals [20]. The potential negative effects of these ingredients on our health warrant further research. Existing research has explored the relationship between processed meat consumption and the incidence of Chronic Obstructive Pulmonary Disease (COPD) where a systematic review and meta-analysis of prospective cohort studies and found a positive association between processed red meat intake and the risk of COPD [21]. A study found that regular meat consumption, including processed meat, is associated with a range of diseases, including heart disease, pneumonia, and diabetes but did not find a significant association between processed meat consumption and the risk of COPD [22]. Also a systematic review and meta-analysis of prospective cohort studies found that higher consumption of red meat and processed meat was associated with an increased risk of colorectal cancer [23]. While this study did not specifically investigate the relationship between processed meat consumption and COPD, it contributes to the broader understanding of the potential health impacts of processed meat consumption. This represents a significant gap in the current body of research and underscores the importance of our study in contributing to this area of knowledge.
While the effects of UPFs on several chronic diseases such as obesity, metabolic syndrome, diabetes, hypertension, dyslipidemia, heart disease, and cancer have been previously studied [24,25,26,27,28,29,30,31], their impact on COPD remains under-investigated. UPFs typically have poor nutritional profiles, are hyper-palatable, and contain biologically harmful compounds, all of which can negatively impact health [32]. In the context of Chronic Obstructive Pulmonary Disease (COPD), it is plausible that the consumption of UPFs could contribute to the development and progression of the disease. For instance, the high levels of free sugars, saturated fats, and sodium found in UPFs could lead to systemic inflammation, a key factor in the pathogenesis of COPD [32, 33]. Furthermore, the additives and preservatives commonly used in UPFs could potentially have a direct detrimental effect on lung function [33]. However, the exact mechanisms linking UPF consumption and COPD are not yet fully understood, and more research is needed in this area. It’s also important to note that while UPF consumption could potentially contribute to COPD, it is likely just one of many factors involved, alongside others such as smoking, air pollution, and genetic predisposition [32].
Therefore, this study aims to investigate the relationship between UPF consumption and the incidence of COPD, contributing to the limited body of research in this area. Our findings provide valuable insights into the potential role of diet, specifically UPF consumption, in the development and progression of COPD.
Materials and methods
Participants
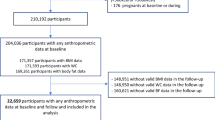
The current case-control study was conducted on 84 COPD patients who were recently diagnosed, and 252 controls in the period between 2015 and 2016 at Al-Zahra Hospital, University of Isfahan, Iran. Cases were patients with forced expiratory volume (FEV1) < 80 or FEV1/ forced vital capacity (FVC) < 70%. The participants were all above the age of 30 and had received their COPD diagnosis from a pulmonologist. The diagnostic criteria were based on spirometry test results, a common method for assessing lung function [34]. A patient was identified as having COPD if their ratio of forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC) was below 70%, or if their FEV1 was less than 80% of the predicted value. The control group was made up of 252 healthy individuals from the same hospital, none of whom had a history of COPD. Both cases and controls were paired based on age (within a 5-year range) and gender. The control subjects were those who visited the same hospital’s outpatient clinics and were enlisted concurrently with the cases. The criteria for including a subject in the case group was a COPD diagnosis confirmed by a physician and a spirometry test. We excluded participants from the study if they had a dementia, stroke, or any condition that would prevent them from participating in an interview. In addition, other chronic diseases such as severe heart failure, chronic liver cirrhosis, inflammatory bowel disease, renal failure, uncontrolled thyroid disease, rheumatoid arthritis, cancer in the last 3 years, a systematic course of long-term treatment with steroid drugs, chronic infections (HIV, tuberculosis, etc.), cachexia, and other lung problems like fibrosis were considered as non-inclusion criteria.
Dietary intakes assessment
A validated 168-item FFQ was used to assess participants’ usual dietary intake during the last year. The reliability and validity of the FFQ have been confirmed in previous studies [35]. This FFQ included of 168 food items which each food item has a standard serving size [36]. A trained interviewer conducted face-to-face interviews to complete the FFQ. Household measures were used to convert reported consumptions to grams per day [37]. Daily energy and nutrient intakes for each person were then calculated using the food composition database of the US Department of Agriculture, which was modified for Iranian foods [38].
According to NOVA classification system which was suggested by Monteiro et al. [39], ultra-processed foods were selected. The NOVA classification system classifies foods into 4 different categories: the first category includes unprocessed and slightly processed foods, including foods that are fresh or processed without any additives such as salt, sugar, fats or oils. The second category includes processed cooking ingredients such as fats, sugar, or salt, consumed in mixture with unprocessed and minimally processed foods in meal preparation. The third group includes processed foods such as canned fruits or vegetables, salted nuts, cured, or smoked meats, and cheese which are produced by adding processed culinary ingredients to unprocessed or least processed foods. The fourth category includes ultra-processed foods, such as ice cream, biscuits, cakes, chocolates, chips, pastries, jams, confectionery, sugar added breakfast cereals, crisps, high caloric snack products, sauces, fruit and milk beverages with added sugar, cereal bars, sweetened and non-caloric soft drinks, and pasta, poultry, fish meat and vegetable dishes, hot dogs, burgers, chicken nuggets fish sticks, sausages pre-prepared pizza, processed soups and noodles, infant formulas and baby food products. These products have undergone the highest level of processing. In the current study, only foods in the fourth group (ultra-processed foods) were analyzed.
In our methodology, we utilized the NOVA classification system to categorize food items, focusing specifically on ultra-processed foods. Each food item was classified as either an ultra-processed food or not, providing us with nominal data. To further refine our analysis, we divided the consumption of ultra-processed foods into quintiles, thereby presenting our data on an ordinal scale. This approach allowed us to examine the relationship between varying levels of ultra-processed food consumption and the risk of COPD in a more nuanced manner.
Ultra processed food score construction
In our study, we evaluated the overall dietary quality by examining both food groups and nutrients across quintiles of the ultra-processed food score. This involved dividing the participants into five distinct groups based on their ultra-processed food consumption. Each group represented a fifth, or 20%, of the data. To create the ultra-processed food score, we used food frequency questionnaires to collect data on the participants’ dietary habits. Each food item was then classified according to the NOVA classification, and the proportion of ultra-processed foods in the diet was calculated. This gave us the ultra-processed food score for each participant. Next, we divided these scores into quintiles. This was done by sorting the scores from lowest to highest and then dividing them into five equal groups. Each quintile thus represents a range of ultra-processed food scores, allowing us to compare the dietary quality across different levels of ultra-processed food consumption.
Pulmonary function assessment
A trained technician used spirometry test to evaluate pulmonary function and computed FVC, FEV1, and FEV1 / FVC. The reliability and validity of the spirometry have been confirmed in previous studies [34]. Evaluation of other respiratory signs, such as persistent cough, sputum production and pain intensity were also assessed. In the current study, persistent cough was defined as cough for more than three weeks [40], while sputum production was defined as the production of sputum for more than three months in two successive years [41, 42]. The visual analog scale was used to assess pain intensity. The Visual Analog Scale is a 100 mm horizontal line used by patients to quantify their pain intensity. One end represents the absence of pain, while the opposite end signifies the most severe pain experienced [43].
Other variables assessment
Through a comprehensive questionnaire, we gathered data on participants’ age, gender, education level, marital status, smoking habits (categorized as never smoker, current smoker, or former smoker), medication and supplement usage, and family history of lung disorders. Participants’ height was measured in a standard upright position without shoes, while body weight was recorded to the nearest 100 g using a digital scale, with participants wearing minimal clothing. These measurements were then used to calculate the Body Mass Index (BMI) by dividing weight (in kilograms) by the square of height (in meters). To assess participants’ daily physical activity, we utilized the long form of the International Physical Activity Questionnaire (IPAQ) [43]. This assessment considered the number of days per week and the duration (in minutes) of physical activity per day. MET minutes of these activities was quantified using the Metabolic Equivalent for Task (MET) and expressed as MET-minutes per week.
Statistical methods
In the current study, classification of participants across quintiles of ultra-processed food intakes was done. The study participants’ general characteristics and dietary intakes were analyzed and compared across different levels of UPF score using t-test and ANOVA test for continuous variables and chi-square tests for categorical variables. Logistic regression was used to investigate the association between UPF and COPD in several models. Model 1 was adjusted for energy intake (kcal/d), gender, and age. Model II was further adjusted for BMI, physical activity, and smoking status. All confounders were selected based on previous publications [44, 45]. To evaluate the normality of our data, we employed the Shapiro-Wilk test and conducted a visual examination of histograms and Q-Q plots. This comprehensive approach allowed us to accurately assess the distribution of our data. The statistical analyses were carried out using SPSS version 21. P-values were considered significant at P < 0.05.
Results
General characteristics of study participants were reported in Table 1. Cases were more likely to be smokers, married, employed, and having a low level of physical activity, lung disease family history, and air pollution exposure compared to controls. As expected, cases were more likely to have lower FVC, FEV1, and FEV1 / FVC ratios compared to controls.
Dietary intakes of study participants were reported in Table 2. Cases consumed less red and processed meats, whole grains, and sugar-sweetened beverages compared to controls. Furthermore, compared to controls, cases had higher energy, carbohydrates, magnesium, sodium, vitamin K, cholesterol, and dietary fiber.
Comparing UPF consumption quintiles, participants in the highest quintile of UPF consumption, were more likely to be young, less employed, smokers, and exposed to air pollution compared to those in the lowest quintile as presented in Table 3. In terms of dietary intakes, people in the highest quintile of UPF have higher energy intake and consumed more vegetables, legumes and nuts, carbohydrates, protein, fat, cholesterol, sodium, magnesium, potassium, folate, vitamin C, vitamin K and dietary fiber, while they have lower consumption of red and processed meat compared to people with the first quintile as shown in Table 4.
Table 5 presents the multivariable-adjusted odds ratios for COPD across quintiles UPFs intake score. The odds ratios were calculated using logistic regression models and are presented for three different models. In the crude model,, consumption of UPFs was not significantly associated with the risk of COPD (OR: 0.78; 95% CI: 0.34–1.77, P = 0.557).After adjustment for potential cofounders in model 1 (energy intake gender and age,, and) and in model 2 (further adjusted for BMI, physical activity, hookah use and smoking status), the relationship also remained not significant (OR: 0.48; 95% CI: 0.19–1.21, P = 0.117 and OR: 0.36; 95% CI: 0.12–1.10, P = 0.074 respectively).
Discussion
In this case-control study, we did not find any association between the consumption of UPFs and COPD. To the best of our knowledge, this is the first study to investigate this relationship.
COPD is a significant global public health concern [46]. While cessation of smoking remains the most critical public health advice for preventing COPD, research indicates that diet could also be a modifiable risk factor for impaired lung function [47]. Unfortunately, no previous studies have examined the association between processed foods and COPD. Ultra-Processed Foods (UPFs), a notable component of the Western diet [15], which is characterized by high consumption of refined grains, desserts, processed and red meats, and French fries, is generally deemed unhealthy [48]. Conversely, diets rich in fruits, vegetables, legumes, whole grains, nuts, dairy, total protein foods, seafood, and plant proteins are believed to play a protective role in the development of COPD [49], This is attributed to their high content of antioxidants (particularly vitamin C), long-chain omega-3 fats, polyunsaturated fatty acids, and dietary fiber, as well as their anti-inflammatory properties [47].
Numerous studies have explored the relationship between the Western diet, its components, and COPD. These studies consistently indicate an inverse relationship between the consumption of Western dietary components (or unhealthy diets) and COPD. For instance, a study by Varraso et al. demonstrated that over a 12-year follow-up period, the risk of newly diagnosed COPD increased with greater adherence to a Western dietary pattern It’s worth noting that this study had certain limitations, such as being conducted exclusively on American men and relying on physician diagnoses for newly diagnosed COPD without lung function test results. However, in our current study, we improved the validity and accuracy of the results by measuring lung function using a spirometry test. A study conducted in Korea by Min et al. reported increased airflow restrictions with higher consumption of soda drinks and coffee [50]. Similarly, Shi et al. found a positive association between the intake of soft drinks and COPD among adults living in South Australia [51]. However, this study’s reliance on telephone interviews for data collection and a fair response rate of 64% could potentially introduce biases. Interestingly, our study observed no significant change in the consumption of sugar-sweetened beverages within the quintiles of ultra-processed foods. This could explain the lack of significance observed in our findings compared to previous research. In other words, our study focused on the overall consumption of Ultra-Processed Foods (UPFs) rather than specific subtypes.
Numerous studies have investigated the correlation between a healthy diet and COPD, with the majority finding an inverse relationship. Steinemann et al.‘s study highlighted the protective effects of a diet rich in vegetables, fruits, nuts, and fish against age-related chronic respiratory diseases [47]. A cohort study revealed an inverse association between a prudent dietary pattern score (characterized by high intake of vegetables, fruits, whole grains, and fish) and the risk of newly diagnosed COPD A cross-sectional study also demonstrated that consumption of whole grains and fruits could positively influence FEV1 and reduce COPD prevalence [52]. However, some studies have found no connection between a healthy diet and COPD. For instance, Butler et al.‘s study found a weak association between a diet high in fruits, vegetables, and soy and the presence of cough and phlegm, but this association disappeared after adjusting for non-starch polysaccharides intake [53]. Regarding fish consumption, a major source of omega-3 polyunsaturated fatty acids in a “prudent” diet, the results from various studies have been inconsistent [54]. There was only one prospective study published on this topic, which found no association between omega-3 intake and the incidence of chronic non-specific lung disease [55].. This highlights the complexity of dietary influences on COPD and the need for further research.
In the study conducted by Fischer et al., it was found that adherence to a Mediterranean-like diet was inversely associated with the development of COPD. However, when analyzing individual components within the modified Mediterranean Diet Score (MDS), only fruit consumption was significantly linked to a reduced risk of developing COPD. This underscores the complexity of assessing dietary habits and emphasizes the importance of examining the impact of diet as a whole, rather than focusing solely on individual nutrients [56]. There seems to be no clear association between a specific food and COPD, suggesting that a more holistic approach to studying diet may provide a more comprehensive understanding of disease prevention [48]. The lack of a connection found in our study could be due to the specific foods we chose to focus on. Although our study found no association between Ultra-Processed Foods (UPFs) and COPD, studies that have observed an association suggest several mechanisms. For instance, processed meats, a component of UPFs, contain high amounts of nitrite. Nitrites produce reactive nitrogen species, which can cause nitrosative stress and potentially contribute to progressive deterioration in lung function [57]. UPFs also include refined grains, desserts, sodas, and sweets that have a high glycemic index, which can increase blood sugar levels. Hyperglycemia is associated with impaired pulmonary function [58], a primary measurement for COPD diagnosis [42]. Furthermore, both COPD and hyperglycemia are positively associated with inflammation [59, 60]. Experimental evidence suggests that foods that increase inflammation and oxidative stress can affect the pathogenesis of COPD, as COPD is associated with inflammation [61]. Sugar consumption can activate the innate immune system in the lungs and increase sensitivity to allergic airway inflammation [62]. It is also known that consumption of soft drinks can increase the risk of obesity [63], which is a risk factor for COPD [64, 65].
While several studies have suggested a potential link between UPF consumption and various health outcomes, including obesity and other diet-related noncommunicable diseases [32], the relationship with COPD is less clear. Some studies have suggested that the high levels of free sugars, saturated fats, and sodium found in UPFs could lead to systemic inflammation, a key factor in the pathogenesis of COPD [32]. However, our study did not find a significant association between UPF consumption and COPD. There could be several reasons for this. First, the effect of diet on COPD may be influenced by a range of other factors, including genetic predisposition, smoking status, and exposure to air pollution1. Second, the specific dietary patterns and food choices of our study population may differ from those in other studies, potentially influencing the observed associations. Finally, it’s also possible that the tools and methods we used to assess UPF consumption and COPD status may not have been sensitive enough to detect a potential association.
The current study is the first to examine the association of UPFs consumption with COPD risk in adults. some of the study strengths is that we adjusted the analysis to a wide range of confounding non-dietary covariates, such as age, sex, smoking, BMI, and physical activity. In addition, we matched two groups of COPD patient and healthy individuals based on age and sex. However, several limitations should be noted. Due to the cross-sectional nature of the study, we could not deduce the causal relationship. UPFs consumption was assessed using FFQ, which has potential recall bias. Also, the low number of included COPD patients, might influence on the results. Additionally, it is important to consider other factors that can highly impact COPD such as smoking or air pollution.
Conclusion
In conclusion, our case-control study did not find any association between the consumption of ultra-processed foods (UPFs) and the risk of Chronic Obstructive Pulmonary Disease (COPD). Further studies, particularly with a prospective design, are needed to confirm these results and provide a more comprehensive understanding of the relationship between UPFs and COPD.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- UPFs:
-
Ultra processed foods
- FEV1:
-
Forced expiratory volume
- FVC:
-
Forced vital capacity
- FFQ:
-
Food frequency questionnaire
- BMI:
-
Body mass index
- HIV:
-
Human immunodeficiency virus
- IPAQ:
-
International physical activity questionnaire
- MET:
-
Metabolic equivalent
- ANOVA:
-
Analysis of variance
- MDS:
-
Mediterranean diet score
References
Safiri S, Carson-Chahhoud K, Noori M, Nejadghaderi SA, Sullman MJ, Heris JA et al. Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990–2019: results from the global burden of Disease Study 2019. BMJ. 2022;378.
Xie M, Liu X, Cao X, Guo M, Li X. Trends in prevalence and incidence of chronic respiratory diseases from 1990 to 2017. Respir Res. 2020;21(1):1–13.
Association AL, Nutrition. and COPD. 2023 May 23.
Foundation C. Nutrition for someone with COPD. 2021 January 14.
He Q, Sun M, Zhao H, Sun N, Han Q, Feng Z, et al. Ultra-processed food consumption, mediating biomarkers, and risk of chronic obstructive pulmonary disease: a prospective cohort study in the UK Biobank. Food Funct. 2023;14(19):8785–96.
McManus K. What are ultra-processed foods and are they bad for our health. Harvard Health Publishing, Harvard Health Blog. https://www.health.harvard… 2020.
Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E et al. Global and regional estimates of COPD prevalence: systematic review and meta–analysis. J Global Health. 2015;5(2).
Organization WH. Chronic obstructive pulmonary disease (COPD. 2023 March 16.
Wang J, Spitz MR, Amos CI, Wilkinson AV, Wu X, Shete S. Mediating effects of smoking and chronic obstructive pulmonary disease on the relation between the CHRNA5-A3 genetic locus and lung cancer risk. Cancer. 2010;116(14):3458–62.
Andersen ZJ, Hvidberg M, Jensen SS, Ketzel M, Loft S, Sørensen M, et al. Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: a cohort study. Am J Respir Crit Care Med. 2011;183(4):455–61.
Schulze MB, Martínez-González MA, Fung TT, Lichtenstein AH, Forouhi NG. Food based dietary patterns and chronic disease prevention. BMJ. 2018;361.
Berthon BS, Wood LG. Nutrition and respiratory health—feature review. Nutrients. 2015;7(3):1618–43.
Zheng P-F, Shu L, Si C-J, Zhang X-Y, Yu X-L, Gao W. Dietary patterns and chronic obstructive pulmonary disease: a meta-analysis. COPD: J Chronic Obstr Pulmonary Disease. 2016;13(4):515–22.
Vasankari T, Härkänen T, Kainu A, Sääksjärvi K, Mattila T, Jousilahti P, Laitinen T. Predictors of new airway obstruction–an 11 year’s population-based follow-up study. COPD: J Chronic Obstr Pulmonary Disease. 2019;16(1):45–50.
Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14:21–8.
Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–9.
Bortoletto MP, Bertazzi L. Processed and ultra-processed Food products: Consumption trends in Canada from 1938 to 2011. Can J Diet Pract Res. 2014.
Venn D, Banwell C, Dixon J. Australia’s evolving food practices: a risky mix of continuity and change. Public Health Nutr. 2017;20(14):2549–58.
Monteiro CA, Moubarac J-C, Levy RB, Canella DS, da Costa Louzada ML, Cannon G. Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutr. 2018;21(1):18–26.
Askari M, Heshmati J, Shahinfar H, Tripathi N, Daneshzad E. Ultra-processed food and the risk of overweight and obesity: a systematic review and meta-analysis of observational studies. Int J Obes. 2020;44(10):2080–91.
Salari-Moghaddam A, Milajerdi A, Larijani B, Esmaillzadeh A. Processed red meat intake and risk of COPD: a systematic review and dose-response meta-analysis of prospective cohort studies. Clin Nutr. 2019;38(3):1109–16.
Oxford Uo. Regular meat consumption linked with a wide range of common diseases. 2021 March 2.
Di Y, Ding L, Gao L, Huang H. Association of meat consumption with the risk of gastrointestinal cancers: a systematic review and meta-analysis. BMC Cancer. 2023;23(1):782.
Mendonça RD, Lopes ACS, Pimenta AM, Gea A, Martinez-Gonzalez MA, Bes-Rastrollo M. Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: the Seguimiento Universidad De Navarra Project. Am J Hypertens. 2017;30(4):358–66.
Fiolet T, Srour B, Sellem L, Kesse-Guyot E, Allès B, Méjean C et al. Consumption of ultra-processed foods and cancer risk: results from NutriNet-Santé prospective cohort. BMJ. 2018;360.
Lavigne-Robichaud M, Moubarac J-C, Lantagne-Lopez S, Johnson-Down L, Batal M, Sidi EAL, Lucas M. Diet quality indices in relation to metabolic syndrome in an indigenous Cree (Eeyouch) population in northern Québec. Can Public Health Nutr. 2018;21(1):172–80.
Tavares LF, Fonseca SC, Rosa MLG, Yokoo EM. Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian family Doctor Program. Public Health Nutr. 2012;15(1):82–7.
Nasreddine L, Tamim H, Itani L, Nasrallah MP, Isma’eel H, Nakhoul NF, et al. A minimally processed dietary pattern is associated with lower odds of metabolic syndrome among Lebanese adults. Public Health Nutr. 2018;21(1):160–71.
Rauber F, Campagnolo PD, Hoffman DJ, Vitolo MR. Consumption of ultra-processed food products and its effects on children’s lipid profiles: a longitudinal study. Nutr Metabolism Cardiovasc Dis. 2015;25(1):116–22.
Steele EM, Juul F, Neri D, Rauber F, Monteiro CA. Dietary share of ultra-processed foods and metabolic syndrome in the US adult population. Prev Med. 2019;125:40–8.
Canella DS, Levy RB, Martins APB, Claro RM, Moubarac J-C, Baraldi LG, et al. Ultra-processed food products and obesity in Brazilian households (2008–2009). PLoS ONE. 2014;9(3):e92752.
Chen X, Zhang Z, Yang H, Qiu P, Wang H, Wang F, et al. Consumption of ultra-processed foods and health outcomes: a systematic review of epidemiological studies. Nutr J. 2020;19(1):1–10.
Program GFR. Ultra-processed foods: A global threat to public health. 2021 May.
Fernández-Villar A, Represas-Represas C, Mouronte-Roibás C, Ramos-Hernández C, Priegue-Carrera A, Fernández-García S, López-Campos JL. Reliability and usefulness of spirometry performed during admission for COPD exacerbation. PLoS ONE. 2018;13(3):e0194983.
Esfahani FH, Asghari G, Mirmiran P, Azizi F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran lipid and glucose study. J Epidemiol. 2010;20(2):150–8.
Mirmiran P, Esfahani FH, Mehrabi Y, Hedayati M, Azizi F. Reliability and relative validity of an FFQ for nutrients in the Tehran lipid and glucose study. Public Health Nutr. 2010;13(5):654–62.
Ghaffarpour M, Houshiar-Rad A, Kianfar H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran: Nashre Olume Keshavarzy. 1999;7(213):42–58.
Haytowitz D, Lemar L, Pehrsson P, Exler J, Patterson K, Thomas R, et al. USDA national nutrient database for standard reference, release 24. Washington, DC, USA: US Department of Agriculture; 2011.
Monteiro CA, Cannon G, Moubarac J-C, Levy RB, Louzada MLC, Jaime PC. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21(1):5–17.
Mason RJ, Broaddus VC, Martin TR, King TE, Schraufnagel D, Murray JF, Nadel JA. Murray and Nadel’s textbook of respiratory medicine E-book: 2-volume set. Elsevier Health Sciences; 2010.
Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) workshop summary. Am J Respir Crit Care Med. 2001;163(5):1256–76.
Br C. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004;23:932–46.
Mahler DA, Weinberg DH, Wells CK, Feinstein AR. The measurement of dyspnea: contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest. 1984;85(6):751–8.
Guo FR, Lundborg AR, Zhao Q. Confounder Selection: Objectives and Approaches. arXiv preprint arXiv:220813871. 2022.
VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34:211–9.
Gómez FP, Rodriguez-Roisin R. Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines for chronic obstructive pulmonary disease. Curr Opin Pulm Med. 2002;8(2):81–6.
Steinemann N, Grize L, Pons M, Rothe T, Stolz D, Turk A, et al. Associations between dietary patterns and post-bronchodilation lung function in the SAPALDIA Cohort. Respiration. 2018;95(6):454–63.
Varraso R, Teresa TF, Frank BH, Willett W, Camargo CA. Prospective study of dietary patterns and chronic obstructive pulmonary disease among US men. Thorax. 2007.
Reedy J, Lerman JL, Krebs-Smith SM, Kirkpatrick SI, Pannucci TE, Wilson MM, et al. Evaluation of the healthy eating index-2015. J Acad Nutr Dietetics. 2018;118(9):1622–33.
Min JE, Huh D-A, Moon KW. The joint effects of some beverages intake and smoking on chronic obstructive pulmonary disease in Korean adults: data analysis of the Korea National Health and Nutrition Examination Survey (KNHANES), 2008–2015. Int J Environ Res Public Health. 2020;17(7):2611.
Shi Z, Dal Grande E, Taylor AW, Gill TK, Adams R, Wittert GA. Association between soft drink consumption and asthma and chronic obstructive pulmonary disease among adults in Australia. Respirology. 2012;17(2):363–9.
Tabak C, Smit H, Heederik D, Ocke M, Kromhout D. Diet and chronic obstructive pulmonary disease: independent beneficial effects of fruits, whole grains, and alcohol (the MORGEN study). Clin Experimental Allergy. 2001;31(5):747–55.
Butler LM, Koh W-P, Lee H-P, Tseng M, Yu MC, London SJ. Prospective study of dietary patterns and persistent cough with phlegm among Chinese singaporeans. Am J Respir Crit Care Med. 2006;173(3):264–70.
Romieu I. Nutrition and lung health [State of the art]. Int J Tuberc Lung Dis. 2005;9(4):362–74.
Miedema I, Feskens EJ, Heederik D, Kromhout D. Dietary determinants of long-term incidence of chronic nonspecific lung diseases: the Zutphen Study. Am J Epidemiol. 1993;138(1):37–45.
Fischer A, Johansson I, Blomberg A, Sundström B. Adherence to a Mediterranean-Like diet as a protective factor against COPD: a nested case-control study. COPD: J Chronic Obstr Pulmonary Disease. 2019;16(3–4):272–7.
Ricciardolo FL, Di Stefano A, Sabatini F, Folkerts G. Reactive nitrogen species in the respiratory tract. Eur J Pharmacol. 2006;533(1–3):240–52.
Walter RE, Beiser A, Givelber RJ, O’Connor GT, Gottlieb DJ. Association between glycemic state and lung function: the Framingham Heart Study. Am J Respir Crit Care Med. 2003;167(6):911–6.
Donaldson G, Seemungal T, Patel I, Bhowmik A, Wilkinson T, Hurst J et al. Airway and systemic inflammation and decline in lung function in patients with COPD: Chest. 2005; 128: 1995–2004. Respiratory Medicine: COPD Update. 2006;1(3):101-2.
Esposito K, Nappo F, Marfella R, Giugliano G, Giugliano F, Ciotola M, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106(16):2067–72.
Majumder K, Mine Y, Wu J. The potential of food protein-derived anti‐inflammatory peptides against various chronic inflammatory diseases. J Sci Food Agric. 2016;96(7):2303–11.
Kierstein S, Krytska K, Kierstein G, Hortobágyi L, Zhu X, Haczku A. Sugar consumption increases susceptibility to allergic airway inflammation and activates the innate immune system in the lung. J Allergy Clin Immunol. 2008;121(2):196.
Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes. 2008;32(6):881–91.
Franssen F, O’Donnell D, Goossens G, Blaak E, Schols A. Obesity and the lung: 5· obesity and COPD. Thorax. 2008;63(12):1110–7.
Sin D, Sutherland E. Obesity and the lung: 4· obesity and asthma. Thorax. 2008;63(11):1018.
Acknowledgements
We thank all those involved and participants for taking part in the present study.
Funding
This work was supported by the Isfahan University of Medical Sciences.
Author information
Authors and Affiliations
Contributions
The manuscript was drafted by ZS. HM contributed to the data analysis. BG contributed to rewriting several sections of the paper, as well as editing and revising the paper and tables. SO, MEA, AF, and AE made substantial contributions to data collection and interpretation. LA contributed in supervision, conception, design, methodology, statistical analyses, data interpretation and manuscript revising. All authors have reviewed and given their approval for the final manuscript to be submitted.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
All participants have given their informed consent to participate in the study. This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures involving human subjects/patients were approved by the Medical Ethics Committee of the Isfahan University of Medical Sciences, Isfahan, Iran (code 393881).
Consent for publication
NA.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Salehi, Z., Malmir, H., Ghosn, B. et al. Exploring the association between ultra-processed foods and COPD: a case-control study. BMC Pulm Med 24, 124 (2024). https://doi.org/10.1186/s12890-024-02903-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-024-02903-3