Abstract
Background
The clinical heterogeneity of chronic rhinosinusitis (CRS) and bronchial asthma is attributable to different underlying inflammatory profiles. However, the similarity between CRS with nasal polyps (CRSwNP) and type-2 asthma pathophysiology speculates that one biological therapy could affect both comorbidities. Despite dupilumab, a monoclonal antibody that targets IL-4α and IL-13 receptors, being used in patients with nasal polyps and severe asthma, real-life data about its efficacy in improving the quality of life and patient symptoms is still lacking. This study’s primary objective was to evaluate dupilumab treatment’s effect on the frequency of olfactory symptoms and health-related quality of life tests as measured by the Sino-nasal outcome test (SNOT-22) in patients with NP. The secondary objective was the effect of dupilumab on asthma symptom control as measured by the asthma control test (ACT).
Methods
A prospective study was conducted of 166 patients with CRSwNP, with or without asthma. The following variables were collected at baseline and after at least six months of continuous dupilumab therapy; SNOT-22, olfactory symptoms frequency, and ACT score.
Results
Asthma prevalence in patients with CRSwNP was high (59.63%), and being female with a history of frequent use of oral corticosteroid (OCS) courses and repeated unsuccessful nasal and para-nasal surgeries for polyposis increased the likelihood of having underlying asthma by 2, 1 and 4 times more, respectively. Additionally, being asthmatic required a longer duration of dupilumab treatment. However, both the health-related quality of life and olfactory symptoms improved equally in both groups.
Conclusion
Even with associated comorbid asthma in patients with CRSwNP, treatment with dupilumab could improve the quality of life, olfactory symptoms, and asthma symptom control.
Similar content being viewed by others
Introduction
Affecting 5–28% of the general population, chronic rhinosinusitis (CRS) is a prevalent condition worldwide that places a heavy financial burden due to increased healthcare costs and loss of productivity [1,2,3,4,5]. CRS is a group of disorders that cause inflammation of the sinonasal mucosa and have a multifactorial etiology involving immunological and epithelial barrier components influenced by the microbiota, environment, and genetic factors [6]. Along with objective evidence, at least two out of the following four cardinal symptoms are necessary to diagnose CRS: facial pain/pressure, hyposmia/anosmia, nasal discharge, and nasal obstruction for at least 12 weeks in a row. Physical examination (anterior rhinoscopy, endoscopy) or radiography, ideally from sinus computed tomography, can provide objective evidence of CRS [7].
Two significant phenotypes are defined for CRS based on nasal endoscopic findings: CRS without nasal polyps (CRSsNP) and CRS with nasal polyps (CRSwNP). CRSwNP, which comprises about 18–20% of all CRS cases, is linked to significant morbidity and may impact adults’ lower airway disease status [8, 9]. Moreover, CRSwNP and asthma are closely linked, as implied by epidemiological, clinical, and pathophysiological studies [10, 11]. Correlation between the inflammatory profiles of nasal and bronchial biopsies in patients with CRSwNP is significant (P < 0.01),[12] which is reflected in the direct relationship between the inflammation in the nasal mucosa and lower airways and adding support to the united airways concept already described in patients with asthma and comorbid allergic rhinitis [6, 13,14,15]. From a pathophysiological view, both disorders, CRSwNP, and asthma share the same type 2 immunopathology (involvement of IgE, eosinophils, interleukin-4 (IL-4)/IL-13, and IL-5) and exhibit epithelial barrier dysfunction [16,17,18,19,20,21].
Patients with CRSwNP and comorbid asthma demonstrate IgE-mediated release of immune mediators and upregulation of type 2 cytokines (IL-4, IL5, and IL-13) in the upper and lower airways [20, 21]. Further, tissue eosinophilia and high local IgE levels are typically characterized in CRSwNP with asthma [6]. Higher rates of polyp recurrence and difficult-to-treat asthma are often demonstrated in patients with CRSwNP identified as having a type-2 immune response [22]. The association between olfactory dysfunction in CRSwNP and tissue eosinophilia implies a role for eosinophils (or their associated cytokines) in partial or total loss of smell typically manifest in CRS [23, 24].
Dupilumab, an IL-4 receptor alpha antagonist, is a human monoclonal antibody of the immunoglobulin G4 subclass that specifically binds to the IL-4 receptor alpha subunit, which is shared by the IL-4 and IL-13 receptor complexes, thus inhibits IL-4 and IL-13 signaling. Dupilumab inhibits IL-4 signaling via the type 1 receptor and both IL-4 and IL-13 signaling via the type 2 receptor. It inhibits IL-4 and IL-13 cytokine-induced responses by blocking the IL-4R alpha subunit, including releasing proinflammatory cytokines, chemokines, and immunoglobulin E [25]. By blocking the shared receptor component for IL-4 and IL-13, dupilumab improves upper and lower airway outcome measures in patients with severe CRSwNP and comorbid asthma, as reported by the body of evidence [26,27,28,29,30]. The present study evaluated dupilumab efficacy in improving CRSwNP patients, with or without asthma, regarding the quality of life, olfactory symptoms, and asthma symptom control.
Patients and methods
Study design, patients, and outcome
This prospective follow-up study was conducted in a tertiary allergy center in Kuwait, Al-Rashed Allergy Center, from January 2021 till the end of May 2022. The primary outcome was to evaluate the frequency of olfactory symptoms (anosmia and hyposmia) and measure SNOT-22 after at least six months of continuous therapy with Dupilumab. The secondary outcome measured the changes in ACT scores in patients with asthma.
Diagnosis of patients with CRSwNP was based on clinical diagnostic criteria; all patients had an endoscopic assessment for nasal polyps; additionally, 141 of 166 (84.9%) patients had a history of nasal polypectomy where the radiological finding of all cases showed polypoidal nasal mucosal thickness. Individuals displaying symptoms indicative of asthma were diagnosed based on the variability of their symptoms and the reversibility of their FEV1%. If the initial spirometry results were inconclusive, further tests such as PEF variability and FeNO were conducted to confirm the diagnosis [31]. Individuals with moderate to severe chronic rhinosinusitis with nasal polyps, with or without asthma, were assessed for their eligibility to start biological therapy as per the guidelines of EPOS, 2020 [32]. Those who received dupilumab treatment for at least six months were enrolled in the study.
Demographic data, SNOT-22, and ACT scores were collected from patients’ medical charts, and all patients were followed up for at least three months. SNOT-22, olfactory symptoms frequency and ACT were re-measured. As per Toma et al., the SNOT-22 score was classified into mild, moderate, and severe [33], which later was adapted as mild and moderate versus severe.
Ethics approval and consent to participate
Ethical approval
has been obtained from Kuwait University and the Ministry of Health, in accordance with the Helsinki Declaration protocol (Research study number 2121/2022), to ensure that the research is conducted ethically and in compliance with internationally recognized standards. Informed consent has been obtained from all participants involved in the study, as well as their legal guardians, to ensure that they are fully aware of the nature and purpose of the research. They have given their voluntary and informed consent to participate.
Data collection
Basic demographic data were collected from the patient’s files, including age, sex, SNOT-22 score, nasal polyps surgery, oral corticosteroid use, presence of anosmia/hyposmia, ACT, and duration of dupilumab therapy. After at least three months of patient recruitment, ACT score, SNOT-22 score, and olfactory symptoms were reassessed.
Statistical methods
Categorical variables were presented as numbers and percentages, while continuous variables were provided as mean and standard deviation (SD). The normality of data was examined using the Shapiro-Wilk test, and the descriptive statistics were performed using Minitab 17.1.0.0 for Windows (Minitab Inc., 2013, Pennsylvania, USA). The comparison between two means or medians was made using an independent t-test or Mann-Whitney test, while the frequency comparison was made using the chi-square test. We conducted a multiple logistic regression analysis using a stepwise elimination technique to identify potential predictors of underlying asthma in patients with CRS and nasal polyps, in which the collinearity among the potential confounders was estimated using correlation coefficient, and a sensitivity analysis was done within the test by removing one potential confounder at a time and examining the changes in the coefficients of the independent variable(s). The performance of oral corticosteroid course number in predicting associated asthma was evaluated using the ROC curve, and the area under the curve (AUC) above 0.6 was considered acceptable. All tests were two-sided, and a p-value below 0.05 was considered significant.
Results
Basic characteristics of patients with CRSwNP
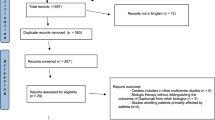
A total of 166 patients were diagnosed with CRSwNP, of which 99 cases (59.63%) were also diagnosed with asthma. However, 25 patients were excluded from the study due to not meeting the criteria for starting biologics, and an additional 33 individuals opted out of biologic treatment, as shown in Fig. 1. The mean (SD) age of patients was 43 (12) years, and 49.4% were females (Table 1); SNOT-22 score, polyposis surgery, oral corticosteroid use, and anosmia/hyposmia were significantly higher in patients with CRSwNP and asthma compared to others without asthma.
Asthma risk factors
In patients with CRSwNP, female sex and polyposis surgery were found to be significant independent risk factors for asthma, with a p-value of less than 0.05 and odds ratios of 2.13 and 4.04, respectively. Additionally, every additional course of OCS increased the likelihood of asthma coexistence up to two times more, with an odds ratio of 1.56 and a p-value of 0.05 (Table 2). Furthermore, ROC analysis was conducted to determine the ability of the number of oral corticosteroid courses to discriminate asthma coexistence in patients with CRSwNP. The results showed an area under the curve (AUC) of 0.60 with a p-value of 0.02 (Fig. 2). When the cutoff number was set at > 1.5, 2.5, and 3.5, the sensitivity and specificity were as follows: 67% and 69%, 45% and 85%, and 23% and 94%, respectively (Table 3).
ROC curve of oral corticosteroid course number to discriminate asthma coexistence in patients with CRSwNP
OCS-CN: oral corticosteroid course number, AUC: area under the curve, P < 0.05 considered significant: Receiver operating characteristic curve (ROC-curve) showed good utility of OCS-CN, AUC = 0.6, P = 0.02
Impact of dupilumab treatment
The duration of dupilumab in CRSwNP patients with asthma was significantly higher than in those without asthma (Fig. 3). The ACT scores after dupilumab treatment was significantly higher than before dupilumab, Fig. 4. For the SNOT-22 score, a significant decrease was recorded after the dupilumab treatment compared to the baseline. However, no significant difference in the SNOT-22 scores before and after dupilumab among each subgroup of CRSwNP patients, Fig. 5.
The impact of dupilumab on olfactory symptoms in Fig. 6; a significant decrease in the overall frequency of anosmia after dupilumab treatment; however, the effect of the presence of asthma was insignificant.
Discussion
This analysis examines real-life data on the effectiveness of dupilumab in improving the quality of life and olfactory symptoms of patients with CRSwNP and associated asthma. Real-world studies are conducted to verify, expand upon, and complement the findings of RCTs to comprehend better how efficacy data are applied at the point of care in routine clinical practice. Of the 166 evaluated patients, 99 (59.6%) were diagnosed with CRSwNP with asthma. These figures were comparable to others reported by Håkansson et al. [34]; to investigate the association between CRSwNP and asthma; they conducted a prospective clinical trial involving 40 CRS patients scheduled for functional endoscopic sinus surgery (FESS) and 21 control subjects. 25% (25%) of the CRSwNP patients had undiagnosed asthma, while asthma was diagnosed in 65% of them. Furthermore, lower airway obstruction in people with asthma and chronic bronchitis was linked to CRSwNP. Although asthma is frequently misdiagnosed, the fact that 25% of CRSwNP patients had undiagnosed and untreated asthma was unexpected [35]. This necessitates more collaboration between otorhinolaryngologists and pulmonologists.
Female sex, SNOT-22 score, SNOT-22 (severe), polyposis surgery, polyposis surgery number, OCS use, and OCS course number; all were statistically significantly higher in the subgroup of patients diagnosed with CRSwNP and asthma compared to the other one. These results imply that asthma independently influences CRSwNP patients’ quality of life.
The results of the current study revealed that female sex and polyposis surgery are independent risk factors for asthma in patients with CRSwNP (P < 0.05). These are compatible with a previous cross-sectional study by Li and colleagues; based on medical histories and clinical examinations, risk factors for concomitant asthma in CRSwNP patients were investigated. The study showed that among patients with CRSwNP, having a female gender, a history of allergic rhinitis, elevated serum T-IgE levels (> 69.0 kU/L), and a blood eosinophils count (> 0.35 109/L) were independent risk factors for comorbid asthma [36]. Female gender has been linked to an increased incidence of asthma in previous studies, and the presence of this factor may make asthma even more likely to occur. Numerous epidemiological studies indicate that women are more likely than men to have adult-onset asthma and more severe conditions [37,38,39].
Exploring risk factors linked to a specific phenotype may be more beneficial for managing individuals with asthma. Compared to asthmatics without CRSwNP, those with concomitant CRSwNP are likely to have more severe and persistent asthma, a lower quality of life, and fixed airflow limitation [26]. Also, asthma is more difficult to manage and more likely to exacerbate when nasal polyposis occurs. It has been demonstrated that nasal polyposis predicts the chronicity and durability of new-onset asthma [40, 41]. The emergence of asthma in CRSwNP patients appears to be cryptogenic; nevertheless, many individuals go misdiagnosed, and some may be asymptomatic [26, 42, 43]. Even rhinologists sometimes mistakenly diagnose CRSwNP as the cause of coughing and dyspnea rather than asthma. As a result, concomitant asthma in CRSwNP patients may be overlooked, especially at an early stage [26, 34, 44]. In order to develop a realistic strategy for specifically rhinologists to screen individuals at high risk, it is vital to investigate the risk factors associated with comorbid asthma in patients with CRSwNP [36].
Our results revealed that the ACT score was significantly higher after dupilumab treatment than before dupilumab treatment, which follows data reported by Dupin et al. [45]. They reported a significant improvement in median ACT scores from 14 (7–16) to 22 (17–24) (P < 0.001) after 12 months of dupilumab treatment in patients with severe asthma. These data are in accordance with results reported by Mümmler and colleagues [46]. They retrospectively analyzed 38 patients who had previously received anti-IgE or anti-IL-5/IL-5 receptor medication and were switched to dupilumab due to a bad outcome. The investigators revealed that the ACT score increased by a mean of 2.9 (P < 0.0001) while exacerbations decreased significantly (P < 0.0001). Another supportive result came from Pelaia et al. [47]; following four weeks with dupilumab, all patients observed significant improvement in severe asthma and nasal polyposis; the ACT score had significantly increased (p < 0.0001); moreover, in a more comprehensive observational study, the ACT score increased from 14 (10–18) to 22 (20–24) (p < 0.0001), [48].
For the SNOT-22 score, the significant decrease recorded after the dupilumab treatment compared to the baseline score in the current study indicated a significant impact on the patient’s QoL. This result aligns with data from a randomized controlled trial by Mustafa and colleagues [49]. AERD patients 18 or older and with a SNOT 22 score below 19 were eligible for their study. The study aimed to assess dupilumab’s effectiveness in treating AERD patients with uncontrolled CRSwNP. Their findings showed that following six months of dupilumab medication, the median baseline SNOT 22 score significantly improved from 46 [IQR: 34 to 64.8] to 9.5 [IQR: 2.5 to 19](P = 0.0050).
For the olfactory symptoms, we reported a significant decrease in the overall frequency of anosmia after dupilumab treatment which is consistent with the results demonstrated by Buchheit and colleagues [50]. They include 22 AERD patients treated with dupilumab for three months for severe asthma and CRS with nasal polyps. Clinical outcomes were assessed at baseline, 1 and 3 months after initiation of dupilumab. The study participants showed rapid improvement in clinical measures, including the sense of smell, sinonasal symptoms, and lung function after one month of treatment with dupilumab; moreover, the improvements were sustained after three months of dupilumab. There were no changes in nasal eosinophilia after dupilumab. The authors concluded that the therapeutic effects of dupilumab are likely due to decreased IL-4Rα signaling on respiratory tissue granulocytes, epithelial cells, and B cells. More than 3400 individuals with CRSwNP from 29 randomized trials evaluating nine treatment options were included in a systematic review and network meta-analysis. The findings showed that there is moderate to high certainty evidence that dupilumab improves HRQoL, sinusitis symptoms, smell, rescue OCS, rescue nasal polyp surgery, and nasal polyp size compared to standard therapy [51].
Conclusion
More than half of our cohort with CRSwNP had associated asthma. However, treatment with Dupilumab effectively controlled asthma symptoms and improved both the quality of life and olfactory symptoms.
Data Availability
The datasets used during the current study available from the corresponding author on reasonable request.
References
Fokkens W, Van Der Lans R, Reitsma S. Dupilumab for the treatment of chronic rhinosinusitis with nasal polyposis. Expert Opin Biol Ther [Internet]. 2021 May 4;21(5):575–85. Available from: https://www.tandfonline.com/doi/full/https://doi.org/10.1080/14712598.2021.1901881.
Hastan D, Fokkens WJ, Bachert C, Newson RB, Bislimovska J, Bockelbrink A et al. Chronic rhinosinusitis in Europe - an underestimated disease. A GA2LEN study. Allergy [Internet]. 2011 Sep;66(9):1216–23. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/j.1398-9995.2011.02646.x.
Hirsch AG, Stewart WF, Sundaresan AS, Young AJ, Kennedy TL, Scott Greene J et al. Nasal and sinus symptoms and chronic rhinosinusitis in a population-based sample. Allergy [Internet]. 2017 Feb;72(2):274–81. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/all.13042.
Obaseki D, Potts J, Joos G, Baelum J, Haahtela T, Ahlström M et al. The relation of airway obstruction to asthma, chronic rhinosinusitis and age: results from a population survey of adults. Allergy [Internet]. 2014 Sep 19;69(9):1205–14. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/all.12447.
Sundaresan AS, Hirsch AG, Storm M, Tan BK, Kennedy TL, Greene JS et al. Occupational and environmental risk factors for chronic rhinosinusitis: a systematic review. Int Forum Allergy Rhinol [Internet]. 2015 Nov;5(11):996–1003. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1002/alr.21573.
Laidlaw TM, Mullol J, Woessner KM, Amin N, Mannent LP. Chronic Rhinosinusitis with Nasal Polyps and Asthma. J Allergy Clin Immunol Pract [Internet]. 2021 Mar;9(3):1133–41. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2213219820311132.
Sedaghat AR. Chronic Rhinosinusitis. Am Fam Physician [Internet]. 2017 Oct 15;96(8):500–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/29094889.
Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S et al. European Position Paper on Rhinosinusitis and Nasal Polyps 2020. Rhinol J [Internet]. 2020 Feb 1;1–464. Available from: https://www.rhinologyjournal.com/Documents/Supplements/supplement_29.pdf.
Orlandi RR, Kingdom TT, Hwang PH, Smith TL, Alt JA, Baroody FM et al. International Consensus Statement on Allergy and Rhinology: Rhinosinusitis. Int Forum Allergy Rhinol [Internet]. 2016 Feb;6(S1):S22–209. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1002/alr.21695.
Mullol J, Langdon C. Nasal polyps in patients with asthma: prevalence, impact, and management challenges. J Asthma Allergy [Internet]. 2016 Mar;45. Available from: https://www.dovepress.com/nasal-polyps-in-patients-with-asthma-prevalence-impact-and-management--peer-reviewed-article-JAA.
Jarvis D, Newson R, Lotvall J, Hastan D, Tomassen P, Keil T et al. Asthma in adults and its association with chronic rhinosinusitis: The GA2LEN survey in Europe. Allergy [Internet]. 2012 Jan;67(1):91–8. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/j.1398-9995.2011.02709.x.
Håkansson K, Bachert C, Konge L, Thomsen SF, Pedersen AE, Poulsen SS et al. Airway Inflammation in Chronic Rhinosinusitis with Nasal Polyps and Asthma: The United Airways Concept Further Supported. Cormier SA, editor. PLoS One [Internet]. 2015 Jul 1;10(7):e0127228. Available from: https://doi.org/10.1371/journal.pone.0127228.
BRAUNSTAHL GJ, OVERBEEK SE, FOKKENS WJ, KLEINJAN A, McEUEN AR, WALLS AF et al. Segmental Bronchoprovocation in Allergic Rhinitis Patients Affects Mast Cell and Basophil Numbers in Nasal and Bronchial Mucosa. Am J Respir Crit Care Med [Internet]. 2001 Sep 1;164(5):858–65. Available from: https://www.atsjournals.org/doi/https://doi.org/10.1164/ajrccm.164.5.2006082.
Bachert C, Vignola AM, Gevaert P, Leynaert B, Van Cauwenberge P, Bousquet J. Allergic rhinitis, rhinosinusitis, and asthma: one airway disease. Immunol Allergy Clin North Am [Internet]. 2004 Feb;24(1):19–43. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0889856103001048.
Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008*. Allergy [Internet]. 2008 Apr;63:8–160. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/j.1398-9995.2007.01620.x.
Stevens WW, Ocampo CJ, Berdnikovs S, Sakashita M, Mahdavinia M, Suh L et al. Cytokines in Chronic Rhinosinusitis. Role in Eosinophilia and Aspirin-exacerbated Respiratory Disease. Am J Respir Crit Care Med [Internet]. 2015 Sep 15;192(6):682–94. Available from: https://www.atsjournals.org/doi/https://doi.org/10.1164/rccm.201412-2278OC.
Meng J, Zhou P, Liu Y, Liu F, Yi X, Liu S et al. The Development of Nasal Polyp Disease Involves Early Nasal Mucosal Inflammation and Remodelling. Cohen NA, editor. PLoS One [Internet]. 2013 Dec 10;8(12):e82373. Available from: https://doi.org/10.1371/journal.pone.0082373.
Holgate ST. Epithelium dysfunction in asthma. J Allergy Clin Immunol [Internet]. 2007 Dec;120(6):1233–44. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674907019768.
Robinson D, Humbert M, Buhl R, Cruz AA, Inoue H, Korom S et al. Revisiting Type 2-high and Type 2-low airway inflammation in asthma: current knowledge and therapeutic implications. Clin Exp Allergy [Internet]. 2017 Feb;47(2):161–75. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/cea.12880.
Tomassen P, Vandeplas G, Van Zele T, Cardell LO, Arebro J, Olze H et al. Inflammatory endotypes of chronic rhinosinusitis based on cluster analysis of biomarkers. J Allergy Clin Immunol [Internet]. 2016 May;137(5):1449–1456.e4. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674916001846.
Pelaia C, Heffler E, Crimi C, Maglio A, Vatrella A, Pelaia G, Canonica GW. Interleukins 4 and 13 in asthma: key pathophysiologic cytokines and druggable molecular targets. Front Pharmacol 2022 Mar 8:756.
Licari A, Brambilla I, De Filippo M, Poddighe D, Castagnoli R, Marseglia GL. The role of upper airway pathology as a co-morbidity in severe asthma. Expert Rev Respir Med [Internet]. 2017 Nov 2;11(11):855–65. Available from: https://www.tandfonline.com/doi/full/https://doi.org/10.1080/17476348.2017.1381564.
Schleimer RP. Immunopathogenesis of Chronic Rhinosinusitis and Nasal Polyposis. Annu Rev Pathol Mech Dis [Internet]. 2017 Jan 24;12(1):331–57. Available from: https://www.annualreviews.org/doi/https://doi.org/10.1146/annurev-pathol-052016-100401.
Mullol J, Mariño-Sánchez F, Valls M, Alobid I, Marin C. The sense of smell in chronic rhinosinusitis. J Allergy Clin Immunol [Internet]. 2020 Mar;145(3):773–6. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674920301135.
D’Ippolito D, Pisano M. Dupilumab (Dupixent): An Interleukin-4 Receptor Antagonist for Atopic Dermatitis. P T [Internet]. 2018 Sep;43(9):532–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/30186024.
Laidlaw TM, Bachert C, Amin N, Desrosiers M, Hellings PW, Mullol J et al. Dupilumab improves upper and lower airway disease control in chronic rhinosinusitis with nasal polyps and asthma. Ann Allergy Asthma Immunol [Internet]. 2021 May;126(5):584–592.e1. Available from: http://www.ncbi.nlm.nih.gov/pubmed/33465455.
Wechsler ME, Klion AD, Paggiaro P, Nair P, Staumont-Salle D, Radwan A et al. Effect of Dupilumab on Blood Eosinophil Counts in Patients With Asthma, Chronic Rhinosinusitis With Nasal Polyps, Atopic Dermatitis, or Eosinophilic Esophagitis. J allergy Clin Immunol Pract [Internet]. 2022 Oct;10(10):2695–709. Available from: http://www.ncbi.nlm.nih.gov/pubmed/35636689.
Nettis E, Brussino L, Patella V, Bonzano L, Detoraki A, Di Leo E et al. Effectiveness and safety of dupilumab in patients with chronic rhinosinusitis with nasal polyps and associated comorbidities: a multicentric prospective study in real life. Clin Mol Allergy [Internet]. 2022 May 19;20(1):6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/35590407.
Berger P, Menzies-Gow A, Peters AT, Kuna P, Rabe KF, Altincatal A et al. Long-term efficacy of dupilumab in asthma with or without chronic rhinosinusitis and nasal polyps. Ann Allergy, Asthma Immunol [Internet]. 2023 Feb;130(2):215–24. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1081120622019123.
Bakakos A, Schleich F, Bakakos P. Biological Therapy of Severe Asthma and Nasal Polyps. J Pers Med [Internet]. 2022 Jun 16;12(6). Available from: http://www.ncbi.nlm.nih.gov/pubmed/35743760.
Louis R, Satia I, Ojanguren I, Schleich F, Bonini M, Tonia T, Rigau D, Ten Brinke A, Buhl R, Loukides S, Kocks JW. European Respiratory Society guidelines for the diagnosis of asthma in adults. European Respiratory Journal. 2022 Sep 1;60(3).
Fokkens WJ, Lund VJ, Hopkins C, Hellings PW, Kern R, Reitsma S, Toppila-Salmi S, Bernal-Sprekelsen M, Mullol J, Alobid I, Anselmo-Lima WT. European position paper on rhinosinusitis and nasal polyps 2020. Rhinology: official organ of the International rhinologic society; 2020 Feb. p. 20.
Toma S, Hopkins C. Stratification of SNOT-22 scores into mild, moderate or severe and relationship with other subjective instruments. Rhinol J [Internet]. 2016 Jun 1;54(2):129–33. Available from: https://www.rhinologyjournal.com/Abstract.php?id=1443.
Håkansson K, Thomsen SF, Konge L, Mortensen J, Backer V, von Buchwald CA, Comparative. and Descriptive Study of Asthma in Chronic Rhinosinusitis with Nasal Polyps. Am J Rhinol Allergy [Internet]. 2014 Sep 1;28(5):383–7. Available from: http://journals.sagepub.com/doi/https://doi.org/10.2500/ajra.2014.28.4076.
Nolte H, Nepper-Christensen S, Backer V. Unawareness and undertreatment of asthma and allergic rhinitis in a general population. Respir Med [Internet]. 2006 Feb;100(2):354–62. Available from: http://www.ncbi.nlm.nih.gov/pubmed/16005621.
Li F, Wang X, Shen S, Huang K, Wang M, Liu X et al. Risk factors associated with comorbid asthma in patients with chronic rhinosinusitis with nasal polyps: a cross-sectional study. BMC Pulm Med [Internet]. 2022 Sep 7;22(1):338. Available from: http://www.ncbi.nlm.nih.gov/pubmed/36071399.
Pignataro FS, Bonini M, Forgione A, Melandri S, Usmani OS. Asthma and gender: The female lung. Pharmacol Res [Internet]. 2017 May;119:384–90. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1043661816311446.
Fuseini H, Newcomb DC. Mechanisms Driving Gender Differences in Asthma. Curr Allergy Asthma Rep [Internet]. 2017 Mar;17(3):19. Available from: http://www.ncbi.nlm.nih.gov/pubmed/28332107.
Larsen K. The Clinical Relationship of Nasal Polyps to Asthma. Allergy Asthma Proc [Internet]. 1996 Sep 1;17(5):243–9. Available from: http://www.ingentaconnect.com/content/10.2500/108854196778662255.
Westerhof GA, Coumou H, de Nijs SB, Weersink EJ, Bel EH. Clinical predictors of remission and persistence of adult-onset asthma. J Allergy Clin Immunol [Internet]. 2018 Jan;141(1):104–109.e3. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674917306620.
Wu W, Bleecker E, Moore W, Busse WW, Castro M, Chung KF et al. Unsupervised phenotyping of Severe Asthma Research Program participants using expanded lung data. J Allergy Clin Immunol [Internet]. 2014 May;133(5):1280–8. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674914001080.
Du K, Zheng M, Zhao Y, Xu W, Hao Y, Wang Y et al. Impaired small airway function in non-asthmatic chronic rhinosinusitis with nasal polyps. Clin Exp Allergy [Internet]. 2020 Dec 12;50(12):1362–71. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/cea.13747.
Williamson PA, Vaidyanathan S, Clearie K, Barnes M, Lipworth BJ. Airway dysfunction in nasal polyposis: a spectrum of asthmatic disease? Clin Exp Allergy [Internet]. 2011 Oct;41(10):1379–85. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/j.1365-2222.2011.03793.x.
Frendø M, Håkansson K, Schwer S, Rix I, Ravn AT, Backer V et al. Asthma in Ear, Nose, and Throat Primary Care Patients with Chronic Rhinosinusitis with Nasal Polyps. Am J Rhinol Allergy [Internet]. 2016 May 1;30(3):e67–71. Available from: http://journals.sagepub.com/doi/https://doi.org/10.2500/ajra.2016.30.4304.
Dupin C, Belhadi D, Guilleminault L, Gamez A, Berger P, De Blay F et al. Effectiveness and safety of dupilumab for the treatment of severe asthma in a real-life French multi‐centre adult cohort. Clin Exp Allergy [Internet]. 2020 Jul 29;50(7):789–98. Available from: https://onlinelibrary.wiley.com/doi/https://doi.org/10.1111/cea.13614.
Mümmler C, Munker D, Barnikel M, Veit T, Kayser MZ, Welte T et al. Dupilumab Improves Asthma Control and Lung Function in Patients with Insufficient Outcome During Previous Antibody Therapy. J Allergy Clin Immunol Pract [Internet]. 2021 Mar;9(3):1177–1185.e4. Available from: https://linkinghub.elsevier.com/retrieve/pii/S2213219820309624.
Pelaia C, Lombardo N, Busceti MT, Piazzetta G, Crimi C, Calabrese C, Vatrella A, Pelaia G. Short-term evaluation of dupilumab effects in patients with severe asthma and nasal polyposis. J Asthma Allergy. 2021 Sep;24:1165–72.
Pelaia C, Benfante A, Busceti MT, Caiaffa MF, Campisi R, Carpagnano GE, Crimi N, D’Amato M, Barbaro MP, Maglio A, Minenna E. Real-life effects of dupilumab in patients with severe type 2 asthma, according to atopic trait and presence of chronic rhinosinusitis with nasal polyps. Front Immunol. 2023;14.
Mustafa SS, Vadamalai K, Scott B, Ramsey A. Dupilumab as Add-on Therapy for Chronic Rhinosinusitis With Nasal Polyposis in Aspirin Exacerbated Respiratory Disease. Am J Rhinol Allergy [Internet]. 2021 May 23;35(3):399–407. Available from: http://journals.sagepub.com/doi/https://doi.org/10.1177/1945892420961969.
Buchheit KM, Sohail A, Hacker J, Maurer R, Gakpo D, Bensko JC et al. Rapid and sustained effect of dupilumab on clinical and mechanistic outcomes in aspirin-exacerbated respiratory disease. J Allergy Clin Immunol [Internet]. 2022 Aug;150(2):415–24. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674922005425.
Oykhman P, Paramo FA, Bousquet J, Kennedy DW, Brignardello-Petersen R, Chu DK. Comparative efficacy and safety of monoclonal antibodies and aspirin desensitization for chronic rhinosinusitis with nasal polyposis: A systematic review and network meta-analysis. J Allergy Clin Immunol [Internet]. 2022 Apr;149(4):1286–95. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0091674921013932.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
M.A. and A.A. wrote the manuscript text, M.K. worked on data collection, and A.A. and T.R. analyzed and interpreted the results. MA, AA and AbA were major contributors to writing up the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval has been obtained from Kuwait University and the Ministry of Health, in accordance with the Helsinki Declaration protocol (Research study number 2121/2022), to ensure that the research is conducted ethically and in compliance with internationally recognized standards. Informed consent has been obtained from all participants involved in the study, as well as their legal guardians, to ensure that they are fully aware of the nature and purpose of the research. They have given their voluntary and informed consent to participate.
Consent for publication
Not applicable.
Competing interests
All authors declare no conflict of interest. Each author has revised and approved the final version of the manuscript independently.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Al-Ahmad, M., Ali, A., Khalaf, M. et al. Comorbid asthma in patients with chronic rhinosinusitis with nasal polyps: did dupilumab make a difference?. BMC Pulm Med 23, 266 (2023). https://doi.org/10.1186/s12890-023-02556-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02556-8