Abstract
Background
With improved prognosis after lung transplantation (LTx), improving health-related quality of life (HRQL) in patients who have undergone LTx is a key goal. Although HRQL is improved significantly after transplantation, it is poorer than that in ordinary healthy people. However, the factors associated with poor HRQL remain unclear. This cross-sectional study aimed to identify the factors associated with poor HRQL in patients who have undergone LTx.
Methods
Between December 2018 and May 2022, 80 patients who had undergone LTx completed St. George’s Respiratory Questionnaire (SGRQ) as a disease-specific quality of life measure, the Short Form-12 (SF-12) as a generic quality of life measure, and modified Medical Research Council (mMRC) scale of dyspnea. The groups were assigned according to the median SGRQ-total score and the Japanese population standard for SF-12, and those with good HRQL were compared with those with poor HRQL. Independent factors were evaluated using multivariate analysis.
Results
With regard to the SGRQ, there were significant differences in the forced expiratory volume in 1 s (FEV1) (P = 0.041), use of bronchodilators (P = 0.026), 6-min walk distance (6MWD) (P < 0.001), and Mmrc (P < 0.001) between better and poorer HRQL. For the SF-12 physical component summary score (PCS), age (P = 0.017), sex (P = 0.011), FEV1 (P < 0.001), forced vital capacity (FVC) (P < 0.001), diagnosis (P = 0.011), handgrip force (P = 0.003), 6MWD (P < 0.001), and Mmrc (P < 0.001) varied. Multivariate analyses revealed that Mmrc was the only independent factor in the SGRQ (P < 0.001, odds ratio [OR] = 6.65, 95% confidence interval [CI]: 2.49–17.74) and SF-12 PCS (P = 0.001, OR = 0.185, 95% CI: 0.07–0.52). There were significant correlations between the SGRQ-Total score and SF-12 PCS (correlation coefficient = -0.612, P < 0.001).
Conclusions
Dyspnea may be an independent factor of poor disease-specific and generic HRQL in LTx patients. The management of dyspnea may improve the HRQL in patients who have undergone LTx.
Similar content being viewed by others
Background
Lung transplantation (LTx) is one of the most effective ways of treating terminal lung diseases. The clinical aim of LTx is to improve the survival rate and Health-Related Quality of Life (HRQL) [1]. The post-transplant survival rate of LTx has improved over time [2]. A 5-year unadjusted survival rate of 54% has been reported by the International Society for Heart and Lung Registry [3]. At our institute, the five-year survival rate is around 75% [4]. With the improved prognosis after LTx, the importance of improving HRQL in patients has been recognized [5, 6].
Previous reports have shown a significant improvement in HRQL in patients 3–6 months after transplantation compared with that before transplantation [6, 7]. However, these reports have also shown that HRQL in patients who have undergone LTx was poorer than that in ordinary healthy people. Some reports have indicated that chronic lung allograft dysfunction (CLAD) is a possible factor leading to poor HRQL [5, 8, 9]. Although CLAD is defined as a decrease in forced expiratory volume in 1 s (FEV1) [10], there may be a dissociation between the results of lung function tests and the patients’ perception of their own health status or disease. Some patients who show a decrease in FEV1 do not report poor health status or exercise tolerance [11]. At present, the factors associated with poor HRQL remain unclear.
Instruments for measuring HRQL are broadly categorized as disease-specific or generic. The advantages of one category typically offset the limitations of the other. Generic HRQL does not reflect respiratory disease-specific symptoms such as dyspnea, cough, and wheezing. Therefore, it is common to utilize both disease-specific and generic instruments in HRQL assessment [11]. In this study, HRQL was evaluated using both disease-specific and generic HRQL measures.
This study aimed to identify the independent factors for poor HRQL in patients after LTx by comparing patients who have better HRQL with those who have poor HRQL in both disease-specific and generic aspects of HRQL. The results may also lead to new therapies to improve HRQL in patients who have undergone LTx with long-term survival.
Methods
Participants and study design
Between March 2000 and May 2021, 136 patients underwent LTx at the Tohoku University Hospital. Among these patients, 91 patients aged ≥ 18 years who had undergone LTx > 3 months prior and were regularly scheduled for clinical follow-up visits at our hospital were included in this cross-sectional study. Forty-five patients were excluded due to the following reasons: four were aged < 18 years, three were admitted to the ward due to deterioration of lung function, and 38 died. Eight patients declined participation or were too disabled to meet. Written informed consent was obtained from all 83 patients. They completed HRQL questionnaires by themselves during their follow-up visit to our hospital between December 2019 and December 2021. Three patients were excluded from the analysis because of missing data. Thus, 80 patients were included in the final analysis. This study was approved by the Medical Ethics Committee of Tohoku University Hospital (approval number: 20181432).
Health-related quality of life
The St. George’s Respiratory Questionnaire (SGRQ) was used to evaluate respiratory disease-specific HRQL [12], whereas the Medical Outcomes Survey Short Form-12 version 2 in Japanese (SF-12) was used to evaluate generic HRQL [13].
The SGRQ is a respiratory disease-specific instrument designed to measure HRQL for chronic obstructive pulmonary disease (COPD) that has been used recently to measure HRQL for various respiratory diseases, such as lymphangioleiomyomatosis (LAM) [14] and idiopathic interstitial pneumonia [15]. An HRQL evaluation method specific to patients who have undergone LTx has not yet been fully established. The most frequently employed respiratory disease-specific HRQL instrument in patients who have undergone LTx is the SGRQ [5, 8, 16,17,18]. The scores range from 0 to 100, with higher scores indicating poorer health. The SGRQ has three components: symptoms, activities, and impacts. The total score was calculated from the summation of these three components.
The SF-12 is a validated and reliable instrument adapted from the Short Form 36-Item Health Survey that has a mean of 50 and standard deviation of 10 for the general Japanese population [19]. The SF-12 comprises the Physical Component Summary Score (PCS) and Mental Component Summary Score, which are widely used to evaluate generic HRQL across various populations [7, 20, 21]. Each scale is scored from 0 to 100, with higher scores indicating better HRQL.
The patients were allocated into two groups based on the median SGRQ-Total score. The group with a score higher than the median score of the SGRQ-Total score for all patients was designated as the high-SGQR (poor respiratory-specific HRQL) group, and the group with a lower score was designated as the low-SGQR (better respiratory-specific HRQL) group. The patients were allocated into two groups according to the Japanese population norm in the SF-12 PCS. The group with a higher score than 50 was designated as the high-PCS (better generic HRQL) group, and the group with a lower score was designated as the low-PCS (poor generic HRQL) group.
Other measures
The modified Medical Research Council (mMRC) scale was used to assess dyspnea. mMRC is a unidimensional five-point scale that describes almost the entire range of respiratory disability, from none (Grade 0) to almost complete incapacity (Grade 4). Higher scores indicate worse dyspnea [22].
Clinical data regarding, including age, sex, body mass index (BMI), time since LTx, lung function test, diagnosis before LTx, type of transplant, CLAD, hospitalization for pulmonary infections, home oxygen therapy (HOT), use of bronchodilators, use of anti-fibrotic agents, handgrip strength assessed using peak handgrip force on the dominant hand with a dynamometer, and 6-min walking distance (6MWD), were obtained from the medical records.
The same immunosuppressive protocol was implemented for all patients after LTx at our institute. All patients received 10–14 ng/ml of tacrolimus for the first 6 months, followed by 9–13 ng/ml until 12 months and 8–10 ng/ml thereafter. In addition, patients weighing above 50 kg received 1500 mg of mycophenolate, whereas those weighing below 50 kg received 1000 mg of mycophenolate. The patients also received 1.0 mg/kg of prednisolone for the first 4 days, and the dose was gradually decreased to 5 mg thereafter [4]. Patients who could not tolerate tacrolimus or mycophenolate received cyclosporine or azathioprine, respectively. None of the patients received anti-fibrotic agents during the follow-up period.
Statistical analysis
Continuous variables are presented as the mean and standard deviation, and categorical variables are presented as count frequencies. The Shapiro–Wilk test was used to compare the distributions with the standard normal distribution.
Non-normally distributed variables were compared using the Mann–Whitney U test, and normally distributed variables were compared using the t-test. Associations between categorical variables were estimated using the chi-squared test. Statistical significance was set at P-value < 0.05. Variables with P-values < 0.1 on comparison between the groups were subsequently analyzed using multivariate logistic regression to identify the independent factors of poor HRQL. Analyses were performed using the statistical software package IBM SPSS version 26.0 (SPSS Inc., Chicago, IL, USA).
Results
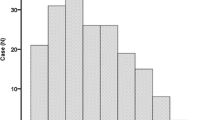
The flow diagram of the patients is shown in Fig. 1. The clinical characteristics of the study participants are shown in Table 1. Among the 80 participants, 48 (60%) were female, the average age was 47.9 ± 10.7 years, and the average time since LTx was 5.6 ± 4.3 years. The average FEV1 was 1.85 ± 0.69 L, and the average %FEV1 was 63.1 ± 19.1% predicted. Regarding diagnoses, 26 (32.5%) patients were diagnosed with LAM, 19 (23.8%) patients were diagnosed with pulmonary hypertension (PAH), 18 (22.5%) patients were diagnosed with interstitial pneumonia (IP), and seven (8.8%) patients were diagnosed with COPD. CLAD was diagnosed in 13 patients. The use of bronchodilators was reported in 23 patients, whereas the use of antifibrotic agents was not reported in any patient. The mean 6MWD was 504 ± 89.3 m. Regarding mMRC, 20 (25.0%) patients had Grade 0, 30 (37.5%) patients had Grade 1, 27 (33.8%) patients had Grade 2, and three (3.8%) patients had Grade 3.
The characteristics of the high-SGRQ and low-SGRQ groups are shown in Table 2. There were significant differences in FEV1, use of bronchodilators, 6MWD, and mMRC between the groups. There were no differences in age, sex, FVC, diagnosis, CLAD, hospitalization for pulmonary infections, or handgrip force between the groups.
Multiple regression analysis was performed to identify the independent factors for the SGRQ. In the SGRQ, variables with P-values < 0.1 were FEV1, handgrip strength, 6 MWD, and mMRC. Multivariate analysis revealed that only mMRC (P < 0.001, odds ratio [OR] = 6.65, 95% confidence interval [CI]: 2.49–17.74) was independently associated with the SGRQ (Table 3).
The characteristics of the high- and low-PCS groups are shown in Table 4. The number of participants in the high-PCS group was smaller than that in the low-PCS group. There were significant differences in age, sex, FEV1, FVC, diagnosis (COPD), handgrip force, 6 MWD, and mMRC between the groups. There were no differences in CLAD or hospitalization for pulmonary infections between the groups. Multiple regression analysis was performed to identify the independent factors for the SF-12 PCS. In the SF-12 PCS, variables with P-values < 0.1 were, age, sex, FEV1, handgrip strength, 6 MWD, and mMRC. The analysis revealed that only mMRC (P = 0.001, OR = 0.185, 95% CI: 0.07–0.52) was independently associated with the SF-12 PCS (Table 5).
There was a significant correlation between the SGRQ-Total Score and SF-12 PCS (Spearman correlation coefficient Rs = -0.612, P < 0.001) (Fig. 2).
Discussion
This study aimed to elucidate the independent factors that had the greatest influence on HRQL in patients who have undergone LTx. The mean SGRQ-Total score in our study was consistent with that reported in previous studies [8, 18, 23]. The mean SF-12 PCS in our study was also consistent with that reported in previous studies [7].
Previous studies have shown that at about 3 months after transplantation, patients experienced significant improvement in the SF-12 PCS, but no significant improvement was observed between 6 and 36 months [7, 24]. Despite substantial improvements in the generic HRQL, these patients could not reach the population norm in PCS [5, 7, 9]. Physical functioning is a particularly important factor for the improvement of HRQL, as the greatest improvements in HRQL are achieved after the improvement of physical functioning following LTx [11].
In our study, there were significant differences in FEV1, 6MWD, and mMRC between the Low-SGRQ and High-SGRQ groups. There was no significant difference in the incidence of CLAD between the low-SGRQ and high-SGRQ groups. Previous studies have shown that respiratory-specific HRQL is also worse in patients with CLAD compared with that in those without CLAD [5, 8]. Patients with advanced CLAD had profound dyspnea [11]. Severe CLAD can affect HRQL if dyspnea emerges as a subjective symptom. The lack of a significant difference related to CLAD in our data can be attributed to the small number of CLAD cases.
The multivariate logistic regression model revealed that only mMRC was an independent risk factor significantly associated with the SGRQ (Table 3). These results suggest that the risk factor that affects disease-specific HRQL is a subjective symptom rather than objective factors, such as lung function and exercise tolerance.
There were differences in age, sex, FEV1, FVC, diagnosis, handgrip force, 6 MWD, and mMRC between the Low-PCS and High-PCS groups. The ages of the patients in our study ranged from 22 to 70 years. Since it has been reported that quality of life due to physical function declines with age [11, 19], age differences in our results might lead to differential physical activity levels, resulting in differences in generic HRQL. In our study, the high proportion of females was attributed to LAM, which affects only women, being the most frequently diagnosed disease before LTx. A previous study reported poorer HRQL in women than that in men. Shahabeddin et al. [25] reported that poor HRQL among females was related to the decline in the physical domains of the Nottingham Health Profile, a generic HRQL. In our study, there was a difference in the type of disease between the low- and high-PCS groups, especially COPD. Since six of the seven patients with COPD were males, COPD may have contributed to the higher PCS.
Although Künsebeck et al. reported that the SF-12 was negatively affected by the onset of severe CLAD [20], the incidence of CLAD did not affect the SF-12 in our study. Similar to the SGRQ, this is because the number of cases of CLAD in our data was small.
The multivariate logistic regression model revealed that only mMRC was significantly associated with the SF-12 PCS scores (Table 5). The independent factor associated with better SF-12 PCS was lower dyspnea sensation, which is a patient-reported outcome, suggesting that subjective symptoms influenced generic HRQL more than objective indicators such as lung function tests and exercise tolerance.
The severity of dyspnea as a subjective symptom, rather than lung function and exercise tolerance, could be an independent factor that lowers HRQL in patients who have undergone LTx. There is a correlation between the SGRQ-Total score as a disease-specific HRQL measure and the SF-12 PCS as a generic HRQL measure (Fig. 2), suggesting that the management of dyspnea plays a pivotal role in improving the quality of life of patients who have undergone LTx.
Dyspnea is a multidimensional symptom. A comprehensive multidisciplinary approach to respiratory rehabilitation, including physical, emotional, social, and spiritual aspects of refractory dyspnea, is important according to the symptoms and background of each patient [26].
Some studies have shown that comprehensive respiratory rehabilitation, which is a combination of exercise training and education, can improve exercise tolerability and HRQL in pulmonary disease [27, 28]. Fuller et al. concluded that 7 and 14 weeks of supervised training after LTx improved exercise tolerance, muscle strength, and the SF-36 PCS scores at 14 weeks, with no significant differences between the two groups [29].
Exertional dyspnea is consistently reported to be reduced by pulmonary rehabilitation [30]. For example, in a report on patients with chronic dyspnea, HRQL and life expectancy were significantly improved by eliminating the cause of dyspnea, physical therapy, occupational therapy, the introduction of social services by social workers, and palliative and spiritual approaches [31]. Exertional dyspnea is an important problem for some patients whose symptoms worsen over time after LTx. Management of dyspnea is also important in patients who do not recover well after LTx. Continued comprehensive respiratory rehabilitation tailored to dyspnea may improve HRQL long after LTx. However, few long-term follow-up studies have been conducted on comprehensive respiratory rehabilitation after LTx. Thus, further research is required in the near future.
Our study had several limitations. First, the survivor bias in HRQL evaluation in patients with relatively good prognoses after LTx was a major limitation. Second, cross-sectional analysis has an inherent limitation in interpreting causes and effects. Although this study examined postoperative HRQL, preoperative respiratory rehabilitation has been shown to improve HRQL [32]. Further studies are needed to compare preoperative and postoperative HRQL in patients who have undergone LTx and are candidates for it.
Conclusions
Dyspnea is an independent factor that reduces both disease-specific and generic HRQL in patients who have undergone LTx. The management of dyspnea may play a pivotal role in improving HRQL in patients who have undergone LTx.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body mass index
- COPD:
-
Chronic obstructive pulmonary disease
- CLAD:
-
Chronic lung allograft dysfunction
- FEV1 :
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- HOT:
-
Home oxygen therapy
- HRQL:
-
Health-related quality of life
- IP:
-
Interstitial pneumonia
- LAM:
-
Lymphangioleiomyomatosis
- MCS:
-
Mental component summary
- mMRC:
-
Modified medical research council dyspnea scale
- PCS:
-
Physical component summary
- PAH:
-
Pulmonary arterial hypertension
- PRO:
-
Patient-reported outcome
- SGRQ:
-
St. George’s respiratory questionnaire
- SF-12:
-
Medical outcomes survey short form-12 version 2
- 6MWD:
-
6-Min walking distance
References
Singer JP, Soong A, Chen J, Shrestha P, Zhuo H, Gao Y, et al. Development and preliminary validation of the lung transplant quality of life (LT-QOL) survey. Am J Respir Crit Care Med. 2019;199(8):1008–19. https://doi.org/10.1164/rccm.201806-1198OC.
Chambers DC, Yusen RD, Cherikh WS, Goldfarb SB, Kucheryavaya AY, Khusch K, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-fourth Adult Lung And Heart-Lung Transplantation Report—2017; Focus Theme: Allograft ischemic time. J Heart Lung Transplant. 2017;36(10):1047–59. https://doi.org/10.1016/j.healun.2017.07.016.
Yusen RD, Edwards LB, Dipchand AI, Goldfarb SB, Kucheryavaya AY, Levvey BJ, et al. The Registry of the International Society for Heart and Lung Transplantation: Thirty-third Adult Lung and Heart-Lung Transplant Report—2016; Focus Theme: Primary Diagnostic Indications for Transplant. J Heart Lung Transplant. 2016;35(10):1170–84. https://doi.org/10.1016/j.healun.2016.09.001.
Nikkuni E, Hirama T, Hayasaka K, Kumata S, Kotan S, Watanabe Y, et al. Recovery of physical function in lung transplant recipients with sarcopenia. BMC Pulm Med. 2021;21(1):124. https://doi.org/10.1186/s12890-021-01442-5.
Smeritschnig B, Jaksch P, Kocher A, Seebacher G, Aigner C, Mazhar S, et al. Quality of life after lung transplantation: a cross-sectional study. J Heart Lung Transplant. 2005;24(4):474–80. https://doi.org/10.1016/j.healun.2003.12.013.
Kugler C, Strueber M, Tegtbur U, Niedermeyer J, Haverich A. Quality of life 1 year after lung transplantation. Prog Transplant. 2004;14(4):331–6. https://doi.org/10.1177/152692480401400408.
Singer JP, Katz PP, Soong A, Shrestha P, Huang D, Ho J, et al. Effect of lung transplantation on health-related quality of life in the era of the lung allocation score: a U.S. Prospective Cohort Study. Am J Transplant. 2017;17(5):1334–45. https://doi.org/10.1111/ajt.14081.
Gerbase MW, Soccal PM, Spiliopoulos A, Nicod LP, Rochat T. Long-term health-related quality of life and walking capacity of lung recipients with and without bronchiolitis obliterans syndrome. J Heart Lung Transplant. 2008;27(8):898–904. https://doi.org/10.1016/j.healun.2008.04.012.
Singer JP, Chen J, Blanc PD, Leard LE, Kukreja J, Chen H. A thematic analysis of quality of life in lung transplant: The existing evidence and implications for future directions. Am J Transplant. 2013;13(4):839–50. https://doi.org/10.1111/ajt.12174.
Verleden GM, Glanville AR, Lease ED, Fisher AJ, Calabrese F, Corris PA, et al. Chronic lung allograft dysfunction: Definition, diagnostic criteria, and approaches to treatment-A consensus report from the Pulmonary Council of the ISHLT. J Heart Lung Transplant. 2019;38(5):493–503. https://doi.org/10.1016/j.healun.2019.03.009.
Singer JP, Singer LG. Quality of Life in Lung Transplantation. Semin Respir Crit Care Med. 2013;34(03):421–30. https://doi.org/10.1055/s-0033-1348470.
Jones PW, Quirk FH, Baveystock CM, Littlejohns P. A Self-complete measure of health status for chronic airflow limitation: the St. George’s Respiratory Questionnaire. Am Rev Respir Dis. 1992;145(6):1321–7. https://doi.org/10.1164/ajrccm/145.6.1321.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. https://doi.org/10.1097/00005650-199603000-00003.
Swigris JJ, Lee HS, Cohen M, Inoue Y, Moss J, Singer LG, et al. St. George’s respiratory questionnaire has longitudinal construct validity in lymphangioleiomyomatosis. Chest. 2013;143(6):1671–8. https://doi.org/10.1378/chest.12-0161.
Swigris JJ, Brown KK, Behr J, du Bois RM, King TE, Raghu G, Wamboldt FS. The SF-36 and SGRQ: Validity and first look at minimum important differences in IPF. Respir Med. 2010;104(2):296–304. https://doi.org/10.1016/j.rmed.2009.09.006.
Ihle F, Neurohr C, Huppmann P, Zimmermann G, Leuchte H, Baumgartner R, et al. Effect of inpatient rehabilitation on quality of life and exercise capacity in long-term lung transplant survivors: a prospective, randomized study. J Heart Lung Transplant. 2011;30(8):912–9. https://doi.org/10.1016/j.healun.2011.02.006.
Stącel T, Jaworska I, Zawadzki F, Wajda-Pokrontka M, Tatoj Z, Urlik M, et al. Assessment of quality of life among patients after lung transplantation: a single-center study. Transplant Proc. 2020;52(7):2165–72. https://doi.org/10.1016/j.transproceed.2020.03.048.
Ricotti S, Vitulo P, Petrucci L, Oggionni T, Klersy C, Italian Group on QoL in Lung Transplant. Determinants of quality of life after lung transplant: an Italian collaborative study. Monaldi Arch Chest Dis. 2006;65(1):5–12. https://doi.org/10.4081/monaldi.2006.579.
Suzukamo Y, Fukuhara S, Green J, Kosinski M, Gandek B, Ware JE. Validation testing of a three-component model of Short Form-36 scores. J Clin Epidemiol. 2011;64(3):301–8. https://doi.org/10.1016/j.jclinepi.2010.04.017.
Künsebeck HW, Kugler C, Fischer S, Simon AR, Gottlieb J, Welte T, et al. Quality of life and bronchiolitis obliterans syndrome in patients after lung transplantation. Prog Transplant. 2007;17(2):136–41. https://doi.org/10.1177/152692480701700209.
Kolaitis NA, Gao Y, Soong A, Greenland JR, Hays SR, Golden J, et al. Primary graft dysfunction attenuates improvements in health-related quality of life after lung transplantation, but not disability or depression. Am J Transplant. 2021;21(2):815–24. https://doi.org/10.1111/ajt.16257.
Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest. 1988;93(3):580–6. https://doi.org/10.1378/chest.93.3.580.
Stavem K, Bjørtuft O, Lund MB, Kongshaug K, Geiran O, Boe J. Health-related quality of life in lung transplant candidates and recipients. Respiration. 2000;67(2):159–65. https://doi.org/10.1159/000029480.
Zhu X, Liang Y, Zhou H, Cai Y, Chen J, Wu B, et al. Changes in health-related quality of life during the first year in lung transplant recipients. Transplant Proc. 2021;53(1):276–87. https://doi.org/10.1016/j.transproceed.2020.06.037.
ShahabeddinParizi A, Krabbe PFM, Verschuuren EAM, Hoek RAS, Kwakkel-van Erp JM, Erasmus ME, et al. Patient-reported health outcomes in long-term lung transplantation survivors: a prospective cohort study. Am J Transplant. 2018;18(3):684–95. https://doi.org/10.1111/ajt.14492.
Pisani L, Hill NS, Pacilli AMG, Polastri M, Nava S. Management of Dyspnea in the Terminally Ill. Chest. 2018;154(4):925–34. https://doi.org/10.1016/j.chest.2018.04.003.
Rochester CL, Vogiatzis I, Holland AE, Lareau SC, Marciniuk DD, Puhan MA, et al. An official American Thoracic Society / European Respiratory Society policy statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. Am J Respir Crit Care Med. 2015;192(11):1373–86. https://doi.org/10.1164/rccm.201510-1966ST.
Spruit MA, Singh SJ, Garvey C, ZuWallack R, Nici L, Rochester C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013;188(8):e13-64. https://doi.org/10.1164/rccm.201309-1634ST.
Fuller LM, Button B, Tarrant B, Steward R, Bennett L, Snell G, et al. Longer versus shorter duration of supervised rehabilitation after lung transplantation: a randomized trial. Arch Phys Med Rehabil. 2017;98(2):220-6.e3. https://doi.org/10.1016/j.apmr.2016.09.113.
Troosters T, Casaburi R, Gosselink R, Decramer M. Pulmonary rehabilitation in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;172(1):19–38. https://doi.org/10.1164/rccm.200408-1109SO.
Higginson IJ, Bausewein C, Reilly CC, Gao W, Gysels M, Dzingina M, et al. An integrated palliative and respiratory care service for patients with advanced disease and refractory breathlessness: a randomised controlled trial. Lancet Respir Med. 2014;2(12):979–87. https://doi.org/10.1016/S2213-2600(14)70226-7.
Polastri M, Dell’Amore A, Eden A, Pehlivan E. Does preoperative rehabilitation influence the quality of life in patients who are candidates for lung transplant? Exp Clin Transplant. 2022;20(6):543–8. https://doi.org/10.6002/ect.2022.0039.
Acknowledgements
All authors are grateful to Ms. Miki Akiba, a transplant coordinator.
Funding
Satoru Ebihara is currently receiving grants (19H03984, 19K22821 and 22K19760) from JSPS KAKENHI, a grant (JP22zf01270019) from AMED, and the Research Funding for Longevity Sciences (22–1) from the National Center for Geriatrics and Gerontology. Masahiro Kohzuki is currently receiving grants (20H04054) from JSPS KAKENHI.
Author information
Authors and Affiliations
Contributions
SE is the guarantor of this manuscript and takes responsibility for all the data presented. He also contributed to the study design, data collection and analysis, and the drafting and approval of the final manuscript. RT contributed substantially to the study design, data collection and analysis, and drafting and approval of the final manuscript. TT, MK, and YO had manuscript preparation and review. All authors discussed the results, commented on the manuscript and approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Medical Ethics Committee of Tohoku University Hospital (approval number: 20181432) and conducted in accordance with the Declaration of Helsinki. Patients provided written informed consent before participation.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Takahashi, R., Takahashi, T., Okada, Y. et al. Factors associated with quality of life in patients receiving lung transplantation: a cross-sectional study. BMC Pulm Med 23, 225 (2023). https://doi.org/10.1186/s12890-023-02526-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02526-0