Abstract
Background
It is unclear whether Ureaplasma-associated pneumonia and azithromycin treatment affect the risk for bronchopulmonary dysplasia (BPD).
Methods
A retrospective cohort study was performed in very low birth weight (VLBW) infants who tested positive for Ureaplasma within 72 h after birth in a tertiary unit. Chest X-ray (CXR) and laboratory test were performed before and after azithromycin treatment. Multivariate logistic regression analysis was used to identify the independent association between BPD and Ureaplasma-associated pneumonia, as well as BPD and effective azithromycin treatment.
Results
A total of 118 infants were included in the current study, of whom 36 developed BPD (defined as supplemental oxygen needed at postmenstrual age 36 weeks or discharge). The rate of BPD was significantly higher in infants with Ureaplasma-associated pneumonia (44.6%) compared to infants with Ureaplasma colonization (17.7%, P = 0.002). After adjusting for confounders, an effective azithromycin treatment was significantly associated with reduced risk of BPD [odd ratio (OR) 0.011; 95% confidence interval (CI): 0.000–0.250), whereas Ureaplasma-associated pneumonia was not significantly associated with BPD (OR 1.835; 95% CI: 0.548–6.147).
Conclusion
Effective Azithromycin treatment in Ureaplasma positive VLBW infants was associated with a reduced risk of BPD.
Similar content being viewed by others
Background
Bronchopulmonary dysplasia (BPD) is a common complication in premature infants and remains prevalent in extremely preterm infants despite great advances in perinatal care [1, 2]. The pathogenesis of BPD is unclear and multifactorial, including but not restricted to oxygen toxicity, mechanical ventilation-induced lung injury and infection/inflammation [3]. Ureaplasma spp. has been reported as one of the earliest microbiotas colonized in the airway of premature infants, potentially contributing to the inflammatory and fibrotic profile of BPD [4]. Ureaplasma spp. has two species, Ureaplasma parvum and Ureaplasma urealyticum, with 14 known serovars. Both species were linked with preterm premature rupture of membranes (PPROM), chorioamnionitis and preterm labor. The association between Ureaplasma and BPD was first discussed by Holtzman et al. in 1989, who concluded that there was not enough evidence to prove the association [5]. Several studies also investigated the association between Ureaplasma and BPD, yielding conflicting findings [6,7,8,9]. Castro-Alcaraz and colleagues found the pattern of Ureaplasma colonization may be related to BPD, given that infants with persistent Ureaplasma had an increased risk of BPD [10]. In a systematic review and meta-analysis, pulmonary colonization with Ureaplasma increased the risk of BPD by three folds in premature infants [11]. However, a recent randomized trial reported that the eradication of Ureaplasma by azithromycin failed to decrease the risk of BPD [12]. Although the trial was underpowered to detect a difference in BPD due to funding problems [13], it indirectly supports the idea that Ureaplasma was not associated with BPD [14]. Noticeably, the detection and diagnosis criteria of Ureaplasma and BPD vary greatly among these studies, which may partially explain the elusive association between Ureaplasma and BPD.
In clinical practice, we observed that infants at a radiographically infectious status display a different respiratory clinical course than those with colonization alone. Inspired by Castro-Alcaraz and colleagues who found the pattern of Ureaplasma colonization was essential [10], this study aims to investigate the association between the proven infection of Ureaplasma with BPD and to evaluate the effect of azithromycin treatment on BPD.
Materials and methods
Study design
A retrospective cohort study was conducted at a level three neonatal intensive care unit (NICU), from June 2017 and October 2019. During the study period, preterm infants with a birth weight less thn 1500 g were routinely screened for Ureaplasma within 12 h after admission using a commercial kit (Rendu Biotechnology, Shanghai, China) by Real-time polymerase chain reaction (RT-PCR) in nasopharyngeal swabs. The RT-PCR assay detects both U. urealyticum and U. parvum, and Ureaplasma was used in the following text. The study was conducted in accordance with the Declaration of Helsinki and approved by the institute Ethical Committee. Written informed consent from the participants’ legal guardian/next of kin was not required in this study in accordance with the national legislation and the institutional requirements.
Definition
The primary outcome is bronchopulmonary dysplasia (BPD), diagnosed as an oxygen requirement at 36 weeks’ postmenstrual age (PMA) or discharge [15]. Secondary outcomes included hospital death, retinopathy of prematurity (ROP), duration of invasive and non-invasive ventilation, duration of supplemental oxygen and hospitalization. Chest-X-ray (CXR) score, assessed by the total score of three aspects: diffuse granularity, interstitial changes, and emphysema, was used to assess the pulmonary infection status in Ureaplasma positive VLBW infants [16,17,18] (Table 1). Ureaplasma-associated pneumonia was defined as Ureaplasma Rt-PCR positive with clinical manifestation of CXR score ≥ 2 (Table 1) and an increased leukocyte ≥ 25*109/L. Ureaplasma colonization was defined as Ureaplasma Rt-PCR positive with no or mild CXR score <2, or leukocyte < 25*109/L. Effect of azithromycin treatment was defined as improvement in both CXR (decrease in score) and laboratory leukocyte (less than 20*109/L). The diagnostic criteria of Ureaplasma-associated pneumonia are summarized in Table 1. The CXR was assessed by one neonatologist and one radiologist, who was blinded to the study design. The representative photos of CXR were displayed in the Supplemental figure.
Azithromycin treatment strategies
VLBW infants were routinely screened for Ureaplasma after admission. The testing result was available within 48–72 h. The treatment was initiated shortly after doctors received the results. There is no current census on azithromycin treatment for Ureaplasma in preterm infants. For infants with Ureaplasma-associated pneumonia, azithromycin was administered orally at a daily dose of ten mg/kg for a week followed by five mg/kg for the next week. This regimen was modified from Ballard et al., where they used ten mg/kg of azithromycin daily for seven days, followed by five mg/kg of azithromycin for an additional five weeks [19]. We shortened the course on consideration of the potential side effect of azithromycin. For infants with Ureaplasma colonization, ten mg/kg azithromycin was administered orally daily for three days, suspended for four days, then repeated for three days. Dosage of azithromycin for Ureaplasma colonization was modified from a local consensus [20]. Eleven infants in Ureaplasma colonized group completed half the treatment course (ten mg/Kg for three days) due to clinical sepsis and feeding intolerance. They were included in the analysis. No RT-PCR test for Ureaplasma was performed after azithromycin treatment. The efficacy of azithromycin treatment was thus assessed based on radiographic improvement and laboratory tests.
Statistics
The sample size was calculated based on a pilot study, where the rate of BPD was 48% in Ureaplasma-associated pneumonic infants, and the rate was 20% in Ureaplasma colonized VLBW infants. At an 80% power and an α = 0.05, 42 infants in each group would be sufficient to detect a significant difference. All statistical analyses were performed with IBM SPSS Statistics 24.0. In the univariate analysis, the chi-square test was used to analyse categorical variables, the nonparametric McNemar test was used for comparison of paired categorical variables, and the Student t-test was used for normally distributed continuous variables. Data were reported as numbers (%), the mean ± standard deviation, and IQR, respectively. Variates with a P-value < 0.1 were included in the multivariate logistic analysis. Multivariate analysis was performed by binary logistic regression and odds ratios (OR) and 95% confidence intervals (CI) were calculated. Statistical significance was accepted at P < 0.05.
Results
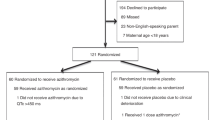
During the study period, 812 VLBW infants were admitted to the NICU. In these infants, 121 (14.9%) were tested positive for Ureaplasma. Three infants were excluded due to death before 14 days. A total of 118 infants are included in the final analysis (Fig. 1), of which 30.5% (36/118) developed BPD. The clinical characteristics of these infants were summarized in Table 2.
Infants with Ureaplasma-associated pneumonia had significantly higher risk of BPD (44.6% vs. 17.7%, P = 0.002), longer invasive ventilation (1.0 vs 0.0 day, P = 0.004], longer non-invasive ventilation (37.0 vs 19.5 days, P < 0.001), longer oxygen support (58.0 vs 33.0 days, P < 0.001) and longer hospital stay (74.0 vs 50.0 days, P < 0.001, Table 3).
We further analysed the association between Ureaplasma-associated pneumonia and BPD, as well as the association between effective azithromycin treatment and BPD, in the multivariate logistic analysis. Univariate analysis was shown in supplemental Table 1. Although a higher rate of Ureaplasma-associated pneumonia was observed in BPD infants compared with those without BPD (58.6% vs. 24.7%), the association did not reach statistically significant after adjustment [OR 1.835, 95%CI (0.548, 6.147), Table 4]. An effective azithromycin treatment was significantly associated with a reduced risk for BPD [OR 0.011, 95% CI (0.000, 0.250), Table 4].
Discussion
This study showed that Ureaplasma-associated pneumonia before treatment was not independently associated with BPD development in Ureaplasma positive VLBW infants, despite a remarkably higher rate of BPD in infants with Ureaplasma-associated pneumonia compared to those with colonization (44.6% vs. 17.7%). In contrast, an effective azithromycin treatment was significantly associated with decreased risk for BPD in Ureaplasma positive VLBW infants [OR 0.011, 95% CI (0.000, 0.250)].
Ureaplasma is smaller than bacteria in diameter and colonizes in the genitourinary tract of pregnant women. Ureaplasma might transmit to the new-borns respiratory tract in the uterus or during delivery, causing interstitial pneumonia and closely associated BPD in premature infants [8]. Some speculations are proposed on the role of Ureaplasma in the pathogenesis of BPD. Phospholipase released by Ureaplasma has long been considered as the virulence factor causing epithelium necrosis [7]. Infants who died from Ureaplasma pneumonia exhibited severe fibrosis, indicating fibroblast involvement [21]. Besides, Ureaplasma infection increased the infiltration of inflammatory cells, releasing cytokines of interleukin 6 (IL-6), matrix metalloproteinase 8 (MMP8), tumour necrosis factor α (TNFα) and contributing to late-onset sepsis (LOS) [14, 21]. These pathophysiological processes justify using interstitial pneumonia as an essential parameter for Ureaplasma infection in the current study. A recent meta-analysis demonstrated a persistent association between Ureaplasma and BPD in preterm infants. However, our findings suggest that an infective pattern of Ureaplasma was not independently associated with the onset of BPD.
Since Ureaplasma in broncho alveolar lavage fluids was first reported in 1988 [22], the role of Ureaplasma in morbidities of prematurity, especially in BPD, has drawn the great interest of neonatologists [5, 9, 23, 24]. However, infants tested positive for Ureaplasma are not routinely treated in NICUs, given that no evidence supports that eradication of Ureaplasma reduces the risk for BPD [12]. Several researchers speculated that the pattern of Ureaplasma infection might determine its contribution to BPD. Castro-Alcaraz et al. reported that only persistent Ureaplasma colonization was associated with BPD [10]. Maternal Ureaplasma abundance might increase the risk of BPD [25]. In the current study, we found Ureaplasma-associated pneumonia was not significantly associated with a higher risk of BPD, despite a striking clinical effect being noticed.
An effective azithromycin treatment was significantly associated with a reduced risk of BPD. These sort of contradictory findings indicate that azithromycin treatment might work by other mechanisms than eradicating Ureaplasma, including but not strict to the anti-inflammatory effect of azithromycin [26]. Viscardi et al. had previously reported that administration of azithromycin at a daily dose of 20 mg/kg for three days effectively eradicated Ureaplasma from the respiratory tract and tended to reduce BPD. However, the effect was not statistically significant, which could be attributed to the under power of the study [12]. The same authors reported an increased rate of death or serious respiratory morbidities in Ureaplasma positive infants (58%) compared to negative infants (21%) in a 2-years-follow-up study of the trial, indicating a compromised lung function in Ureaplasma positive infants [27].
We acknowledge that the clinical setting regarding Ureaplasma, azithromycin and BPD is highly complicated. The complicated issues include the association between Ureaplasma and BPD, azithromycin and pneumonia resolution, the influence of pneumonia on BPD, the effect of azithromycin on the development of BPD, etc. Addressing these issues would be challenging even in a series of well-designed prospective studies. However, we hope the findings in our study could add to the body of evidence regarding these topics. There could be some confounders compromising the accuracy of CXR assessment. A severe RDS might interfere with the initial assessment of CXR (20% in this cohort), while other concurrent pulmonary infections and PDA might impede the second accurate assessment of CXR. Furthermore, sampling from tracheal aspirates would be more accurate than nasopharyngeal swabs in PCR testing for Ureaplasma [27].
In summary, we found that radiographic improvement following azithromycin treatment was associated with a reduced risk for BPD in Ureaplasma positive VLBW infants. However, these data need to be interpreted with caution since potential confounders might affect the accuracy of the CXR evaluation.
Availability of data and materials
The raw data supporting the conclusions of this article will be made available by the corresponding authors to any qualified researcher.
References
Thébaud B, Goss KN, Laughon M, Whitsett JA, Abman SH, Steinhorn RH, et al. Bronchopulmonary dysplasia. Nat Rev Dis. 2019;5:78.
Tracy MK, Berkelhamer SK. Bronchopulmonary Dysplasia and Pulmonary Outcomes of Prematurity. Pediatr Ann. 2019;48:e148–53.
Savani RC. Modulators of inflammation in Bronchopulmonary Dysplasia. Semin Perinatol. 2018;42:459–70.
Pammi M, Lal CV, Wagner BD, Mourani PM, Lohmann P, Luna RA, et al. Airway Microbiome and Development of Bronchopulmonary Dysplasia in Preterm Infants: A Systematic Review. J Pediatr. 2019;204:126-33.e2.
Holtzman RB, Hageman JR, Yogev R. Role of Ureaplasma urealyticum in bronchopulmonary dysplasia. J Pediatr. 1989;114:1061–3.
van Waarde WM, Brus F, Okken A, Kimpen JL. Ureaplasma urealyticum colonization, prematurity and bronchopulmonary dysplasia. Eur Respir J. 1997;10:886–90.
Kallapur SG, Kramer BW, Jobe AH. Ureaplasma and BPD. Semin Perinatol. 2013;37:94–101.
Gancia P, Delogu A, Pomero G. Ureaplasma and bronchopulmonary dysplasia. Early Human Dev. 2014;90(Suppl 1):S39-41.
Viscardi RM, Kallapur SG. Role of Ureaplasma Respiratory Tract Colonization in Bronchopulmonary Dysplasia Pathogenesis: Current Concepts and Update. Clin Perinatol. 2015;42:719–38.
Castro-Alcaraz S, Greenberg EM, Bateman DA, Regan JA. Patterns of colonization with Ureaplasma urealyticum during neonatal intensive care unit hospitalizations of very low birth weight infants and the development of chronic lung disease. Pediatrics. 2002;110:e45.
Lowe J, Watkins WJ, Edwards MO, Spiller OB, Jacqz-Aigrain E, Kotecha SJ, et al. Association between pulmonary ureaplasma colonization and bronchopulmonary dysplasia in preterm infants: updated systematic review and meta-analysis. Pediatr Infect Dis J. 2014;33:697–702.
Viscardi RM, Terrin ML, Magder LS, Davis NL, Dulkerian SJ, Waites KB, et al. Randomised trial of azithromycin to eradicate Ureaplasma in preterm infants. Arch Dis Child Fetal Neonatal Ed. 2020;105(6):615–22.
Gandecha H, Boyle EM. Randomised trial of azithromycin to eradicate Ureaplasma in preterm infants. Acta Paediatrica (Oslo, Norway: 1992). 2022;111:696–7.
Glaser K, Gradzka-Luczewska A, Szymankiewicz-Breborowicz M, Kawczynska-Leda N, Henrich B, Waaga-Gasser AM, et al. Perinatal Ureaplasma Exposure Is Associated With Increased Risk of Late Onset Sepsis and Imbalanced Inflammation in Preterm Infants and May Add to Lung Injury. Front Cell Infect Microbiol. 2019;9:68.
Jensen EA, Dysart K, Gantz MG, McDonald S, Bamat NA, Keszler M, et al. The Diagnosis of Bronchopulmonary Dysplasia in Very Preterm Infants. An Evidence-based Approach. Am J Respir Crit Care Med. 2019;200:751–9.
Crouse DT, Odrezin GT, Cutter GR, Reese JM, Hamrick WB, Waites KB, et al. Radiographic changes associated with tracheal isolation of Ureaplasma urealyticum from neonates. Clin Infect Dis. 1993;17(Suppl 1):S122–30.
Theilen U, Lyon AJ, Fitzgerald T, Hendry GM, Keeling JW. Infection with Ureaplasma urealyticum: is there a specific clinical and radiological course in the preterm infant? Arch Dis Child Fetal Neonatal Ed. 2004;89:F163–7.
Pacifico L, Panero A, Roggini M, Rossi N, Bucci G, Chiesa C. Ureaplasma urealyticum and pulmonary outcome in a neonatal intensive care population. Pediatr Infect Dis J. 1997;16:579–86.
Ballard HO, Shook LA, Bernard P, Anstead MI, Kuhn R, Whitehead V, et al. Use of azithromycin for the prevention of bronchopulmonary dysplasia in preterm infants: a randomized, double-blind, placebo controlled trial. Pediatr Pulmonol. 2011;46:111–8.
Respiratory branch of Chinese Pediatric Society CMA. Expert Consensus on the Diagnosis and Treatment of Mycoplasma Pneumoniae Pneumonia in Children and Adolescents (2015 Edition). Chin J Appl Clin Pediatr. 2015;30:5.
Viscardi RM. Ureaplasma species: role in diseases of prematurity. Clin Perinatol. 2010;37:393–409.
Parides GC, Bloom JW, Ampel NM, Ray CG. Mycoplasma and ureaplasma in bronchoalveolar lavage fluids from immunocompromised hosts. Diagn Microbiol Infect Dis. 1988;9:55–7.
Viscardi RM. Ureaplasma species: role in neonatal morbidities and outcomes. Arch Dis Child Fetal Neonatal Ed. 2014;99:F87-92.
Abele-Horn M, Genzel-Boroviczény O, Uhlig T, Zimmermann A, Peters J, Scholz M. Ureaplasma urealyticum colonization and bronchopulmonary dysplasia: a comparative prospective multicentre study. Eur J Pediatr. 1998;157:1004–11.
Chun J, Chun SH, Han YS, Sung TJ. Different degrees of maternal Ureaplasma colonization and its correlation with bronchopulmonary dysplasia in <32 weeks’ preterm infants. Pediatr Neonatol. 2019;60:441–6.
Cramer CL, Patterson A, Alchakaki A, Soubani AO. Immunomodulatory indications of azithromycin in respiratory disease: a concise review for the clinician. Postgrad Med. 2017;129:493–9.
Viscardi RM, Terrin ML, Magder LS, Davis NL, Dulkerian SJ, Waites KB, et al. Randomized trial of azithromycin to eradicate Ureaplasma respiratory colonization in preterm infants: 2-year outcomes. Pediatr Res. 2022;91:178–87.
Acknowledgements
The authors kindly acknowledge Chun Chen for her help in data collection.
Funding
This study supported by Shenzhen Science and Technology Innovation Committee (JCYJ20190809170009528 to XC), Shenzhen Fund for Guangdong Provincial Highlevel Clinical Key Specialties (SZGSP009) and Liuzhou Science and Technology Bureau Self-funding Project (2020NBAB0115Zi, XH). The funders are not involved in any process of the study.
Author information
Authors and Affiliations
Contributions
XC and XH conceptualized and designed the study and wrote the first draft of the manuscripts. YL carried out the clinical data collection. BL and CY (Chunyu) scored the Chest-X-ray. ZH performed data analysis. XC and CY reviewed and revised the manuscript. All authors read and approved the final manuscript. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Shenzhen Maternity and Child Healthcare Hospital Ethical Committee approved the collection and usage of the clinical information for research purposes and waived the requirement for informed consent [SFYLS (2019)-065]. All methods were carried out in accordance with Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplemental Figure.
Representative photos of CXR in diffuse granularity, interstitial changesand emphysema, with none, mild and severe changes.
Additional file 2: Supplemental Table 1.
Clinical characteristics stratified by BPD status.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, X., Huang, X., Lin, Y. et al. Association of Ureaplasma infection pattern and azithromycin treatment effect with bronchopulmonary dysplasia in Ureaplasma positive infants: a cohort study. BMC Pulm Med 23, 229 (2023). https://doi.org/10.1186/s12890-023-02522-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02522-4