Abstract
Background
Numerous reports have shown that medical treatment confers excellent survival benefits to patients with advanced stage IV non-small cell lung cancer (NSCLC). However, the implications of surgery for primary lesions as palliative treatment remain inconclusive.
Methods
We retrospectively extracted clinical data from the Surveillance, Epidemiology, and End Results Program (SEER) database and selected patients with stage IV NSCLC. Patients were classified into non-surgery and surgery groups, and propensity score matching (PSM) analysis was performed to balance the baseline information. Patients in the surgery group, whose overall survival (OS) was longer than the median survival time of those in the non-surgery group, were deemed to benefit from surgery. We evaluated the efficacy of three surgical techniques, namely, local destruction, sub-lobectomy, and lobectomy, on the primary site in the beneficial population.
Results
The results of Cox regression analyses revealed that surgery was an independent risk factor for both OS (hazard ratio [HR]: 0.441; confidence interval [CI]: 0.426–0.456; P < 0.001) and cancer-specific survival (CSS) (HR: 0397; CI: 0.380–0.414; P < 0.001). Notably, patients who underwent surgery had a better prognosis than those who did not (OS: P < 0.001; CSS: P < 0.001). Moreover, local destruction and sub-lobectomy significantly compromised survival compared to lobectomy in the beneficial group (P < 0.001). After PSM, patients with stage IV disease who underwent lobectomy needed routine mediastinal lymph node clearing (OS: P = 0.0038; CSS: P = 0.039).
Conclusion
Based on these findings, we recommend that patients with stage IV NSCLC undergo palliative surgery for the primary site and that lobectomy plus lymph node resection should be conventionally performed on those who can tolerate the surgery.
Similar content being viewed by others
Introduction
According to the Global Cancer Statistics of 2020, approximately 19.3 million new cases and 10 million cancer-related deaths occurred in 2020 alone, with lung cancer being classified as the most lethal cancer [1]. Current advancements in diagnostics and medical technology have contributed to significant improvement in the survival of patients with non-small cell lung cancer (NSCLC), which accounts for 80% of all lung cancer cases. In the United States, the 5-year survival rate of patients with NSCLC has improved from 16.4% to 25.1% from 1975 to 2015. However, almost 55% of these patients eventually develop advanced lung cancers [2, 3]. Although immune therapy and targeted drugs have significantly improved patient prognosis, the future of advanced tumour treatment remains unknown, necessitating further research. Notably, surgery is generally not recommended for patients with advanced NSCLC, especially for those with distant progression. Nevertheless, some scholars have suggested that surgical operations should be expanded to include patients with stage IV NSCLC, especially those with oligometastatic tumours [4,5,6,7]. However, the benefit of surgery in patients with advanced NSCLC is inconclusive, and the most optimal surgical technique among local destruction, ablation therapy, sub-lobectomy, and lobectomy, remains unknown [8]. In the present study, we analysed the clinical information of patients with stage IV NSCLC from the Surveillance, Epidemiology, and End Results Program (SEER) database and investigated the implications of surgery on survival outcomes.
Methods
Patient selection
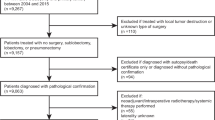
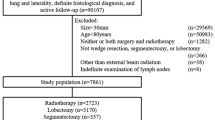
Clinical data for patients diagnosed with NSCLC between 2004–2016 (C34.0–C34.9) were extracted from the SEER database. A total of 122,650 patients with stage IV NSCLC were retrospectively selected, and the surgical codes for the primary site were set as 00 (non-surgery); 12, 13, and 15 (local destruction: ablation); 21 and 22 (sub-lobectomy); and 30 and 33 (lobectomy with or without mediastinal lymph node clearing). Pathologies were defined as large cell carcinoma, adenocarcinoma, squamous cell carcinoma, adenosquamous carcinoma, and neuroendocrine carcinoma. Patients with small cell lung cancer, as well as those with unknown TNM stage and unknown survival status, including cancer-specific survival (CSS), were excluded from the list.
Study design
Eligible patients were divided into the non-surgery group (code 00) and surgery group (codes 12, 13, 15, 21, 22, 30, and 33), based on the operation on the primary site. Further, we compared the long-term outcomes between the groups after balancing their baseline information. Notably, we classified patients whose median survival times were greater than those in the non-surgical group into the benefit group. We compared different outcomes among the three surgical methods: local destruction, lobectomy, and sub-lobectomy, including wedge resection and segmental resection. Furthermore, we investigated the significance of lymph node dissection in the lobectomy group after balancing the baseline characteristics. The TNM stage in this study was reclassified according to the American Joint Committee on Cancer (AJCC), 8th version, and the outcomes were overall survival (OS) and CSS (Fig. 1).
Statistical analysis
Statistical analyses were performed using SAS version 9.4 and packages implemented in R software version 4.0.3. Continuous variables are expressed as means ± standard deviations. Differences in continuous variables between the two groups were compared using independent two-sample t-test, whereas those for categorical variables were analysed using Fisher’s exact or chi-square tests. Baseline characteristics between the surgery and non-surgery groups were balanced using propensity score matching (PSM; Caliper = 0.001). Further, we applied the product-limit algorithm implemented using the Kaplan–Meier method and the log-rank test to evaluate OS and CSS. Thereafter, we performed Cox regression analyses based on univariate and multivariate methods to determine the significance of surgery in stage IV NSCLC (Method = “enter”). We also applied the nearest propensity score on the logit scale to a 1:1 match (Caliper = 0.01) for the lymph node dissection and non-dissection groups to evaluate the implication of lymph node resection in the lobectomy group. Additionally, we manually converted multiple categorical variables to dummy variables for regression analysis. Statistical significance was set at P ≤ 0.05.
Results
Baseline characteristics of patients with stage IV NSCLC
A summary of the baseline characteristics of the two groups is presented in Table 1. A total of 122,650 patients were included, of whom 3.70% underwent surgery. Before PSM, we collected clinical information regarding age, race, sex, laterality, position, T stage, N stage, M stage, clinical stage, grade, histology, radiation, chemotherapy, and distant progression. Almost all variables were unbalanced between the surgical and non-surgical groups. Notably, the lesions were more common in the upper lobes. Additionally, adenocarcinoma accounted for the majority of pathological types, with most of the patients having grade III and stage IVa. After PSM, we found a total of 4,232 patients in the two matched groups, and all baseline variables were 1:1 matched and finally balanced (Table 1).
Efficacy of surgery on OS and CSS
The variables with significant differences (P < 0.05) in the univariate analysis were selected for the multivariate Cox analysis (Table 2). Results from the Cox analysis indicated that surgical operation was a significant independent risk factor for both OS (hazard ratio [HR]: 0.441; confidence interval [CI]: 0.426–0.456; P < 0.001) and CSS (HR: 0.397; CI: 0.380–0.414; P < 0.001). Additionally, T, N, and M stages, as well as grade (P < 0.001), significantly correlated with the prognosis of patients with advanced NSCLC after surgery.
Efficacy of surgery on the prognosis of patients with stage IV NSCLC
We applied the log-rank test to compare the survival rates between patients in the non-surgery and surgery groups in the matched population after PSM and then generated Kaplan–Meier curves to investigate patient survival (Fig. 2). The results revealed that patients in the surgery group had a significantly better prognosis than those in the non-surgery group, regardless of OS or CSS (P < 0.001). The median survival (MS) times for OS were 7 and 19 months in the non-surgery and surgery groups, respectively. Regarding CSS, we found an MS of 11 and 33 months for the non-surgery and surgery groups, respectively. Results from the long-term follow-up revealed 1-, 5-, and 10-year OS rates of 34.5%, 5.4%, and 1.3%, respectively, for the non-surgery group, while those of the palliative surgery group were 61.2%, 22.4%, and 11.2%, respectively. Based on these survival rates, we stratified patients who had OS rates greater than the MS times in the non-surgery group into two categories, namely beneficial and non-beneficial groups (P < 0.001).
Effect of surgical methods on the beneficial group after PSM
Three surgical methods were used to treat patients with advanced NSCLC between 2004–2016. Local destruction, sub-lobectomy, and lobectomy were performed in 129, 1078, and 1844, patients, respectively. Local destruction included laser ablation, microwave ablation, cryoablation, and radiofrequency ablation, whereas sub-lobectomy included segmental and wedge resection. Statistically significant differences were observed between the groups (P < 0.001) (Fig. 3). The results from the log-rank test indicated that local destruction had the worst prognosis (MS = 21 months), with 1-, 5-, and 10-year OS rates of 79.8%, 11.2%, and 2.9%, respectively. Moreover, sub-lobectomy with a MS of 28 months and 1-, 5-, and 10-year OS rates of 81.7%, 25.7%, and 11.8%, respectively, had worse long-term outcomes than lobectomy (MS = 38 months; and 1-, 5-, and 10-year OS rates of 87.1%, 35.5%, and 18.6%, respectively).
Efficacy of mediastinal lymph node dissection in the lobectomy technique
We found no statistically significant differences in OS (P = 0.07) and CSS (P = 0.37) between the two groups before matching (Fig. 4). Considering the interference of baseline characteristics, we repeated PSM in the lymph node resection and non-resection surgery groups. After PSM, it was clear that lymph node clearing is beneficial for patients with stage IV NSCLC (OS: P = 0.0038; CSS: P = 0.039) (Fig. 5), as evidenced by the MS and OS times of 30 and 46 months, respectively. However, no significant differences were observed with regard to long-term outcomes, with the non-dissection group showing 1-, 5-, and 10-year OS rates of 82.7%, 32.7%, and 19.0%, respectively, while those in the other group were 88.6%, 36.5%, and 18.4% at 1, 5, and 10 years, respectively.
Discussion
According to the Global Cancer Statistics of 2020, lung cancer, which accounts for an estimated 1.8 million deaths, remains a major deadly disease, second only to breast cancer [1]. Although previous studies have shown that surgical intervention is beneficial for patients with early cell lung cancer and has a good prognosis, the feasibility of this approach for stage III-IV NSCLC remains controversial [9]. Numerous studies have shown that the prognosis of patients with resectable stage III NSCLC who undergo surgery after neoadjuvant therapy depends on lymph node invasion [10]. Moreover, surgery is generally discouraged in patients with stage IV NSCLC because of their limited survival time [11]. In the present study, we found that palliative surgery improved the prognosis of patients with stage IV NSCLC to some extent, as evidenced by a 2-fold longer MS times in the surgical group than in the non-surgical group. These findings were consistent with those of He et al., [5] who reported a predictive model for identifying optimal patients with stage IV NSCLC for surgery. Results from another study that analysed a SEER dataset, found that patients with stage IV NSCLC had superior OS following thoracic surgery in combination with chemotherapy or chemoradiation. Patients who underwent surgery had longer MS times (15 months) than those in the non-surgery group (8 months) [12].
The 5-year survival rate (22.4%) recorded in the present study was comparable to that reported by Hanagiri et al., [13] who reported long-term follow-up outcomes of 25% in patients with stage IV NSCLC after surgical resection of the primary lesion, as well as aggressive treatment of metastases using radiotherapy, stereotactic radiosurgery (SBRT), or surgery [13]. Additional evidence showed that salvage lung resection of R0 after concurrent neoadjuvant chemoradiotherapy (CRT) was necessary for advanced lung cancer in patients who could tolerate the surgery and was accompanied by a MS time of 24 months. Moreover, their findings further indicated that non-extensive lung resection was sufficient, with a prognostic value comparable to that of extensive surgery [6, 14]. Apart from CRT, targeted therapy is the most common drug-based treatment for advanced patients with positive driver genes, while EGFR mutations are the most frequently targeted genetic factor. The retrospective study conducted by Gong et al., revealed the safety and rationality of palliative surgery after 2–46 months of targeted therapy, with median event-free and postoperative survival rates of 14 and 17 months, respectively [15]. SBRT has also been found to be a selective therapy for metastases [4]. Notably, an acceptable prognosis for salvage surgery was observed following SBRT, with 5-year progression-free survival and OS rates of 15% and 40.6%, respectively [16].
We also compared three types of surgical techniques, namely local destruction (laser ablation, microwave ablation, cryoablation, and radiofrequency ablation), sub-lobectomy (segmental resection and wedge resection), and lobectomy, and found that lobectomy was superior to the others, as evidenced by the highest long-term prognosis. Conversely, the ablation technique was the least effective, although it was still superior to the non-surgery group, which is consistent with previous studies. Ablation has recently emerged as a treatment option for patients with advanced tumours. Indeed, Solomon et al., [17] demonstrated advantages of thermal ablation over surgery for the treatment of lesions < 3 cm (especially < 2 cm) in terms of safety and quality of life. Notably, patients who underwent ablation therapy exhibited longer OS when the lesion was < 3 cm relative to those in the non-surgery group, with 5-year survival rates of 10% and 5% in the ablation and no surgery groups, respectively [18]. Cryoablation is another new alternative to thermal ablation that may enhance treatment responses to immunotherapy in patients with advanced lung cancer (cryoimmunotherapy) [19].
In the present study, although patients who received lobectomy were found to have a good prognosis, ablation therapy was considered a good choice for patients who could not tolerate surgical trauma. However, the lobectomy approach remains controversial given that its benefits in progression-free and OS rates, as well as in enhancing the quality of life, remain unclear for mediastinal lymph node clearing during surgery. The results of the present study support the use of lymph node resection, consistent with the findings of Dr Daniel L and Daigo Kawano. Miller showed that the presence of mediastinal lymph node metastases significantly affected the postoperative 5-year survival rates of patients with distant metastasis [20, 21]. However, further studies are required to validate these findings.
This study has some limitations that warrant discussion. First, as this was a retrospective study, we anticipate some bias compared to that observed with randomised controlled trials. Second, we only extracted clinical information on chemotherapy and radiotherapy but not about other treatment approaches such as targeted therapy and immunotherapy. Third, the efficacy of drug therapy or surgery in patients with distant metastasis is unclear. It is possible that the postoperative prognosis of patients with advanced NSCLC is affected by distant organ types. As surgery on different oligometastatic systems can generate different results [22], further research is needed to ascertain the efficacy of standard treatment in patients with stage IV NSCLC.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. 2021;71(1):7–33.
SEER Cancer Statistics Review, 1975–2016, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2016/, based on November 2018 SEER data submission, posted to the SEER web site, April 2019.
Opitz I. Commentary: surgery expanding to stage IV non-small cell lung cancer treatment?! J Thorac Cardiovasc Surg. 2021;161(4):1508–9.
Liang H, Liu Z, Huang J, Liu J, Wang W, Li J, Xiong S, Li C, Cheng B, Zhao Y, et al. Identifying optimal candidates for primary tumor resection among metastatic non-small cell lung cancer patients: a population-based predictive model. Transl Lung Cancer Res. 2021;10(1):279–91.
Coster JN, Groth SS. Surgery for locally advanced and oligometastatic non-small cell lung cancer. Surg Oncol Clin N Am. 2020;29(4):543–54.
David EA, Andersen SW, Beckett LA, Melnikow J, Clark JM, Brown LM, Cooke DT, Kelly K, Canter RJ. Survival benefits associated with surgery for advanced non-small cell lung cancer. J Thorac Cardiovasc Surg. 2019;157(4):1620–8.
Collaud S, Stahel R, Inci I, Hillinger S, Schneiter D, Kestenholz P, Weder W. Survival of patients treated surgically for synchronous single-organ metastatic NSCLC and advanced pathologic TN stage. Lung Cancer. 2012;78(3):234–8.
Yokoi K, Taniguchi T, Usami N, Kawaguchi K, Fukui T, Ishiguro F. Surgical management of locally advanced lung cancer. Gen Thorac Cardiovasc Surg. 2014;62(9):522–30.
Donington JS, Pass HI. Surgical approach to locally advanced non-small cell lung cancer. Cancer J. 2013;19(3):217–21.
Roy MS, Donington JS. Management of locally advanced non small cell lung cancer from a surgical perspective. Curr Treat Options Oncol. 2007;8(1):1–14.
Jia J, Guo B, Yang Z, Liu Y, Ga L, Xing G, Zhang S, Jin A, Ma R, Wang J. Outcomes of local thoracic surgery in patients with stage IV non-small-cell lung cancer: a SEER-based analysis. Eur J Cancer. 2021;144:326–40.
Hanagiri T, Takenaka M, Oka S, Shigematsu Y, Nagata Y, Shimokawa H, Uramoto H, Tanaka F. Results of a surgical resection for patients with stage IV non–small-cell lung cancer. Clin Lung Cancer. 2012;13(3):220–4.
Bograd AJ, Mann C, Gorden JA, Gilbert CR, Farivar AS, Aye RW, Louie BE, Vallières E. Salvage lung resections after definitive chemoradiotherapy: a safe and effective oncologic option. Ann Thorac Surg. 2020;110(4):1123–30.
Song W, Di S, Liu J, Fan B, Zhao J, Zhou S, Chen S, Dong H, Yue C, Gong T. Salvage surgery for advanced non-small cell lung cancer after targeted therapy: a case series. Thorac Cancer. 2020;11(4):1061–7.
Kobayashi AK, Horinouchi H, Nakayama Y, Ohe Y, Yotsukura M, Uchida S, Asakura K, Yoshida Y, Nakagawa K, Watanabe SI. Salvage surgery after chemotherapy and/or radiotherapy including SBRT and proton therapy: a consecutive analysis of 38 patients. Lung Cancer. 2020;145:105–10.
Ghosn M, Solomon SB. Current management of oligometastatic lung cancer and future perspectives: results of thermal ablation as a local ablative therapy. Cancers (Basel). 2021;13(20):5202.
Halsey K, Wu J, Su C, Hsieh B, Yi T, Collins SA, Kimia B, Zhang PJ, Healey T, Zhang Z, et al. Ablation therapy for advanced stage non-small cell lung cancer: a national cancer database study. J Vasc Interv Radiol. 2020;31(8):1210-1215.e1214.
Katzman D, Wu S, Sterman DH. Immunological aspects of cryoablation of non-small cell lung cancer: a comprehensive review. J Thorac Oncol. 2018;13(5):624–35.
Billing PS, Miller DL, Allen MS, Deschamps C, Trastek VF, Pairolero PC. Surgical treatment of primary lung cancer with synchronous brain metastases. J Thorac Cardiovasc Surg. 2001;122(3):548–53.
Kawano D, Takeo S, Katsura M, Tsukamoto S, Masuyama E, Nakaji Y. Surgical treatment of stage IV non-small cell lung cancer. Interact Cardiovasc Thorac Surg. 2012;14(2):167–70.
Pfannschmidt J, Dienemann H. Surgical treatment of oligometastatic non-small cell lung cancer. Lung Cancer. 2010;69(3):251–8.
Acknowledgements
The datasets generated and/or analysed during the current study are obtained from publicly available database which can be accessed from the https://seer.cancer.gov/
Informed consent statement
The submission of manuscript has been verified and approved by all authors.
Funding
This research was funded by National Natural Science Fundation of China Project No. 81871497.
Author information
Authors and Affiliations
Contributions
Conception and design were performed by Jianghao Ren, Qiang Tan. Material preparation, data collection was taken by Jianghao Ren, Jiangbin Ren, Kan Wang. Statistic analysis were operated by Qiang tan, Jianghao Ren, Jiangbin Ren, Kan Wang. All authors contributed to the manuscript writing and final approval of manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by by Ethics Committee in Shanghai Chest hospital.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ren, J., Ren, J., Wang, K. et al. The consideration of surgery on primary lesion of advanced non-small cell lung cancer. BMC Pulm Med 23, 118 (2023). https://doi.org/10.1186/s12890-023-02411-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02411-w