Abstract
Objective
We aimed to identify new classes in acute respiratory distress syndrome (ARDS) using physiological and clinical variables and to explore heterogeneity in the effects of glucocorticoid therapy between classes.
Methods
Using the Medical Information Mart for Intensive Care-IV database, we identified patients with ARDS. Potential profile analysis was used to identify classes with physiological and clinical data as delineating variables. Baseline characteristics and clinical outcomes were compared between classes. The effect of glucocorticoid treatment was explored by stratifying by class and glucocorticoid treatment.
Results
From 2008 to 2019, 1104 patients with ARDS were enrolled in the study. The 2-class potential analysis model had the best fit (P < 0.0001), with 78% of patients falling into class 1 and 22% into class 2. Additional classes did not improve the model fit. Patients in class 2 had higher anion gap, lactate, creatinine, and glucose levels and lower residual base, blood pressure, and bicarbonate compared with class 1. In-hospital mortality and 28-day mortality were significantly higher among patients in class 2 than those in class 1 (P < 0.001). Heterogeneity of glucocorticoid treatment was observed, stratified by class and treatment, with no significant effect in class 1 (P = 0.496), increased mortality in class 2 (P = 0.001), and a significant interaction (P = 0.0381). In class 2, 28-day survival was significantly lower with glucocorticoid treatment compared with no hormone treatment (P = 0.001).
Conclusion
We used clinical and physiological variables to identify two classes of non-COVID-19-associated ARDS with different baseline characteristics and clinical outcomes. The response to glucocorticoid therapy varied among different classes of patients.
Similar content being viewed by others
Introduction
Acute respiratory distress syndrome (ARDS) is a complex and heterogeneous clinical syndrome defined on the basis of clinical criteria. In the 50 years since Ashbaugh and colleagues first described ARDS, substantial progress has been made in identifying causative factors of the syndrome and improving ventilatory support for patients [1]. Although the mechanisms that cause ARDS are now better understood than ever before and decades of progress have been made in the experimental understanding of ARDS and in preclinical studies to identify potentially effective new therapies, most clinical trials of ARDS have not shown a benefit in terms of mortality [2, 3]. In recent years, an explanation for the failure of these clinical trials has been proposed, namely, that ARDS has widely defined criteria, which inevitably leads to clinical and biological heterogeneity [4]. The large amount of clinical and biological heterogeneity in this syndrome is widely recognized as an important barrier to identifying effective treatments for ARDS.
To reduce heterogeneity, recent studies have focused on identifying specific ARDS subphenotypes or endophenotypes of patients who either have a higher risk of disease-related outcomes (prognostic enrichment) or respond differently to treatment (predictive enrichment), allowing for accurate drug trials in critical care [5, 6]. In 2014, Calfee and colleagues conducted a review of two reanalyses of baseline clinical and plasma biomarker data from patients with ARDS in randomized controlled trials (RCTs; the ARMA study and the ALVEOLI study) and identified two ARDS subgroups: a hyperinflammatory phenotype characterized by higher levels of inflammatory biomarkers, shock, metabolic acidosis, and mortality, and a second, non-hyperinflammatory phenotype [7]. In addition, Famous et al. used latent class analysis to reanalyze baseline clinical and biomarker data from 1000 patients with ARDS in the RCT “Fluid and Catheterization Trial” (FACTT) and identified two different phenotypes that were similar but responded differently to fluid management strategies [8]. A number of subsequent ARDS subphenotype studies have also identified two distinct ARDS phenotypes with similar clinical outcomes (mortality, ventilator-free days, organ failure-free days and days in the intensive care unit [ICU]) [9,10,11]. Importantly, with respect to the idea that the temporal evolution of ARDS may influence subphenotype assignment, studies have shown that both ARDS phenotypes remain stable over 3 days [12]. Predictive enrichment has also been identified for both phenotypes in terms of differential treatment response to positive end-expiratory pressure strategies [7], fluid therapy [8], and simvastatin [10, 11].
These subphenotypes were derived in independent unsupervised examinations of clinical trial populations, including LCA of clinical and biomarker variables [13], and observational cohort studies with cluster analysis of biomarker data only. Researchers have shown that ARDS subphenotypes can be accurately identified with parsimonious classifier models using three (interleukin [IL]-8, bicarbonate, and protein C) or four variables (IL-8, bicarbonate, protein C, and vasopressin use), thereby facilitating the identification of ARDS phenotypes for use in clinical trials and practice [14].
In previous studies, the identification of ARDS phenotypes has been limited to patients enrolled in RCTs, so it is unclear whether these phenotypes can be generalized to the broader ARDS population. The identification of these phenotypes has been dependent on the quantification of study biomarkers, with plasma biomarkers being a key component of phenotype identification. To translate phenotypic findings into patient care, we need to be able to analyze and measure biomarkers in real time or in the field to classify patients into subphenotypes. There are currently no commercially available immediate or real-time quantifiable analyses of biomarkers. In this context, we wanted to test whether the use of clinical data (physiological and clinical variables) available at the bedside as class definition variables in the LPA model would lead to the identification of new potential classes.
Based on the results of randomized clinical trials, there are no specific drugs that have been shown to be effective in the treatment of ARDS. According to the pathological features of ARDS, glucocorticoids have generated considerable interest for their ability to reduce lung and systemic damage in patients with ARDS due to their potent anti-inflammatory and anti-fibrotic properties [15]. For example, it has been shown that long-term methylprednisolone administration in patients with refractory ARDS is associated with improved lung injury and multiple organ dysfunction scores and reduced mortality [16]. In another RCT, although methylprednisolone improved cardiopulmonary physiology, the results did not support its routine use in the treatment of persistent ARDS. Moreover, starting methylprednisolone therapy more than two weeks after the onset of ARDS may increase the risk of death. [17]. In addition, early administration of dexamethasone may reduce the duration of mechanical ventilation and overall mortality in patients with established moderate-to-severe ARDS [18]. In a recent meta-analysis of RCTs summarizing the use of corticosteroids in all examined patients with ARDS, it was shown that the use of corticosteroids may reduce mortality in these patients. This effect was consistent between patients with COVID-19 and non-COVID-19-related ARDS, corticosteroid type, and dose [19]. Different corticosteroid regimens have been tested in patients with ARDS but without conclusive results. Notably, given the lack of use of simvastatin drugs for different subtypes of ARDS in the HARP-2 study [10] and more recently in a COVID-19-related ARDS subgroup, subphenotypes had different therapeutic responses to corticosteroids [20]. We observed that trials testing corticosteroids did not use subphenotypes of non-COVID-19-associated ARDS. Thus, it remains to be determined whether glucocorticoids have different therapeutic responses and provide different survival benefits for different ARDS subphenotypes identified in the non-COVID-19 population.
We hypothesized that all patients with ARDS in the Medical Information Mart for Intensive Care (MIMIC)-IV database could be identified in two different patient classes with different clinical outcomes using their easily accessible bedside clinical data (physiological and clinical variables) as class-defining variables in the LPA model. Furthermore, in the two classes of ARDS identified, glucocorticoids may have different treatment responses, and their benefit may be more evident in one class.
Methods and materials
Data sources
This was a retrospective study in which data were obtained from a large intensive care database of multi-parameter intelligent monitoring, MIMIC-IV version 1.0 (https://physionet.org/content/mimiciv/1.0/). The MIMIC-IV database contains clinical information of patients in the Beth Israel Deaconess Medical Center (BIDMC) ICU between 2008 and 2019. The database has been approved by the Massachusetts Institute of Technology and BIDMC Institutional Review Board [21]. We were granted access to the database for data extraction following successful completion of the National Institutes of Health web-based training course and the Protecting Human Research Participants Examination (Fellowship No. 9,650,688, Record ID 39,539,950). Informed consent was not required as all health data were anonymous.
Study population
The total number of inpatients listed in the MIMIC-IV database from 2008 to 2019 was 523,740, and we selected patients with a diagnosis of ARDS for analysis by combining the diagnostic information recorded in the database with the Berlin criteria. Patient diagnoses were determined according to the International Classification of Diseases criteria (ICD-9-CM, ICD-10-CM) [22]. The following exclusion criteria were used: (1) patients with multiple repeat hospitalizations (only data from the first hospitalization were included); (2) patients aged < 18 years at the time of ICU admission; (3) ICU length of stay < 48 h; and (4) patients with massive data loss.
Data collection
We used the Navicat Premium 15 platform and Structured Query Language to extract identifiers (ID, ICU admission number), demographics (age, sex, height, weight), vital signs (temperature, heart rate, respiratory rate, blood pressure, SPO2, urine output), arterial blood gas parameters (lactate, PO2 PCO2, alveolar-arterial oxygen partial pressure difference, PaO2/FiO2 ratio, residual base, total CO2, anion gap, bicarbonate), invasive ventilation parameters (tidal volume, plateau pressure, PEEP, minute ventilation, oxygen concentration), laboratory parameters (white blood cells, hemoglobin, platelets, hematocrit, glucose, potassium, sodium, chloride, calcium, blood creatinine, blood urea nitrogen), and ARDS. The data on risk factors (such as pneumonia, sepsis, trauma, and malabsorption) were analyzed using vital signs, ventilator parameters, and laboratory parameters generated within 24 h of ICU admission. For some variables with multiple measurements within 24 h, maximum and minimum values were evaluated according to clinical characteristics (Additional file 1). Laboratory parameters such as albumin, CRP, and bilirubin were not included in the analysis due to excessive missing data. Medication use (including vasoactive drugs and glucocorticoids) was also extracted for the entire hospitalization, where vasoactive drugs included use 24 and 48 h before admission to the ICU and for the entire hospitalization, and glucocorticoids were used for the entire ICU admission, and the route of administration was intravenous.
The following outcome indicators were identified in this study: in-hospital mortality, days on ventilation, ventilator-free days, ICU length of stay, length of stay, and 28-day mortality.
Latent profile analysis (LPA)
LPA is similar to latent class analysis (LCA) in that it assumes that the data contain many unobserved groups or classes and determines group heterogeneity by mixture modelling to determine the best-fit model for a set of data [23]. When used to deal with continuous variables, it is called LPA. Potential class-based methods have been widely used in other disciplines, medicine, and related ARDS studies [7, 8, 10, 20].
Data on continuous physiological and clinical variables in demographics, vital signs, invasive respiratory parameters, blood gas analysis parameters, and laboratory parameters were assessed as class-defining variables for LPA, excluding all categorical variables. Partially similar demographics, vital signs, and laboratory parameters were used as defining variables, according to previous studies [7, 8, 10, 20]. Unlike previous studies, we also included variables not used in previous LCA studies, such as residual base, total CO2, and anion gap. All variables are easily available at the bedside. Among variables, urine volume was subjected to unit changes to reduce variance exceeding the upper limit of analytical detection, and highly correlated variables were excluded. The full set of class-defined variables used for LPA (31 continuous variables) is shown in Additional file 1. Clinical outcome variables and categorical variables were not included in the model.
To determine the optimal number of classes, we sequentially fitted class models from 1 to 5 using LPA and then performed these five model evaluations to determine the best class model. The model fit evaluation metrics were entropy, information metrics, and significance tests. The entropy value (Entropy) evaluates the classification accuracy and takes a value in the range of 0–1, with values closer to 1 indicating more accurate classification (0.8 indicates a classification accuracy of more than 90%). Information indicators included Akaike information criterion (AIC), Bayesian information criterion (BIC), and adjusted Bayesian information criterion (aBIC); the smaller the statistical value, the better the model fit. Significance tests including the likelihood ratio test (bootstrap-based; BLRT) and LMR were used to compare the difference in fit between k − 1 and k classes; a significant p-value indicated that the k-class model outperformed the k-1 class model. To estimate the model parameters, all continuous variables were zero-mean normalized, with all means normalized to 0 and standard deviations of 1. Once the optimal number of classes was determined using the metrics, each individual was assigned to the class to which they belonged according to the maximum posterior categorical probability. Correlations between classes and clinical outcomes were then tested using a method developed by Lanza [24] and stratified by class and glucocorticoid treatment modality, to determine if there was a differential treatment effect based on potential classes. The LPA process was performed using Mplus8.
Statistical analysis
For baseline characteristics, continuous variables are expressed as mean and standard deviation or median and interquartile range (IQR), depending on whether they were normally distributed; categorical variables are expressed as number and percentage. The t-test, chi-square test (χ2), Kruskal–Wallis test, and Wilcoxon rank-sum test were used for comparisons of baseline characteristics between classes, according to the nature of the variables.
The chi-square test for mortality (i.e., proportion of deaths) and the Wilcoxon rank-sum test for correlation between class assignment of ventilator-free days and clinical outcomes were used. To test for interactions between treatment and class assignment, we used logistic regression of mortality and performed post hoc subgroup analyses.
To assess the prognostic value of individual variables and to explore treatment interactions between different classes and glucocorticoid exposure, a logistic regression model was used to estimate the dominance ratio, with in-hospital mortality as the dependent variable. For 28-day mortality, Kaplan–Meier survival curves were plotted according to different strata.
Missing data were < 20% for all variables, and for variables with 5% < proportion missing < 20%, missing data were subjected to multiple interpolations using the chained equation (MICE) method [25]. The outlier values were replaced with the 99th and 1st percentiles. The percentage of missing data is described in detail in Additional file 1. Additional file 2 shows the distribution of each parameter before and after multiple interpolations of the missing data.
Data were collapsed and combined and statistically analyzed using Stata SE16 (StataCorp LLC, College Station, TX, USA) and IBM SPSS version 26.0 (IBM Corp., Armonk, NY, USA). P values < 0.05 were considered statistically significant.
Results
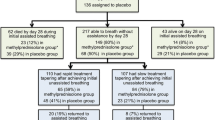
During the study period, 523,740 hospitalized patients were included in the MIMIC-IV database, and 1261 patients admitted to the ICU for the first time with ARDS were included based on diagnostic criteria. Of these, 157 patients were excluded from the study. Of these, 156 were excluded due to ICU stays of less than 48 h and 1 patient was excluded due to missing key respiratory parameters, resulting in the inclusion of 1104 patients in the cohort (see flow chart, Fig. 1).
Clinical characteristics
Of the 1104 patients (Table 1), the mean age was 63 (± 18) years, 603 patients (54.6%) were women, and most patients (63.0%) were non-Hispanic White. Regarding risk factors for ARDS, 319 patients with ARDS had pneumonia, 378 experienced trauma (including surgery), 247 had sepsis, 14 experienced aspiration, and 382 had other risk factors (including acute hypoxic respiratory failure, and pancreatitis). The median tidal volume of invasive breathing during patients’ stay in the ICU was 410 mL (345.5–482.5 mL), which may be related to the protective ventilation strategy adopted. Vasoactive drugs were required in 217 (19.7%) patients throughout the entire hospital stay and were administered to 119 (10.8%) patients within 24 h of ICU admission and 150 (13.6%) patients within 48 h. Glucocorticoids were administered to 172 (15.6%) patients. The median length of stay in the ICU was 9 days (IQR, 5–15), the median length of stay in the hospital was 15 days (IQR, 9–23), and the median days of ventilation were 3 (IQR, 1–6).
Potential profile analysis LPA
The 2-class potential class model provided the best model fit according to the potential profile analysis. We fitted potential class models from 2 to 5 classes. The summary information is presented in Table 2. All models had entropy values > 0.8, indicating > 90% accuracy in classification, and 2-class entropy values > 0.9, indicating > 95% accuracy in classification. Among the information metrics, the BIC decreases as the number of classes fitted increases, indicating that the model fits better as the number of classes increases. Similarly, the decrease in the AIC and aBIC also indicates that the model fits better as the number of classes increases. The 2-class model had the largest decrease in information metrics and outperformed the 1-class model whereas the significance test showed that LMR < 0.0001 and BLRT < 0.0001 for the 2-class model was significant. The 3-, 4-, and 5-class models had lower information metrics than the 2-class model, but the LMR of class 3 = 0.0730 and the class 5 LMR = 0.4354, both with P-value > 0.05. The LMR of the class 4 model = 0.0459, but the sample size of one class was too small, so the 2-class model was the best fit. In the 2-class model, 866 (78.4%) patients were assigned to class 1 and 238 (21.6%) were assigned to class 2. The mean class probability for the most likely class was 0.981 for class 1 and 0.957 for class 2 (see Additional file 3).
Baseline characteristics of each class
Patients were assigned to their two most likely classes based on posterior classification probabilities. For simplicity, we refer to these two classes as class 1 and class 2. There were 866 patients in class 1 and 238 patients in class 2 (Table 1). In the 2-class model, risk factors for ARDS (pneumonia, trauma, sepsis, and other, mainly acute hypoxic respiratory failure) were more common. In class 2, the proportion of pneumonia was higher. In class 1, the main risk factor was acute hypoxic respiratory failure, among others. The use of vasoactive drugs increased with hospitalization duration, from 24 to 48 h of ICU admission to the entire hospitalization period. The number of patients using vasoactive drugs was higher in class 2 compared with class 1 patients, with the proportion being > 30%, possibly indicating that class 2 patients were at greater risk of shock (Fig. 2). Among the 2-class of ARDS patients, the proportion of male patients was > 50% (53.46%; 58.82%), and the proportion of white patients in the race was > 50%. We standardized all continuous variables to a zero mean and arranged them in order of magnitude of the variable values in class 2 (Fig. 3). (Results normalized for original continuous variables were presented in the Additional file 4). Among all continuous class-defined variables, anion gap, lactate value, creatinine, residual base, bicarbonate, and total carbon dioxide differed more in class 2. In class 2, anion gap, lactate value, and creatinine were significantly higher than in class 1, whereas residual base, bicarbonate, and total carbon dioxide were significantly lower than in class 1, possibly indicating that patients in class 2 had more severe acidosis and poorer renal function than patients in class 1.
Two classes of vasoactive drug use(A) and ARDS-related risk factors at 24 h, 48 h, and throughout hospitalization in the ICU(B). Abbreviations: K = degrees of freedom; AIC = Akaike information criterion; BIC = Bayesian information criterion; aBIC = corrected Bayesian information criterion, the smaller the statistical value, the better the model fit. bLRT = likelihood ratio test (Bootstrap-based BLRT); LMR = Vuong-Lo-Mendell-Rubin test
Standardized values of continuous variables. The continuous classes used in the latent class model define the normalized values of the variables. For the highest values in class 2, variables are sorted from left to right in descending order. Standardized values were calculated by zero-meaning the mean of the variables to 0 and specifying the standard deviation as 1. AG, anion gap; Bun, urea nitrogen; PEEP, positive end-expiratory pressure; HR, heart rate; WBC, white blood cell count; RR, respiratory rate; and SBP, systolic blood pressure
Clinical outcomes in two potential classes
The clinical and biological characteristics of patients in class 2 were similar to the hyperinflammatory subphenotype in a previous study [7, 8, 10]. In that study, patients in class 2 had significantly higher in-hospital mortality and 28-day mortality compared with those in class 1 (27.3% vs. 13.9%, P < 0.001; 25.3% vs. 12.9%, P < 0.001). Patients in class 2 had significantly more days of ICU stay and overall length of stay than patients in class 1 (P < 0.0001). For ventilator-free days, patients in class 2 had longer days than patients in class 1 (P < 0.0001) (see Table 3). In logistic regression, by adjusting for covariates such as age, gender, corticosteroids, vasoactive drug use, SAPS II score and SOFA score, the mortality rate in class 2 was equivalent to approximately 1.31 times that of class 1 patients (odds ratio [OR] = 1.31; P = 0.038) (Table 4). Across the cohort, although associated with an increased risk of mortality, glucocorticoid use was statistically non-significant (P = 0.094). In addition, in both class Kaplan-Meier survival curves (Fig. 4A), class 2 patients had significantly lower 28-day survival than those in class 1 (P < 0.0001)
K-M survival curves, stratified by ARDS class and glucocorticoid treatment. Kaplan-Meier survival curves for patients with ARDS at 28 days, with class 2 patients having significantly lower survival than class 1 in panel A (P < 0.0001). panel B, stratified by ARDS class and treatment (glucocorticoid use versus no use). Curves were compared using the log-rank test. Overall p < 0.003; p < 0.0005 for class 2 patients treated with glucocorticoids versus not treated with glucocorticoids; p = 0.301 for hormone exposure in class 1 versus not
Treatment response of glucocorticoids between classes
In logistic regression stratified by ARDS class and glucocorticoids, class 1 OR = 1.20 indicated that the risk of death may be increased approximately 1.2-fold with glucocorticoids in class 1 (P = 0.496), with a non-significant P-value. Class 2 OR = 3.27 indicated that the risk of death with glucocorticoid use in class 2 may be increased approximately 3.27 times (P = 0.001). The final interaction test (P = 0.0381) indicated that for in-hospital mortality, the effect of glucocorticoids was significantly different between the two classes. Glucocorticoid exposure was associated with a trend toward increased mortality in ARDS class 2 and was not significantly associated with changes in mortality in class 1 (Table 5). We observed significant differences in survival curves among patients stratified by class and treatment (Fig. 4B; overall P < 0.003). Specifically, in patients in class 2, 28-day survival was significantly lower with glucocorticoid treatment than in patients without it (P < 0.0005). In class 1, no difference was observed for glucocorticoid treatment (P = 0.301).
As a sensitivity analysis to determine whether general severity of illness scores could supplant class identification, we tested for interactions between SAPS II score and corticosteroids. In contrast to the analyses using class, there were no significant interactions between SAPS II score and corticosteroids for the outcomes of mortality (p = 0.809 for interactions).
Discussion
This study aimed to verify whether using only clinical data (physiological and clinical variables) available at the bedside of patients with ARDS (excluding biomarkers) as a class definition variable could identify new potential classes. We identified two new potential classes of ARDS with different biological and clinical characteristics and clinical outcomes using clinical data as class definition variables for LPA. Patients with ARDS in class 2 had more severe acidosis, more vasoactive drug use, and worse clinical outcomes compared with those in class 1. There was a significant interaction between the two class pairs in our study and glucocorticoid therapy, with glucocorticoid use increasing mortality in class 2 in this study but not in class 1.
In this study, we performed LPA potential profiling in a larger sample size (n = 1104) of patients with ARDS than in previous studies [7, 8, 10, 20, 26]. In our study cohort, the informational metrics and VLMR and BLRT test P-values for the two classes strongly suggested that the 2-class model was the best fit in this study. Although the P-value of VLMR for the four classes = 0.0459, the 3-class model fit was not significant due to the two classes, which, together with the smaller size of the fourth class, led us to focus on the 2-class model. A possible reason for this is that the final decision on the optimal number of classes determined by the LPA model requires consideration of many different factors. Assuming that there are “X” potential classes in the data, the potential class model seeks to find the best model fit. If there are only two classes, but we fit a 3-class model, the third class will be forced in by selecting a few cases with more extreme or unique sets of values. A relatively small class provides very little information and may represent an anomaly rather than a useful finding.
We observed that the LPA class-defining variables with the largest contributions to potential classes included anion gap, base residual, lactate, bicarbonate, total carbon dioxide, and creatinine, with the contribution of bicarbonate having been reported in previous studies [7, 8, 10, 20]. These contributing clinical variables are extra-pulmonary variables that provide a greater correlation between circulatory and organ function in patients, and it can be briefly hypothesized that class 2 patients likely have poorer circulatory and organ function than class 1 patients. The possible explanation for the smaller contribution of lung-related indicators, such as respiratory parameters, to the identification of potential classes is that patients with ARDS who meet the diagnostic criteria of ARDS syndrome have less heterogeneity in the inverse of respiratory parameters.
With subsequent subgroup analysis of the two classes, we found heterogeneity in the effect of glucocorticoid therapy in both ARDS classes. Importantly for the subgroup analysis, first, we are a retrospective study, and glucocorticoid treatment was nonrandomized and could not be predetermined for planned subgroup analysis. We performed an unplanned exploratory subgroup analysis and a “robustness check”; the interaction of glucocorticoid treatment was significant across classes. Given the limitations of the study design, interpretation of the presented findings should be made with caution and limited to hypothesis generation. Second, although we noted that the proportion of glucocorticoid therapy was close in class 1 and class 2 (14% vs. 19%), we did not perform further subgroup analyses because the proportion of patients receiving each glucocorticoid was too small.
In the present study, the effect of glucocorticoid therapy reflected heterogeneity across different subclasses of ARDS. Of the three largest clinical trials testing the benefit of glucocorticoids in critically ill patients with COVID-19, the CoDEX randomized clinical trial (COVID-19 dexamethasone), the randomized clinical trial of hydrocortisone in critically ill patients with COVID-19, and the REMAP-CAP randomized clinical trial of COVID-19 corticosteroids, no significant reduction in absolute mortality was observed [27,28,29]. Notably, glucocorticoid treatment in all these studies had a signal of mortality benefit. It can be speculated that treating different subphenotypes may have different therapeutic effects, which requires prospective clinical trials. In addition, regarding dexamethasone in patients hospitalized with COVID-19, a preliminary report of a reduction in 28-day mortality with dexamethasone in patients randomized to invasive mechanical ventilation or oxygen alone, but not in patients not receiving respiratory support, suggests heterogeneity in terms of disease severity [30]. In patients with COVID-19-associated ARDS, glucocorticoid exposure was associated with reduced mortality in the high inflammatory phenotype and with increased mortality in the low inflammatory subphenotype [20]. Compared with previous studies, the effect of glucocorticoid treatment in our study differed across phenotypes. Our study population of patients with non-COVID-19-related ARDS had a broader range of risk factors for ARDS and greater heterogeneity. The potential classes identified by reducing heterogeneity may differ from the subphenotypes of COVID-19-related ARDS, so their glucocorticoid treatment effects differ across classes. Although no significant effect of glucocorticoid treatment was observed among patients with relatively mild illness in our study class 1, the sample size of this population was large, the signal-to-noise ratio was small, and glucocorticoid treatment likely had a harmful effect on this small group of people. This needs to be further evaluated in the future.
Our study found that patients using glucocorticoids had a lower probability of survival. The decision to use glucocorticoid may be influenced by factors such as comorbidity, disease severity, and prior treatment, which may also affect survival. To reduce indication bias, we excluded patients who may have used corticosteroids for comorbidities and also performed a sensitivity analysis, which found no significant interaction between disease severity SAPS II score and corticosteroids on the outcome of mortality. However, we acknowledge that there may be residual confounding that cannot be fully controlled in our study, which could be a potential limitation.
The present study has several strengths. First, most of the previous studies exploring ARDS heterogeneity have been based on a combination of clinical traits and biomarkers to distinguish their heterogeneity. Biomarkers are difficult in clinical practice because they are not available promptly or are difficult to obtain. We used clinical and physiological variables easily accessible at the patient’s bedside to perform LPA and obtained two different classes of ARDS. One study identified two ARDS subtypes using clinical variables [31], but we studied inconsistent methods so that the presence of ARDS subphenotypes could be verified from different perspectives. Second, we relied on the data-driven and unbiased nature of LPA for latent class identification without considering patient clinical outcome data. We included a large sample size, in comparison with previous studies, including ARDS patients with different risk factors. In addition, there has been controversy regarding the use of glucocorticoids in patients with ARDS in terms of whether glucocorticoids have different treatment effects in different classes. In this study, we further analyzed the two different classes of ARDS obtained. In patients with ARDS in class 1, glucocorticoid use was not statistically different for in-hospital mortality. In class 2 patients, glucocorticoid use increased patient mortality, which yields hypotheses for future studies.
This study also has some limitations. Although two classes were identified, we cannot guarantee that the addition of plasma biomarker variables (e.g., sRAGE, SP-D, ANG1/2, vWF, VEGF) and pathology-related variables will yield a different phenotype [5, 32,33,34,35] as the pathology of ARDS is also variable at autopsy. Hormone therapy was measured throughout the patient’s hospitalization, and we were unable to test for heterogeneous changes in the effect of hormone therapy in a given period. In addition, we were unable to obtain follow-up data on patients over time, and their long-term mortality is unknown. Finally, the low percentage of ARDS selected in the MIMIV-IV database is also one of the limitations of our study.
In conclusion, we identified two classes of non-COVID-19-associated ARDS using clinical and physiological variables with specifically different clinical and biological characteristics and clinical outcomes, with class 2 having a poorer clinical outcome. Differential treatment effects of glucocorticoids were observed in the different classes. Prospective clinical studies may be needed to verify the therapeutic heterogeneity of glucocorticoids in the different classes.
Availability of data and materials
The datasets generated and analyzed during the current study are not publicly available due to the need for licenses from MIT and Beth Israel Deaconess Medical Center (BIDMC) but are available from the author Qingbo Liao on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- RCT:
-
Randomized controlled trial
- ICU:
-
Intensive care unit
- LCA:
-
Latent class analysis
- IL:
-
Interleukin
- LPA:
-
Latent profile analysis
- MIMIC:
-
Mart for Intensive Care
- BIDMC:
-
Beth Israel Deaconess Medical Center
- PaO2 :
-
Pressure of oxygen
- FiO2 :
-
Fraction of inspired oxygen
- PEEP:
-
Positive end-expiratory pressure
- CRP:
-
C-reactive protein
- AIC:
-
Akaike information criterion
- BIC:
-
Bayesian information criterion
- K:
-
Degrees of freedom
- aBIC:
-
Adjusted Bayesian information criterion
- BLRT:
-
Likelihood ratio test (Bootstrap-based BLRT)
- LMR:
-
Vuong-Lo-Mendell-Rubin test
- IQR:
-
Interquartile range
- Aado2 :
-
Alveolar-arterial oxygen difference
- Be:
-
Residual base
- AG:
-
Aniongap
- Bun:
-
Urea nitrogen
- PEEP:
-
Positive end-expiratory pressure
- HR:
-
Heart rate
- WBC:
-
White blood cell count
- RR:
-
Respiratory rate
- SBP:
-
Systolic blood pressure
- OR:
-
Odds ratio
References
Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–8. https://doi.org/10.1056/nejm200005043421801.
Beitler JR, Sarge T, Banner-Goodspeed VM, Gong MN, Cook D, Novack V, Loring SH, Talmor D. Effect of titrating positive end-expiratory pressure (PEEP) with an esophageal pressure-guided strategy vs an empirical high PEEP-Fio2 strategy on death and days free from mechanical ventilation among patients with Acute Respiratory Distress Syndrome: a Randomized Clinical Trial. JAMA. 2019;321(9):846–57. https://doi.org/10.1001/jama.2019.0555.
Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, Lefrant JY, Prat G, Richecoeur J, Nieszkowska A, et al. Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA. 2008;299(6):646–55. https://doi.org/10.1001/jama.299.6.646.
Matthay MA, McAuley DF, Ware LB. Clinical trials in acute respiratory distress syndrome: challenges and opportunities. Lancet Respir Med. 2017;5(6):524–34. https://doi.org/10.1016/s2213-2600(17)30188-1.
Prescott HC, Calfee CS, Thompson BT, Angus DC, Liu VX. Toward smarter lumping and smarter splitting: rethinking strategies for Sepsis and Acute Respiratory Distress Syndrome Clinical Trial Design. Am J Respir Crit Care Med. 2016;194(2):147–55. https://doi.org/10.1164/rccm.201512-2544CP.
Shankar-Hari M, Fan E, Ferguson ND. Acute respiratory distress syndrome (ARDS) phenotyping. Intensive Care Med. 2019;45(4):516–9. https://doi.org/10.1007/s00134-018-5480-6.
Calfee CS, Delucchi K, Parsons PE, Thompson BT, Ware LB, Matthay MA. Subphenotypes in acute respiratory distress syndrome: latent class analysis of data from two randomised controlled trials. Lancet Respir Med. 2014;2(8):611–20. https://doi.org/10.1016/s2213-2600(14)70097-9.
Famous KR, Delucchi K, Ware LB, Kangelaris KN, Liu KD, Thompson BT, Calfee CS. Acute Respiratory Distress Syndrome Subphenotypes Respond differently to Randomized Fluid Management Strategy. Am J Respir Crit Care Med. 2017;195(3):331–8. https://doi.org/10.1164/rccm.201603-0645OC.
Bos LD, Schouten LR, van Vught LA, Wiewel MA, Ong DSY, Cremer O, Artigas A, Martin-Loeches I, Hoogendijk AJ, van der Poll T, et al. Identification and validation of distinct biological phenotypes in patients with acute respiratory distress syndrome by cluster analysis. Thorax. 2017;72(10):876–83. https://doi.org/10.1136/thoraxjnl-2016-209719.
Calfee CS, Delucchi KL, Sinha P, Matthay MA, Hackett J, Shankar-Hari M, McDowell C, Laffey JG, O’Kane CM, McAuley DF. Acute respiratory distress syndrome subphenotypes and differential response to simvastatin: secondary analysis of a randomised controlled trial. Lancet Respir Med. 2018;6(9):691–8. https://doi.org/10.1016/s2213-2600(18)30177-2.
Sinha P, Delucchi KL, Thompson BT, McAuley DF, Matthay MA, Calfee CS. Latent class analysis of ARDS subphenotypes: a secondary analysis of the statins for acutely injured lungs from sepsis (SAILS) study. Intensive Care Med. 2018;44(11):1859–69. https://doi.org/10.1007/s00134-018-5378-3.
Delucchi K, Famous KR, Ware LB, Parsons PE, Thompson BT, Calfee CS. Stability of ARDS subphenotypes over time in two randomised controlled trials. Thorax. 2018;73(5):439–45. https://doi.org/10.1136/thoraxjnl-2017-211090.
Zhou M, Thayer WM, Bridges JFP. Using latent class analysis to Model Preference heterogeneity in Health: a systematic review. PharmacoEconomics. 2018;36(2):175–87. https://doi.org/10.1007/s40273-017-0575-4.
Sinha P, Delucchi KL, McAuley DF, O’Kane CM, Matthay MA, Calfee CS. Development and validation of parsimonious algorithms to classify acute respiratory distress syndrome phenotypes: a secondary analysis of randomised controlled trials. Lancet Respir Med. 2020;8(3):247–57. https://doi.org/10.1016/s2213-2600(19)30369-8.
Rhen T, Cidlowski JA. Antiinflammatory action of glucocorticoids–new mechanisms for old drugs. N Engl J Med. 2005;353(16):1711–23. https://doi.org/10.1056/NEJMra050541.
Meduri GU, Headley AS, Golden E, Carson SJ, Umberger RA, Kelso T, Tolley EA. Effect of prolonged methylprednisolone therapy in unresolving acute respiratory distress syndrome: a randomized controlled trial. JAMA. 1998;280(2):159–65. https://doi.org/10.1001/jama.280.2.159.
Steinberg KP, Hudson LD, Goodman RB, Hough CL, Lanken PN, Hyzy R, Thompson BT, Ancukiewicz M. Efficacy and safety of corticosteroids for persistent acute respiratory distress syndrome. N Engl J Med. 2006;354(16):1671–84. https://doi.org/10.1056/NEJMoa051693.
Villar J, Ferrando C, Martínez D, Ambrós A, Muñoz T, Soler JA, Aguilar G, Alba F, González-Higueras E, Conesa LA, et al. Dexamethasone treatment for the acute respiratory distress syndrome: a multicentre, randomised controlled trial. Lancet Respir Med. 2020;8(3):267–76. https://doi.org/10.1016/s2213-2600(19)30417-5.
Chaudhuri D, Sasaki K, Karkar A, Sharif S, Lewis K, Mammen MJ, Alexander P, Ye Z, Lozano LEC, Munch MW, et al. Corticosteroids in COVID-19 and non-COVID-19 ARDS: a systematic review and meta-analysis. Intensive Care Med. 2021;47(5):521–37. https://doi.org/10.1007/s00134-021-06394-2.
Sinha P, Furfaro D, Cummings MJ, Abrams D, Delucchi K, Maddali MV, He J, Thompson A, Murn M, Fountain J, et al. Latent class analysis reveals COVID-19-related Acute Respiratory Distress Syndrome Subgroups with Differential responses to Corticosteroids. Am J Respir Crit Care Med. 2021;204(11):1274–85. https://doi.org/10.1164/rccm.202105-1302OC.
Johnson AE, Stone DJ, Celi LA, Pollard TJ. The MIMIC Code Repository: enabling reproducibility in critical care research. J Am Med Inform Assoc. 2018;25(1):32–9. https://doi.org/10.1093/jamia/ocx084.
Sottile PD, Kiser TH, Burnham EL, Ho PM, Allen RR, Vandivier RW, Moss M. An observational study of the efficacy of Cisatracurium compared with Vecuronium in patients with or at risk for Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med. 2018;197(7):897–904. https://doi.org/10.1164/rccm.201706-1132OC.
Rhoades STLBL. Latent Class Analysis: An Alternative Perspective on Subgroup Analysis in Prevention and Treatment. 2011.DOI
Lanza ST, Tan X, Bray BC. Latent class analysis with distal outcomes: a flexible model-based Approach. Struct Equ Modeling. 2013;20(1):1–26. https://doi.org/10.1080/10705511.2013.742377.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4(2):30DOI. https://doi.org/10.3978/j.issn.2305-5839.2015.12.63.
Sinha P, Calfee CS, Cherian S, Brealey D, Cutler S, King C, Killick C, Richards O, Cheema Y, Bailey C, et al. Prevalence of phenotypes of acute respiratory distress syndrome in critically ill patients with COVID-19: a prospective observational study. Lancet Respir Med. 2020;8(12):1209–18. https://doi.org/10.1016/s2213-2600(20)30366-0.
Angus DC, Derde L, Al-Beidh F, Annane D, Arabi Y, Beane A, van Bentum-Puijk W, Berry L, Bhimani Z, Bonten M, et al. Effect of hydrocortisone on mortality and organ support in patients with severe COVID-19: the REMAP-CAP COVID-19 corticosteroid domain Randomized Clinical Trial. JAMA. 2020;324(13):1317–29. https://doi.org/10.1001/jama.2020.17022.
Dequin PF, Heming N, Meziani F, Plantefève G, Voiriot G, Badié J, François B, Aubron C, Ricard JD, Ehrmann S, et al. Effect of hydrocortisone on 21-Day mortality or respiratory support among critically ill patients with COVID-19: a Randomized Clinical Trial. JAMA. 2020;324(13):1298–306. https://doi.org/10.1001/jama.2020.16761.
Tomazini BM, Maia IS, Cavalcanti AB, Berwanger O, Rosa RG, Veiga VC, Avezum A, Lopes RD, Bueno FR, Silva M, et al. Effect of dexamethasone on days alive and ventilator-free in patients with moderate or severe Acute Respiratory Distress Syndrome and COVID-19: the CoDEX Randomized Clinical Trial. JAMA. 2020;324(13):1307–16. https://doi.org/10.1001/jama.2020.17021.
Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, et al. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med. 2021;384(8):693–704. https://doi.org/10.1056/NEJMoa2021436.
Duggal A, Kast R, Van Ark E, Bulgarelli L, Siuba MT, Osborn J, Rey DA, Zampieri FG, Cavalcanti AB, Maia I, et al. Identification of acute respiratory distress syndrome subphenotypes de novo using routine clinical data: a retrospective analysis of ARDS clinical trials. BMJ Open. 2022;12(1):e053297. https://doi.org/10.1136/bmjopen-2021-053297.
Seymour CW, Gomez H, Chang CH, Clermont G, Kellum JA, Kennedy J, Yende S, Angus DC. Precision medicine for all? Challenges and opportunities for a precision medicine approach to critical illness. Crit Care. 2017;21(1):257. https://doi.org/10.1186/s13054-017-1836-5.
Sweeney TE, Khatri P. Generalizable biomarkers in critical care: toward Precision Medicine. Crit Care Med. 2017;45(6):934–9. https://doi.org/10.1097/ccm.0000000000002402.
Thille AW, Esteban A, Fernández-Segoviano P, Rodriguez JM, Aramburu JA, Peñuelas O, Cortés-Puch I, Cardinal-Fernández P, Lorente JA, Frutos-Vivar F. Comparison of the Berlin definition for acute respiratory distress syndrome with autopsy. Am J Respir Crit Care Med. 2013;187(7):761–7. https://doi.org/10.1164/rccm.201211-1981OC.
Thille AW, Esteban A, Fernández-Segoviano P, Rodriguez JM, Aramburu JA, Vargas-Errázuriz P, Martín-Pellicer A, Lorente JA, Frutos-Vivar F. Chronology of histological lesions in acute respiratory distress syndrome with diffuse alveolar damage: a prospective cohort study of clinical autopsies. Lancet Respir Med. 2013;1(5):395–401. https://doi.org/10.1016/s2213-2600(13)70053-5.
Acknowledgements
We would like to thank CJM for his help with this study.
Funding
This study was supported by the Gusu Talent Project of Suzhou Health Commission (GSWS2020065).
Author information
Authors and Affiliations
Contributions
All the authors contributed substantially to the work presented in this article. QD and QBL conceived the study. YFP and XEJ contributed to the data interpretation. QBL and XWX contributed to the study protocol and wrote the article. GQL, XQR, and ZWZ revised the article. The corresponding author had full access to all of the data and the final responsibility for the decision to submit this article for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with Good Clinical Practice (Declaration of Helsinki 2002). MIMIC-III was an anonymized public database. To apply for access to the database, we passed the Protecting Human Research Participants exam (Fellowship No. 9650688, Record ID 39539950). The project was approved by the institutional review boards of the Massachusetts Institute of Technology (MIT) and Beth Israel Deaconess Medical Center (BIDMC) and was given a waiver of informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liao, Q., Pu, Y., Jin, X. et al. Physiological and clinical variables identify ARDS classes and therapeutic heterogeneity to glucocorticoids: a retrospective study. BMC Pulm Med 23, 92 (2023). https://doi.org/10.1186/s12890-023-02384-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-023-02384-w