Abstract
Background
Immune checkpoint inhibitors (ICIs) have been shown to significantly improve the survival of patients with advanced lung adenocarcinoma (LUAD). However, only limited proportion of patients could benefit from ICIs. Novel biomarkers with strong predictability are needed for clinicians to maximize the efficacy of ICIs. Our study aimed to identify potential biomarkers predicting ICIs efficacy in LUAD.
Methods
The Cancer Genome Atlas (TCGA) PanCancer Atlas studies in cBioportal were used to evaluate the mutation frequency of ANK2 across multiple cancers. Clinical and mutational data for LUAD from ICIs-treated cohorts (Hellmann et al. and Rizvi et al.) were collected to explore the correlation between ANK2 mutation and clinical outcomes. In addition, the relationship between ANK2 expression and clinical outcomes was analyzed using LUAD data from TCGA and Gene Expression Omnibus. Furthermore, the impact of ANK2 mutation and expression on the tumor immune microenvironment of LUAD was analyzed using TCGA and TISIDB databases.
Results
Patients with ANK2 mutation benefited more from ICIs. In ICIs-treated cohort, prolonged progression-free survival (PFS) (median PFS: NR (not reached) vs. 5.42 months, HR (hazard ratio) 0.31, 95% CI 0.18–0.54; P = 0.0037), improved complete response rate (17.65% vs. 1.85%, P = 0.0402), and improved objective response rate (64.71% vs. 24.07%, P = 0.0033) were observed in LUAD patients with ANK2 mutation compared to their wild-type counterparts. Regarding ANK2 expression, it was observed that ANK2 expression was decreased in LUAD (P < 0.05) and a higher level of ANK2 expression was associated with longer overall survival (HR 0.69, 95% CI 0.52–0.92; P = 0.012) in TCGA LUAD cohort. Moreover, ANK2 mutation or higher ANK2 expression correlated with enhanced antitumor immunity and “hot” tumor microenvironment in LUAD, which could be potential mechanisms that ANK2 mutation facilitated ICIs therapy and patients with higher ANK2 expression survived longer.
Conclusion
Our findings suggest that ANK2 mutation or increased ANK2 expression may serve as a favorable biomarker for the efficacy of ICIs in patients with LUAD.
Similar content being viewed by others
Background
Lung cancer is the leading cause of cancer-related deaths [1], among which lung adenocarcinoma (LUAD) being the most prevalent subtype [2]. Given the fact that the majority of LUAD patients are diagnosed at an advanced stage, surgery is improbable and chemotherapy has historically been the primary treatment option [3]. However, the 5-year survival rate is less than 5% for advanced LUAD patients receiving chemotherapy [4]. Recently, the introduction of immune checkpoint inhibitors (ICIs) is a major breakthrough in LUAD treatment, which has improved the 5-year survival rate of advanced LUAD from less than 5% in the era of chemotherapy to approximately 30% currently for patients lacking sensitizing EGFR (epidermal growth factor receptor) or ALK (anaplastic lymphoma kinase) mutations [5]. Nevertheless, in most scenarios, only 20–40% of patients respond to ICI treatment and even fewer achieve long-term disease remission [6, 7], making the identification of biomarkers for patients likely to respond to ICIs therapy a critical step in identifying the candidate population.
Notably, PD-L1 expression on tumor cells or immune cells, as well as tumor mutation burden (TMB), can predict the therapeutic benefit of ICIs, with ICIs being more efficacious in prolonging the survival of patients with higher PD-L1 expression or higher TMB [8, 9]. Consequently, PD-L1 expression and TMB are approved as biomarkers in predicting efficiency of ICIs. However, certain limitations exist in these biomarkers. KEYNOTE-001 showed that the response rate to ICIs was 45.2% for those with PD-L1 expression ≥ 50% [10], whereas prolonged survival was also observed for patients with PD-L1 < 1% [11], suggesting that PD-L1 alone as a predicting biomarker would miss some responders and include some non-responders. In addition, inter-assay and intra-tumoral heterogeneity are identified, severely affecting the sensitivity and specificity of its predictability [12, 13]. TMB encounter similar concerns. Therefore, novel biomarkers with powerful predictability are urgently needed to optimize the treatment strategies of ICIs.
Unlike lung cancer of other histological types, advanced LUAD is characterized with higher prevalence of driver mutations, which determines the therapeutic strategy [14]. Representatively, targeted therapy is considered the first choice for patients with EGFR mutation or ALK mutation due to their superior performance [14]. Notwithstanding, gene mutations also have dramatic impacts on the efficacy of immunotherapy. Clinically, EGFR or ALK mutations are discovered to weaken the efficacy of immunotherapy [15, 16]. Likewise, patients harboring KEAP1 or STK11 mutations benefit less from immunotherapy compared to those with wild-type [17]. In contrast, LRP1B mutation [18], NOTCH4 mutation [19], ZFHX3 mutation [20], EPHA7 mutation [21], SETD2 mutation [22] and POLE/POLD1 mutation [23] were proven to be favorable biomarkers for ICIs treatment. Therefore, genetic mutations in LUAD play vital roles in regulating the sensitivity of ICIs treatment. Elucidating the relationship between key genetic mutations and ICIs efficacy will provide crucial evidence for distinguishing beneficiary patients.
Through analysis of the cBioportal database, we found that Ankyrin-B (ANK2) exhibited a higher mutation frequency in LUAD. The Ankyrins, belonging to the adapter protein family, consist of Ankyrin-R (ANK1), Ankyrin-B (ANK2), and Ankyrin-G (ANK3) [24]. Initially, ANK2 was considered as a key cytoskeletal-associated protein in the brain [25]. Besides, it was discovered as a pivotal adaptor and scaffolding protein in the heart [26]. Remarkably, recent studies have demonstrated that Ankyrins contribute to the modulation of various biological activities in cancers. Ying and his colleagues proved that ANK2 was overexpressed in pancreatic ductal adenocarcinoma and inhibition of ANK2 reduced invasion ability of pancreatic cancer cells [27]. Moreover, vital roles of Ankyrins have been observed in gastric cancer, breast cancer, and prostate cancer [28,29,30]. However, the impact of ANK2 (ANK2 mutation and expression) on the prognosis of LUAD patients, especially those treated with ICIs, is unknown.
In this study, the relationship between ANK2 mutation and ICIs efficacy in LUAD was analyzed through systematically collected and integrated clinical and genomic data from the cBioportal database (Hellmann et al. and Rizvi et al. cohorts). Besides, the prognostic value of ANK2 expression in LUAD was evaluated using the Cancer Genome Atlas (TCGA) database. Gene Expression Omnibus (GEO) datasets were used for further validation. Moreover, we analyzed the impact of ANK2 mutation or expression on immune-related signatures in tumor immune microenvironment (TIME) using TISIDB.
Materials and methods
Data collection
The flowchart of our study was showed in Fig. 1. A total of 10,967 samples from the TCGA PanCancer Atlas studies in cBioportal (https://www.cbioportal.org/) [31] were selected to evaluate the mutation frequency of ANK2 across multiple cancers. 12 LUAD studies in cBioportal totaling 4309 samples were used to perform survival analysis [31]. Moreover, the clinical and mutational data of ICIs-treated lung cancer cohort in cBioportal (Hellmann et al. and Rizvi et al.) [32, 33] were downloaded in order to investigate the effect of ANK2 mutation on ICIs efficacy for LUAD patients. Samples with histology adenocarcinoma were included. After excluding 17 squamous samples, 74 LUAD samples were eventually included as the ICIs-treated cohort. LUAD harboring ANK2 nonsynonymous somatic mutations was defined as ANK2-mutant (ANK2-MT), otherwise, it was defined as ANK2 wild type (ANK2-WT). Furthermore, RNA-seq and clinical data of LUAD were downloaded from TCGA (www.tcga-data.nci.nih.gov/tcga) to explore the influence of ANK2 expression on the survival of LUAD patients [34].
ANK2 mutation and outcomes of LUAD receiving ICIs
ICIs-treated cohort was used to analyze the relationship between ANK2 mutation and progression-free survival (PFS) in LUAD patients, as well as the response to ICIs treatment. The response to ICIs was evaluated according to the Response Evaluation Criteria in Solid Tumors (RECIST) 1.1. Durable clinical benefit (DCB) was defined as complete response (CR), partial response (PR) or stable disease (SD) lasting over six months. All other patients were considered to have no durable benefit (NDB). The objective response rate (ORR) was defined as the percentage of patients with CR or PR. Besides, we investigated the association between ANK2 mutation and multiple existing biomarkers for ICIs, including TMB, predicted neoantigen burden (PNB), and PD-L1 expression levels, using ICIs-treated cohort. TMB was defined as the number of nonsynonymous alterations (SNVs or indels) per patient. PD-L1 expression levels on tumor cells or infiltrating immune cells of < 1%, 1–49%, ≥ 50%, were considered negative, weak, and strong, respectively. Moreover, co-mutations of ANK2 with other genes, such as DNA damage repair (DDR)-related genes and mismatch repair (MMR)-related genes, etc., were calculated with 12 LUAD studies from cBioportal.
ANK2 expression in LUAD
The CPTAC pan cancer samples in UALCAN database (http://ualcan.path.uab.edu/) were used to explore ANK2 expression levels across various cancers [35]. Then, the downloaded LUAD data from TCGA were employed to compare ANK2 expression between LUAD and healthy tissues.
RNA extraction and quantitative-PCR (q-PCR)
Q-PCR was further performed to validate the difference in ANK2 expression between LUAD and healthy tissues. In detail, total RNA was isolated from healthy lung epithelial cell line (BEAS-2B) and lung adenocarcinoma cell lines (PC9, H1975, A549 and HCC827) using Trizol reagent and cDNA was synthesized according to the manufacturer’s protocol (Accurate Biology, China). Next, q-PCR was performed using SYBR® Green Premix Pro Taq HS qPCR kit (Accurate Biology, China). The mRNA levels were normalized to that of β-actin based on the threshold cycle of each sample. Primer sequences were as follows:
ANK2 forward primer: CGCTAGGAAAGACGACACCA,
ANK2 reverse primer: CCACTCTCAGTTGTCCTATTCAC,
β-actin forward primer: GAAGAGCTACGAGCTGCCTGA,
β-actin reverse primer: CAGACAGCACTGTGTTGGCG.
Survival analyses based on ANK2 expression in LUAD patients
Based on median ANK2 expression, TCGA LUAD samples were divided into two groups, high ANK2 expression group and low ANK2 expression group. Next, the Kaplan–Meier survival curves were depicted utilizing the survival package [36]. Ten LUAD cohorts (GSE11969, GSE13213, GSE26939, GSE29013, GSE30219, GSE31210, GSE37745, GSE42127, GSE50081, GSE72094) from GEO were utilized to validate the relationship between ANK2 expression and patient survival. Moreover, the relationship between ANK2 expression and clinicopathological parameters (including tumor stage, tumor grade, and various pathway alterations) in LUAD was investigated through UALCAN database (http://ualcan.path.uab.edu/) [35].
Correlation analysis of immune characteristics
The infiltration levels of 22 tumor-infiltrating lymphocyte subsets between ANK2-MT and ANK2-WT were evaluated using LUAD data from TCGA by CIBERSORT algorithm (https://cibersort.stanford.edu/) [37]. Single-sample GSEA (ssGSEA) with the “GSVA” R package was employed to quantify the infiltration scores of 15 immune cells between the low- and high-ANK2 expression group using TCGA LUAD data [38, 39]. TIMER database was used to further validate the correlation between ANK2 (ANK2 expression or ANK2 mutation) and immune infiltrating cells [40]. The impact of ANK2 copy number variation (CNV) on immune cell infiltration of LUAD was explored by TIMER as well [40]. Further, we evaluated the association between ANK2 expression and gene markers of various immune cells in LUAD using TIMER [40]. The gene markers of immune cells were determined through R&D Systems (www.rndsystems.com/cn/resources/cell-markers/immune-cells). The association of ANK2 with varying immune characteristics (immuno-stimulators, immuno-inhibitors, major histocompatibility complex (MHC) molecules, chemokines, and their receptors) in LUAD was evaluated using TISIDB (http://cis.hku.hk/TISIDB/index.php) [41], an integrated repository portal for tumor-immune system interactions.
Statistical analyses
The Kaplan–Meier method was applied to depict survival curves, and log-rank test was applied to evaluate P values. ANK2 expression between LUAD and healthy tissues was compared utilizing Mann–Whitney U test. The q-PCR results were analyzed by One-way ANOVA test. The association between ANK2 mutation and clinicopathological parameters (such as PD-L1, CR, PR, SD, PD, ORR, DCB) was analyzed through Pearson chi-squared test or Fisher’s exact test. The relationship between ANK2 mutation and TMB or PNB was analyzed by Mann–Whitney U test. All analyses in our study were conducted through R software (version 3.6.3), GraphPad Prism (version 9.0), Stata (version 16) or online databases (TIMER, UALCAN, TISIDB, cBioportal). Statistical difference was considered when P < 0.05.
Results
ANK2 mutation frequency and its correlation with survival of patients with LUAD
Using the cBioportal database, we first evaluated the ANK2 mutation frequency across multiple cancers. As shown in Fig. 2A, LUAD ranked second among all cancers, with a mutation frequency of 19.61%, followed by stomach adenocarcinoma and endometrial carcinoma. The distribution of various ANK2 mutation subtypes in LUAD was depicted in Fig. 2B, among which G1252V/R was the most prevalent. To investigate the influence of ANK2 mutation on LUAD patient survival, 12 studies from cBioportal with a total of 4309 LUAD patients, mainly receiving surgery and chemotherapy, were subjected to survival analysis. The results showed that the median overall survival (OS) (66.64 vs. 54.00 months, HR 0.99, 95% CI 0.76–1.29) (Fig. 2C), median PFS (35.84 vs. 36.13 months, HR 0.91, 95% CI 0.65–1.28) (Fig. 2D), and median disease-specific survival (DSS) (66.64 vs. 88.14 months, HR 0.92, 95%CI 0.58–1.46) (Fig. 2E) were comparable between LUAD patients with ANK2-MT and ANK2-WT (all P > 0.05).
ANK2 mutation frequency across cancers and survival analysis of LUAD based on ANK2 mutation status. A: The prevalence of ANK2 mutation across 30 types of cancers. B: Lollipop plot shows the distribution of ANK2 mutation in LUAD. C: Overall survival (OS) analysis stratified by ANK2 mutation status in LUAD from cBioportal. D: Progress-free survival (PFS) analysis stratified by ANK2 mutation status in LUAD from cBioportal. E: Disease-specific survival (DSS) analysis stratified by ANK2 mutation status in LUAD from cBioportal
Association of ANK2 mutation with survival of LUAD patients treated with ICIs
To further investigate the impact of ANK2 mutation on ICIs efficacy in LUAD patients, a ICIs-treated cohort (Hellmann et al. and Rizvi et al.) from the cBioportal database was analyzed. The clinical characteristics of patients were summarized in Table 1. ANK2 mutated higher in LUAD patients with age ≥ 65 years than age < 65 years (P = 0.028), while ANK2 mutation frequency was comparable for males and females or smokers and non-smokers (all P > 0.05). Survival analysis revealed that PFS was significantly prolonged in patients with ANK2-MT than those with ANK2-WT (median PFS: NR vs. 5.42 months, HR 0.31, 95% CI 0.18–0.54, P = 0.0037) (Fig. 3A). Meanwhile, LUAD patients harboring ANK2-MT had significantly higher CR (17.65% vs. 1.85%, P = 0.0402), ORR (64.71% vs. 24.07%, P = 0.0033), and DCB (70.59% vs. 38.60%, P = 0.0272) (Fig. 3B, C) compared to their WT counterparts. In addition, tumor immunogenicity between ANK2-MT and ANK2-WT LUAD were compared. Higher TMB and PNB were observed in ANK2-MT LUAD (all P < 0.01) (Fig. 3D, E). The proportion of PD-L1-strong patients was higher in ANK2-MT LUAD than in ANK2-WT LUAD (21.1% vs. 17.6%) (Additional file 1: Fig. S1A). Notably, MMR-related genes (MLH1, PMS2) and DDR-related genes (BARD1, BRCA1, BRCA2, BRIP1, and RAD50) mutated more frequently in the ANK2-MT than in the ANK2-WT (all P < 0.05) (Fig. 3F, G). Furthermore, the frequency of co-mutations with ANK2 was analyzed. Multiple genes positively associated with ICIs efficacy, including LRP1B, KRAS, EPHA7, NOTCH4, and POLD1, had significantly higher mutational frequencies in ANK2-MT LUAD than in ANK2-WT LUAD (all P < 0.05) (Additional file 1: Fig. S1B). Conversely, lower frequency of EGFR mutation was observed in ANK2-MT LUAD (P < 0.05) (Additional file 1: Fig. S1C). The detailed mutation frequencies for each gene were summarized in Additional file 1: Table S1.
Association of ANK2 mutation with clinical outcomes in ICIs-treated LUAD cohort. A: Kaplan–Meier survival curves comparing PFS between the ANK2-MT and ANK2-WT LUAD in ICIs-treated cohort. B: Comparison of the proportion of patients with complete response (CR), partial response (PR), stable disease (SD) and progression disease (PD) between ANK2-MT and ANK2-WT LUAD in ICIs-treated cohort. C: Comparison of the proportion of patients with durable clinical benefit (DCB) or no durable benefit (NDB) between ANK2-MT and ANK2-WT LUAD in ICIs-treated cohort. D: Comparison of the TMB between ANK2-MT and ANK2-WT LUAD in ICIs-treated cohort. E: Comparison of the PNB between ANK2-MT and ANK2-WT LUAD in ICIs-treated cohort. F: The landscape of co-mutation between ANK2 and MMR pathway-related genes in LUAD. G: The landscape of co-mutation between ANK2 and DDR pathway-related genes in LUAD (NR, not reached; *P < 0.05, **P < 0.01, ****P < 0.0001)
Correlation between ANK2 mutation and TIME in LUAD
Given the growing evidence on the pivotal role of TIME in ICIs efficacy, the correlation between ANK2 mutation and TIME in LUAD was investigated. The ANK2-MT LUAD was characterized by higher immune cell infiltration, including CD8+ T cells (P = 0.021), activated memory CD4+ T cells (P = 0.001), and M1 macrophages (P = 0.016) (Fig. 4A). TIMER database was used for further verification and similar results were obtained (Additional file 1: Fig. S2). Additionally, multiple “immuno-stimulator” genes were found to be much more abundant in the ANK2-MT LUAD than in the ANK2-WT LUAD, including IL2RA, KLRC1, KLRK1, MICB, TNFRSF18, TNFRSF25, TNFRSF4 and ULBP1 (all P < 0.05) (Fig. 4B). Furthermore, CD274, which encodes PD-L1 and is a predictive biomarker for increased ICIs efficacy, was higher in LUAD with ANK2-MT than with ANK2-WT (P < 0.05) (Fig. 4C). Several other immune checkpoints, including CTLA4, LAG3, PDCD1, TGFB1, and TIGIT, were upregulated in ANK2-MT LUAD as well (P < 0.05) (Fig. 4C). As shown in Fig. 4D, MHC molecules, particularly TAP2, were upregulated in ANK2-MT LUAD (P < 0.05). Besides, most chemokines (such as CXCL9, CXCL10, CXCL11 and XCL1) were more abundant in ANK2-MT LUAD, while CCL15 and CXCL3 expression was increased in ANK2-WT LUAD (all P < 0.05) (Fig. 4E). In terms of chemokine receptors, CCR10 and CXCR3 was upregulated in ANK2-MT LUAD; while CCR3 and CX3CR1, on the other hand, were downregulated (all P < 0.05) (Fig. 4F).
Association of ANK2 mutation with immune-related signatures in LUAD. A: Differences in immune cell infiltration between ANK2-MT and ANK2-WT LUAD. B, C: Differences in immuno-stimulators (B) and immuno-inhibitors (C) between ANK2-MT and ANK2-WT LUAD. D: Correlation of ANK2 mutation with the expression levels of MHC molecules in LUAD. E, F: The effect of ANK2 mutation on the expression of chemokines (E) and their receptors (F) in LUAD (*P < 0.05, **P < 0.01, ***P < 0.001)
Association of ANK2 expression with clinical features and survival of LUAD patients
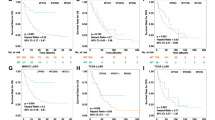
Firstly, ANK2 expression was compared between tumor tissues and healthy tissues. As shown in Fig. 5A, the CPTAC database revealed that ANK2 expression was lower compared to healthy tissues across multiple cancers, including lung cancer. Likewise, compared with healthy tissue, LUAD expressed lower ANK2 expression in TCGA database (P < 0.001) (Fig. 5B, C). For further verification, q-PCR was performed. ANK2 expression was significantly lower in lung adenocarcinoma cell lines (PC9, H1975, A549 and HCC827, all P < 0.05) than in healthy lung epithelial cell line (BEAS-2B) (Fig. 5D). Secondly, correlation between ANK2 expression and multiple clinical characteristics was analyzed using TCGA data. It was observed that higher ANK2 expression at mRNA level correlated with earlier T-stage, earlier N-stage, earlier pathological stage, and fewer dead events (all P < 0.05) (Table 2). CPTAC database further validated that higher ANK2 expression at protein level was associated with earlier pathological stage (P < 0.05) (Fig. 6A) and lower histological grade (P < 0.01) (Fig. 6B). Moreover, we found that ANK2 expression was decreased in LUAD harboring SWI-SNF complex alteration, P53/Rb-related pathway alteration, MYC alteration, WNT pathway alteration, and HIPPO pathway alteration (all P < 0.05) (Fig. 6C–G), all of which have been shown to play important roles in tumorigenesis. Next, survival analyses were conducted to investigate the prognostic value of ANK2 expression in LUAD. Notably, patients with higher ANK2 expression experienced longer OS (P = 0.012, HR = 0.69, 95% CI 0.52–0.92) (Fig. 6H) and longer DSS (P = 0.045, HR = 0.69, 95% CI 0.47–0.99) (Fig. 6I). The meta-analysis of ten GEO LUAD cohorts showed a pooled HR of 0.65 (0.55–0.78) between high ANK2 expression and OS (Fig. 6J), further confirming the protective role of ANK2 in LUAD. The ROC curve demonstrated that the diagnosticity of ANK2 was excellent with an AUC of 0.758 (Fig. 6K).
Comparison of ANK2 expression in healthy tissue versus tumor tissue. A: ANK2 expression levels in pan-cancer were measured using UALCA database. B: Comparison of ANK2 expression between LUAD and non-paired healthy tissues in TCGA. C: Comparison of ANK2 expression between LUAD and paired healthy tissues in TCGA. D: Comparison of ANK2 expression between healthy lung epithelial cell line (BEAS-2B) and LUAD cell lines (PC9, H1975, A549, and HCC827) (*P < 0.05, ***P < 0.001)
Association of ANK2 expression with clinical features and survival of LUAD patients A: Pathological stage. B: Histological grade. C: SWI-SNF complex alteration. D: P53/Rb-related pathway alteration. E: MYC/MYCN alteration. F: WNT pathway alteration. G: HIPPO pathway alteration. H: Kaplan–Meier curves for OS of patients in the high- and low-ANK2 expression LUAD. I: Kaplan–Meier curves for DSS of patients in the high- and low-ANK2 expression LUAD. J: Meta-analysis was performed to integrate HR values about ANK2 expression and OS from ten GEO LUAD cohorts. K: Diagnostic ROC curve analysis of ANK2 in LUAD (*P < 0.05, **P < 0.01, ***P < 0.001)
Correlation between ANK2 expression and TIME in LUAD
The correlation between ANK2 expression and immune cell infiltration was further explored. The results showed that increased ANK2 expression correlated with increased infiltration of a variety of immune cells, including T cells, CD8+ T cells, cytotoxic T cells, B cells, DC, aDC, iDC, pDC, NK cells, neutrophils, mast cells, macrophages, eosinophils, Tregs, and T helper cells (all P < 0.05) (Fig. 7A). Using the TIMER database, positive correlations were further established between ANK2 expression and infiltration of immune cells (CD4+ T cells, CD8+ T cells, B cells, macrophages, DC, and neutrophils) (Additional file 1: Fig. S3A). Meanwhile, significant positive correlations were identified between ANK2 expression and molecular biomarkers of multiple immune cells, including T cells, CD8+ T cells, Tfh, NK cells, and dendritic cells (all P < 0.05) (Table 3). Notably, ANK2 copy number was correlated with immune cell infiltration as well, with a higher level of immune cell infiltration in ANK2 arm-level gain LUAD compared to ANK2 arm-level deletion LUAD (Additional file 1: Fig. S3B). Moreover, LUAD with high ANK2 expression was more abundant in C2 (IFN-gamma dominant) and C3 (inflammatory) immune subtypes (P < 0.001) (Additional file 1: Fig. S3C).
Association between ANK2 expression and immune-related signatures in LUAD A: Differences in immune cell infiltration between high- and low-ANK2 expression LUAD. B, C: Association of ANK2 expression with immuno-stimulators (B) and immuno-inhibitors (C) in LUAD. D: Correlation of ANK2 expression with MHC molecules expression in LUAD. E, F: Correlation of ANK2 expression with the expression of chemokines (E) and their receptors (F) in LUAD (*P < 0.05, **P < 0.01, ***P < 0.001)
Immuno-stimulators, immuno-inhibitors, MHC molecules, chemokine and their receptors are essential components for immune response. Therefore, the association of these signatures with ANK2 expression was evaluated. Most of the immuno-stimulators, immune checkpoint molecules and MHC molecules were positively correlated with ANK2 expression (most P < 0.05) (Fig. 7B–D). In terms of chemokines and their receptors, significantly positive correlations with ANK2 expression were detected (most P < 0.05) (Fig. 7E, F). Taken together, these results suggested that high ANK2 expression was associated with immunologically “hot” tumor microenvironment and enhanced anti-tumor immunity.
Discussion
ICIs treatment has revolutionized the treatment of lung cancer including LUAD, but disappointingly only a subset of patients responds to ICIs. Identifying novel biomarkers are imperative. In this study, we revealed that ANK2 was a predictive biomarker for ICIs efficacy in LUAD patients, with individuals harboring ANK2 mutation experiencing longer PFS. Moreover, high ANK2 expression correlated with prolonged survival for LUAD patients. Importantly, ANK2 mutation or high ANK2 expression was associated with the development of enhanced anti-tumor immunity.
The gene mutation status in LUAD guides the therapeutic decision-making, with targeted therapy being the first choice for patients harboring EGFR or ALK mutations [14]. Of note, a growing number of studies demonstrate that certain gene mutations have profound impacts on the efficacy of immunotherapy [15,16,17]. In our study, ANK2 mutation was first identified to be associated with longer PFS and higher response rates for patients receiving ICIs, indicating a favorable effect of ANK2 mutation on immunotherapy. LUAD patients with EGFR mutation rarely benefit from ICIs [42], which could be attributed to the immune-inert phenotype of EGFR mutated LUAD [43]. In contrast, ANK2-MT LUAD exhibited higher levels of TMB and PD-L1 expression, providing stronger evidence that ANK2 mutation support a better survival benefit from ICIs for LUAD patients. In clinical practice, precisely identifying the dominant benefiting population from ICIs is essential but challenging. ANK2, with a high mutation frequency in LUAD, could be a promising biomarker given the increased efficacy for ICIs.
An activated cancer-immunity cycle is indispensable for the success of ICIs [44, 45], with antigen release being the critical first step [44]. In our study, high PNB were observed in the ANK2-MT LUAD, indicating that the ANK2-MT LUAD had heightened tumor immunogenicity [46]. In addition, higher mutation frequencies of MMR-related genes, DDR-related genes and POLD1 were found in ANK2-MT LUAD, which were reported to be positively correlated with increased immunogenicity [47,48,49]. Therefore, ANK2 mutation might enhance the immunogenicity of LUAD, hence boosting the cancer-immunity cycle. Presenting tumor antigens to T cells is the second step of cancer-immunity cycle [44, 50] and our results revealed that in ANK2-MT LUAD, DCs and MHC molecules, two key participants in antigen-presenting [51, 52], were elevated. The third step of the cancer immunity cycle is the trafficking of activated effector T cells into TIME, which guarantees their anti-tumor immunity [44]. ANK2-MT LUAD was characterized by high expression of chemokines (CXCL9, CXCL10, CXCL11, and CXCR3) involved in the recruitment of anti-cancer immune cells [53]. Consequently, ANK2-MT LUAD exhibited a TIME characterized by increased anti-tumor immune cells.
Concerning ANK2 expression, it has been found to be downregulated in breast cancer and colon adenocarcinoma [30, 54], which was consistent with the findings of our pan-cancer analysis. In terms of lung cancer, ANK2 has not been studied and we proved that ANK2 was downregulated in LUAD. As we all know, the type of TIME plays an important role in the elimination of cancer cells [55, 56], with “hot” TIME facilitating cancer cell killing. According to our findings, ANK2 expression was strongly associated with multiple immune cell infiltration, promoting the formation of "hot" TIME. Moreover, positive correlations were observed between ANK2 expression and immune-related signatures (MHC molecules, immuno-stimulators, immuno-inhibitors, chemokines and their receptors), with the majority of these profiles enhancing antitumor TIME [55, 57, 58]. These findings suggested that LUAD patients with high ANK2 expression had improved antitumor immunity and enhanced "hot" TIME, which provided explanations for a better prognosis of these patients. Thus, it could be speculated that ANK2 agonists are likely to promote antitumor immunity and thus increase the efficacy of immunotherapy. Given the similar impact of ANK2 mutation and high ANK2 expression on TIME of LUAD, we conjectured that ANK2 mutation might alter ANK2 expression, however, statistical analysis revealed no correlation between ANK2 mutation and ANK2 expression (Additional file 1: Fig. S4).
Although we have systematically and comprehensively explored the predictive and prognostic roles of ANK2 in LUAD, some non-negligible limitations exist in our study. Firstly, the limited sample size and the absence of OS data for ICIs-treated cohort could bias the role of ANK2 mutation in LUAD patients receiving immunotherapy. Secondly, the potential role of ANK2 in TIME was analyzed based on the LUAD samples from public databases where clinical characteristics of patients were likely to be highly heterogeneous, which could influence the reliability of the findings. Further validation utilizing in vitro experiments and in vivo animal models is required. Thirdly, there is a lack of direct evidence on the relationship between ANK2 expression and prognosis of patients with LUAD treated with ICIs. Notwithstanding, our study provided comprehensively predictive and prognostic evidence concerning ANK2 in LUAD for the first time, particularly the favorable significance of ANK2 mutation in LUAD patients treated with ICIs, paving the way for future molecular studies on the role of ANK2 in LUAD.
Conclusion
Our study was the first to propose that ANK2 mutation correlated with prolonged PFS and enhanced response for LUAD patients receiving ICIs therapy. LUAD patients with higher ANK2 expression experienced more favorable outcomes. In conclusion, it was demonstrated that ANK2 (ANK2 mutation or high ANK2 expression) was potentially favorable biomarker for LUAD prognosis. Moreover, ANK2 (ANK2 mutation or high ANK2 expression) is related to strengthened tumor immunogenicity and inflamed antitumor immunity, which could be the underlying mechanism for the function of ANK2 in LUAD.
Availability of data and materials
This study was conducted based on publicly available databases, including TCGA (https://portal.gdc.cancer.gov/repository?facetTab=cases), GEO (https://www.ncbi.nlm.nih.gov/geo/), TIMER (https://cistrome.shinyapps.io/timer/), UALCAN (http://ualcan.path.uab.edu/), TISIDB (http://cis.hku.hk/TISIDB/index.php) and cBioportal (https://www.cbioportal.org/). The detailed databases used in the study were described in the method section.
Abbreviations
- ANK2:
-
Ankyrin-2
- ANK2-MT:
-
ANK2-mutant
- ANK2-WT:
-
ANK2 wild type
- ALK:
-
Anaplastic lymphoma kinase
- CR:
-
Complete response
- CTLA-4:
-
Cytotoxic T lymphocyte-associated antigen 4
- DCB:
-
Durable clinical benefit
- DDR:
-
DNA damage repair
- DFS:
-
Disease free survival
- DSS:
-
Disease specific survival
- EGFR:
-
Epidermal growth factor receptor
- GEO:
-
Gene Expression Omnibus
- ICIs:
-
Immune checkpoint inhibitors
- LUAD:
-
Lung adenocarcinoma
- MHC:
-
Major histocompatibility complex
- MMR:
-
Mismatch repair
- NDB:
-
No durable benefit
- NSCLC:
-
Non-small cell lung cancer
- ORR:
-
Objective response rate
- OS:
-
Overall survival
- PD:
-
Progressive disease
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed cell death protein ligand 1
- PFS:
-
Progression free survival
- PNB:
-
Predicted neoantigen burden
- PR:
-
Partial response
- q-PCR:
-
Quantitative polymerase chain reaction
- SD:
-
Stable disease
- ssGSEA:
-
Single-sample gene set enrichment analysis
- TCGA:
-
The Cancer Genome Atlas
- TCR:
-
T cell receptor
- TIME:
-
Tumor immune microenvironment
- TMB:
-
Tumor mutation burden
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Thai AA, Solomon BJ, Sequist LV, Gainor JF, Heist RS. Lung cancer. Lancet. 2021;398(10299):535–54.
Leighl NB. Treatment paradigms for patients with metastatic non-small-cell lung cancer: first-, second-, and third-line. Curr Oncol. 2012;19(Suppl 1):S52-58.
Noone A, Howlader N, Krapcho M, Miller D, Brest A, Yu M, et al. SEER cancer statistics review, 1975–2015. 2018.
Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, et al. Five-year outcomes with pembrolizumab versus chemotherapy for metastatic non-small-cell lung cancer with PD-L1 tumor proportion score≥ 50. J Clin Oncol. 2021;39(21):2339–49.
Miller M, Hanna N. Advances in systemic therapy for non-small cell lung cancer. BMJ. 2021;375:n2363.
Herbst RS, Giaccone G, de Marinis F, Reinmuth N, Vergnenegre A, Barrios CH, et al. Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N Engl J Med. 2020;383(14):1328–39.
Sha D, Jin Z, Budczies J, Kluck K, Stenzinger A, Sinicrope FA. Tumor mutational burden as a predictive biomarker in solid tumors. Cancer Discov. 2020;10(12):1808–25.
Cristescu R, Mogg R, Ayers M, Albright A, Murphy E, Yearley J, et al. Pan-tumor genomic biomarkers for PD-1 checkpoint blockade-based immunotherapy. Science. 2018. https://doi.org/10.1126/science.aar3593.
Garon EB, Rizvi NA, Hui R, Leighl N, Balmanoukian AS, Eder JP, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med. 2015;372(21):2018–28.
Socinski MA, Jotte RM, Cappuzzo F, Orlandi F, Stroyakovskiy D, Nogami N, et al. Atezolizumab for first-line treatment of metastatic nonsquamous NSCLC. N Engl J Med. 2018;378(24):2288–301.
Haragan A, Field JK, Davies MPA, Escriu C, Gruver A, Gosney JR. Heterogeneity of PD-L1 expression in non-small cell lung cancer: Implications for specimen sampling in predicting treatment response. Lung Cancer. 2019;134:79–84.
Doroshow DB, Bhalla S, Beasley MB, Sholl LM, Kerr KM, Gnjatic S, et al. PD-L1 as a biomarker of response to immune-checkpoint inhibitors. Nat Rev Clin Oncol. 2021;18(6):345–62.
Tan AC, Tan DSW. Targeted therapies for lung cancer patients with oncogenic driver molecular alterations. J Clin Oncol. 2022;40(6):611–25.
Lee CK, Man J, Lord S, Links M, Gebski V, Mok T, et al. Checkpoint inhibitors in metastatic EGFR-mutated non-small cell lung cancer-a meta-analysis. J Thorac Oncol. 2017;12(2):403–7.
Seegobin K, Majeed U, Wiest N, Manochakian R, Lou Y, Zhao Y. Immunotherapy in non-small cell lung cancer with actionable mutations other than EGFR. Front Oncol. 2021;11:750657.
Shang X, Li Z, Sun J, Zhao C, Lin J, Wang H. Survival analysis for non-squamous NSCLC patients harbored STK11 or KEAP1 mutation receiving atezolizumab. Lung Cancer. 2021;154:105–12.
Chen H, Chong W, Wu Q, Yao Y, Mao M, Wang X. Association of LRP1B mutation with tumor mutation burden and outcomes in melanoma and non-small cell lung cancer patients treated with immune check-point blockades. Front Immunol. 2019;10:1113.
Long J, Wang D, Yang X, Wang A, Lin Y, Zheng M, et al. Identification of NOTCH4 mutation as a response biomarker for immune checkpoint inhibitor therapy. BMC Med. 2021;19(1):154.
Zhang J, Zhou N, Lin A, Luo P, Chen X, Deng H, et al. ZFHX3 mutation as a protective biomarker for immune checkpoint blockade in non-small cell lung cancer. Cancer Immunol Immunother. 2021;70(1):137–51.
Zhang Z, Wu HX, Lin WH, Wang ZX, Yang LP, Zeng ZL, et al. EPHA7 mutation as a predictive biomarker for immune checkpoint inhibitors in multiple cancers. BMC Med. 2021;19(1):26.
Lu M, Zhao B, Liu M, Wu L, Li Y, Zhai Y, et al. Pan-cancer analysis of SETD2 mutation and its association with the efficacy of immunotherapy. NPJ Precis Oncol. 2021;5(1):51.
Wang F, Zhao Q, Wang YN, Jin Y, He MM, Liu ZX, et al. Evaluation of POLE and POLD1 mutations as biomarkers for immunotherapy outcomes across multiple cancer types. JAMA Oncol. 2019;5(10):1504–6.
Koenig SN, Mohler PJ. The evolving role of ankyrin-B in cardiovascular disease. Heart Rhythm. 2017;14(12):1884–9.
Davis JQ, Bennett V. Brain Ankyrin. A membrane-associated protein with binding sites for spectrin, tubulin, and the cytoplasmic domain of the erythrocyte anion channel. J Biol Chem. 1984;259(21):13550–9.
Sucharski HC, Dudley EK, Keith CBR, El Refaey M, Koenig SN, Mohler PJ. Mechanisms and alterations of cardiac ion channels leading to disease: role of Ankyrin-B in cardiac function. Biomolecules. 2020. https://doi.org/10.3390/biom10020211.
Chen Y, Lohr M, Jesnowski R. Inhibition of ankyrin-B expression reduces growth and invasion of human pancreatic ductal adenocarcinoma. Pancreatology. 2010;10(5):586–96.
Wang T, Abou-Ouf H, Hegazy SA, Alshalalfa M, Stoletov K, Lewis J, et al. Ankyrin G expression is associated with androgen receptor stability, invasiveness, and lethal outcome in prostate cancer patients. J Mol Med (Berl). 2016;94(12):1411–22.
Cao W, Wei W, Zhan Z, Xie D, Xie Y, Xiao Q. Regulation of drug resistance and metastasis of gastric cancer cells via the microRNA647-ANK2 axis. Int J Mol Med. 2018;41(4):1958–66.
Schabort JJ, Nam AR, Lee KH, Kim SW, Lee JE, Cho JY. ANK2 Hypermethylation in canine mammary tumors and human breast cancer. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21228697.
Cerami E, Gao J, Dogrusoz U, Gross BE, Sumer SO, Aksoy BA, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–4.
Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science. 2015;348(6230):124–8.
Hellmann MD, Nathanson T, Rizvi H, Creelan BC, Sanchez-Vega F, Ahuja A, et al. Genomic features of response to combination immunotherapy in patients with advanced non-small-cell lung cancer. Cancer Cell. 2018;33(5):843-852.e844.
Tomczak K, Czerwinska P, Wiznerowicz M. The cancer genome atlas (TCGA): an immeasurable source of knowledge. Contemp Oncol (Pozn). 2015;19(1A):A68-77.
Chandrashekar DS, Bashel B, Balasubramanya SAH, Creighton CJ, Ponce-Rodriguez I, Chakravarthi B, et al. UALCAN: a portal for facilitating tumor subgroup gene expression and survival analyses. Neoplasia. 2017;19(8):649–58.
Liu J, Lichtenberg T, Hoadley KA, Poisson LM, Lazar AJ, Cherniack AD, et al. An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell. 2018;173(2):400-416.e411.
Newman AM, Liu CL, Green MR, Gentles AJ, Feng W, Xu Y, et al. Robust enumeration of cell subsets from tissue expression profiles. Nat Methods. 2015;12(5):453–7.
Hanzelmann S, Castelo R, Guinney JGSVA. gene set variation analysis for microarray and RNA-seq data. BMC Bioinform. 2013;14:7.
Bindea G, Mlecnik B, Tosolini M, Kirilovsky A, Waldner M, Obenauf AC, et al. Spatiotemporal dynamics of intratumoral immune cells reveal the immune landscape in human cancer. Immunity. 2013;39(4):782–95.
Li T, Fan J, Wang B, Traugh N, Chen Q, Liu JS, et al. TIMER: a web server for comprehensive analysis of tumor-infiltrating immune cells. Cancer Res. 2017;77(21):e108–10.
Ru B, Wong CN, Tong Y, Zhong JY, Zhong SSW, Wu WC, et al. TISIDB: an integrated repository portal for tumor-immune system interactions. Bioinformatics. 2019;35(20):4200–2.
Qiao M, Jiang T, Liu X, Mao S, Zhou F, Li X, et al. Immune checkpoint inhibitors in EGFR-mutated NSCLC: Dusk or dawn? J Thorac Oncol. 2021;16(8):1267–88.
Le X, Negrao MV, Reuben A, Federico L, Diao L, McGrail D, et al. Characterization of the immune landscape of EGFR-mutant NSCLC identifies CD73/adenosine pathway as a potential therapeutic target. J Thorac Oncol. 2021;16(4):583–600.
Chen DS, Mellman I. Oncology meets immunology: the cancer-immunity cycle. Immunity. 2013;39(1):1–10.
Kim JM, Chen DS. Immune escape to PD-L1/PD-1 blockade: seven steps to success (or failure). Ann Oncol. 2016;27(8):1492–504.
Graham LS, Pritchard CC, Schweizer MT. Hypermutation, mismatch repair deficiency, and defining predictors of response to checkpoint blockade. Clin Cancer Res. 2021;27(24):6662–5.
Bateman AC. DNA mismatch repair proteins: scientific update and practical guide. J Clin Pathol. 2021;74(4):264–8.
Wang Z, Zhao J, Wang G, Zhang F, Zhang Z, Zhang F, et al. Comutations in DNA damage response pathways serve as potential biomarkers for immune checkpoint blockade. Cancer Res. 2018;78(22):6486–96.
Chen YX, Wang ZX, Yuan SQ, Jiang TJ, Huang YS, Xu RH, et al. POLE/POLD1 mutation in non-exonuclease domain matters for predicting efficacy of immune-checkpoint-inhibitor therapy. Clin Transl Med. 2021;11(9): e524.
Jhunjhunwala S, Hammer C, Delamarre L. Antigen presentation in cancer: insights into tumour immunogenicity and immune evasion. Nat Rev Cancer. 2021;21(5):298–312.
Wculek SK, Cueto FJ, Mujal AM, Melero I, Krummel MF, Sancho D. Dendritic cells in cancer immunology and immunotherapy. Nat Rev Immunol. 2020;20(1):7–24.
Garcia-Lora A, Algarra I, Garrido F. MHC class I antigens, immune surveillance, and tumor immune escape. J Cell Physiol. 2003;195(3):346–55.
Matsuo K, Yoshie O, Nakayama T. Multifaceted roles of chemokines and chemokine receptors in tumor immunity. Cancers (Basel). 2021. https://doi.org/10.3390/cancers13236132.
Liao C, Huang X, Gong Y, Lin Q. Discovery of core genes in colorectal cancer by weighted gene co-expression network analysis. Oncol Lett. 2019;18(3):3137–49.
Chen DS, Mellman I. Elements of cancer immunity and the cancer-immune set point. Nature. 2017;541(7637):321–30.
Binnewies M, Roberts EW, Kersten K, Chan V, Fearon DF, Merad M, et al. Understanding the tumor immune microenvironment (TIME) for effective therapy. Nat Med. 2018;24(5):541–50.
Matsuo K, Yoshie O, Nakayama T. Multifaceted roles of chemokines and chemokine receptors in tumor immunity. Cancers (Basel). 2021;13(23):6132.
Laha D, Grant R, Mishra P, Nilubol N. The role of tumor necrosis factor in manipulating the immunological response of tumor microenvironment. Front Immunol. 2021;12:656908.
Acknowledgements
Not applicable.
Funding
This study was funded by grants from the National Natural Science Foundation of China (No. 81874044) and the Shandong Provincial Natural Science Foundation (No. ZR2020MH236 and No. ZR2019MH050).
Author information
Authors and Affiliations
Contributions
YG-L and XW-W designed and supervised the study. WG-Z, XL-S, NL and XC-M performed analysis and drafted the manuscript. RY, HD-X, YQ-Z, and QZ collected and assembled the data, collected the literature, edited figures, and checked the manuscript. XW-W and YG-L revised the manuscript. All authors contributed to the article and approved the final version. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1
. Figure S1 Relationship between ANK2 mutation and clinical features in LUAD. A: ANK2 mutation was associated with enhanced PD-L1 expression in LUAD. B: Frequency of gene mutations with positive effects on immunotherapy in ANK2-MT and ANK2-WT LUAD. C: Frequency of gene mutations with negative effects on immunotherapy in ANK2-MT and ANK2-WT LUAD (*P < 0.05). Figure S2 Comparison of immune infiltration between ANK2-MT and ANK2-WT LUAD from TIMER database (*P < 0.05). Figure S3 Association of ANK2 expression with immune infiltration in LUAD. A: Correlation of ANK2 expression with immune infiltration in LUAD patients from TIMER database. B: ANK2 copy number variation affects the infiltrating levels of CD8+ T cell, CD4+ T cell, B cell, dendritic cell, macrophages, and neutrophils in LUAD. C: ANK2 expression in different immune subtypes in LUAD via TISIDB (*P < 0.05, **P < 0.01, ***P < 0.001). Figure S4 Relationship between ANK2 mutation and ANK2 expression in LUAD.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, W., Shang, X., Liu, N. et al. ANK2 as a novel predictive biomarker for immune checkpoint inhibitors and its correlation with antitumor immunity in lung adenocarcinoma. BMC Pulm Med 22, 483 (2022). https://doi.org/10.1186/s12890-022-02279-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-02279-2