Abstract
Objectives
To compare overall survival (OS) and cancer-specific survival (CSS) outcomes of surgery with radiotherapy in octogenarians with stage Ia non-small cell lung cancer (NSCLC).
Materials and methods
Patients aged ≥ 80 years with clinical stage Ia (T1N0M0) NSCLC between 2012 and 2017 were identified from the population-based Surveillance, Epidemiology, and End Results (SEER) database. Patients were assigned into surgery and radiotherapy groups. Multivariate Cox regression analysis was used to identify survival-associated factors. Treatment groups were adjusted by propensity score matching (PSM) analysis while OS and CSS outcomes were compared among groups by Kaplan–Meier analysis.
Results
A total of 1641 patients were identified, with 46.0% in the surgical group and 54.0% in the radiotherapy group. Compared to surgery, radiotherapy-treated patients were older, later diagnosed, had more often unmarried, more squamous cell carcinoma, more unknown grade and increased tumor sizes. Radiotherapy was associated with a significantly worse OS, compared to surgery (hazard ratio 2.426; 95% CI 2.003–2.939; P < .001). After PSM, OS (P < 0.001) and CSS (P < 0.001) were higher in the surgery group. The 1-, 3-, and 5-year OS rates of surgical and radiotherapy group were 90.0%, 76.9%, 59.9%, and 86.0%, 54.3%, 28.0%, respectively. The 1-, 3-, and 5-year CSS rates of surgical and radiotherapy group were 94.5%, 86.1%, 78.0% and 90.7%, 74.5%, 61.0%, respectively. There were no survival differences between the matched surgery without lymph node examination (LNE) and radiotherapy group, as well as between the matched surgery and radiotherapy who were recommended but refused surgery group.
Conclusions
In octogenarians with stage Ia NSCLC, surgery with lymph node dissection offers better OS and CSS outcomes than radiotherapy.
Similar content being viewed by others
Introduction
Lung cancer is a serious health issue (11.6% of total cancer cases) and the leading cause of cancer-associated death (18.4% of total cancer deaths) [1]. The prevalence of early-stage non-small cell lung cancer (NSCLC) has been projected to increase in the elderly, with the lung cancer screening recommendations and aging of the general population. Elderly individuals are often associated with multiple comorbidities, poor cardiopulmonary functions, frailty, and higher operative risks, which complicates lung cancer treatment [2]. Therefore, it is important to determine the best treatment strategies for octogenarians with early stage NSCLC.
Optimal treatment options for octogenarians and older patients with early-stage NSCLC have not been established. Surgery combined with lymph node dissection is the standard treatment option for early-stage NSCLC [3]. However, due to comorbidities, surgery is often precluded in elderly patients aged ≥ 80 years. Radiotherapy (RT), especially stereotactic ablative radiotherapy (SABR), is the first-line recommendation for inoperable early-stage NSCLC [3]. Over the last decade, SABR has gained an increasing popularity, particularly among older patients. In the United States and European countries, RT has replaced surgery as the most commonly used treatment modality for early-stage NSCLC in patients aged ≥ 80 years [4,5,6]. However, whether radiotherapy or surgery has a better impact on the treatment for such patients remains unclear. It is difficult to perform randomized clinical trials in octogenarians. In this study, the SEER database was used to compare survival differences between octogenarians and older patients receiving surgery versus those receiving radiotherapy as the sole treatment for stage Ia NSCLC.
Materials and methods
Data sources
The SEER database was analyzed via SEER Stat (version 8.3.9; http://www.seer.cancer.gov) in March 2022 with the identifier 15362-Nov2020. SEER 18 Regs Research Plus Data (with additional treatment fields) was chosen to select patients. Its’ follow-up ended by December 31, 2018. This study was conducted in accordance with the Declaration of Helsinki (as revised in Tokyo 2004). Given the retrospective nature of this study anonymization of patient data, patient consent and Institutional Review Board approval were waived.
Study population
Patients aged ≥ 80 years with histologically diagnosed primary NSCLC in the early stage and treated with surgery or radiation alone from January 2012 to December 2017 were included. Early stage was defined as clinical T1N0M0 (T ≤ 3 cm), classified as stage Ia according to the 8th Edition of the American Joint Committee on Cancer (AJCC) Staging Manual. Patients who had multiple cancers or a second diagnosis of lung cancer, diagnosed by autopsy/death certificate, without sufficient survival data and receiving chemotherapy were excluded.
The following information were obtained for each patient in the SEER database: patient ID, age at diagnosis, sex, race, marital status (unmarried status included widowed, single, divorced and separated), year of diagnosis, anatomical tumor location, size, tumor histology, grade, type of treatment, number of regional lymph node examined (LNE) in patients who underwent surgery, reasons for no cancer-directed surgery in patients who underwent radiotherapy, RX Summ–Surg/Rad Seq and cause of death. Types of treatment categories were: (1) surgery alone, (2) radiotherapy alone. Preoperative or postoperative use of radiotherapy were excluded.
Statistical analysis
Statistical Analysis were performed using SPSS 26.0 (IBM Corp, Armonk, NY). Patients were assigned into surgery or radiotherapy groups. Survival time was measured from the time of diagnosis to the time of death or last follow-up. The χ2 test or Students’t test was used to compare demographic and clinical characteristics while the influence of patient’s characteristics and treatment on OS outcomes were evaluated by Cox regression analysis. Multivariate Cox regression analysis was performed with factors identified as significant in univariate analysis (p < 0.05). Propensity score–matched (PSM) analysis was performed based on factors significant in Cox regression analysis for OS. The t-test and χ2 test were used to assess the success of propensity score matching. The OS and CSS outcomes before and after PSM were analyzed by Kaplan–Meier (KM) analyses, and evaluated by log-rank test. All tests were 2-sided, with p ≤ 0.05 being the threshold for significant differences.
Results
Patient characteristics
A total of 1641 patients with stage Ia NSCLC were included in this study (755 (46%) subjected to surgery and 886 (54%) subjected to radiotherapy). Figure 1 illustrates the flow diagram for patient selection. The mean age of the entire cohort was 83 ± 2.9 years, while the median follow-up time was 42 months. Baseline demographics and clinical characteristics for surgical and radiotherapy groups are presented in Table 1. Most patients who underwent surgery received either lobectomy (63.4%) or wedge resection (27.5%). Regional LNE was performed in 611 (80.9%) patients in the surgery cohort. Of the 886 patients who received radiotherapy, reasons for no cancer-directed surgery in 808 patients (91.2%) were “not recommended”, while in only 78 (8.8%) patients the reasons were “recommended but not performed, patient refused”. Compared to surgery, patients treated with radiotherapy were older, later diagnosed, and had more often unmarried, more squamous cell carcinoma, more unknown grade and increased tumor sizes.
Survival analysis
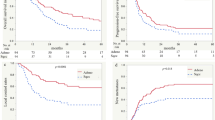
Unadjusted Kaplan–Meier survival curves for unmatched groups are shown in Fig. 2. The median OS time for the entire cohort was 56.0 months (95% CI 51.7–60.3 months). The OS and CSS outcomes of the surgical group were significantly higher than those of the radiotherapy group (both p < 0.001). The median OS time was 41.0 months (95% CI, 36.7–45.3 months) in the radiotherapy group while not reached in the surgery group. The 1-, 3-, and 5-year OS rates were 91.4%, 78.6%, and 63.6% in the surgery group, 87.2%, 54.4%, and 30.4% in the radiotherapy group, respectively. The 1-, 3-, and 5-year CSS rates were 95.9%, 89.4%, and 81.4% in the surgery group, and 92.9%, 74.8%, and 62.6% in the radiotherapy group, respectively.
Univariate and multivariate analysis for OS predictors are shown in Table 2. In univariate analysis, age at diagnosis, sex, years of diagnosis, tumor sizes, histology, grades, and treatment patterns were significantly associated with survival outcomes. In multivariate Cox regression analysis, patients who underwent radiotherapy had significantly worse survival outcomes, compared to patients who had surgery (hazard ratio 2.426; 95% CI 2.003–2.939; p < 0.001). Younger age, female sex, later year of diagnosis, histology of adenocarcinoma, well or moderate differentiation, and smaller tumor sizes were independent prognostic factors for better OS.
Propensity score matching(PSM) based on age, sex, race, year of diagnosis, tumor size, histology, and pathologic grade resulted in 372 patients in both surgery and radiotherapy groups (1:1 ratio). The demographics and clinical variables were well balanced as shown in Tables 3. After PSM, the OS (P < 0.001) and CSS (P < 0.001) of the surgery group were still higher than that of the radiotherapy group. Median survival time were 79.0 and 41.0 months in the surgery and radiotherapy groups, respectively. The 1-, 3-, and 5-year OS rates were 90.0%, 76.9%, and 59.9% in the surgery group, and 86.0%, 54.3%, and 28.0% in the radiotherapy group. The 1-, 3-, and 5-year CSS rates were 94.5%, 86.1%, and 78.0% in surgery group, and 90.7%, 74.5%, and 61.0% in radiotherapy group, respectively (Fig. 3).
Survival outcomes were compared between matched subgroups of surgery without LNE versus radiotherapy. The demographics and clinical variables were well matched after propensity score matching (Additional file 1: eTable 1). Kaplan–Meier survival curves for the matched groups are displayed in Fig. 4. No differences in the OS (P = 0.146) and CSS (P = 0.675) were found between the surgery without LNE and radiotherapy group.
Survival outcomes were also compared between matched patients of those who subjected to surgery versus those subjected to radiotherapy who were recommended to surgery but refused. The demographics and clinical variables were well matched after propensity score matching (Additional file 1: eTable 2). Kaplan–Meier survival curves for the matched groups are displayed in Fig. 5. No differences in the OS (P = 0.104) and CSS (P = 0.414) were found between the two groups.
Discussion
The present study showed that compared with surgery, octogenarians treated with radiotherapy were older, later diagnosed, and had more often unmarried, more squamous cell carcinoma, unknown grade and increased tumor size. Younger age, female sex, later year of diagnosis, adenocarcinoma histology, well or moderately differentiation, smaller tumor size and receiving surgery were independent prognostic factors for better OS. Surgery with regional LNE offers better survival than radiotherapy in octogenarians with clinical stage Ia NSCLC after PSM. The 1-, 3-, and 5-year OS rates of surgery and radiotherapy group were 90.0%, 76.9%, 59.9%, and 86.0%, 54.3%, 28.0%, respectively. The 1-, 3-, and 5-year CSS rates of surgery and radiotherapy group were 94.5%, 86.1%, 78.0% and 90.7%, 74.5%, 61.0%, respectively.
The results of our study are consistent with those of most studies and meta-analyses comparing the clinical outcomes of surgery versus radiotherapy in elderly or non-elderly patients [7,8,9,10]. However, these studies span a long time, from 1998 to 2018, during which techniques of radiotherapy and surgery developed rapidly, and the results may not be able to guide current medical decisions. We selected the cases in the last 10 years (2012–2017) to eliminate the influence of unbalanced development of technology in radiotherapy and surgery, so that the results can better guide the current clinical decision. We advocate that although the popularity of radiotherapy in elderly patients and the great progress in radiotherapy in the last 10 years, surgery should still be the first choice for patients with stage Ia NSCLC, in view of the better OS and CSS, even for the elderly over 80 years old. As the conclusion of a single-center study [11], age is no reason to deny patients surgery for early-stage lung cancer. Studies [12] have also found that quality of life among octogenarians after surgery remains similar to younger patients even after anatomical lung resection. Though there is still controversy about which operation procedure is the best. Most patients in the surgery group in our study received either lobectomy (63.4%) or wedge resection (27.5%). Chan et al. [13] believes that lobectomy provided better 5-year survival compared with sublobar resection regardless of the age in octogenarians with pathologic stage I lung cancer. Yet the JACS1303 study [14] showed that wedge resection might be equivalent to lobectomy or segmentectomy in selected octogenarians or older with early-stage NSCLC who can tolerate lobectomy. Study from Mimae et al. [15] showed that the influence of wedge resection on death due to other causes was lower than that of lobectomy or segmentectomy in patients with NSCLC aged ≥ 80 years. We speculate that a multidisciplinary team discussion on performance status, cardio-pulmonary function, and so on, may be helpful to choose the surgical procedure.
It is worth mentioning that there were no survival advantages when surgery without LNE compared to matched radiotherapy in the subgroup analysis. An analysis of the National Cancer Database (NCDB) also showed no survival differences between the lobectomy with 0 LN and SABR among healthy patients with clinical stage I NSCLC [16]. We speculate that the patients with stage Ia in surgery with LNE group was “net stage Ia”, while the stage Ia in radiotherapy and surgery without LNE group were not, and patients with lymph node metastasis might be included in these group. There are two inspirations from these results. First, for the surgeons, it is crucial to choose appropriate patient who can tolerate the surgery and perform regional LNE to ensure better survival benefits; Secondly, the disadvantage of radiotherapy compared to surgery is the impossibility of regional lymph node dissection, which may leave out occult lymph node metastasis and affect the overall prognosis [17]. Larger tumors are known to be associated with higher rates of occult nodal involvement [18, 19]. In order to reduce the influence of occult lymph node metastasis as much as possible, patients with a tumor size more than 3 cm were excluded in our study. However, the rate of occult lymph node involvement was 12.9% even in less than 3 cm NSCLC [19]. For radiologists, it is important to perform accurate clinical staging before radiotherapy. Conventional imaging examination such as enhanced computed tomography (CT) or 18F-fluorodeoxyglucose positron emission tomography (PET-CT) [20,21,22] may not be able to judge the nature of lymph nodes accurately. Use of endobronchial ultrasound bronchoscopy (EBUS) with hilar and mediastinal nodal fine-needle aspiration sampling may provide more information on lymph node staging [23, 24]. Recently, the revised STARS study, in which pathological nodal sampling using EBUS was performed in > 90% patients, showed that the 3-year OS rate of SABR and surgical group (video-assisted thoracoscopic surgical lobectomy with mediastinal lymph node dissection, VATS L-MLND) was 91%, the 5-year OS rate in SABR group was 87%, and 84% in surgical group. Long-term survival after SABR was non-inferior to VATS L-MLND for operable stage Ia NSCLC [25]. One may be able to expect better survival outcomes of radiotherapy in early stage NSCLC by accurate lymph node staging.
The findings of this study should not be interpreted as a comparative analysis of surgery and radiotherapy yet, since it may magnify the survival difference between radiotherapy and surgery. Although the outcomes were significantly lower in patients undergoing radiotherapy, these patients were vast majority (91.2%) nonsurgical candidates, that is, these patients were generally with poor physical status, and might have a shorter life expectancy. Bei et al. [26] demonstrated that pretreatment physical state was significantly associated with OS in patients > 80 years old with early-stage NSCLC receiving SABR. Watanabe et al. also revealed that inoperability was the predictors of poor overall survival after SABR in elderly patients [27]. Although we performed PSM to adjust the two groups as much as possible, the lack of data about patient’s performance status and comorbid conditions in SEER database makes it impossible to match completely. This was confirmed by further comparison of outcomes between matched patients of surgery versus radiotherapy who were recommended to surgery but refused. There were no survival advantages when surgery compared to radiotherapy in matched operable stage Ia patients. It is also worth mentioning that not all radiotherapy in SEER database were SABR. As we know, there were significant survival differences between conventional fractionated radiotherapy and SABR [28, 29], which may be one of the reasons for the survival advantages of surgery to radiotherapy in our study. At present, SABR has become the standard radiotherapy modality for inoperable early lung cancer. The revised STARS study selected operable Ia NSCLC and showed that survival of SABR was non-inferior than that of VATS L-MLND [25]. A propensity score‑matching analysis from Tomita et al., in which performance status, forced expiratory volume and Charlson comorbidity index between groups were all matched, also demonstrated that survivals were not significantly different between surgery and SBRT in patients with c-stage I NSCLC [30]. One may infer that survival difference between surgery and radiotherapy may not be as great as in our study among operable patients or patients with good performance status. Therefore, larger RCT studies are required to further clarify which is better for octogenarians with early stage NSCLC. Studies such as STABLE-MATES trial [31] are already under way, and we look forward to the results.
There are several limitations in this study. First, given the retrospective nature of the data collection from the SEER database, inherent selection bias was inevitable. Second, prognostic factors of NSCLC, such as the performance status, comorbid conditions and specific details regarding radiotherapy regimens were not provided by the SEER database. Although propensity score matching analysis was performed, biases cannot be excluded. Prospective trials are required to confirm the findings reported here.
In summary, our study demonstrates that surgery with lymph node dissection is associated with better OS and CSS than radiotherapy in octogenarians and older with stage Ia NSCLC. Our results should be interpreted with caution given the limitations discussed above. More research is needed to determine which is better for stage Ia NSCLC in patients who are operable or have good performance status and patients with accurate lymph node staging.
Availability of data and materials
All data in this paper are from SEER database. All data discussed in the manuscript are included within this published article. This data can be found here: https://seer.cancer.gov/.com
Abbreviations
- OS:
-
Overall survival
- CSS:
-
Cancer-specific survival
- NSCLC:
-
Non-small cell lung cancer
- SEER:
-
Surveillance, Epidemiology, and End Results database
- PSM:
-
Propensity score‑matching
- LNE:
-
Lymph node examination
- RT:
-
Radiotherapy
- SABR:
-
Stereotactic ablative radiotherapy
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49. https://doi.org/10.3322/caac.21660.
Clérigo V, Hasmucrai D, Teixeira E, Alves P, Vilariça AS, Sotto-Mayor R. Characterization and management of elderly and very elderly patients with non-small cell lung cancer. Clin Respir J. 2020;14(7):683–6. https://doi.org/10.1111/crj.13184.
Ettinger DS, Wood DE, Aisner DL, Akerley W, Bauman JR, Bharat A, et al. NCCN guidelines insights: non-small cell lung cancer, version 2.2021. J Natl Compr Canc Netw. 2021;19(3):254–66. https://doi.org/10.6004/jnccn.2021.0013.
de Ruiter JC, Heineman DJ, Daniels JM, van Diessen JN, Damhuis RA, Hartemink KJ. The role of surgery for stage I non-small cell lung cancer in octogenarians in the era of stereotactic body radiotherapy in the Netherlands. Lung Cancer. 2020;144:64–70. https://doi.org/10.1016/j.lungcan.2020.04.005.
Bei Y, Chen X, Raturi VP, Liu K, Ye S, Xu Q, et al. Treatment patterns and outcomes change in early-stage non-small cell lung cancer in octogenarians and older: a SEER database analysis. Aging Clin Exp Res. 2021;33(1):147–56. https://doi.org/10.1007/s40520-020-01517-z.
Damhuis RAM, Senan S, Khakwani A, Harden S, Helland Ȧ, Strand TE. Age-related treatment patterns for stage I NSCLC in three European countries. J Geriatr Oncol. 2021;12(8):1214–9. https://doi.org/10.1016/j.jgo.2021.05.005.
Cao C, Wang D, Chung C, Tian D, Rimner A, Huang J, et al. A systematic review and meta-analysis of stereotactic body radiation therapy versus surgery for patients with non-small cell lung cancer. J Thorac Cardiovasc Surg. 2019;157(1):362-373.e8. https://doi.org/10.1016/j.jtcvs.2018.08.075.
Wu J, Bai HX, Chan L, Su C, Zhang PJ, Yang L, et al. Sublobar resection compared with stereotactic body radiation therapy and ablation for early stage non-small cell lung cancer: a National Cancer Database study. J Thorac Cardiovasc Surg. 2020;160(5):1350-1357.e11. https://doi.org/10.1016/j.jtcvs.2019.11.132.
Ganti AK, Shostrom V, Alorabi M, Zhen WK, Marr AS, Trujillo K, et al. Early stage non-small-cell lung cancer in octogenarian and older patients: a SEER database analysis. Clin Lung Cancer. 2016;17(4):285–91. https://doi.org/10.1016/j.cllc.2015.11.014.
Ijsseldijk MA, Shoni M, Siegert C, Wiering B, van Engelenburg AKC, Tsai TC, et al. Oncologic outcomes of surgery versus SBRT for non-small-cell lung carcinoma: a systematic review and meta-analysis. Clin Lung Cancer. 2021;22(3):e235–92. https://doi.org/10.1016/j.cllc.2020.04.017.
Saftic I, Bille A, Asemota N, Berjon de la Vega L, Routledge T, King J, et al. Risks and rewards of the surgical treatment of lung cancer in octogenarians. Interact Cardiovasc Thorac Surg. 2021;33(6):905–12. https://doi.org/10.1093/icvts/ivab194.
Asemota N, Saftic I, Tsitsias T, King J, Pilling J, Bille A. Quality of life in octogenarians after lung resection compared to younger patients. Clin Lung Cancer. 2022;23(2):e118–30. https://doi.org/10.1016/j.cllc.2021.05.008.
Chan EY, Amirkhosravi F, Nguyen DT, Chihara RK, Graviss EA, Kim MP. Lobectomy provides the best survival for stage I lung cancer patients despite advanced age. Ann Thorac Surg. 2022;26:S0003-4975(22)00452-0. https://doi.org/10.1016/j.athoracsur.2022.03.031.
Mimae T, Saji H, Nakamura H, Okumura N, Tsuchida M, Sonobe M, et al. Survival of octogenarians with early-stage non-small cell lung cancer is comparable between wedge resection and lobectomy/segmentectomy: JACS1303. Ann Surg Oncol. 2021;28(12):7219–27. https://doi.org/10.1245/s10434-021-09835-w.
Mimae T, Miyata Y, Yoshimura K, Tsutani Y, Imai K, Ito H, et al. Risk of death due to other causes is lower among octogenarians with non-small cell lung cancer after wedge resection than lobectomy/segmentectomy. Jpn J Clin Oncol. 2021;51(10):1561–9. https://doi.org/10.1093/jjco/hyab122.
Razi SS, Kodia K, Alnajar A, Block MI, Tarrazzi F, Nguyen D, et al. Lobectomy versus stereotactic body radiotherapy in healthy octogenarians with stage I lung cancer. Ann Thorac Surg. 2021;111(5):1659–65. https://doi.org/10.1016/j.athoracsur.2020.06.097.
Chi A, Fang W, Sun Y, Wen S. Comparison of long-term survival of patients with early-stage non-small cell lung cancer after surgery vs stereotactic body radiotherapy. JAMA Netw Open. 2019;2(11): e1915724. https://doi.org/10.1001/jamanetworkopen.2019.15724.
Verma V, Shostrom VK, Kumar SS, Zhen W, Hallemeier CL, Braunstein SE, et al. Multi-institutional experience of stereotactic body radiotherapy for large (≥ 5 centimeters) non-small cell lung tumors. Cancer. 2017;123(4):688–96. https://doi.org/10.1002/cncr.30375.
Haque W, Singh A, Park HS, Teh BS, Butler EB, Zeng M, et al. Quantifying the rate and predictors of occult lymph node involvement in patients with clinically node-negative non-small cell lung cancer. Acta Oncol. 2022;61(4):403–8. https://doi.org/10.1080/0284186X.2021.2012253.
Schmidt-Hansen M, Baldwin DR, Zamora J. FDG-PET/CT imaging for mediastinal staging in patients with potentially resectable non-small cell lung cancer. JAMA. 2015;313(14):1465–6. https://doi.org/10.1001/jama.2015.2365.
Wu Y, Li P, Zhang H, Shi Y, Wu H, Zhang J, et al. Diagnostic value of fluorine 18 fluorodeoxyglucose positron emission tomography/computed tomography for the detection of metastases in non-small-cell lung cancer patients. Int J Cancer. 2013;132(2):E37-47. https://doi.org/10.1002/ijc.27779.
Gao SJ, Kim AW, Puchalski JT, Bramley K, Detterbeck FC, Boffa DJ, et al. Indications for invasive mediastinal staging in patients with early non-small cell lung cancer staged with PET-CT. Lung Cancer. 2017;109:36–41. https://doi.org/10.1016/j.lungcan.2017.04.018.
Crombag LMM, Dooms C, Stigt JA, Tournoy KG, Schuurbiers OCJ, Ninaber MK, et al. Systematic and combined endosonographic staging of lung cancer (SCORE study). Eur Respir J. 2019;53(2):1800800. https://doi.org/10.1183/13993003.00800-2018.
Hegde P, Molina JC, Thivierge-Southidara M, Jain RV, Gowda A, Ferraro P, et al. Combined endosonographic mediastinal lymph node staging in positron emission tomography and computed tomography node-negative non-small-cell lung cancer in high-risk patients. Semin Thorac Cardiovasc Surg. 2020;32(1):162–8. https://doi.org/10.1053/j.semtcvs.2019.07.007.
Chang JY, Mehran RJ, Feng L, Verma V, Liao Z, Welsh JW, et al. Stereotactic ablative radiotherapy for operable stage I non-small-cell lung cancer (revised STARS): long-term results of a single-arm, prospective trial with prespecified comparison to surgery. Lancet Oncol. 2021;22(10):1448–57. https://doi.org/10.1016/S1470-2045(21)00401-0.
Bei Y, Murakami N, Nakayama Y, Okuma K, Kashihara T, Raturi VP, et al. Stereotactic body radiation therapy for early-stage non-small-cell lung cancer in octogenarians and older: an alternative treatment. J Radiat Res. 2020;61(4):586–93. https://doi.org/10.1093/jrr/rraa027.
Watanabe K, Katsui K, Sugiyama S, Yoshio K, Kuroda M, Hiraki T, et al. Lung stereotactic body radiation therapy for elderly patients aged ≥ 80 years with pathologically proven early-stage non-small cell lung cancer: a retrospective cohort study. Radiat Oncol. 2021;16(1):39. https://doi.org/10.1186/s13014-021-01769-7.
Ball D, Tao Mai G, Vinod S, Babington S, Ruben J, Kron T, et al. Stereotactic ablative radiotherapy versus standard radiotherapy in stage 1 non-small-cell lung cancer (TROG 09.02 CHISEL): a phase 3, open-label, randomised controlled trial. Lancet Oncol. 2019;20(4):494–503. https://doi.org/10.1016/S1470-2045(18)30896-9.
Phillips I, Sandhu S, Lüchtenborg M, Harden S. Stereotactic ablative body radiotherapy versus radical radiotherapy: comparing real-world outcomes in stage I lung cancer. Clin Oncol (R Coll Radiol). 2019;31(10):681–7. https://doi.org/10.1016/j.clon.2019.07.013.
Tomita N, Okuda K, Osaga S, Miyakawa A, Nakanishi R, Shibamoto Y. Surgery versus stereotactic body radiotherapy for clinical stage I non-small-cell lung cancer: propensity score-matching analysis including the ratio of ground glass nodules. Clin Transl Oncol. 2021;23(3):638–47. https://doi.org/10.1007/s12094-020-02459-8.
Teke ME, Sarvestani AL, Hernandez JM, Fernando HC, Timmerman RD. A randomized, phase III study of sublobar resection (SR) versus stereotactic ablative radiotherapy (SAbR) in high-risk patients with stage I non-small cell lung cancer (NSCLC). Ann Surg Oncol. 2022;29(8):4686–7. https://doi.org/10.1245/s10434-022-11584-3.
Acknowledgements
The authors gratefully acknowledge the support from Healthcare Research Project of the Central Health Committee (Grant 2020YB32).
Funding
This study was supported by Healthcare Research Project of the Central Health Committee (Grant 2020YB32).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. LN and XL contributed to the conception of the study and drafting of the manuscript. DS and ZL contributed to the data extraction. GL and ZZ contributed to the statistical analysis. The first draft of the manuscript was written by LN, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
eTable 1. Characteristics of patients receiving surgery without LNE and radiotherapy after PSM. eTable 2. Characteristics of patients in the surgery and radiotherapy (refused surgery) groups after PSM
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ni, L., Lin, G., Zhang, Z. et al. Surgery versus radiotherapy in octogenarians with stage Ia non‑small cell lung cancer: propensity score matching analysis of the SEER database. BMC Pulm Med 22, 411 (2022). https://doi.org/10.1186/s12890-022-02177-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-02177-7