Abstract
Background
Lymphoepithelioma-like carcinoma (LELC) is a rare and unique subtype of cancer that histologically resembles undifferentiated nasopharyngeal carcinoma (NPC). The population-based analysis of LELC and the optimal treatment remains unclear.
Materials and methods
This real-world, retrospective study investigated 770 patients with LELC for primary site, treatment, and survival outcomes from 2005 to 2019 from five cancer centres in China. The overall survival (OS) of different subgroups was appraised by log-rank tests and Kaplan–Meier analysis.
Results
Primary sites LELC included the lung (597 cases, 77.5%), salivary gland (115 cases, 14.9%), and others. The median progression-free survival (PFS) of LELC patients was 47.4 months. The median overall survival (OS) was not reached. The 5-year survival rate for LELC patients was 77.8%. Most patients in stages I and II received surgery. The majority of patients in stage III received surgery and radiotherapy. More than half of the patients in stage IV received chemotherapy. Among relapsed or metastatic cases receiving chemotherapy, patients who received immunotherapy at any time presented with a superior OS than those without immunotherapy (P < 0.0001, HR = 0.39, 95% CI 0.25–0.63). Compared with the SEER database, patients with LELC had a better prognosis than NPC, with a 5-year overall survival of 77.3% vs. 56.8% (P < 0.001).
Conclusion
Our data provide treatment patterns and outcomes for LELC from various primary sites. Randomized controlled studies are necessary to further define the standard of care for patients with LELC.
Trial registration This clinical trial was registered at ClinicalTrials.gov (No. NCT04614818).
Similar content being viewed by others
Introduction
Lymphoepithelioma-like carcinoma (LELC), an Epstein-Barr virus (EBV)-driven cancer, resemble nasopharynx carcinoma but can originate from the pharyngeal and other foregut-derived organs, such as the lung and gastrointestinal tract [1]. The 2004 World Health Organization classification previously recognized LELC of the lung as a subtype of large cell carcinoma, whereas the current 2015 World Health Organization classification scheme categorizes LELC under other and unclassified carcinomas. The lung is the most common primary site of LELC, and some retrospective studies have summarized cases of pulmonary LELC [2]. Several case reports have focused on LELC from different primary sites, such as parotid glands, submandibular glands, stomach, breast, skin, and liver [3,4,5].
Since LELC is a rare type of cancer, its optimal management is not clear. Total resection of tumours seems to be the proper treatment for early-stage LELC in the salivary glands, liver, and thymus [5,6,7]. Lin and colleagues reported that gemcitabine-based chemotherapy and palliative thoracic radiotherapy were associated with a better overall survival in 127 irresectable pulmonary LELC patients from a single centre [8]. Although several studies have shown high programmed death legand-1 (PD-L1) expression in LELCs [6, 9,10,11,12], its response to immunotherapy is controversial in different reports [13, 14]. The genome landscape of LELC revealed a similarity to NPC [9, 12, 15], but comparisons of the survival and prognosis of LELC and NPC are lacking. Analysis of the characteristics, treatment, survival, and prognosis of LELC is warranted. Thus, we collected data from multiple centres to explore the optimal treatment pattern of LELC and summarized the prognosis of LELC compared to NPC.
Materials and methods
Patient selection
From August 2005 to September 2019, we enrolled patients with LELC at five cancer centres, including Sun Yat-sen Cancer Centre (SYSUCC), Sichuan Cancer Centre, Henan Cancer Hospital, Hunan Cancer Hospital and Guangxi Medical University Cancer Hospital. Eligible patients had histologically confirmed LELC and had clear medical records. Their medical records were analysed for investigation. All patients underwent treatment selected by experienced doctors at cancer centres. The study protocol was approved by the ethical committee of the Sun Yat-sen University Cancer Centre (approval number B2020–289–01). This clinical trial was registered at ClinicalTrials.gov (No. NCT04614818) since 4th, November, 2020.
To compare the prognosis of LELC with NPC and pulmonary squamous carcinoma, two cohorts were established from the Surveillance, Epidemiology, and End Results (SEER) database. The patient data from 2010 to 2016 were acquired by SEER ∗ Stat software (Version 8.3.5, http://seer.cancer.gov/seerstat/download). The inclusion criteria for the NPC and lung cancer cohort were as follows: (1) a clear pathological diagnosis of NPC and squamous cell carcinoma of the lung, respectively; (2) a diagnosis from 2010 to 2016; (3) the TNM stage of the patients followed the seventh edition of the AJCC; and (4) a clear survival time. The exclusion criteria in both cohorts were cases with only autopsy or death certificates and invalid follow-up. The data cut-off was at March 12, 2021.
Parameters
The following clinical and laboratory data were collected: age, gender, smoking history, Eastern Cooperative Oncology Group performance status (ECOG PS), metastatic sites, clinical stage, treatment modality, EBV DNA, genome mutation status, and ALK rearrangement status. The detection for EBV infection was demonstrated by serum EBV-DNA levels. EBER in situ hybridization was exanimated as routine pathology process. Patient follow-ups were obtained through medical records or by telephone interview. Efficacy was assessed according to Response Evaluation Criteria in Solid Tumours (RECIST) version 1.1 [16].
For the SEER database, the demographic data included age (0–24, 25–49, 50–74, and ≥ 75 years), gender (male, female), and race (white, black, and others (American Indian/Alaska Native or Asian/Pacific Islander)). The clinical properties incorporated T stage (T0, T1, T2, T3, T4, and unknown), N stage (N0, N1, N2, N3, and unknown), and organ metastases (none, yes, and unknown).
Statistical analysis
The study population for all analyses included patients enrolled in the study who had an adequate baseline tumour assessment. Descriptive statistics were used to summarize the patient characteristics, treatment administration, and objective response, and the results are presented as medians and ranges. Survival was measured from the initiation of therapy until death. Overall survival (OS) was defined as the time between the initiation of treatment to death from any cause. Patients who did not die were censored at the date of last contact. The date of censoring data was at March 12, 2021. The objective response rate (ORR), disease control rate (DCR), disease-free survival (DFS) and progression-free survival (PFS) were also analysed. Pearson chi-square or Fisher’s exact test and Wilcoxon tests were used to identify between-group differences for categorical variables and continuous variables, respectively. Univariable Cox regression analyses and multivariable proportional hazards regression models were carried out to identify independent prognostic factors. All reported P values were two-sided, and P < 0.05 was considered to be statistically significant. All statistical analyses were carried out using SPSS version 25 (SPSS Inc., Chicago, IL, USA) and R version 4.0.2.
Results
Baseline character
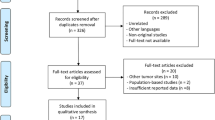
In our study, 831 cases of LELC were collected, 15 patients did not receive any treatment. Three hundred patient follow-ups were obtained by telephone interview and 470 patients followed through clinic interview. As of the data cut-off, 46 patients were lost to follow-up. Finally, a total of 770 consecutive patients were included in the analyses. 117 (15.2%) patients died, and 653 (84.8%) were alive. The median follow-up time was 34.6 months (range 0.3–179 months). The baseline characteristics of the patients are summarized in Table 1. Among the 770 patients, the median age was 52 years (range, 12–82), 408 (53.0%) were female, 721 (93.6%) had an ECOG PS of 0, and 618 (80.3%) were never-smokers. The origin of the LELCs is summarized in Fig. 1A. The majority of patients had LELC of lung origin (77.7%). A total of 115 patients (14.9%) had the primary site at the salivary gland, and 16 patients (2.2%) were diagnosed with gastric LELC. The other uncommon primary sites (less than 1%) included the thymus, uterine cervix, mediastinum, oropharynx, oesophagus, liver, tonsil, ovary, penis, and external auditory canal. Eight patients were diagnosed with LELC of unknown primary source.
In 679 cases with EBER results, 98.4% of them was EBER positive. A total of 344 (44.7%) patients had baseline tests for EBV-DNA, and 174 (50.6%) showed EBV DNA copy numbers higher than 103 copy/mL. A total of 305 (39.6%) patients underwent genetic tests, including EGFR mutations and ALK fusion. EGFR mutations were detected in only 10 (3.3%) patients. ALK mutations were detected in only 3 (1.0%). Seven cases presented with a mutation of TP53. Thirty-four patients had PD-L1 expression detected, and 16 patients had PD-L1 expression greater than 50%. 25 patients (73.5%) presented PD-L1 expression higher than 1%. Most patients were at stage III (32.7%) or IV (33.5%) at the time of initial diagnosis (Fig. 1B).
Survival outcome
The PFS and OS of all LELC patients are shown in Fig. 2A and B, respectively. The median PFS in LELC patients was 47.4 months, and the median OS was not reached. The survival analysis among the different stages and primary sites is shown in Fig. 2C, D and E, respectively, resulting in PLELC presenting worse outcomes than any other primary site. Compared with NPC from the SEER database, LELC showed a better OS (Fig. 3A), and subgroup analysis for stage I, II, III and IV LELC revealed the same results compared with NPC at stage I, II, III and IV, respectively (Fig. 3 B, C, D and E). When comparing pulmonary LELC with squamous carcinoma of the lung, it was found that pulmonary LELC also showed superior OS than squamous cell carcinoma of the lung (Fig. 3F).
Treatment pattern for patients at stage I–II
The treatment pattern for patients at different stages varied. The survival of LELC patients at different stages is shown in Fig. 2D. For 118 patients in stage I, all patients underwent surgery. Among them, 5 patients received neoadjuvant chemotherapy before surgery. Thirty-eight patients received adjuvant chemotherapy, and 9 patients received adjuvant radiotherapy. Patients receiving adjuvant chemotherapy showed inferior DFS (P = 0.028, HR = 3.77, 95% CI 1.15–12.3) and a similar OS to those without adjuvant chemotherapy (Fig. 4A and Additional file 1: Fig. S1A). Due to limited number of patients received radiotherapy at stage I, the role of radiotherapy was uncertain (Additional file 1: Fig. S1B, C). For 133 patients in stage II, 131 patients received surgery, while one patient with oesophageal LELC received sequencing chemotherapy and radiotherapy, and one patient with PLELC received concurrent chemotherapy and radiotherapy. Seventeen patients received neoadjuvant chemotherapy. Eighty patients received adjuvant chemotherapy, and 20 patients received adjuvant radiotherapy. Patients receiving adjuvant chemotherapy showed a longer DFS (P = 0.023, HR = 0.38, 95% CI 0.16–0.87) but similar OS to those without adjuvant chemotherapy (Fig. 4B and Additional file 2: Fig. S2A). No significant difference was observed between patients with and without adjuvant radiotherapy (Additional file 2: Fig. S2B, C).
DFS in patients receiving adjuvant chemotherapy at stage I (A) and II (B). DFS in patients receiving adjuvant radiotherapy at stage III (C). PFS (D) and OS (E) in patients receiving pemetrexed-based chemotherapy as first-line regimen at stage IV or after relapsed. OS in patients at stage IV or after relapsed receiving immunotherapy at any time (F)
Treatment pattern for patients at stage III
For 252 patients in stage III, 169 patients underwent surgery, among whom 24 patients received neoadjuvant chemotherapy. In 169 patients who underwent surgery, 121 patients received adjuvant therapy, with 107 receiving chemotherapy and 50 radiotherapies. Patients unsuitable for surgery received chemotherapy (n = 28) and radiotherapy (n = 55) based on the evaluation case by case of experienced physicians. The median PFS in stage III patients was 46.1 months, but the median OS was not reached. Patients receiving adjuvant chemotherapy showed similar OS rates to those without adjuvant chemotherapy (Additional file 3: Fig. S3A, B). However, patients receiving adjuvant radiotherapy showed a longer DFS (P = 0.043, HR = 0.59, 95% CI 0.35–0.98) but a similar OS (Fig. 4C and Additional file 3: Fig. S3C).
Treatment pattern for patients at stage IV
For 258 patients in stage IV at initial diagnosis, 133 patients received first-line chemotherapy, and 87 patients received surgery; 35 patients received radiotherapy; 3 patients received targeted therapy including osimertinib, afatinib and alectinib; 179 patients relapsed after surgery or radiotherapy, and 69 of them received chemotherapy as first-line treatment. For 226 patients treated with different chemotherapy regimens, it was demonstrated that most patients received a platinum-based regimen as first-line chemotherapy. The ORR and DCR for all regimens were 46.9% and 83.2%, respectively. According to the different regimens, 48 patients received pemetrexed- and platinum-based regimens, 33 patients received gemcitabine- and platinum-based regimens, and the majority of patients (n = 110) received paclitaxel- and platinum-based regimens. The median PFS in stage IV patients was 12.5 months, and the median OS was 68.4 months. Comparing the different regimens, pemetrexed-based regimens had a worse PFS and OS (Fig. 4D, E). The paclitaxel-based regimen showed a superior OS but similar PFS (Additional file 4: Fig. S4A, B). However, gemcitabine-based regimens presented better PFS but a similar OS (Additional file 4: Fig. S4C, D). In addition to chemotherapy, some patients were also treated with antiangiogenic therapy, such as bevacizumab, anti-EGFR antibodies and immune checkpoint inhibitors. Seventeen patients received chemotherapy combined with antiangiogenic regimens, including bevacizumab, recombinant human endostatin, apatinib and nilotinib. Eight patients received chemotherapy combined with anti-EGFR antibodies, including cetuximab and nituzumab. For patients with and without anti-angiogenesis or anti-EGFR, no significant difference was shown in their survival outcome (Additional file 5: Fig. S5A, B).
Ninety-six patients received immune checkpoint inhibitors, including PD-1 antibody and PD-L1 antibody. Thirty-two patients received immunotherapy as first-line treatment. Among relapsed or metastatic cases receiving chemotherapy, patients who received immunotherapy at any time with metastasis or relapses presented a superior OS than those without immunotherapy (P < 0.0001, HR = 0.39, 95% CI 0.25–0.63, Fig. 4F). No significant difference in OS was found between patients receiving immunotherapy as first-line or after prior chemotherapy. For patients at stage IV, those who had received radiotherapy showed better outcomes than those who had not received radiotherapy (Additional file 4: Fig. S4E).
Prognosis predictors
For the prognosis of LELC patients, it was found that the following clinical factors significantly predicted poor survival in univariable analysis: ECOG PS ≥ 2, stage III-IV, lung as the primary site, bone metastasis, liver metastasis, pleura metastasis, nonregional lymph node metastasis, adrenal metastasis, and a high level of serum EBV DNA copy (Additional file 6: Fig. S6). Multivariable analysis demonstrated that five variables had a negative prognostic influence on OS, including ECOG PS ≥ 2, stage III–IV, a high level of EBV-DNA, liver metastasis and bone metastasis (Table 2).
Discussion
The understanding for LELC was generally based on single centre study for PLELC, LELC of salivary glands [2, 15, 17]. The rare origin of LELC included thyroid, skin, thymus, liver, breast, external auditory canal, lips, laryngopharyngeal, urinary tract, and tonsil mainly reported by a few cases [5, 18,19,20,21,22,23,24,25,26]. The clinicopathological characteristics and prognosis of LELC from other origins based on multiple centres and large sample sizes are unknown.
In our study, we reported the clinicopathological characteristics, treatment pattern and prognosis of LELC from different origins at multiple cancer centres, with the largest sample size of LELC so far. In summary, we reported the treatment pattern of 770 LELC cases from five cancer centres. It was demonstrated that LELC presented better survival outcomes than NPC patients. The benefit of adjuvant chemotherapy and radiotherapy varied among different stages of LELC. For advanced disease, the pemetrexed-based regimen showed inferior PFS and OS. Patients receiving immunotherapy at any time with metastasis or relapses presented a superior OS than those without immunotherapy. Radiotherapy was also beneficial for patients at an advanced stage.
The pathological characteristics among different primary sites of LELC were fairly consistent and histologically resembled undifferentiated NPC. Most cases of LELC were closely related to EBV infection and were EBER-positive [1, 3, 11, 27, 28], but EBER was negative in most cases of LELC from the head and neck skin [18, 23]. In our study, p40, CK5/6, p63 and EBER were positive in most patients. More than half of the patients (174 out of 344 cases detected EBV-DNA) revealed a high level of baseline serum EBV DNA. High EBV-DNA was also associated with poor survival. EBV DNA should be monitored during treatment and follow-up. In a multivariate model of 127 advanced PLELC cases, cycles of first-line chemotherapy, palliative thoracic radiotherapy, and baseline EBV DNA were significantly associated with OS [8]. Chen B and colleagues also showed that positive serum EBV-DNA appeared to be a predictor of PFS [29]. In our study, high EBV DNA was correlated with poor survival, which is consistent with a previous study [8, 29]. It was also concluded that ECOG PS ≥ 2, stage III–IV, liver metastasis and bone metastasis independently predicted survival in LELC patients. Thus, the evaluation of liver and bone as well as serum EBV DNA is important for patients with LELC at the time of initial diagnosis.
In our study, compared with NPC in the SEER database, LELC showed a superior prognosis. The reason might be that most patients at an early stage had opportunities for radical surgery. Several case reports have shown that surgical resection is the basic treatment for LELC of the breast, liver, thyroid, thymus, and skin [4, 11, 18, 21]. The analysis from the SEER database of 179 cases of salivary gland LELC demonstrated that surgery and postsurgical radiotherapy significantly improved OS [30]. For adjuvant therapy, patients in stage I did not benefit from adjuvant chemotherapy or radiotherapy. Although adjuvant chemotherapy prolonged DFS, OS was not improved. The survival outcome varied among patients at stage III. For patients receiving surgery at stage III, adjuvant radiotherapy improved DFS. In our study, neither adjuvant chemotherapy nor radiotherapy improved OS. Thus, more prospective exploration of the application of adjuvant therapy is necessary.
The sensitivity to radiotherapy and chemotherapy in LELC is not clear. Most patients diagnosed with parotid LELC receive radiotherapy [7, 30], and concurrent chemoradiotherapy is effective for patients with middle ear and sinonasal LELC [26, 31]. The prognosis for patients receiving surgery seems to be based on the primary site. The recurrence rate for liver LELC is much lower than that for hepatic cell carcinoma and intrahepatic cholangiocarcinoma [3, 5]. However, patients with thymic LELC relapse rapidly after surgery [4, 6]. In our study, 141 out of 383 patients relapsed after surgery. The treatment for patients in an advanced stage or after a relapse needs further exploration. In our study, the patients receiving radiotherapy had a superior OS. First-line chemotherapy was selected based on experience in different cancer centers. In a study including 127 patients with advanced PLELC, paclitaxel and platinum-based chemotherapy presented a median PFS of 12 months, while pemetrexed-based regimens only achieved a median PFS of 5 months [8]. Our study included 226 patients receiving first-line chemotherapy and demonstrated that the pemetrexed-based regimen showed a poor PFS and OS. However, the benefit of TP and GP regimens is controversial. GP revealed a prolonged PFS but a similar OS, while TP presented the opposite result. The optimal regimen for LELC and the role of radiotherapy should be further explored in prospective studies. Multimodality treatment is also warranted for LELC.
The majority of pulmonary LELCs (74.3%–75.8%) overexpressed PD-L1 [10, 32]. High expression of PD-L1 was also detected in LELC of the thymus and liver [6, 33]. However, the efficacy of immunotherapy in LELC remains unclear. Some case reports presented a promising response to PD-L1 blockade [34]. However, other cases revealed rapid progression after immunotherapy [14]. In our study, patients receiving immunotherapy at any time showed a prolonged OS, which suggested an important role of immune checkpoint inhibitors. Similar to NPC, the genomic landscape of LELC for the lung and liver showed a high frequency of TP53 mutations [9, 12, 15]. However, mutation analysis suggested a low tumour burden and low levels of driver gene mutations in PLELC patients [15, 32, 35]. The mechanism by which patients respond or are resistant to PD-1/PD-L1 blockade needs further understanding. In our study, one patient with advanced PLELC treated with pembrolizumab and paclitaxel-based chemotherapy progressed after six cycles and harbored secondary amplification of PI3KCA and IL-7R, which might be one possible mechanism for PD-1 resistance [14]. In our study, NGS analysis and PD-L1 expression were only detected in a few patients. Among patients detected PD-L1, 73.5% of them presented PD-L1 overexpression high than 1%. More biomarkers to predict the outcome of immunotherapy are under exploration. Anti-EGFR antibody and anti-angiogenesis therapy play an important role in NPC and lung cancer, respectively. However, no significant difference was shown in patients receiving either anti-EGFR antibody or anti-angiogenesis therapy. Thus, the role of anti-EGFR and antiangiogenic agents needs more exploration.
The major limitation of this study lies in its retrospective nature and its heterogeneity in baseline risk and treatment factors, which may have led to potential bias. In outr study, the number of patients with PD-L1 detection and NGS results was limited, which made it difficult to understand the relation between efficacy of immunotherapy and biomarkers. Our further research might focus on PD-L1 expression and NGS in available samples. Nonetheless, these findings add to the growing body of data demonstrating the clinicopathological and treatment patterns in patients with LELC from many kinds of primary sites. The main strength of the present study is that it is the first report summarizing LELC from different origins, including a large number of real-world patients; thus, these findings might be generalizable to a broad population of patients. Therefore, prospective clinical trials to confirm the optimal treatment for LELC are warranted.
Conclusion
LELC from various primary sites resembles NPC but with better survival outcomes. The benefit of adjuvant therapy for LELC at early stage varied. The immunotherapy and radiotherapy showed better survival outcome for advanced LELC patients. The optional treatment for different stage of LELC needed more prospective studies.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- LELC:
-
Lymphoepithelioma-like carcinoma
- NPC:
-
Nasopharyngeal carcinoma
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- EBV:
-
Epstein-Barr virus
- PD-L1:
-
Programmed death legand-1
- SEER:
-
Surveillance, Epidemiology, and End Results
- ECOG PS:
-
Eastern Cooperative Oncology Group performance status
- RECIST:
-
Response Evaluation Criteria in Solid Tumours
- ORR:
-
Objective response rate
- DCR:
-
Disease control rate
- DFS:
-
Disease-free survival
References
Sathirareuangchai S, Hirata K. Pulmonary lymphoepithelioma-like carcinoma. Arch Pathol Lab Med. 2019;143(8):1027–30.
Qin Y, Gao G, Xie X, Zhu Z, Guan W, Lin X, Xie Z, Ming O, Chen R, Zhong N, et al. Clinical features and prognosis of pulmonary lymphoepithelioma-like carcinoma: summary of eighty-five cases. Clin Lung Cancer. 2019;20(3):e329–37.
Ding Y, Sun Z, You W, Zhang S, Chang C, Yan S, Wang W. Lymphoepithelioma-like intrahepatic cholangiocarcinoma with Epstein-Barr virus infection: report of a rare case. Ann Transl Med. 2019;7(18):497.
Kawagishi S, Ose N, Minami M, Funaki S, Kanou T, Kimura K, Taniguchi S, Morii E, Shintani Y. Total thymectomy for thymic lymphoepithelioma-like carcinoma-report of two cases. Surg Case Rep. 2019;5(1):158.
Labgaa I, Stueck A, Ward S. Lymphoepithelioma-like carcinoma in liver. Am J Pathol. 2017;187(7):1438–44.
Suster D, Pihan G, Mackinnon A, Suster SJ, Mpaojot US. Canadian Academy of Pathology I: Expression of PD-L1/PD-1 in lymphoepithelioma-like carcinoma of the thymus. Modern Pathol. 2018;31(12):1801–6.
Hsiung C, Huang C, Wang C, Huang E, Huang H. Lymphoepithelioma-like carcinoma of salivary glands: treatment results and failure patterns. Br J Radiol. 2006;79(937):52–5.
Lin Z, Fu S, Zhou Y, Zhang X, Chen C, He L, Li H, Wang Y, Chen T, Zhang L, et al. First-line platinum-based chemotherapy and survival outcomes in locally advanced or metastatic pulmonary lymphoepithelioma-like carcinoma. Lung Cancer. 2019;137:100–7.
Hong S, Liu D, Luo S, Fang W, Zhan J, Fu S, Zhang Y, Wu X, Zhou H, Chen X, et al. The genomic landscape of Epstein-Barr virus-associated pulmonary lymphoepithelioma-like carcinoma. Nat Commun. 2019;10(1):3108.
Fang W, Hong S, Chen N, He X, Zhan J, Qin T, Zhou T, Hu Z, Ma Y, Zhao Y, et al. PD-L1 is remarkably over-expressed in EBV-associated pulmonary lymphoepithelioma-like carcinoma and related to poor disease-free survival. Oncotarget. 2015;6(32):33019–32.
Chen J, Zhou L, Qiu X, Yang R, Liang J, Pan Y, Li H, Peng G, Shao C. Determination and genome-wide analysis of Epstein-Barr virus (EBV) sequences in EBV-associated gastric carcinoma from Guangdong, an endemic area of nasopharyngeal carcinoma. J Med Microbiol. 2018;67(11):1614–27.
Chan A, Zhang Z, Chong C, Tin E, Chow C, Wong N. Genomic landscape of lymphoepithelioma-like hepatocellular carcinoma. J Pathol. 2019;249(2):166–72.
Kumar V, Dave V, Harris J, Huang Y. Response of advanced stage recurrent lymphoepithelioma-like carcinoma to nivolumab. Immunotherapy. 2017;9(12):955–61.
Chen M, Wang Z, Yuan M, Fang X, Lin T. Treatment of pembrolizumab and chemotherapy results in pulmonary lymphoepithelioma-like carcinoma progression through harboring secondary amplification of PI3KCA and IL-7R. Lung Cancer. 2020;144:87–9.
Chen B, Zhang Y, Dai S, Zhou P, Luo W, Wang Z, Chen X, Cheng P, Zheng G, Ren J, et al. Molecular characteristics of primary pulmonary lymphoepithelioma-like carcinoma based on integrated genomic analyses. Signal Transduction Targeted Ther. 2021;6(1):6.
Eisenhauer E, Therasse P, Bogaerts J, Schwartz L, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Kim Y, Hong H, Jeong S, Lee E, Jung MJM. Lymphoepithelial carcinoma of the salivary glands. Medicine. 2017;96(7): e6115.
Welch P, Williams S, Foss R, Tomaszewski M, Gupta A. Ojha JJOs, oral medicine, oral pathology, oral radiology, endodontics: Lymphoepithelioma-like carcinoma of head and neck skin: a systematic analysis of 11 cases and review of literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol. 2011;111(1):78–86.
Sekihara K, Okuma Y, Kawamoto H, Hosomi Y. Clinical outcome of thymic lymphoepithelioma-like carcinoma: Case report of a 14-year-old male. Oncol Lett. 2014;8(5):2183–6.
Attaran Y, Moghdam S, Monabati A, Sarkeshikian R. Lymphoepithelial-like carcinoma with papillary transitional cell carcinoma of the urinary bladder associated with carcinoma in situ changes of the urothelium; A case report and review of literature. Iran J Pathol. 2019;14(2):156–64.
Fadila K, Faycal A, Lamiaa J, Mohammed B, Nabil I. Lymphoepithelioma-like carcinoma of the breast: a case report and review of the literature. Pan Afr Med J. 2019;32:18.
Sairin M, Yahya N, Kuan C, Yunus M, Abdullah M. Management of a rare lymphoepithelial carcinoma of the submandibular gland in elderly. Indian J Otolaryngol Head Neck Surg. 2019;71:18–20.
Almeida L, Silveira H, Silva E, Barbeiro C, de Paula J, Bufalino A, Ribeiro-Silva A, León JE. EBV-negative lymphoepithelial-like carcinoma of the lower lip. Autopsy Case Rep. 2020;10(1): e2020138.
Faisal M, Hartenbach S, Schratter A, Köstler W, Kaufmann H, Seemann R, Lill C, Hamzavi S, Wutzl A, Erovic BM. Lymphoepithelial carcinoma of larynx and hypopharynx: a rare clinicopathological entity. Cancers. 2020;12(9):2431.
Whelan A, Al-Sayed A, Bullock M, Taylor SM. Primary parotid lymphoepithelial carcinoma: a case report and literature review of a rare pathological entity. Int J Surg Case Rep. 2020;72:610–4.
Fong P, Tan T, Kiong KL. Concurrent chemoradiation in locally advanced primary middle ear lymphoepithelial carcinoma: an effective treatment modality case report. J Otolaryngol Head Neck Surg. 2021;50(1):1.
Monteiro F, Baldaia H, Ribeiro L, Sousa M, Oliveira P, Ferreira E, de Almeida M, Condé A. Epstein-Barr virus-associated with lymphoepithelial carcinoma: a rare tumor of the larynx. Clin Med Insights Ear Nose Throat. 2019;12:1179550619865551.
Liu C, Huang SH. EBV-associated lymphoepithelioma-like thyroid carcinoma with favorable outcome: case report with cytopathologic and histopathologic study. Diagn Pathol. 2018;13(1):39.
Chen B, Chen X, Zhou P, Yang L, Ren J, Yang X, Li W. Primary pulmonary lymphoepithelioma-like carcinoma: a rare type of lung cancer with a favorable outcome in comparison to squamous carcinoma. Respir Res. 2019;20(1):262.
Wang J, Deng R, Liu H, Luo Y, Yang ZC. Clinicopathological characteristics and prognostic analysis of lymphoepithelial carcinoma of salivary gland: a population-based study. Gland Surg. 2020;9(6):1989–97.
Takakura H, Tachino H, Fujisaka M, Nakajima T, Yamagishi K, Ishida M, Shojaku HJM. Lymphoepithelial carcinoma of the maxillary sinus: a case report and review of the literature. Medicine. 2018;97(28): e11371.
Wu Q, Wang W, Zhou P, Fu Y, Zhang Y, Shao Y, Jiang L. Primary pulmonary lymphoepithelioma-like carcinoma is characterized by high PD-L1 expression, but low tumor mutation burden. Pathol Res Pract. 2020;216(8):153043.
Wang L, Dong H, Ni S, Huang D, Tan C, Chang B, Sheng W. Programmed death-ligand 1 is upregulated in intrahepatic lymphoepithelioma-like cholangiocarcinoma. Oncotarget. 2016;7(43):69749–59.
Narayanan A, Knollmann F, Walby J, Lim S, Gandara D, Riess JW. EBV-positive primary pulmonary lymphoepithelioma-like carcinoma response to PD-L1 blockade. Clin Lung Cancer. 2019;20(3):e238–41.
Chau S, Tong J, Chow C, Kwan J, Lung R, Chung L, Tin E, Wong S, Cheung A, Lau R, et al. Distinct molecular landscape of Epstein-Barr virus associated pulmonary lymphoepithelioma-like carcinoma revealed by genomic sequencing. Cancers. 2020;12(8):2065.
Acknowledgements
The authors thank all the patients, their families, and the institutions for supporting this study. They acknowledge all medical staff, nurses, and research nurses, all of whom strongly contributed to the success of the study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
TL and He Huang designed the study; MC, YC, ML, Huangming Hong, CL, HG, XP, FP and QL collected the data. MC, ML, Huangming Hong, CL, HG, XP, ZW, XF assembled the data; MC, TL and He Huang analysed and interpreted the data; All authors wrote and gave final approval to the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethical committee of the Sun Yat-sen University Cancer Centre (approval number B2020-289-01). The informed consent was not required because this study was a retrospective report of cases, which is a retrospective analysis of clinical data with no relevant to human biological ethic problems. The need of informed consent was waived by the ethical committee of the Sun yat-sen University Cancer Centre. The study was performed in accordance with the principles of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Figure S1:
Kaplan–Meier survival analysis for OS in patients receiving adjuvant chemotherapy at stage I (A). DFS(B) and OS(C) in patients receiving adjuvant radiotherapy at stage I
Additional file 2. Figure S2:
Kaplan–Meier survival analysis for OS in patients receiving adjuvant chemotherapy at stage II (A). DFS(B) and OS(C) in patients receiving adjuvant radiotherapy at stage II
12890_2022_2097_MOESM3_ESM.tif
Additional file 3 Supplement Figure 3 Kaplan–Meier survival analysis for OS in patients receiving adjuvant radiotherapy at stage III (A). DFS(B) and OS(C) in patients receiving adjuvant chemotherapy at stage III
Additional file 4. Figure S4:
Kaplan–Meier survival analysis for PFS (A) and OS (B) in patients receiving paclitaxel-based chemotherapy as first-line regimen at stage IV or after relapsed. PFS (C) and OS (D) in patients receiving gemcitabine-based chemotherapy as first-line regimen at stage IV or after relapsed. OS in patients at stage IV or after relapsed receiving radiotherapy (E)
Additional file 5. Figure S5:
Kaplan–Meier survival analysis for OS in patients receiving anti- angiogenesis (A) and anti- EGFR (B) therapy at stage IV or after relapsed. Kaplan–Meier survival analysis for PFS in patients receiving anti-angiogenesis (C) and anti-EGFR (D) therapy at stage IV or after relapsed
Additional file 6. Figure S6:
Kaplan–Meier survival analysis for OS according to ECOG PS≥2 (A), stage III-IV (B) , high level of EBV-DNA (C), liver metastasis (D) and bone metastasis (E)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, M., Chen, Y., Fang, X. et al. Clinical features and treatment outcome of lymphoepithelioma-like carcinoma from multiple primary sites: a population-based, multicentre, real-world study. BMC Pulm Med 22, 360 (2022). https://doi.org/10.1186/s12890-022-02097-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-02097-6