Abstract
Background
Lung clearance index (LCI) is accepted as an early marker of lung disease in cystic fibrosis (CF), however the utility of LCI to identify subgroups of CF disease in the paediatric age group has never been explored. The aim of the study was to characterize phenotypes of children with CF using LCI as a marker of ventilation inhomogeneity and to investigate whether these phenotypes distinguished patients based on time to pulmonary exacerbation (PE).
Methods
Data were collected on patients with CF aged < 18 years old, attending the CF Center of Milan during outpatient follow-up visits between October 2014 and September 2019. Cluster analysis using agglomerative nesting hierarchical method was performed to generate distinct phenotypes. Time-to-recurrent event analysis investigated association of phenotypes with PE.
Results
We collected 313 multiple breath washout tests on 125 children aged 5.5–16.8 years. Cluster analysis identified two divergent phenotypes in children and adolescents of same age, presenting with almost normal FEV1 but with substantial difference in markers of ventilation inhomogeneity (mean LCI difference of 3.4, 95% Confidence Interval [CI] 2.6–4.2). A less severe phenotype was associated with a lower risk of PE relapse (Hazard Ratio 0.45, 95% CI 0.34–0.62).
Conclusions
LCI is useful in clinical practice to characterize distinct phenotypes of children and adolescents with mild/normal FEV1. A less severe phenotype translates into a lower risk of PE relapse.
Similar content being viewed by others
Introduction
Lung clearance index (LCI) is the main derivative of the multiple breath washout test (MBW), and it has gained lot of attention during the last years as a promising outcome measure in cystic fibrosis (CF), complementary to conventional spirometry. Being CF characterized by a progressive lung disease, LCI has denoted itself as an early marker of ventilation inhomogeneity [1], measuring the unevenness of ventilation and thus recognizing early signs of CF lung disease [2], especially in children with a normal/above normal spirometry.
Evidence collected so far has recognized LCI as an outcome measure in interventional trials [3,4,5]. Only recently, LCI was found sensitive to assess CF disease progression without overt clinical symptoms [6], however the utility of LCI as a clinical marker to guide the multidisciplinary practice of the CF team is still a matter of discussion [7, 8]. Considering that personalized medicine not only aims to target therapies but also to identify individuals at elevated risk that could benefit most from therapies, we hypothesized that LCI can help to characterize clinical phenotypes of children with CF with regards to severity of lung disease.
In order to describe individuals who could benefit most from personalized therapies, we aimed to identify subgroups of children and adolescents with CF using known markers of the disease together with early markers of ventilation inhomogeneity. Furthermore, we investigated whether resulting phenotypes could discriminate young individuals with CF based on time to pulmonary exacerbation (PE).
Methods
Study design
With the aim to profile children with CF according to their clinical characteristics, we adopted a cross-sectional design, using data generated on the first MBW assessment to identify clusters (i.e., phenotypes). On the contrary, a 4-year cohort design was considered to explore the association between phenotypes and the risk of PE relapse, conceived as the time since the first MBW performed to date(s) of PE.
The study has been approved by local ethics committee of Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico (456/2021), and written informed consent was obtained from parents or guardians of participants. All research was conducted in accordance with relevant guidelines and regulations.
Participants
Clinical data were collected on children and adolescents aged < 18 years old, attending the CF Center of Milan during routine outpatient visits between October 2014 and September 2019. As per current clinical practice, children perform MBW test and spirometry as part of their clinical review. For the cross-sectional analysis, only lung function test results from participants in clinical stable condition were considered. Clinical stability was defined as the absence of change in treatment (i.e., antibiotic treatment, systemic corticosteroids), hospital admissions and/or signs and symptoms of pulmonary exacerbation [9]. Further, we included only paediatric individuals with at least two MBW assessments during the study period, in order to have at least one follow-up measure to assess phenotypes over time.
Pulmonary measures
Lung volumes were measured by a 830 L plethysmograph (Master Screen Body 4.2, E. Jaeger GmbH) in the sitting position, according to ATS/ERS guidelines [10]. Flow and volume were measured by a pneumotachograph with a 0.036 kPa L/-1 s resistance and 160 ml dead volume. Values from spirometry are reported as a percentage of predicted values and as Z score, according to Quanjer’s equation developed under the Global Lung Function initiative [11]. Patients’ lung function was considered in the normal range when FEV1 was above the − 1.64 Z score (lower limit of normal at 5th centile).
An open-circuit MBW hard- and software package with nitrogen as tracer gas (MBWN2) was used (Exhalyzer® D and Spiroware 3.2.2 Ecomedics AG, CH) and calibration and measurement procedures were performed as suggested [12,13,14,15]. Only results from three reproducible runs were considered, defined as a variation of functional residual capacity and LCI (1/40th of the starting concentration) values within 10%. LCI together with convective gas mixing in the conducting airways (Scond*VT) and diffusion–convection interaction within the acinus (Sacin*VT) were therefore recorded, before patients performed spirometry. In children under 6 years old, upper limit of normal (ULN) was calculated based on the equation reported by Lum et al. [16]. For the paediatric age, the cut-off of normality equals to 7.91 was adopted, as recently published [17]. Newly normative data published on LCI Z score were reported as well [17]. An adequate environment with adequate distraction for younger children was assured during each test [14]. Data from earlier software versions were re-run in the version of Spiroware 3.2.2.
Clinical measures
Along with lung function measures, we collected age, sex, genotype and pancreatic status. Nutritional health was expressed as Z score of body mass index (BMI) based on Italian reference equation [18]. Also, we collected presence of CF-related diabetes (CFRD) and colonization by Pseudomonas aeruginosa, which was defined as chronic, intermittent of free [19]. Pulmonary exacerbation was defined as the need for additional antibiotic treatment following change in respiratory signs and symptoms [9, 20]. PEs in the 12 months preceding LCI together with the number of hospitalizations in the previous year due to respiratory symptoms were also used in order to define clusters not only based just on classic features of the disease. For the time-event analysis, we considered PE as an event treated at home or at hospital.
Statistical analysis
Descriptive statistics were used to summarize demographic and clinical features. Difference between continuous or categorical variables were tested with Student’s t or Wilcoxon rank sum test or Fisher test, according to variables distribution.
The agglomerative nesting (AGNES) hierarchical method using Gower’s distance was the approach selected to generate phenotypes, using variables collected throughout the study, the derivatives of MBWN2, namely LCI, Sacin*VT and Scond*VT but not FEV1. To determine the optimal number of clusters, elbow and silhouette methods, gap statistics and the visual inspection of dendrogram were taken into consideration. Additional detail on cluster analysis is provided in the Additional file 1.
We assessed the association between phenotypes and subsequent time to PE using the Prentice, Williams and Peterson (PWP) gap time models [21]. PWP models are an extension of Cox regression models; for every subsequent event, the population at risk includes only those with a previous event. The PWP model was used to evaluate if there is an association between phenotype and number of PEs, calculating hazard ratios (HR) of repeated PE relapses. Since 7% of children had more than three follow-up events, risk set groups were not refined further to avoid unreliable estimates. All statistical tests were performed using the open-source software R Core Team, version 3.6.1 [22].
Results
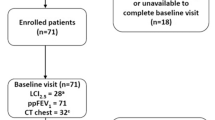
Between October 2014 and September 2019, 313 MBWN2 tests were performed during outpatient clinic visits on 125 children and adolescents with CF, representing the 44.3% (125/282) of eligible CF population at our center.
Cluster characteristics
Table 1 describes the baseline characteristics of the 125 patients evaluated at least twice, grouped by the two clusters found applying AGNES algorithm. Children who performed only one MBWN2 test were excluded (n = 120), since they could not contribute to longitudinal evaluation of phenotypes.
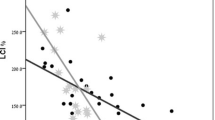
The average age of participants in the two clusters is very similar. Cluster #1 is characterized by the co-presence of several negative known prognostic factors (i.e., pancreatic insufficiency and presence of Pseudomonas aeruginosa). The sole analysis of FEV1%predicted returns all patients in the two clusters in the range of moderate to mild/normal air flow obstruction. Particularly, 90.5% and 100% of patients, respectively in clusters #1 and #2, could be considered having mild/normal FEV1. These percentages vary if one adopts Z score of FEV1, under which case the percentage of patients with a normal lung function drops to 81.1% and to 97.7% in the first and second cluster, respectively. Using MBWN2, ventilation inhomogeneity (i.e., LCI > ULN) characterizes the majority of patients in cluster #1, 92.3% compared to 42.6% in cluster #2. At a population level, 95% Confidence Interval (CI) for the mean LCI in cluster #1 goes from 10.7 to 12.0, whereas 95%CI for the mean LCI in cluster #2 is much lower, namely 7.5–8.4. Acinar and conductive ventilation inhomogeneity is less pronounced in cluster #2 compared to cluster #1. Patients in cluster #1 show also more variability in ventilation inhomogeneity measurements (Fig. 1), whereas patients in cluster #2 look more stable over time. Under these two distinct phenotypic clusters, no sex difference is detectable (P = 0.466) nor any significant difference in nutritional status, − 0.34 (95% CI − 0.65 to 0.03) BMI Z score. Age span is pretty much identical between the two partitions, 5.5–16.8 and 7.7–16.3 years, respectively in clusters #1and #2.
Time to recurrent pulmonary exacerbations in CF phenotypes
Most children had at least one PE (n = 114, 91.2%) during the 4-year follow-up. Mean number of PE was 2.3, varying from 0 to 4. One to 3 relapses of PE occurred in 114, 89, and 28 children, respectively (Table 2).
The clinical characteristics became more severe as patients had more events, as summarized by Table 2, although the percentage of children without Pseudomonas aeruginosa remained stable over time. According to PWP model, the best phenotype was associated with a lower risk of PE relapse (HR 0.45, 95% CI 0.34–0.62). When estimating the association between phenotypes and PE relapse separately for children having experienced one, two or three follow-up PE events, there was no evidence of difference between the different strata (P = 0.102). Overall, the median time with interquartile range to first PE was 0.30 (0.15–0.71) years for children and adolescents in cluster #1 and 1.19 (0.46–2.89) years for patients in cluster #2.
Discussion
In the present study, derivatives of MBWN2 test contributed to characterize phenotypic clusters of children and adolescents with CF in stable conditions. Most interestingly, the association found between relapse of pulmonary exacerbations and phenotypes promotes the importance of LCI when related to the burden of disease, considering how impactful can be pulmonary exacerbations either treated at home or at hospital on children and their families.
Cluster analysis identified two different profiles of patients of the same age, equally represented by boys and girls and without clinically significant difference in nutritional status. Cluster #2 depicts individuals with less severe genotype and better lung status. Interestingly, absence of pancreatic insufficiency uniquely defines individuals in cluster #2. By the contrary, cluster #1 identifies peers with a more severe expression of the disease. The most important aspect to consider is that divergent phenotypes emerged during preadolescence, showing different lung health and a differently compromised lung periphery, only when evaluated by score indices of ventilation inhomogeneity and FEV1 Z score together. This is furthermore of interest, taking into consideration that clustering used information derived by MBWN2 and not by spirometry. Although statistically different between the two clusters, FEV1 remains above 90% predicted. This reinforces its poor sensitivity in discriminating lung health in patients with CF during childhood and adolescence, as already reported elsewhere [2, 23, 24]. The overall compromise of cluster #1 is also supported by the higher prevalence of pulmonary exacerbations compared to cluster #2 and by the absence of hospitalization at all in cluster #2. Practically, children in cluster #1 may be identified at elevated risk, being the target of more personalized interventions. In fact, despite these individuals may present with FEV1 in the normal range, their LCI was higher compared to those of same age who were pancreatic sufficient, thus suggesting that tailored and intensive intervention to also treat lung periphery is appropriate. As commented by Nyilas et al., children with different phenotypes and particularly with distinct ventilation inhomogeneity profiles, may benefit from different therapeutic approaches, such as aerosol therapy performed with distinct devices in order to deliver different particle sizes [25] as well as physiotherapy interventions targeting small or large airways, or different scheduling of follow-up visit. A few cluster-based approaches are reported in the literature about CF [26,27,28,29], and it is worth to be mentioned that adolescence was the time when individuals with rapid FEV1 decline differentiate from other phenotypes characterized by slower lung function decline [26]. Our findings showed divergent phenotypic characteristics already at 11 years old, thus underlying the importance of introducing early markers of lung functional status along the routine CF care. So far, only one study used LCI to define physiological phenotypes in children with different lung diseases, including CF [25], showing how determinant was using MBW test to characterize children with normal and abnormal MBW derivatives.
In the present study, physicians and healthcare staff were not blinded to MBW assessment, therefore it is questionable if the steady trend in LCI observed in our study, especially in children defined by cluster #2, should be attributed to any medical decision and subsequent intervention triggered by the evaluation of LCI during the routine follow-up visits. In a recent study [30], an increase in LCI larger than 1 unit was not associated with increased antimicrobial use or pathogens load over 2-year follow-up based on LCI-triggered bronchoalveolar lavage. However, an increase in LCI over time between 0.24 and 0.29 units/year was just reported [6], suggesting that even small fluctuations may be required to trigger change in the multidisciplinary management of CF, especially in children and adolescents with stable conditions. Thus, it is plausible that such small variations could be currently used in a clinical setting to guide therapies or to require additional assessment. Indeed, it is to be recalled how meaningful was the rescue of MBW test from the armoury of lung function tests in the 2010s CF scenario worldwide. It would not be surprising if higher LCI values than 7—which was considered a standard cut-off of normality back in time—could have opened to clinicians more options in the care of their patients. It is well known that information with a high emotional impact can alter the decisional process, even though the probabilistic rules to guide decisions are already there. Anyway, the observed stability in ventilation inhomogeneity is encouraging for our CF team, especially considering the recent findings from Sandvik et al. [31], showing that no progression of structural lung disease at CT scan is expected in children with stable LCI.
Our findings describe for the first time an association between phenotypes based on ventilation inhomogeneity and the risk of PE relapse in children and adolescents with CF. The conditional model of PWP with gap time particularly fits the data on PEs in CF, since it does not allow to consider an individual at risk until the end of the previous episode.
Earlier, Vermeulen et al. [32] showed an association between baseline LCI and FEV1 and time to first PE in a cohort of 5–19 years old patients with CF. Annual PE rate was higher in children with the worst Z score of LCI and FEV1, however LCI Z score was identified as the only predictor of the PE rate in the 12 months following the baseline assessment. Their methods relied on Kaplan–Meier and Negative Binomial regression, which assume that each patient has recurrent events according to individual Poisson event rate which in turn varies according to a specific distribution across patients. Negative Binomial regression model seems appropriate to estimate recurrent events when information on time is not available [33], differently from the present study, in which we collected the exact time of PE throughout the follow-up. Moreover, the study from Vermeulen et al. used information on PEs up to first event only, potentially leading to an inaccurate evaluation of the association of selected covariates with an event that occurs more than once and that are possibly dependent. However, both these studies show how useful was MBWN2 to capture relevant association with the course of CF disease. Furthermore, these results remind us of the paramount importance to delay the occurrence of PE and to concentrate the efforts of the multidisciplinary team to preserve lung function, especially in terms of ventilation homogeneity in children.
Strength and limitations
Cluster analysis is a multivariate method aimed to classify individuals based on a set of measured variables. By consequence, the variable selection is a crucial step and could have been done differently from the one we are proposing here, which relied on a minimum set of widely available CF clinical characteristics. With regard to phenotypic clusters, further steps should take into consideration the anatomical correlates of CF lung disease to address to each cluster a specific level of anatomical damage. Despite these limitations, our study is characterized by several unique strengths. Not only we generated clusters based on a large cohort of Italian children and adolescents with CF using LCI but also, we adopted an ad-hoc statistical approach to evaluate the association between phenotypes and PE relapses, which are considered high-impactful events in patients and their families’ life, therefore assuming a unique relevance under the patient’s perspective.
Conclusion
LCI is useful in the clinic to characterize ventilation inhomogeneity in distinct phenotypes of children and adolescents with mild/normal FEV1. A less severe phenotype translates into a lower risk of pulmonary exacerbation relapse. Altogether these findings add to the available literature in confirming the clinical utility of MBWN2 to monitor lung disease during childhood and adolescence in CF.
Availability of data and materials
The datasets generated during and analyzed during the current study are not publicly available due to privacy restrictions but are available from the corresponding author on reasonable request.
Abbreviations
- LCI:
-
Lung clearance index
- MBW:
-
Multiple breath washout
- CF:
-
Cystic fibrosis
- PE:
-
Pulmonary exacerbation
- FEV1 :
-
Forced expiratory volume in the first second
- MBWN2 :
-
Nitrogen multiple breath washout
- ULN:
-
Upper limit of normal
- BMI:
-
Body mass index
- CFRD:
-
CF-related diabetes
- AGNES:
-
Agglomerative nesting
- PWP:
-
Prentice, Williams and Peterson
- IQR:
-
Interquartile range
- CI:
-
Confidence interval
References
Aurora P, Bush A, Oliver C, Wallis C, Price J, Stroobant J, et al. Multiple-breath washout as a marker of lung disease in preschool children with cystic fibrosis. Am J Respir Crit Care Med. 2005;171(3):249–56.
Gustafsson PM, Aurora P, Lindblad A. Evaluation of ventilation maldistribution as an early indicator of lung disease in children with cystic fibrosis. Eur Respir J. 2003;22:972–9.
Davies JC, Sermet-Gaudelus I, Naehrlich L, Harris RS, Campbell D, Ahluwalia N, et al. A phase 3, double-blind, parallel-group study to evaluate the efficacy and safety of tezacaftor in combination with ivacaftor in participants 6 through 11 years of age with cystic fibrosis homozygous for F508del or heterozygous for the F508del-CFTR mutati. J Cyst Fibros. 2021;20(1):68–77.
Milla CE, Ratjen F, Marigowda G, Liu F, Waltz D, Rosenfeld M. Lumacaftor/ivacaftor in patients aged 6–11 years with cystic fibrosis and homozygous for F508del-CFTR. 2017.
Ratjen F, Hug C, Marigowda G, Tian S, Huang X, Stanojevic S, et al. Efficacy and safety of lumacaftor and ivacaftor in patients aged 6–11 years with cystic fibrosis homozygous for F508del-CFTR : a randomised, placebo-controlled phase 3 trial. Lancet Respir Med. 2017;5(7):557–67.
Frauchiger BS, Binggeli S, Yammine S, Spycher B, Krüger L, Ramsey KA, et al. Longitudinal course of clinical lung clearance index in children with cystic fibrosis. Eur Respir J. 2021;58(1):2002686.
Short C, Saunders C, Davies JC. Utility of lung clearance index in CF: what we know, what we don’t know and musings on how to bridge the gap. J Cyst Fibros. 2020;19(6):852–5.
Spano J, Milla CE. Defining the clinical utility of the lung clearance index. Are we there yet? Am J Respir Crit Care Med. 2021;203(8):937–9.
Bilton D, Canny G, Conway S, Dumcius S, Hjelte L, Proesmans M, et al. Pulmonary exacerbation: towards a definition for use in clinical trials. Report from the EuroCareCF Working Group on outcome parameters in clinical trials. J Cyst Fibros. 2011;10:S79-81.
Graham BL, Steenbruggen I, Barjaktarevic IZ, Cooper BG, Hall GL, Hallstrand TS, et al. Standardization of spirometry 2019 update an official American Thoracic Society and European Respiratory Society technical statement. Am J Respir Crit Care Med. 2019;200(8):E70-88.
Quanjer PH, Stanojevic S, Cole TJ, Baur X, Hall GL, Culver BH, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J. 2012;40(6):1324–43.
Jensen R, Green K, Gustafsson P, Latzin P, Pittman J, Ratjen F, et al. Standard operating procedure: multiple breath nitrogen washout. 2013. http://www.mbwtraining.com/ECFS_MBW_SOP.pdf.
Robinson PD, Latzin P, Verbanck S, Hall GL, Horsley A, Gappa M, et al. Consensus statement for inert gas washout measurement using multiple- and single-breath tests. Eur Respir J. 2013;41(3):507–22.
Robinson PD, Latzin P, Ramsey KA, Stanojevic S, Aurora P, Davis SD, et al. Preschool multiple-breath washout testing. An official American thoracic society technical statement. Am J Respir Crit Care Med. 2018;197(5):e1-19.
Jensen R, Stanojevic S, Klingel M, Pizarro ME, Hall GL, Ramsey K, et al. A systematic approach to multiple breath nitrogen washout test quality. PLoS ONE. 2016;11(6):e0157523.
Lum S, Stocks J, Stanojevic S, Wade A, Robinson P, Gustafsson P, et al. Age and height dependence of lung clearance index and functional residual capacity. Eur Respir J. 2013;41(6):1371–7.
Anagnostopoulou P, Latzin P, Jensen R, Stahl M, Harper A, Yammine S, et al. Normative data for multiple breath washout outcomes in school-aged Caucasian children. Eur Respir J. 2020;55(4):1901302.
Cacciari E, Milani S, Balsamo A, Spada E, Bona G, Cavallo L, et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J Endocrinol Investig. 2006;29(7):581–93.
Lee TWR, Brownlee KG, Conway SP, Denton M, Littlewood JM. Evaluation of a new definition for chronic Pseudomonas aeruginosa infection in cystic fibrosis patients. J Cyst Fibros. 2003;2(1):29–34.
Ng C, Nadig T, Smyth AR, Flume P. Treatment of pulmonary exacerbations in cystic fibrosis. Curr Opin Pulm Med. 2020;26(6):679–84.
Prentice RL, Williams BJ, Peterson AV. On the regression analysis of multivariate failure time data. Biometrika. 1981;68(2):373–9.
R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019.
Ramsey KA, Rosenow T, Turkovic L, Skoric B, Banton G, Adams AM, et al. Lung clearance index and structural lung disease on computed tomography in early cystic fibrosis. Am J Respir Crit Care Med. 2016;193(1):60–7.
Aurora P, Gustafsson P, Bush A, Lindblad A, Oliver C, Wallis CE, et al. Multiple breath inert gas washout as a measure of ventilation distribution in children with cystic fibrosis. Thorax. 2004;59:1068–73.
Nyilas S, Singer F, Kumar N, Yammine S, Meier-Girard D, Koerner-Rettberg C, et al. Physiological phenotyping of pediatric chronic obstructive airway diseases. J Appl Physiol. 2016;121(1):324–32.
Szczesniak RD, Li D, Su W, Brokamp C, Pestian J, Seid M, et al. Phenotypes of rapid cystic fibrosis lung disease progression during adolescence and young adulthood. Am J Respir Crit Care Med. 2017;196(4):471–8.
Hafen GM, Hurst C, Yearwood J, Smith J, Dzalilov Z, Robinson PJ. A new scoring system in cystic fibrosis: statistical tools for database analysis—a preliminary report. BMC Med Inform Decis Mak. 2008;8:1–11.
Conrad DJ, Bailey BA. Multidimensional clinical phenotyping of an adult cystic fibrosis patient population. PLoS ONE. 2015;10(3):1–14.
Filipow N, Davies G, Main E, Sebire NJ, Wallis C, Ratjen F, et al. Unsupervised phenotypic clustering for determining clinical status in children with cystic fibrosis. Eur Respir J. 2021;58(2):2002881.
Voldby C, Green K, Kongstad T, Ring AM, Sandvik RM, Skov M, et al. Lung clearance index-triggered intervention in children with cystic fibrosis—a randomised pilot study. J Cyst Fibros. 2020;19(6):934–41.
Sandvik RM, Kongstad T, Green K, Voldby C, Buchvald F, Skov M, et al. Prospective longitudinal association between repeated multiple breath washout measurements and computed tomography scores in children with cystic fibrosis. J Cyst Fibros. 2021;20(4):632–40.
Vermeulen F, Proesmans M, Boon M, Havermans T, De Boeck K. Lung clearance index predicts pulmonary exacerbations in young patients with cystic fibrosis. Thorax. 2013;69:1–4.
Yadav CP, Sreenivas V, Khan M, Pandey R. An overview of statistical models for recurrent events analysis: a review. Epidemiology. 2018;8(4):354.
Acknowledgements
The authors acknowledge support from the University of Milan through the APC initiative.
Funding
None.
Author information
Authors and Affiliations
Contributions
SG: Conceptualization, Methodology, Formal analysis, Writing—Original Draft; FA: Formal analysis, Writing—Review and Editing; FC: Software, Investigation, Data Curation; LM: Investigation, Data Curation; MR: Investigation, Writing—Review and Editing; AB: Software, Investigation, Supervision; CC: Resources, Supervision, Writing—Review and Editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was designed according to the principles of the Declaration of Helsinki (October 2013) and other guidelines, regulations, and Acts such as Good Clinical Practice. Written, informed consent signed by parents or guardians of the child was obtained. The study has been approved by local ethics committee of Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico, Milan, Italy (456/2021).
Consent for publication
Anonymity is not compromised as data are presented in this manuscript.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Validity and stability indices and other descriptive clusters properties.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gambazza, S., Ambrogi, F., Carta, F. et al. Lung clearance index to characterize clinical phenotypes of children and adolescents with cystic fibrosis. BMC Pulm Med 22, 122 (2022). https://doi.org/10.1186/s12890-022-01903-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-022-01903-5