Abstract
Background
Allergic bronchopulmonary aspergillosis (ABPA) is a bronchopulmonary disease caused by a complex hypersensitivity to Aspergillus and is usually associated with underlying respiratory diseases such as asthma or cystic fibrosis. Mucus plugging can lead to segmental or lobar atelectasis, but complete lung atelectasis has been exceptionally reported in the literature, making it difficult to diagnose. The diagnosis of ABPA may however be suggested in patients without known predisposing respiratory disorder, even in the absence of other relevant radiographic findings.
Case presentation
We report five cases of total unilateral lung collapse secondary to ABPA in 70–81-year-old women. Two of them had a past history of ABPA, while total unilateral lung collapse was the first sign of the disease in the other three patients, contributing to the initial misdiagnosis. Flexible bronchoscopy was initially performed to remove mucus plugs from the obstructed airways but was inefficient in four cases. Corticosteroid and/or antifungal treatment was needed.
Conclusion
ABPA can cause total unilateral lung collapse even in patients without known underlying chronic respiratory disease, making the diagnosis difficult. Flexible bronchoscopy should be considered when lung collapse is associated with respiratory distress but corticosteroids are the mainstay treatment for ABPA.
Similar content being viewed by others
Background
Allergic bronchopulmonary aspergillosis (ABPA) is an immune-mediated inflammatory disease resulting from a complex hypersensitivity reaction to bronchial colonization by Aspergillus spp. [1]. It can be defined as an aberrant immune response against Aspergillus leading to a lymphocyte response and to immediate immunoglobulin E (IgE)-mediated hypersensitivity to Aspergillus [2]. It is the most common Aspergillus-related disorder and usually affects patients with a preexisting respiratory disorder such as asthma or cystic fibrosis [3,4,5]. The radiographic findings associated with ABPA usually include proximal or distal mucoid impaction, pulmonary infiltrates or condensations, and centrolobular nodules [6,7,8]. Mucus plugs can lead to segmental or lobar atelectasis, and are more often described in the literature [6,7,8]. However, complete lung atelectasis due to ABPA is extremely rare with only a few cases reported in the literature [9,10,11,12,13,14,15,16], so that specific therapeutic guidelines are lacking.
Here, we reported five cases of total unilateral lung collapse caused by ABPA in patients without known respiratory disorders. All the patients were hospitalized in Nantes University Hospital (‘CHU Nantes’), France. In this series, the International Society for Human and Animal Mycology (ISHAM) Working Group criteria [17] and the new clinical diagnostic criteria for ABPA/allergic bronchopulmonary mycosis (ABPM) proposed by Asano et al [18] were used to make the diagnosis of ABPA. The optimal management of these patients was discussed, based on our own experience and on the description of other cases reported since 1982, and we raised specialists’ awareness about this uncommon presentation of ABPA that may be life-threatening in case of respiratory distress.
A literature review was performed in January 2021. The terms “aspergillosis”, “ABPA”, “lung collapse” and “atelectasis” were searched in PubMed. Clinical reports of cases of total unilateral lung collapse secondary to ABPA were included.
Case presentation
Case 1
A 70-year-old woman without any past history of asthma or cystic fibrosis had been diagnosed with ABPA in 1999. In April 2008, she presented with dry and non-productive cough associated with increased dyspnea. The laboratory tests showed a normal eosinophil count (210/mm3), normal C-reactive protein (CRP) levels, total IgE levels increased from 200 to 791 kU/L, elevated Aspergillus fumigatus-specific IgE levels (8.05 kU/L) and positive results for Aspergillus fumigatus precipitins (4 precipitin bands). Chest imaging showed total collapse of the left lung.
Flexible bronchoscopy was performed twice but failed to completely remove all bronchial mucus plugs. The analysis of the collected mucus plugs allowed detecting Aspergillus fumigatus in both direct examination and culture. The patient was treated with corticosteroids for six weeks and itraconazole for six months. One month later, the clinical presentation was improved and the chest X-ray was normalized. Disease remission was maintained and she did not experience any recurrent exacerbation to date.
Case 2
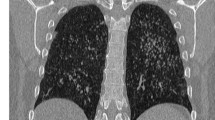
A 74-year-old woman without any significant history of pulmonary disease reported cough and rhinorrhea since last winter. In June 2013, she complained of productive cough and very thick sputum associated with left chest pain, anorexia and asthenia. No improvement was noted after two lines of antibiotics, so that a chest X-ray was performed and showed total collapse of the left lung (Fig. 1A). The thoracic computed tomography (CT) scan showed bronchiectasis, a mucus plug in the middle lobe and mucus plugs in the left central bronchus. Laboratory tests showed hypereosinophilia (2500/mm3), elevated total IgE levels (3364 kU/L) and positive results for Aspergillus fumigatus-specific IgG (94 kUA/L) and IgE (62.6 kU/L). The skin prick test to Aspergillus fumigatus antigen was positive.
The patient underwent flexible bronchoscopy that failed to remove the mucus plugs. Medical treatment with corticosteroids was initiated and itraconazole was also given for 9 months. After 10 days of corticosteroids, flexible bronchoscopy was repeated and numerous plugs were aspirated. The chest X-ray was normalized (Fig. 1B). Aspergillus fumigatus was found in the endoscopic samples. A home environment assessment showed a damp house with high concentrations of Aspergillus fumigatus. To date, the patient did not report any recurrent exacerbation.
Case 3
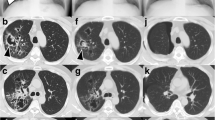
A 73-year-old woman without underlying pulmonary disease complained of asthenia with chronic cough for several months and expectoration of dark brown mucus plugs. Due to the absence of improvement after two lines of antibiotics, a chest CT scan was performed and revealed total left lung collapse in the absence of other findings consistent with ABPA in October 2014.
Initial flexible bronchoscopy revealed a tumor that could not be mobilized in the left bronchus, suggesting an underlying lung cancer. One week later, rigid bronchoscopy allowed removing a giant mucus plug and the atelectasis (Fig. 2). It contained numerous Charcot-Leyden crystals and septate hyphae. Total IgE and Aspergillus fumigatus-specific IgE levels (406 kU/L and 10.3 kUA/L, respectively) were elevated. The results for Aspergillus fumigatus-specific IgG were negative and the eosinophil count was moderately high (800/mm3). One month later, chest radiography was normalized. The patient was treated with itraconazole but treatment was discontinued 2 months later due to the occurrence of hepatic cytolysis. Oral corticosteroids were resumed for 6 weeks. The patient did not experience any recurrent exacerbation thereafter.
Case 4
A 72-year-old woman without any underlying pulmonary disorder was diagnosed with ABPA in 1998. Her last exacerbation occurred in 2008. In December 2016, she experienced dry cough for 1 month with no improvement after two lines of antibiotics. A chest X-ray was performed and showed complete atelectasis of the left lung and tram-track opacities in the right lower field (Fig. 1C). Total IgE and Aspergillus fumigatus-specific IgE levels (2442 kU/L and 56.6 kUA/L, respectively) were elevated. The results for Aspergillus fumigatus-specific IgG were positive and the eosinophil count were negative while oral corticosteroids were initiated a few days earlier.
Flexible bronchoscopy showed a large mucus plug that was partially removed after suction. Aspergillus fumigatus was found in the endoscopic samples. Itraconazole and corticosteroids were initiated. A few days later, the symptoms worsened, resulting in respiratory distress for which intubation and mechanic ventilation were needed. Flexible bronchoscopy was repeated and the use of a cryoprobe to freeze the plug allowed its removal. Medical treatment was continued and the patient was rapidly extubated. Two months later, she reported a significant improvement in cough and the chest X-ray showed a full resolution (Fig. 1D).
Case 5
An 81-year-old former smoker woman was followed since 2013 for chronic bronchitis with respiratory symptoms, including wheezing. She was hospitalized in December 2020 for productive cough and dyspnea for over a week. A chest X-ray showed total right lung collapse (Fig. 1E). Based on her smoking history, a lung cancer was first suspected. A CT scan was performed and showed pulmonary embolism and confirmed the presence of right lung atelectasis due to the right main bronchus obstruction without any other finding supporting an underlying neoplastic process (Fig. 3). Her condition deteriorated rapidly with respiratory distress for which emergency flexible bronchoscopy was needed. Bronchoscopy showed that the right main bronchus was obstructed by a thick and large mucus plug that could be completely removed. Her condition improved rapidly thereafter and chest radiography no longer showed atelectasis (Fig. 1F). Total IgE and Aspergillus fumigatus-specific IgE levels (2464 kU/L and 71.5 kUA/L, respectively) were elevated. The results for Aspergillus fumigatus-specific IgG were negative and the eosinophil count was high (1009/mm3). Aspergillus fumigatus was found in the mucus plug. She was treated with systemic corticosteroids.
Discussion and conclusions
ABPA may present as an acute respiratory distress secondary to lung collapse [9,10,11,12,13,14]. Mucoid impaction may obstruct the lobar bronchi, leading to the finger-in-glove sign with lobar atelectasis seen on chest radiography. Lobar or segmental lung collapses have been described in 14–39% of patients with ABPA [6,7,8]. Our study showed that total lung collapse could also be a manifestation of ABPA although it is less frequently reported in the literature [9,10,11,12,13,14,15,16].
Interestingly, our cases were exclusively elderly women. However, no correlation has been reported between ABPA and the sex or age [19]. Moreover, 6 out of the 11 cases of total unilateral atelectasis described in the literature are male patients aged 6–74 years old [9, 10, 13, 15].
Not all of our five cases of total lung collapse due to ABPA met the criteria for ABPA, according to the latest definition of the ISHAM Working group [17] (Table 2). Indeed, total and specific IgE levels greater than 1000 IU/mL and 0.35 kUA/L, respectively, are both considered essential criteria [20, 21]. Agarwal et al. have found that only 39% of patients with ABPA met at least 7 out of the 8 components of the Rosenberg-Patterson criteria, including total serum IgE elevated, more than 1000 IU/mL [22]. In two out of our five cases, the total IgE levels were less than this threshold, as well as in two cases reported in the literature (Table 1). However, the relevance of the 1000 IU/mL threshold has been discussed by Saxena et al. A total IgE level greater than 500 IU/mL has been identified as an essential criteria associated with an improved diagnostic performance [23]. Moreover, if we used Asano et al. criteria for ABPA/ABPM [18] that have shown better sensitivity and specificity for the diagnosis of ABPA compared to the Rosenberg and Patterson criteria and to the ISHAM criteria, especially in atypical cases without asthma, all our patients could be considered as definite or probable cases of ABPA (Table 2).
Although cystic fibrosis and asthma are the main respiratory conditions usually associated with ABPA [3, 4], none of our patients had a significant history of respiratory disease or atopy. Our observation is consistent with the few cases of total unilateral atelectasis described in the literature and summarized in Table 1: only 6 out of the 11 patients had a significant respiratory history. Interestingly, in a cohort of 530 patients, Muthu et al. have suggested two phenotypes of ABPA defined according to the status of asthma (yes/no). Patients with ABPA and asthma were more symptomatic, experienced more exacerbations and had a worse lung function [20]. As reported in the study by Glancy et al., in which 11 out of the 42 patients with allergic broncho-pulmonary fungal diseases did not have clinical asthma, the absence of an underlying respiratory condition made it difficult to establish the diagnosis of ABPA [24]. Patients sometimes underwent surgery before the diagnosis of ABPA could be made, in particular when a tumor was initially suspected.
In this context, the diagnosis of ABPA may be supported by the presence of typical radiologic findings. The most common CT-scan findings are mucoid impactions and bronchiectasis predominantly involving the segmental and subsegmental bronchi of the upper lobes, with centrilobular nodules [6,7,8]. In case of total unilateral lung collapse, these imaging findings should be investigated in the contralateral lung. A CT scan was performed in three of our patients. Unfortunately, only one had imaging findings consistent with ABPA in the contralateral lung that could have guided the diagnosis. In the other cases, bronchoscopy was first performed rather than a CT scan because the clinical and biological findings strongly suggested the diagnosis of ABPA, especially in the two patients with a history of ABPA.
The diagnosis of ABPA is always challenging in patients with total lung collapse, in the absence of a preexisting respiratory condition and other characteristic findings on the CT scan. Many criteria have been proposed over the years with different diagnostic algorithms [17, 25, 26] but there is a lack of consensus for standardized criteria. When a patient present with total lung collapse associated with clinical and biological findings consistent with ABPA, we recommend to use the 10-component diagnostic criteria for ABPA/ABPM proposed by Asano et al. [18]. Flexible bronchoscopy should be considered when lung collapse is associated with respiratory distress, with the objective of removing obstructive mucus plugs. Besides, the endoscopic aspect of the mucus may be helpful for the diagnosis, and Asano et al. have retained this criterion in their recent criteria for ABPA/ABPM. Interestingly, the use of a cryoprobe may increase the likelihood of successfully removing the plugs, as shown here in one patient.
In addition, the microscopic analysis of the plugs could be the cornerstone of the diagnosis of ABPA. Cytologic findings associate necrotic eosinophils, Charcot Leyden crystals, small numbers of degenerating fungal hyphae, and eosinophil-rich inflammation with isolation of Aspergillus spp. in the fungal culture [27]. Nevertheless, flexible bronchoscopy is usually associated with limited success, as shown in our cases. Even if therapeutic rigid bronchoscopy could be another option, the endoscopic removal of the mucus plugs was inefficient in 4 out of our 5 cases. In this situation, additional drug treatment is often needed, such as systemic corticosteroids that suppress the inflammatory activity and Aspergillus hypersensitivity [3, 21]. Corticosteroids alone could be sufficient but repeated bronchoscopy may be required once corticosteroids have been initiated. Prolonged therapy is often needed [24]. To limit glucocorticoid-related adverse effects, itraconazole may also be used [28]. Itraconazole was used in combination with steroids as a first-line treatment in 4 out of our 5 patients to achieve a steroid-sparing effect and to decrease the fungal load. As described by Agarwal et al., itraconazole alone may be considered for the management of acute ABPA, and we used it in one patient (case 3) [19]. Other azoles may be proposed as a second line but Aspergillus susceptibility to azoles needs to be assessed to choose the optimal treatment. Lastly, a home visit performed by a medical indoor environment counselor is helpful to identify the source of exposure and to provide advice to reduce Aspergillus exposure [29, 30].
In conclusion, ABPA can cause total unilateral lung collapse even in patients without underlying chronic respiratory disease, making the diagnosis challenging. Initial flexible bronchoscopy may fail to completely remove the mucus plugs but seems essential in case of respiratory distress. It is very helpful to make the diagnosis (typical aspect of the mucus plugs) and to rule out other conditions, especially a lung cancer. Medical treatment with corticosteroids should be initiated early to suppress immune hyperreactivity although well-designed trials using steroids in ABPA are lacking. However, rigid bronchoscopy should be considered in the second line and the use of a cryobiopsy probe may be helpful to rapidly remove large plugs.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ABPA:
-
Allergic bronchopulmonary aspergillosis
- ABPM:
-
Allergic bronchopulmonary mycosis
- Af:
-
Aspergillus fumigatus
- BW:
-
Bronchial wash
- CT:
-
Computed tomography
- CRP:
-
C-reactive protein
- EC:
-
Eosinophil count
- FB:
-
Flexible bronchoscopy
- IgE:
-
Immunoglobulin E
- LABA:
-
Long-acting beta2-agonists
- MD:
-
Missing data
- RB:
-
Rigid bronchoscopy
References
Agarwal R. Allergic bronchopulmonary aspergillosis. Chest. 2009;135(3):805–26. https://doi.org/10.1378/chest.08-2586.
Moss RB. Pathophysiology and immunology of allergic bronchopulmonary aspergillosis. Med Mycol. 2005;43(Suppl 1):S203-206. https://doi.org/10.1080/13693780500052255.
Maturu VN, Agarwal R. Prevalence of Aspergillus sensitization and allergic bronchopulmonary aspergillosis in cystic fibrosis: systematic review and meta-analysis. Clin Exp Allergy. 2015;45(12):1765–78. https://doi.org/10.1111/cea.12595.
Denning DW, Pleuvry A, Cole DC. Global burden of allergic bronchopulmonary aspergillosis with asthma and its complication chronic pulmonary aspergillosis in adults. Med Mycol. 2013;51(4):361–70. https://doi.org/10.3109/13693786.2012.738312.
Agarwal R, Aggarwal AN, Gupta D, Jindal SK. Aspergillus hypersensitivity and allergic bronchopulmonary aspergillosis in patients with bronchial asthma: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2009;13(8):936–44.
McCarthy DS, Simon G, Hargreave FE. The radiological appearances in allergic broncho-pulmonary aspergillosis. Clin Radiol. 1970;21(4):366–75. https://doi.org/10.1016/s0009-9260(70)80070-8.
Greene R. The radiological spectrum of pulmonary aspergillosis. Med Mycol. 2005;43(Suppl 1):S147-154. https://doi.org/10.1080/13693780500064771.
Garg MK, Sharma M, Agarwal R, et al. Allergic bronchopulmonary aspergillosis: all a radiologist needs to know. Curr Pediatr Rev. 2016;12(3):179–89. https://doi.org/10.2174/1573396312666160831143951.
Berkin KE, Vernon DR, Kerr JW. Lung collapse caused by allergic bronchopulmonary aspergillosis in non-asthmatic patients. Br Med J Clin Res Ed. 1982;285(6341):552–3. https://doi.org/10.1136/bmj.285.6341.552.
Nomura K, Sim JJ, Yamashiro Y, et al. Total collapse of the right lung in a patient with allergic bronchopulmonary aspergillosis. Nihon Kokyuki Gakkai Zasshi. 1998;36(5):469–72.
Agarwal R, Aggarwal AN, Gupta N, Gupta D. A rare cause of acute respiratory failure—allergic bronchopulmonary aspergillosis. Mycoses. 2011;54(4):e223–7. https://doi.org/10.1111/j.1439-0507.2009.01830.x.
Braude S, Bowen D. Allergic bronchopulmonary aspergillosis: a reversible cause of complete lung collapse. Intern Med J. 2011;41(10):754–5. https://doi.org/10.1111/j.1445-5994.2011.02573.x.
Kumar R, Poongadan MN, Singh M. Allergic bronchopulmonary aspergillosis presenting as lobar or total lung collapse. Pneumonol Alergol Pol. 2015;83(2):144–50. https://doi.org/10.5603/PiAP.2015.0023.
Ghosh K, Sanders BE. Allergic bronchopulmonary aspergillosis causing total lung collapse. Case Rep. 2012;2012:bcr1220115349–bcr1220115349. https://doi.org/10.1136/bcr.12.2011.5349.
Brueton MJ, Ormerod LP, Shah KJ, Anderson CM. Allergic bronchopulmonary aspergillosis complicating cystic fibrosis in childhood. Arch Dis Child. 1980;55(5):348–53. https://doi.org/10.1136/adc.55.5.348.
Bhagat R, Shah A, Jaggi OP, Khan ZU. Concomitant allergic bronchopulmonary aspergillosis and allergic Aspergillus sinusitis with an operated aspergilloma. J Allergy Clin Immunol. 1993;91(5):1094–6. https://doi.org/10.1016/0091-6749(93)90224-4.
Agarwal R, Chakrabarti A, Shah A, et al. Allergic bronchopulmonary aspergillosis: review of literature and proposal of new diagnostic and classification criteria. Clin Exp Allergy. 2013;43(8):850–73. https://doi.org/10.1111/cea.12141.
Asano K, Hebisawa A, Ishiguro T, et al. New clinical diagnostic criteria for allergic bronchopulmonary aspergillosis/mycosis and its validation. J Allergy Clin Immunol. 2021;147(4):1261-1268.e5. https://doi.org/10.1016/j.jaci.2020.08.029.
Agarwal R, Sehgal IS, Dhooria S, et al. Allergic bronchopulmonary aspergillosis. Indian J Med Res. 2020;151(6):529–49. https://doi.org/10.4103/ijmr.IJMR_1187_19.
Shah A, Panjabi C. Allergic aspergillosis of the respiratory tract. Eur Respir Rev. 2014;23(131):8–29. https://doi.org/10.1183/09059180.00007413.
Agarwal R, Sehgal IS, Dhooria S, Aggarwal AN. Developments in the diagnosis and treatment of allergic bronchopulmonary aspergillosis. Expert Rev Respir Med. 2016;10(12):1317–34. https://doi.org/10.1080/17476348.2016.1249853.
Agarwal R, Maskey D, Aggarwal AN, et al. Diagnostic performance of various tests and criteria employed in allergic bronchopulmonary aspergillosis: a latent class analysis. PLoS ONE. 2013;8(4): e61105. https://doi.org/10.1371/journal.pone.0061105.
Saxena P, Choudhary H, Muthu V, et al. Which are the optimal criteria for the diagnosis of allergic bronchopulmonary aspergillosis? A latent class analysis. J Allergy Clin Immunol Pract. 2020. https://doi.org/10.1016/j.jaip.2020.08.043.
Glancy JJ, Elder JL, McAleer R. Allergic bronchopulmonary fungal disease without clinical asthma. Thorax. 1981;36(5):345–9. https://doi.org/10.1136/thx.36.5.345.
Rosenberg M, Patterson R, Mintzer R, Cooper BJ, Roberts M, Harris KE. Clinical and immunologic criteria for the diagnosis of allergic bronchopulmonary aspergillosis. Ann Intern Med. 1977;86(4):405–14. https://doi.org/10.7326/0003-4819-86-4-405.
Greenberger PA. When to suspect and work up allergic bronchopulmonary aspergillosis. Ann Allergy Asthma Immunol. 2013;111(1):1–4. https://doi.org/10.1016/j.anai.2013.04.014.
Chen KT. Cytology of allergic bronchopulmonary aspergillosis. Diagn Cytopathol. 1993;9(1):82–5. https://doi.org/10.1002/dc.2840090118.
Agarwal R, Dhooria S, Singh Sehgal I, et al. A randomized trial of itraconazole vs prednisolone in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Chest. 2018;153(3):656–64. https://doi.org/10.1016/j.chest.2018.01.005.
Kraemer JP, Ott M, Kopferschmitt MC, et al. Usefulness of an environmental advisor in a case of invasive pulmonary aspergillosis. Rev Mal Respir. 2004;21(1):165–7. https://doi.org/10.1016/S0761-8425(04)71252-8.
Radin RC, Greenberger PA, Patterson R, Ghory A. Mould counts and exacerbations of allergic bronchopulmonary aspergillosis. Clin Allergy. 1983;13(3):271–5. https://doi.org/10.1111/j.1365-2222.1983.tb02598.x.
Acknowledgements
Not applicable.
Funding
No financial support and sponsorship.
Author information
Authors and Affiliations
Contributions
NB and SD conceived the study, performed the literature review and analysis, and drafted the manuscript. PG, AC, TP, MR, TM, FC, and LC treated the patients and performed the analysis. CD analyzed the CT scans and performed the analysis. CS and FXB revised the manuscript critically. All authors read and approved the submitted manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent to publication
Written informed consent for the publication of these case reports and associated images was obtained from all patients.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Benkalfate, N., Dirou, S., Germaud, P. et al. Total unilateral pulmonary collapse secondary to allergic bronchopulmonary aspergillosis: a case series of an unusual cause of complete atelectasis. BMC Pulm Med 21, 425 (2021). https://doi.org/10.1186/s12890-021-01789-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-021-01789-9