Abstract
Background/objectives
Assessment of Health-Related Quality of Life (HRQL) in patients with chronic respiratory insufficiency requiring Home Mechanical Ventilation (HMV) requires a valid measurement tool. The Severe Respiratory Insufficiency (SRI) questionnaire, originally developed in German, has been translated into different languages and tested in different contexts, but has so far not been in use in Arabic-speaking populations. The objective of this study is to validate the Arabic version of the SRI questionnaire in a sample of Arabic-speaking patients from Lebanon.
Methods
Following forward/backward translations, the finalized Arabic version was administered to 149 patients (53 males–96 females, age 69.80 ± 10 years) receiving HMV. Patients were recruited from outpatient clinics and visited at home. The Arabic SRI and the 36-Item Short-Form Health Survey (SF-36) were administered, in addition to questions on sociodemographics and medical history. Exploratory Factor Analysis (EFA) was used to explore dimensionality; internal consistency reliability of the unidimensional scale and its subscales was assessed using Cronbach’s alpha. External nomological validity was examined by assessing the correlation between the SRI and SF-36 scores.
Results
The 49-item Arabic SRI scale showed a high internal consistency reliability (Cronbach alpha for the total scale was 0.897 and ranged between 0.73 and 0.87 for all subscales). Correlations between the SF-36-Mental Health Component MHC and SF-36-Physical Health Component with SRI-Summary Scale were 0.57 and 0.66, respectively, with higher correlations observed between the SF-36 and specific sub-scales such as the Physical Functioning and the Social Functioning subscales [r = 0.81 and r = 0.74 (P < 0.01), respectively].
Conclusion and recommendations
The Arabic SRI is a reliable and valid tool for assessing HRQL in patients with chronic respiratory insufficiency receiving home mechanical ventilation.
Similar content being viewed by others
Introduction
Health-related quality of life (HRQL), which is comprised of various health components related to functional capabilities, physical conditions, psychological well-being, and social functioning, is a key component of evaluating outcomes of clinical practice and medical interventions [1, 2]. Several tools have been developed and used to assess HRQL, particularly for patients with chronic conditions, including the Sickness Impact Profile [3] and the 36-Item Short-Form Health Survey (SF-36) [4]. These tools, however, examine the general health status regardless of the underlying disease. In the field of pulmonary medicine, disease-specific scales have been developed and validated, and these include the Chronic Respiratory Disease Questionnaire [5] and the St. George’s Respiratory Questionnaire [6] both of which assess fastidious issues related to patients with chronic obstructive pulmonary disease (COPD).
Patients with chronic respiratory insufficiencies, whether caused by obstructive (i.e. COPD) or restrictive ventilatory disorders (i.e. neuromuscular diseases (NMD), restrictive chest wall disorders (RWCD), lung fibrosis, or obesity hypoventilation syndrome (OHS)) are of special medical concern as they represent a unique group given the severe limitations and comorbid effects of their respiratory health. One main intervention for these patients is non-invasive home mechanical ventilation (HMV) that is mostly delivered via a nasal or facial mask. Despite HMV’s proven benefits in improving clinical and physiological parameters specific to patients with severe respiratory insufficiency [7,8,9,10,11,12], the continued monitoring of the quality of life of these patients remains crucial to assess the impact of disease progression or effect of treatment regimen on daily life [13]. Evaluation of their quality of life has been typically done using the aforementioned generic and other disease-specific scales [10, 14,15,16]. Yet, these scales lack proper assessment of the important characteristics and specific symptoms exclusive to this patient population leading to an imperfect evaluation of their quality of life [14, 17]. For this reason, the Severe Respiratory Insufficiency (SRI) questionnaire was developed by German researchers to assess central aspects relevant to this patient population [17]. The original SRI, a multidimensional HRQL tool with high reliability [17], has been translated into different languages (e.g. English, Spanish, Norway, Japanese, Chinese, Greek, Hungarian, Portuguese, and French) and tested in different contexts [18,19,20,21,22,23, 26,27,28], but notably not in any Arabic-speaking populations of the Arab world. It is worth noting that Arabic is the official language in 27 countries that constitute the Arab League, and the co-official language in 6 additional states [29, 30]. The aim of the current study is to validate an Arabic version of the SRI among patients with chronic respiratory insufficiency.
Methods
Patients and study design
Following ethical approval obtained from the Institutional Review Board at the American University of Beirut, a convenient sample of 149 adult patients with chronic respiratory insufficiency receiving HMV was identified and recruited on a rolling basis from clinics specialized in pulmonary medicine until the minimum desired sample size was met based on a 3 subjects per variable recommendation [31, 32]. Patients were recruited across all of Lebanon between March 2016 and May 2018. All patients receiving HMV and clinically stable for more than one month before enrolment were eligible for the study. Patients with a tracheostomy tube, a history of left-sided congestive failure and an exacerbation during the preceding month were not eligible to participate. Eligible patients were initially approached by their attending physicians who explained the objectives of the study and took their approval to be contacted by the research team. Patients were then contacted over the phone by the research team for informed oral consent to participate in the study and for eligibility screening. Consenting eligible patients were visited in their homes for face-to-face interviews.
Measures
SRI scale
The SRI scale is a multidimensional instrument comprised of 49 items, and seven subscales including: Respiratory Complaints (SRI-RC), Physical Functioning (SRI-PF), Attendant Symptoms and Sleep (SRI-AS), Social Relationships (SRI-SR), Psychologic Well-being (SRI-WB), Anxiety (SRI-AX) and Social Functioning (SRI-SF). The SRI questionnaire assesses the patients’ quality of life during the preceding one week based on his/her level of agreement rated using a five Likert-scale from “strongly agree” to “strongly disagree”. Typically, subscale scores are generated or a total scale score is generated (SRI-SS) yielding a score ranging between 0 and 100, with higher scores indicating a better quality of life.
SF36
The Arabic SF-36 item scale was administered to measure the general quality of life among our sample. The SF‐36 consists of eight subscales measuring diverse components of health status with a score ranging between 0 and 100; with higher scores indicating better health. The eight subscales are the following: SF‐36‐PF = Physical Functioning; SF‐36‐RP = Role Physical; SF‐36‐BP = Bodily Pain; SF‐36‐GH = General Health; SF‐36‐VT = Vitality; SF‐36‐SF = Social Functioning; SF‐36‐RE = Role‐Emotional; SF‐36‐MH = Mental Health [4].
Sociodemographic and other correlates
Sociodemographic data collected included sex, age, highest educational level, occupation, as well as living situation (e.g. who lives with you at home, and who cares for you at home). Questions on cigarette and waterpipe smoking behavior were also included including questions on current smoking status, age at smoking initiation and quitting (for ex-smokers), and quantity smoked per day [allowing the calculation of pack-years]. Data on the underlying diagnosis leading to respiratory failure as well as the main indication for the initiation of HMV was also collected. Finally, the patient was asked to specify the time in years s/he have been using the therapy at home and the hours of use during the day (Additional file 1).
Cross cultural adaptation
The main purpose behind cross-cultural adaptation is to come up with a comparable version between the original scale (German) and the target version (Arabic).
Translation and back translation
The German original was translated to formal Arabic by two different professional sworn translators, whose native language was Arabic. Four authors (M.A., L.G., A.S., and M.K.) reviewed and discussed the two translations, synthesized the results of the two translations and agreed on a common modified Arabic version. The two translations were very similar except for a few minor linguistic differences. The pre-final Arabic version was then back translated to German by a third independent translator, blinded to the original German version; the back-translated version was compared with the original version by a fourth translator. This step was undertaken to ensure correctness of the forward translations.
Pretesting the pre-final Arabic version
The version was then pretested among 10 patients receiving HMV, identified and recruited in a similar manner through which the study sample was assembled. The objective of this step was to ensure that the adapted version retains the adequacy of content, clarity of wording and usefulness. No amendments were done as the participants highlighted that the Arabic SRI was easy and understandable. The final Arabic version resulting from the pretest was used within the data collection tools for the validation study.
Analysis
Descriptive statistics were generated for the patients’ socio-demographics, disease characteristics, HMV utilization, general quality of life scores, and SRI scores. Exploratory Factor Analysis (EFA) was used to assess the dimensionality of the items in the scale, or its factor structure. Principal Components Analysis (PCA) was used as the extraction method, and the scree test to determine the number of factors [33, 34]. The internal consistency reliability of the Arabic-SRI scale and its subscales were assessed by calculating the Cronbach alpha coefficient for the total scale and the subscales. Values of Cronbach’s alpha above 0.7 were considered acceptable [24]. The internal construct validity was assessed using Confirmatory Factor Analysis (CFA) assuming the factor structure as per the original SRI. The model fit was evaluated using the Root Mean Square Error of Approximation (RMSEA) and the Comparative Fit Index (CFI). Values of RMSEA less than or equal to 0.05 indicate a good fit, between 0.05 and 0.08 indicate an adequate fit, and values greater than 0.10 indicate a poor fit. A lower bound of RMSEA 90% confidence interval (CI) less than 0.05, as well as an upper limit less than 0.08, indicate a good fit, whereas a maximum upper bound of 0.10 indicates an acceptable fit. Values of CFI ≥ 0.95 indicate a good fit, values less than 0.95 but greater than 0.90 indicate an adequate fit, and values ≤ 0.90 indicate a poor fit [25]. External nomological validity was finally assessed by examining the Pearson correlation between the Arabic-SRI and the ArabicSF-36. All statistical analyses were done using the Statistical Package for Social Sciences (SPSS) version 23.0.
Results
Patients profiles
The questionnaire was surveyor-assisted and had 100% item response rate. However, forty-eight percent of patients did not respond to the item 31 “My marriage/relationship is suffering because of my illness” since they were not married or in a relation at time of filling the questionnaire. Given that the item 31 is one question in determining the social functioning of a patient, it is believed that the response to that item would be in same direction with the entire SRI-SF subscale. Therefore, the “not applicable” answers of the item 31 were substituted by the SRI-SF mean of the same patient calculated based on the responses of the remaining 7 items of that particular subscale. The interview took 15 ± 4 min to complete. The sample was two-thirds female, aged 69.80 ± 10 years, and the majority suffered from COPD (77.00%, n = 114); the remaining patients suffered from a variety of conditions including neuromuscular diseases, Obesity Hypoventilation Syndrome, Restrictive Chest Wall Disorders, among others. About one in four (21.00%, n = 31) were current smokers, two-thirds (62.00%, n = 93) had quit smoking, and 17% (n = 25.00) had never smoked. HMV had been utilized for a mean of 32.60 ± 36.2 months and was applied for a mean of 8.10 ± 3.9 h per day. Demographic and clinical characteristics of the surveyed patients are summarized in Table 1.
Dimensionality and internal construct validity
The scree test (Fig. 1) suggests that a 1-factor solution is optimal. The ratio of the first to second eigenvalue in our sample was greater than 4, which is further evidence for unidimensionality of the overall scale.
Initial CFA on each subscale did not show a good fit. Modification indices suggested the correlation of residual errors for some items in the SRI-RC, SRI-AS, SRI-WB and SRI-SF sub-scales to improve fit. This resulted in an acceptable RMSEA 90% CI for the subscales RC, WB & SF (upper bound did not exceed 0.1). Moreover, CFI results reflected a good model fit of the observed values in all subscales (above 0.9) (Additional file 2: Table S1).
Internal consistency reliability
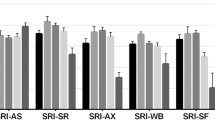
Scores of the Arabic SRI-SS and all subscales are shown in Table 2. Cronbach’s alpha was high for the summary scale, and all subscales ranging between 0.73 and 0.89 (Table 2).
External nomological validity
Table 3 depicts the observed correlations between each of the subscales of the Arabic SRI and subscales of the Arabic SF-36. All correlations in the table are statistically significant at a P-value < 0.01 level. Correlation between the SF-36-MHC and SF-36-PHC with SRI-SS scale was 0.57 and 0.66, respectively. The highest correlations were found between the Physical Functioning and the Social Functioning subscales of both instruments. Correlations were also high between the SRI-WB and SF-36-MH, and the SRI-AX and SF-36-RE. The lowest correlated subscales were the SRI-PF and the SF-36-MH (r = 0.21). The correlation between the SRI-Summary Scale and the SF-36-Physical Health Component Summary (r = 0.66) was slightly higher than the correlation between the SRI-Summary Scale and the SF-36-Mental Health Component Summary (r = 0.57).
Discussion
The evidence supporting the benefits of using a disease-specific questionnaire to assess Health-Related Quality of Life (HRQL) in patients with chronic respiratory insufficiency in multiple languages and contexts necessitates the availability of an Arabic-validated SRI. Following a rigorous translation and back-translation process, and pretesting, the final Arabic-SRI scale showed a high internal consistency reliability, and good external nomological validity. Adding to its utility is the fact that formal Arabic was used in the translation (as opposed to the Lebanese dialect), as a result, the instrument can be used in any Arab-speaking population given that formal Arabic is understood by all Arabic-speaking nations. When assessing reliability, all subscales had high internal consistency almost identical to the original version [17], and results were comparable to findings of other validation studies [18,19,20, 22].
Our estimates of internal consistency (0.897 vs. 0.89), and percent variance explained by the 49-items (63.0% vs. 60.0%) are comparable to the original findings of the German scale. Also corroborating the findings of Windisch et al. [17], we found high correlations between comparable subscales of the SRI and the SF-36. This implying that the Arabic SRI is capable of accurately and consistently measuring certain aspects of the quality of life available in the SF-36, tool typically applied to assess general HRQL. High correlations, as expected and desired, were attained between the physical functioning subscales of both SRI and SF-36, the SRI-WB and the SF-36-MH, as well as the SRI-AX and the SF-36-RE, which is expected and desirable since these subscales measure similar aspects of quality of life. In contrast, subscales measuring different aspects of quality of life such as SRI-RC and SRI-AS had low correlations with SF-36 subscales, as the latter does not explicitly measure respiratory complaints and sleep disturbances.
The low correlations between the subscales of the SRI and the SF-36 measuring different domains ascertains the necessity of having a tool that assesses unique concepts of HRQL related to patients with chronic respiratory failure that are not available in the SF-36 or other tools.
The study findings need to be interpreted considering certain limitations. Tracheostomized patients were not included in this validation study to make it comparable with the original study, keeping in mind that patients receiving mechanical ventilation via tracheostomy tubes have different characteristics than those receiving it non-invasively and thus have implications on their HRQL. However, validating the Arabic SRI among patients receiving HMV via tracheostomy is of a special interest since the prevalence of this group has been significantly increasing over years. Clinical parameters including blood gas values and lung function test were not collected for the current study since the sample was home-based recruited all over Lebanon governorates rather than hospital/clinical based.
Additionally, and unlike the original version that was self-administered, the Arabic version was surveyor-assisted to ensure the best questionnaire administration technique based on our sample characteristics. Assisted administration was adopted to avoid major discrepancies in the mode of administration due to the relatively higher proportion of elderly subjects, and substantial proportion of patients with low education status in our sample. Therefore, assisted administration might have contributed to the low missing item rate in our study, which could have positively influenced the results as other validation studies used self-administered methodology.
Conclusion
The Arabic SRI version is a valid and reliable tool with high internal consistency reliability and good external nomological validity, comparable to the original German version. The formal Arabic-SRI might be administered across several Arab-speaking populations to allow a valid assessment of quality of life in patients receiving HMV. Such a tool is useful in future epidemiological studies or clinic-based settings to help delineate factors influencing a better quality of life, evaluate interventions and ultimately inform the allocation of resources within the Lebanese context, and possibly other Arab countries.
Availability of data and materials
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request. The authors are happy to share the datasets if the manuscript passes the screening phase and reaches preliminary acceptance.
References
Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40.
Higginson IJ, Carr AJ. Measuring quality of life: using quality of life measures in the clinical setting. BMJ. 2001;322:1297–300.
Marilyn B, Bobbitt RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of a health status measure. Medical Care. 1981;8XI(8):787–805.
Ware JE, Reorian J, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–83.
Guyatt GH, Berman LB, Townsend M, Pugsley SO, Chambers LW. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42:773–8.
Sullivan CE, Issa FG, Berthon-Jones M, Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981;1(862):865.
Bach JR, Alba AS. Management of chronic alveolar hypoventilation by nasal ventilation. Chest. 1990;97:52–7.
Leger P, Bedicam JM, Cornette A, Reybet-Degat O, Langevin B, Polu JM, Jeannin L, Robert D. Nasal intermittent positive pressure ventilation. Long-term follow-up in patients with severe chronic respiratory insufficiency. Chest. 1994;105:100–5.
Meecham JDJ, Paul EA, Jones PW, Wedzicha JA. Nasal pressure support ventilation plus oxygen compared with oxygen therapy alone in hypercapnic COPD. Am J Respir Crit Care Med. 1995;152:538–44.
Simonds AK, Elliott MW. Outcome of domiciliary nasal intermittent positive pressure ventilation in restrictive and obstructive disorders. Thorax. 1995;50:604–9.
Anonymous. Clinical Indications for noninvasive positive pressure ventilation in chronic respiratory failure due to restrictive lung disease, COPD, and nocturnal hypoventilation—a consensus conference report (CHEST 1999; 116:521–534)
Mehta S, Hill NS. Noninvasive ventilation. Am J Respir Crit Care Med. 2001;163:540–77.
Duiverman ML, Wempe JB, Bladder G, Kerstjens HAM, Wijkstra PJ. Health related quality of life in COPD patients with chronic respiratory failure. Eur Respir J. 2008;32:379–86. https://doi.org/10.1183/09031936.00163607.
Elliott MW, Simonds AK, Carroll MP, Wedzicha JA, Branthwaite MA. Domiciliary nocturnal nasal intermittent positive pressure ventilation in hypercapnic respiratory failure due to chronic obstructive lung disease: effects on sleep and quality of life. Thorax. 1992;47:342–8.
Sivasothy P, Smith IE, Shneerson JM. Mask intermittent positive pressure ventilation in chronic hypercapnic respiratory failure due to chronic obstructive pulmonary disease. Eur Respir J. 1998;11:34–40.
Pehrsson K, Olofson J, Larsson S, Sullivan M. Quality of life of patients treated by home mechanical ventilation due to restrictive ventilatory disorders. Respir Med. 1994;88:21–6.
Windisch W, Freidel K, Schucher B, Baumann H, Wiebele M, Matthys H, Petermann F. The Severe Respiratory Insufficiency (SRI) Questionnaire: a specific measure of health-related quality of life in patients receiving home mechanical ventilation. J Clin Epidemiol. 2003;56:752–9. https://doi.org/10.1016/S0895-4356(03)00088-X.
López-Campos JL, Failde I, Masa JF, Benítez-Moya JM, Barrot E, Ayerbe R, León-Jimenez A, Windisch W. Transculturally adapted Spanish SRI Questionnaire for home mechanically ventilated patients was viable, valid, and reliable. J Clin Epidemiol. 2008. https://doi.org/10.1016/j.jclinepi.2007.09.002.
Ghosh D, Rzehak P, Elliott MW, Windisch W. Validation of the English Severe Respiratory Insufficiency Questionnaire. ERJ Express. 2011. https://doi.org/10.1183/09031936.00152411.
Markussen H, Lehmann S, Nilsen RM, Natvig GK. The Norwegian version of the Severe Respiratory Insufficiency (SRI) Questionnaire. Int J Nurs Pract. 2015;21:229–38.
Tsara V, Michailidis V, Perantoni E1 , Nena E2 , Moysiadis N, Windisch W, Steiropoulos P. HIPPOKRATIA. 2017; 21(4):186–90.
Chen R, Guan L, Wu W, et al. The Chinese version of the Severe Respiratory Insufficiency questionnaire for patients with chronic hypercapnic chronic obstructive pulmonary disease receiving non-invasive positive pressure ventilation. BMJ Open. 2017;7:e017712. https://doi.org/10.1136/bmjopen-2017-017712.
Oga T, Taniguchi H, Kita H, Tsuboi T, Tomii K, Ando M, Kojima E, Tomioka H, Taguchi Y, Kaji Y, Maekura R, Hiraga T, Sakai N, Kimura T, Mishima M, Windisch W, Chin K. Validation of the Japanese Severe Respiratory Insufficiency Questionnaire in hypercapnic patients with non-invasive ventilation. Respir Investig. 2017;55:166–72.
Nunnally JC, Bernstein I. Psychometric theory. 3rd ed. New York: McGraw-Hill; 1994.
Brown TA, Moore MT. Confirmatory factor analysis. In: Hoyle RH, editor. Handbook of structural equation modeling. New York: Guilford Press; 2012. p. 361–79.
Ribeiro C, Ferreira D, Conde S, Oliveira P, Windisch W. Validation of the Portuguese Severe Respiratory Insufficiency Questionnaire for home mechanically ventilated patients. Rev Port Pneumol. 2017;23(3):139–45. https://doi.org/10.1016/j.rppnen.2017.01.001.
Valko L, Baglyas S, Kunos L, Terray-Horvath A, Lorx A, Gal J, Windisch W. Validation of the Hungarian version of the SRI Questionnaire. BMC Pulm Med. 2020;20(1):130. https://doi.org/10.1186/s12890-020-1171-5.PMID:32380984;PMCID:PMC7204221.
Cuvelier A, Lamia B, Molano LC, Muir JF, Windisch W. Groupe assistance ventilatoire (GAV) de la Société de pneumologie de langue française (SPLF). Traduction française et adaptation culturelle du questionnaire SRI. Questionnaire de qualité de vie liée à la santé des patients insuffisants respiratoires chroniques traités par ventilation à domicile [The French translation and cultural adaptation of the SRI questionnaire. A questionnaire to assess health-related quality of life in patients with chronic respiratory failure and domiciliary ventilation]. Rev Mal Respir. 2012;29(5):705–13 (French). https://doi.org/10.1016/j.rmr.2011.12.015(French).
Bobkova I. Message from Ms Irina Bokova, Director-General of UNESCO, on the occasion of the First World Arabic Language Day 18 December 2012. UNESCO; 2012. www.unesco.org/new/en/unesco/events/prizes-and-celebrations/celebrations/international-days/world-arabic-language-day/.
List of Countries where Arabic is an Official Language. Wikipedia; 2017. http://en.wikipedia.org/wiki/List_of_countries_where_Arabic_is_an_official_language.
Pearson RH, Mundform DJ. Recommended sample size for conducting exploratory factor analysis on dichotomous data. J Mod Appl Stat Methods. 2010;9(2):5–74. https://doi.org/10.22237/jmasm/1288584240.
Mundfrom DJ, Shaw DG, Ke TL. Minimum sample size recommendations for conducting factor analyses. Int J Test. 2005;5(2):159–68.
Cattell RB. The scree test for the number of factors. Multivar Behav Res. 1966;1(2):245–76.
Netemeyer RG, Bearden WO, Sharma S. Scaling procedures: issues and applications. Sage; 2003.
Acknowledgements
We acknowledge the support of Mrs. Ghina Al-Ghosh for preparing and assisting in logistics for data collection.
Funding
The study was funded by the Conseil National de la Recherche Scientifique (CNRS)—Lebanon to cover data collection costs. Fund reference number: 01-08-15. Role of the CNRS: The CNRS had no role in the preparation of data or the manuscript.
Author information
Authors and Affiliations
Contributions
M.F.A., R.N.B., M.F.K., L.F.G., S.M.Z., L.F.G., A.M.S., M.F.A., and M.F.E. developed the tools. M.F.A.. & R.N.B. conducted statistical analysis and wrote the manuscript. L.F.G., A.N.S., S.M.Z. and M.F.E. critically revised and provided feedback on the manuscript. L.F.G. provided technical feedback and advise on psychometric analysis. S.M.Z. and M.F.E. provided expert advice (pulmonary related) for the analysis. M.F.A., R.N.B., L.F.G., M.F.E., and A.M.S. reviewed and responded to the editorial revision. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board at the American University of Beirut, Lebanon. The informed consent forms were obtained from all participants. The American University of Beirut and its Institutional Review Board, under the Institution’s Federal Wide Assurance with OHRP, comply with the Department of Health and Human Services (DHHS) Code of Federal Regulations for the Protection of Human Subjects (“The Common Rule”) 45CFR46, subparts A, B, C, and D, with 21CFR56; and operate in a manner consistent with the Belmont report, FDA guidance, Good Clinical Practices under the ICH guidelines, and applicable national/local regulations. The statement for “ethical approval” and the “informed consent” are attached in the system.
Consent for publication
Not applicable.
Competing interests
All authors do not have any conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Questionnaire.
Additional file 2. Table S1
. Confirmatory Factor Analysis Results.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alawieh, M.F., Bzeih, R.N., El-Khatib, M.F. et al. Validation of the Arabic Severe Respiratory Insufficiency Questionnaire. BMC Pulm Med 21, 315 (2021). https://doi.org/10.1186/s12890-021-01644-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-021-01644-x