Abstract
Background
Although antifibrotic drugs, including nintedanib and pirfenidone, slow the progression of idiopathic pulmonary fibrosis (IPF), there is little data about the timing of start of antifibrotic treatment in real-world clinical practice. The present study aimed to clarify the efficacy of nintedanib and pirfenidone in patients with early-stage IPF.
Methods
We compared survival and disease progression between patients with IPF with Japanese Respiratory Society (JRS) disease severity system stage I with and without oxygen desaturation on the 6-min walk test (6MWT) and increased the gender–age–physiology (GAP) staging. We examined the efficacy of antifibrotic drugs in patients with early-stage IPF.
Results
The severity of stage I IPF (n = 179) according to the JRS criteria consisted of the following GAP staging criteria: stage I, 111 cases; stage II, 58 cases; stage III, 10 cases. The duration from the initial visit to disease progression and survival time was significantly shorter in JRS stage I patients with oxygen desaturation on the 6MWT or with increased GAP staging (unfavorable group) compared with patients without those factors. In the unfavorable group, the relative decline in percentage predicted forced vital capacity (%FVC) over 6 months was significantly lower in patients undergoing antifibrotic treatment compared with non-treated patients.
Conclusion
Antifibrotic drugs have a beneficial effect on the decline in %FVC in Japanese patients with early-stage IPF who have oxygen desaturation on the 6MWT or increased GAP staging.
Similar content being viewed by others
Introduction
Idiopathic pulmonary fibrosis (IPF) is a fatal and progressive lung disease of undetermined etiology that has a heterogeneous clinical course. The median survival time from diagnosis is 3–5 years [1, 2]. Although there are no cures and few treatment options for patients with IPF, nintedanib and pirfenidone significantly reduce the decline in forced vital capacity (FVC) and have been approved for the treatment of IPF [3, 4]. Indeed, more recent IPF registries have demonstrated that the use of antifibrotic drugs (pirfenidone or nintedanib) are associated with improved survival of IPF patients in the era of antifibrotic therapies [5, 6]. Several retrospective and prospective studies have shown that a 5–10% decline in FVC within 6 or 12 months is associated with a significant increase in mortality [7,8,9]. Thus, we propose that antifibrotic treatment for IPF should be started as soon as the diagnosis is made. However, a “watch and wait” approach is not uncommon and the question of when to start antifibrotic treatment is still widely debated [10].
In Japan, IPF disease severity is assessed using the Japanese Respiratory Society (JRS) disease severity system, which is based on the partial pressure of oxygen in arterial blood (PaO2) at rest and the presence of oxygen desaturation during the 6-min walk test (6MWT) [11]. On the other hand, the gender–age–physiology (GAP) staging system is developed as a mortality risk prediction tool in IPF [12].
Recently, a post-hoc analysis of pooled date from the INPULSIS trials suggested that nintedanib had a similar beneficial effect on the rate of decline in FVC in patients with GAP stage I versus patients with GAP stage II/III at baseline [13].
To our best knowledge, little has been reported on the appropriate time to start antifibrotic treatment in Japanese patients with early-stage IPF. Herein, we aimed to clarify the efficacy of antifibrotic drugs, including nintedanib and pirfenidone, for patients with early-stage IPF in real-world clinical practice.
Methods
Study population
In this retrospective study, patients with IPF at two centers in Japan (Tsuboi Hospital and Toho University Omori Medical Center) were enrolled from April 2006 to March 2019. IPF was diagnosed based on 2011 international IPF guidelines [1]. The diagnosis of emphysema was based on upper lobe predominant and scattered distribution of low attenuation areas on chest HRCT, either no wall or with wall of less than 1 mm in thickness [14]. Combined pulmonary fibrosis and emphysema (CPFE) was defined as concomitant IPF and ≥ 10% emphysema on chest HRCT by criteria proposed by Ryerson, et al. [15]. Based on these findings, we excluded patients with CPFE in this study. The diagnosis of all patients was evaluated by a multidisciplinary team based on patients’ clinical, radiological and/or pathological findings. In total, 431 patients with suspected IPF were enrolled. Patients with absence of pulmonary function test findings at baseline and at a follow-up of 6 months (n = 45), unavailable chest high-resolution computed tomography (HRCT) results (n = 17), lung cancer (n = 33), and untraceable survival (n = 21) were excluded. A total of 315 patients were included. The number of patients with JRS stage I, II, III, and IV was 179, 28, 71, and 71, respectively (Fig. 1).
The modified diagnostic criteria for acute exacerbation (AE) of IPF proposed by Collard et al. [16] was as follows: (1) previous/concurrent IPF diagnosis; (2) unexplained worsening or development of dyspnea within 30 days; (3) chest HRCT with new bilateral ground-glass opacities and/or consolidation superimposed on a reticular or honeycomb background; (4) exclusion of alternative causes of acute lung injury such as pneumonia, left-sided heart failure, and pulmonary embolism.
Clinical and laboratory data was obtained from medical records, including IPF disease severity, efficacy of antifibrotic treatment, changes in pulmonary function (every 6 months), and prognosis. In Japan, classification of IPF disease severity in IPF is as follows: stage I (PaO2 ≥ 80 Torr at rest), stage II (80 > PaO2 ≥ 70 Torr at rest), stage III (70 > PaO2 ≥ 60 Torr at rest), and stage IV (PaO2 < 60 Torr at rest). If patients with stage II or III have oxygen desaturation (the lowest SpO2 is < 90%) during the 6MWT, they are classified as stage III or IV, respectively [11]. The GAP score and stage were calculated according to a method described by Ley et al. [12].
In this study, pirfenidone and nintedanib have been used since 2008, and 2015, respectively. In addition, patients who were diagnosed as IPF from 2006 to 2008, were treated as non-treated group. To evaluate the response to treatment, we defined disease progression as a relative decline of ≥ 5% and stable disease as a relative decline of < 5% in percentage predicted FVC (%FVC) over a period of 6 months.
All methods were carried out in accordance with relevant guidelines and regulations.
The study was approved by the Institutional Review Board of Tsuboi Hospital (no. Zizan 1-3). The Ethical Committees of Tsuboi Hospital waived the need for informed consent because of the retrospective clinical review.
Chest computed tomography (CT) scan
Helical CT scanners (Aquilion 16, Toshiba, Tokyo, Japan and Aquilion Prime, Canon, Tokyo, Japan) were used. Thin-section CT images were obtained during full inspiration, and the scanning protocol consisted of reconstruction of a 1- to 2-mm slice thickness with a high spatial frequency algorithm. Thin-section chest CT images were photographed at window settings appropriate for the lung parenchyma (window level, − 600 to − 450 HU; width, 1600–1900 HU) in all patients.
Pulmonary function test
Spirometry and measurements of diffusing capacity of the lungs for carbon monoxide (DLco) were performed using a pulmonary function test (PFT) system (Chestac-33, CHEST Co. Ltd., Tokyo, Japan). The diffusion capacity was measured using the single breath technique. These PFTs were performed by two technicians according to the method described in the American Thoracic Society criteria [17].
6MWT
The 6MWT was performed according to the ATS recommendations [17], and continuous monitoring of heart rate and oxygen arterial saturation with pulse oximetry, and walking distance were recorded. During 6MWT, patients were instructed to walk as fast as possible and were allowed to slow down or to stop if necessary. The oxygen desaturation on the 6MWT was defined as indicating < 90% on oxygen saturation with pulse oximetry during 6MWT.
Statistical analysis
Data is presented as the number of patients with percentage or mean with standard deviation, as appropriate. The comparisons between the two groups were evaluated using Pearson’s Chi-squared test or Fisher’s exact test for categorical variables and the Student’s t-test for parametric continuous variables. Survival curves and the cumulative incidence of disease progression were estimated using the Kaplan–Meier method, and differences in the curves were calculated using the log-rank test. A two-sided p value of < 0.05 was considered statistically significant. Statistical analyses were performed using JMP statistical software (version 10.0.0, SAS Institute, Cary, NC, USA).
Results
Baseline demographic characteristics of patients with stage I IPF according to the JRS severity system
The study population consisted of 179 patients [148 males (83%) and 31 females (17%)] with a mean age of 71.5 years (range 43–86 years). One hundred fifty seven patients had a smoking history. Mean PaO2 was 90.3 Torr in room air. The percentage of patients with oxygen desaturation on the 6MWT was 37.4%. The mean %FVC and predicted DLco (%DLco) were 81.5% (range 37.4–129.1%) and 68.8% (range 23.7–143.2%), respectively (Table 1).
Correlation between the numbers of patients with different JRS disease severities according to the JRS severity system and the GAP staging model
JRS stage I (n = 179) consisted of the following GAP staging model breakdown: stage I, 111 cases; stage II, 58 cases; stage III, 10 cases. The percentage of patients with GAP stage II/III with JRS stage I was 37.9% (Table 2).
Comparison of clinical and demographic characteristics between JRS stage I with and without oxygen desaturation on the 6MWT
Baseline GAP staging, modified Medical Research Council (mMRC) value, serum Krebs von den Lungen (KL)-6, and serum surfactant protein (SP)-D in patients with JRS stage I with oxygen desaturation were significantly higher compared with patients with JRS stage I without oxygen desaturation on the 6MWT, and PaO2, %FVC, %DLco, 6-min walking distance (6MWD), and lowest percutaneous oxygen saturation (SpO2) on the 6MWT were significantly lower for patients with JRS stage I with oxygen desaturation on the 6MWT compared with patients with JRS stage I without oxygen desaturation on the 6MWT (Table 3).
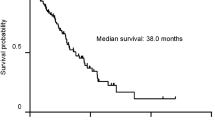
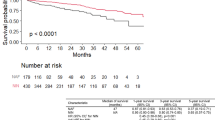
The duration from the initial visit to disease progression was shorter in patients with JRS stage I with oxygen desaturation on the 6MWT compared with patients with JRS stage I without oxygen desaturation on the 6MWT [median survival time (MST), 13.9 months vs. 37.4 months, P = 0.002] (Fig. 2A). The Kaplan–Meier survival curve showed a significantly poorer outcome in patients with JRS stage I with oxygen desaturation on the 6MWT compared with patients with JRS stage I without oxygen desaturation on the 6MWT (MST = 40.8 months vs. 64.9 months, P = 0.002) (Fig. 2B).
Comparison of clinical and demographic characteristics between patients with JRS stage I with GAP stage I and GAP stage II/III
The mean age, ratio of male, GAP staging, mMRC, and serum SP-D were significantly higher in patients with JRS stage I with GAP stage II/III compared with patients with JRS stage I with GAP stage I. In contrast, body mass index, %FVC, %DLco, 6MWD, and lowest SpO2 on the 6MWT were significantly lower in patients with JRS stage I with GAP stage II/III compared with patients with JRS stage I with GAP stage I (Table 4).
The duration from the initial visit to disease progression was shorter in patients with JRS stage I with GAP stage II/III compared with patients with JRS stage I with GAP stage I (MST = 17.3 months vs. 34.4 months, P = 0.006) (Fig. 3A). The survival time for patients with JRS stage I with GAP stage II/III was significantly shorter compared with patients with JRS stage I with GAP stage I (MST = 39.1 months vs. 64.1 months, P = 0.004) (Fig. 3B).
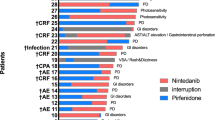
Antifibrotic treatment for patients with JRS stage I with oxygen desaturation on the 6MWT and JRS stage I with GAP stage II/III
Forty eight patients with JRS stage I with oxygen desaturation on the 6MWT and 39 patients with JRS stage I with GAP stage II/III were treated with antifibrotic drugs during 6 months. Fifteen of 48 patients with JRS stage I with oxygen desaturation on the 6MWT and 11 of 39 patients with JRS stage I with GAP stage II/III were treated with nintedanib, and each remaining patient received pirfenidone. There was no difference in comparative clinical and demographic characteristics between antifibrotic drug-treated patients and non-treated patients in JRS stage I with oxygen desaturation on the 6MWT and JRS stage I with GAP stage II/III (Tables 5, 6).
As a result, in patients with JRS stage I with oxygen desaturation on the 6MWT, the rate of decline in FVC over 6 months was − 61 mL ± 178 mL in the antifibrotic drug-treated group and − 147 mL ± 172 mL in the non-treated group (P = 0.02) (Fig. 4A). In patients with JRS stage I with GAP stage II/III, the rate of decline in FVC over 6 months was − 32 mL ± 176 mL in the antifibrotic drug-treated group and − 121 mL ± 185 mL in the non-treated group (P = 0.04) (Fig. 4B). Moreover, the relative decline in %FVC over 6 months was significantly lower in antifibrotic drug-treated patients compared with non-treated patients (JRS stage I with oxygen desaturation on the 6MWT: − 7.0% ± 8.4% vs − 2.4% ± 9.8%, P = 0.02; Fig. 5A, JRS stage I with GAP stage II/III: − 6.8% ± 9.2% vs − 0.6% ± 10.1%, P = 0.009; Fig. 5B).
Comparison with the rate of decline in FVC over 6 months between the antifibrotic drug-treated group and the non-treated group in patients with JRS stage I with oxygen desaturation on the 6MWT or those with JRS stage I with GAP stage II/III. (A) In patients with JRS stage I with oxygen desaturation on the 6MWT. (B) In patients with JRS stage I with GAP stage II/III
Comparison with the relative decline in %FVC over 6 between the antifibrotic drug-treated group and the non-treated group in patients with JRS stage I with oxygen desaturation on the 6MWT or those with JRS stage I with GAP stage II/III. (A) In patients with JRS stage I with oxygen desaturation on the 6MWT. (B) In patients with JRS stage I with GAP stage II/III
Although there was no difference in comparative efficacy between antifibrotic drug-treated patients and non-treated patients (rate of disease progression in JRS stage I with oxygen desaturation on the 6MWT: antifibrotic drug-treated group vs. non-treated group, 41.6% vs. 62.1%, respectively, P = 0.08; JRS stage I with GAP stage II/III: antifibrotic drug-treated group vs. non-treated group, 38.4% vs. 53.1%, respectively, P = 0.23), the efficacy of antifibrotic treatments tended to be better.
Discussion
Our data indicate that patients with IPF who have JRS stage I with oxygen desaturation on the 6MWT or increased GAP staging (II/III) had a significantly poorer prognosis compared with patients without these risk factors. Among these patients’ group, it is noteworthy that antifibrotic treatments had a beneficial effect on the rate of decline in FVC, as the relative decline in %FVC over 6 months was significantly lower in antifibrotic drug-treated patients compared with in non-treated patients. The findings support that treatment with antifibrotic drugs for IPF should be started in the early-stage patients with these conditions. However, delays in antifibrotic treatments are not uncommon, because some pulmonologists tend to fear adverse effects induced by antifibrotic drugs and thus postpone antifibrotic treatments until disease progression is observed [10, 18]. In particular, although medical cost subsidization for intractable diseases is essentially adapted to patients with stage III or IV disease in Japan, patients with IPF of JRS stage I or II are not covered immediately. Therefore, this limited subsidization system is one of the major causes of delay in the administration of antifibrotic treatments.
In Japan, the JRS severity system is used and is based on PaO2 and the presence of oxygen desaturation during the 6MWT to decide on medical cost subsidization for IPF. If patients with stage II or III disease present with oxygen desaturation during the 6MWT, they are classified into stage III or IV, respectively [11]. Kondoh et al. reported that no significant difference in survival between patients with JRS stage I and II IPF, although prognosis for patients with JRS stage IV was significantly poorer compared with patients with JRS stage III [19]. Thus, a revision of the JRS severity system was proposed. This revision stipulated that if patients with original JRS stage I demonstrate oxygen desaturation during the 6MWT, they are classified as JRS stage II. As a result, a significant difference in survival is observed between patients with revised JRS stage I and stage II. In the present study, patients with JRS stage I with oxygen desaturation on the 6MWT had a significantly worse prognosis compared with JRS stage I patients without oxygen desaturation.
The GAP staging model proposed by Ley et al. has been widely studied and validated in the United States, Italy, Korea, and Japan [12, 20, 21]. Recently, a Japanese study demonstrated the relationship of mortality risk with the JRS severity system and the GAP staging model [21]. According to the study, 64 patients (45.4%) with JRS stage I (n = 141) were classified into GAP stage II or III. In our study, overall survival in patients with JRS stage I IPF and GAP stage II or III [68 patients (37.9%) with JRS stage I (n = 179)] was significantly poorer compared with patients with JRS stage I and GAP stage I. Furthermore, they had a significantly shorter 6MWD, higher mMRC score, a lower SpO2, %FVC, and %DLco. Several baseline clinical characteristics including age, FVC, DLco, and oxygen desaturation on the 6MWT are reported to be prognostic factors for IPF [1]. These findings may indicate that damage to pulmonary function does not always reflect the PaO2 at rest. Therefore, the JRS staging system solely based on resting oxygenation may not be practically helpful. On the other hand, the GAP staging system is regarded as a well-validated staging system in IPF, because this system strongly correlates with disease severity and mortality. As a result, we believe that it is important to integrate oxygen desaturation on the 6MWT or the GAP staging with JRS stage I into the original JRS staging system.
Kolb et al. reported that treatment with nintedanib had the same annual rate of decline in FVC in patients with a predicted %FVC of > 90% and ≤ 90% [22]. Furthermore, Albera et al. described that no significant difference in the effect of treatment with pirfenidone between patients with more preserved (%FVC ≥ 80% or GAP stage I) versus less preserved lung function (%FVC < 80% or GAP stage II–III) [23]. Recently, a post-hoc analysis of pooled date from the INPULSIS trials suggested that nintedanib had a similar beneficial effect on the annual rate of decline in FVC in patients with GAP stage I versus GAP stage II/III at baseline [13]. These findings support the efficacy and safety of early antifibrotic treatments for IPF.
This study has some limitations. First, this was a retrospective study with a small sample size. Therefore, our results may not be representative of the entire IPF population in Japan. Second, although many studies have shown that a relative or absolute decline in predicted %FVC of ≥ 10% at 12 months is associated with a significant increase in mortality, we defined disease progression as a relative decline of ≥ 5% and stable disease as a relative decline of < 5% in predicted %FVC over a 6-month period. However, Zappala et al. described that a decline in predicted %FVC of 5–10% is related to an increase in the risk of mortality at 6 months [7]. Thus, we believe that a smaller decline in FVC may predict a worse prognosis more quickly. Third, we excluded patients who did not undergo PFTs at baseline and who did not undergo chest HRCT. Indeed, the considerable number of excluded patients may have led to selection bias.
In conclusion, our data suggests that antifibrotic drugs have a beneficial effect on the rate of decline in FVC in Japanese patients with early-stage IPF who demonstrated oxygen desaturation on the 6MWT or increased GAP staging. Further large prospective studies are needed in order to propose modified new staging system of IPF for future guidance of starting antifibrotic treatments.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- IPF:
-
Idiopathic pulmonary fibrosis
- MST:
-
Median survival time
- HRCT:
-
High-resolution computed tomography
- AE:
-
Acute exacerbation
- BMI:
-
Body mass index
- mMRC:
-
Modified Medical Research Council
- KL-6:
-
Krebs von den Lungen-6
- SP-D:
-
Surfactant protein-D
- GAP:
-
Gender–age–physiology
- JRS:
-
Japanese Respiratory Society
- FVC:
-
Forced vital capacity
- %FVC:
-
Percentage predicted FVC
- DLco:
-
Diffusing capacity of the lung for carbon monoxide
- FEV1 :
-
Forced expiratory volume in 1 s
- TLC:
-
Total lung capacity
- PFT:
-
Pulmonary function test
- PaO2 :
-
Partial pressure of oxygen in arterial blood
- PaCO2 :
-
Partial pressure of carbon dioxide in arterial blood
- CI:
-
Confidence interval
- SD:
-
Standard deviation
References
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
King TE Jr, Pardo A, Selman M. Idiopathic pulmonary fibrosis. Lancet. 2011;378:1949–61.
Richeldi L, du Bois RM, Raghu G, Azuma A, Brown KK, Costabel U, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2071–82.
King TE Jr, Bradford WZ, Castro-Bernardini S, Fagan EA, Glaspole I, Glassberg MK, et al. A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med. 2014;370:2083–92.
Jo HE, Glaspole I, Grainge C, Goh N, Hopkins PM, Moodley Y, et al. Baseline characteristics of idiopathic pulmonary fibrosis: analysis from the Australian Idiopathic Pulmonary Fibrosis Registry. Eur Respir J. 2017;49(2):1601592.
Guenther A, Krauss E, Tello S, Wagner J, Paul B, Kuhn S, et al. The European IPF registry (eurIPFreg): baseline characteristics and survival of patients with idiopathic pulmonary fibrosis. Respir Res. 2018;19(1):141.
Zappala CJ, Latsi PI, Nicholson AG, Colby TV, Cramer D, Renzoni EA, et al. Marginal decline in forced vital capacity is associated with a poor outcome in idiopathic pulmonary fibrosis. Eur Respir J. 2010;35:830–6.
Collard HR, King TE Jr, Bartelson BB, Vourlekis JS, Schwarz MI, Brown KK. Changes in clinical and physiologic variables predict survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2003;168:538–42.
Flaherty KR, Mumford JA, Murray S, Kazerooni EA, Gross BH, Colby TV, et al. Prognostic implications of physiologic and radiographic changes in idiopathic interstitial pneumonia. Am J Respir Crit Care Med. 2003;168:543–8.
Torrisi SE, Pavone M, Vancheri A, Vancheri C. When to start and when to stop antifibrotic therapies. Eur Respir Rev. 2017;26:170053.
Homma S, Sugino K, Sakamoto S. Usefulness of a disease severity staging classification system for IPF in Japan: 20 years of experience from empirical evidence to randomized control trial enrollment. Respir Investig. 2015;53:7–12.
Ley B, Ryerson CJ, Vittinghoff E, Ryu JH, Tomassetti S, Lee JS, et al. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann Intern Med. 2012;156:684–91.
Ryerson CJ, Kolb M, Richeldi L, Lee J, Wachtlin D, Stowasser S, et al. Effects of nintedanib in patients with idiopathic pulmonary fibrosis by GAP stage. ERJ Open Res. 2019;5:00127–2018.
Sugino K, Nakamura Y, Ito T, Isshiki T, Sakamoto S, Homma S. Comparison of clinical characteristics and outcomes between combined pulmonary fibrosis and emphysema associated with usual interstitial pneumonia pattern and non-usual interstitial pneumonia. Sarcoidosis Vasc Diffuse Lung Dis. 2015;32:129–37.
Ryerson CJ, Hartman T, Elicker BM, Ley B, Lee JS, Abbritti M, et al. Clinical features and outcomes in combined pulmonary fibrosis and emphysema in idiopathic pulmonary fibrosis. Chest. 2013;144:234–40.
Collard HR, Ryerson CJ, Corte TJ, Jenkins G, Kondoh Y, Lederer DJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am J Respir Crit Care Med. 2016;194:265–75.
ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7.
Maher TM, Strek ME. Antifibrotic therapy for idiopathic pulmonary fibrosis: time to treat. Respir Res. 2019;20:205.
Kondoh Y, Taniguchi H, Kataoka K, Furukawa T, Ando M, Murotani K, et al. Disease severity staging system for idiopathic pulmonary fibrosis in Japan. Respirology. 2017;22:1609–14.
Kim ES, Choi SM, Lee J, Park YS, Lee CH, Yim JJ, et al. Validation of the GAP score in Korean patients with idiopathic pulmonary fibrosis. Chest. 2015;147:430–7.
Kondoh S, Chiba H, Nishikiori H, Umeda Y, Kuronuma K, Otsuka M, et al. Validation of the Japanese disease severity classification and the GAP model in Japanese patients with idiopathic pulmonary fibrosis. Respir Investig. 2016;54:327–33.
Kolb M, Richeldi L, Behr J, Maher TM, Tang W, Stowasser S, et al. Nintedanib in patients with idiopathic pulmonary fibrosis and preserved lung volume. Thorax. 2017;72:340–6.
Albera C, Costabel U, Fagan EA, Glassberg MK, Gorina E, Lancaster L, et al. Efficacy of pirfenidone in patients with idiopathic pulmonary fibrosis with more preserved lung function. Eur Respir J. 2016;48:843–51.
Acknowledgements
This work was supported by a grant-in-aid for interstitial lung diseases from the Japanese Ministry of Health, Labor, and Welfare. We would like to thank Dr. A. Kurosaki (Department of Radiology, Fukujuji Hospital) for interpreting the radiological findings. We would like to thank Dr. A. Hebisawa (Department of Diagnostic Pathology, Asahi General Hospital) and Dr. T. Uekusa (Department of Pathology, Labor Health and Welfare Organization, Kanto Rosai Hospital) for performing the histopathological investigation.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
KS, HO, ET, SH, and KK contributed to the study conception and design. KS, HO, NW, MA, and KK analyzed and interpreted the clinical data. KS, HO, SH, and KK drafted the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Tsuboi Hospital (No. Zizan 1–3). The Ethical Committees of Tsuboi Hospital waived the need for informed consent because of the retrospective clinical review.
Consent for publication
Not applicable.
Competing interest
All authors contributed substantially to this work and are responsible for the consent of the manuscript. SH is a member of an endowed department sponsored by Teijin Pharma, Co., Ltd., Nippon Boehringer Ingelheim, Co., Ltd., Shionogi & Co., Ltd., and Chugai Pharmaceutical Co., Ltd. SH, KK, and KS have received lecture fees from Nippon Boehringer Ingelheim Co., Ltd. KK has received research funding from Nippon Boehringer Ingelheim Co., Ltd. The other authors have no financial relationships relevant to this article. All authors have no competing non-financial interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sugino, K., Ono, H., Watanabe, N. et al. Efficacy of early antifibrotic treatment for idiopathic pulmonary fibrosis. BMC Pulm Med 21, 218 (2021). https://doi.org/10.1186/s12890-021-01595-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-021-01595-3