Abstract
Background
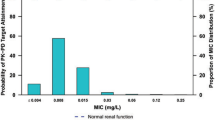
Lefamulin, a first-in-class pleuromutilin antibiotic approved for intravenous and oral use in adults with community-acquired bacterial pneumonia (CABP), was noninferior to moxifloxacin in the Lefamulin Evaluation Against Pneumonia (LEAP) 1 intravenous-to-oral switch study and the LEAP 2 oral-only study. Using pooled LEAP 1/2 data, we examined lefamulin efficacy/safety overall and within subgroups of patients presenting with comorbidities typical in CABP management.
Methods
In LEAP 1, adults with CABP were randomized to receive intravenous lefamulin (150 mg every 12 h) for 5‒7 days or moxifloxacin (400 mg every 24 h) for 7 days, with optional intravenous-to-oral switch if predefined improvement criteria were met. In LEAP 2, adults with CABP were randomized to receive oral lefamulin (600 mg every 12 h) for 5 days or moxifloxacin (400 mg every 24 h) for 7 days. Both studies assessed early clinical response (ECR) at 96 ± 24 h after first study drug dose and investigator assessment of clinical response (IACR) at test-of-cure (5‒10 days after last dose). Pooled analyses of the overall population used a 10% noninferiority margin.
Results
Lefamulin (n = 646) was noninferior to moxifloxacin (n = 643) for ECR (89.3% vs 90.5%, respectively; difference − 1.1%; 95% CI − 4.4 to 2.2); IACR success rates at test-of-cure were similarly high (≥ 85.0%). High efficacy with both lefamulin and moxifloxacin was also demonstrated across all well-represented patient subgroups, including those with advanced age, diabetes mellitus, a history of cardiovascular diseases (e.g., hypertension, congestive heart failure, or arrhythmia) or chronic lung diseases (e.g., asthma or chronic obstructive pulmonary disease), elevated liver enzymes, or mild-to-moderate renal dysfunction. No new safety signals were identified.
Conclusions
Lefamulin may provide a valuable intravenous/oral monotherapy alternative to fluoroquinolones or macrolides for empiric treatment of patients with CABP, including cases of patients at risk for poor outcomes due to age or various comorbidities.
Trial registration
ClinicalTrials.gov LEAP 1 (NCT02559310; Registration Date: 24/09/2015) and LEAP 2 (NCT02813694; Registration Date: 27/06/2016).
Similar content being viewed by others
Background
Pneumonia, a leading cause of US hospitalizations and infection-related deaths [1,2,3], is associated with substantial morbidity and mortality [4]. Pneumonia-associated economic burden is considerable, with annual costs estimated at €10.1 billion in Europe [5] and exceeding $17 billion in the United States [6]. Pneumonia prognoses can range from rapid resolution to death [7], and clinical management of community-acquired bacterial pneumonia (CABP) can be complicated by many factors [1]. CABP incidence and impact are greater in older versus younger individuals, and older patients with CABP often present with challenges (e.g., increased resistance rates, polypharmacy/drug interactions) that can impede treatment efficacy and safety [8, 9]. Comorbidities such as chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), or diabetes mellitus (DM) increase the risk of severe CABP and may aggravate clinical symptoms and complicate management [9, 10]. Underlying cardiac or liver disease also increase the risk of potential cardiac or liver toxicities, respectively, associated with CABP antimicrobials [11,12,13].
Increasingly, new CABP treatment options are needed owing to rising antibacterial resistance rates and undesirable risks/adverse effects associated with current treatments, including allergic reactions and fluoroquinolone-associated disability (e.g., tendon injury, aortic rupture, glucose homeostasis imbalance, and neurocognitive effects, especially in older patients) [1, 11, 14,15,16]. Lefamulin, a first-in-class pleuromutilin antibiotic that selectively inhibits bacterial protein synthesis [17, 18], is approved for intravenous (IV) and oral use in adults with CABP [19]. In adults with CABP, lefamulin demonstrated noninferiority to moxifloxacin in the IV-to-oral switch Lefamulin Evaluation Against Pneumonia (LEAP) 1 study [20] and the oral-only LEAP 2 study [21]. Lefamulin has demonstrated potent in vitro activity against a global collection of typical (eg, Streptococcus pneumoniae, Staphylococcus aureus, Haemophilus influenzae, Moraxella catarrhalis) and atypical (e.g., Mycoplasma pneumoniae, Legionella pneumophila, Chlamydophila pneumoniae) CABP-causative pathogens, including antimicrobial-resistant strains [22, 23]; lefamulin has also demonstrated clinical efficacy against these and other CABP pathogens [20, 21]. Moreover, lefamulin has demonstrated weak activity against Bacteroides fragilis group strains and Enterobacteriaceae, suggesting decreased potential for disruption to gastrointestinal (GI) microbiota by IV lefamulin (Data on file, Nabriva Therapeutics, Vienna, Austria). In contrast to other common CABP therapies, the suitability of lefamulin for oral administration and its targeted antimicrobial activity [19] may position it as an attractive option for use in patients with advanced age, various comorbid conditions, increased disease severity, or drug allergies. Therefore, data from the 2 pivotal phase 3 LEAP studies in adults with CABP were pooled to further examine lefamulin efficacy and safety overall and within various patient subgroups.
Methods
Study design and participants
The LEAP 1 (NCT02559310; Registration Date: 24/09/2015) [20] and LEAP 2 (NCT02813694; Registration Date: 27/06/2016) [21] studies were double-blind, double-dummy, parallel-group trials evaluating lefamulin versus moxifloxacin in adults with moderate to severe CABP. Before study initiation, participating centers obtained study approval from appropriate ethics committees/institutional review boards (Additional file 1: Appendices 1‒2), and patients provided written informed consent. Trials were compliant with the ethical principles of the Declaration of Helsinki, Good Clinical Practice guidelines, and local laws/regulations.
Detailed methods for both studies have been published elsewhere [20, 21]. Briefly, randomization (1:1) was stratified in both studies by Pneumonia Outcomes Research Team (PORT) risk class (III vs IV/V [LEAP 1]; II vs III/IV [LEAP 2]), geographic region (US vs ex-US), and receipt of a single dose of a short-acting antibacterial for CABP before randomization (yes vs no). In LEAP 1, patients received IV lefamulin 150 mg every 12 h (q12h) for 5‒7 days or moxifloxacin 400 mg every 24 h (q24h) for 7 days. If methicillin-resistant S. aureus (MRSA) was suspected at screening, blinded IV linezolid (600 mg q12h) was added to moxifloxacin, or linezolid placebo was added to lefamulin.
In LEAP 1, patients could switch to oral therapy (lefamulin 600 mg q12h or moxifloxacin 400 mg q24h) after 6 IV doses (~ 3 days) if predefined improvement criteria were met. The original study protocol indicated a 5-day lefamulin treatment period (10 days in patients with CABP due to L. pneumophila or MRSA or in patients with S. pneumoniae and bacteremia); however, this was later adjusted to 7 days (except in confirmed MRSA cases, which continued to receive 10 days of treatment) to reduce medication errors and limit study site burden. In LEAP 2, patients received oral lefamulin 600 mg q12h (5 days) or moxifloxacin 400 mg q24h (7 days).
Patients eligible for enrollment included adults with radiographically diagnosed pneumonia, PORT risk class III‒V (LEAP 1) or II‒IV (LEAP 2), acute onset of ≥ 3 CABP symptoms (e.g., dyspnea), ≥ 2 vital sign abnormalities (e.g., tachycardia), and ≥ 1 other clinical sign or laboratory finding of CABP (e.g., hypoxemia). Exclusion criteria included receipt of > 1 dose of a short-acting CABP oral/IV antibacterial within 72 h before randomization, being at risk for major cardiac events or dysfunction, significant hepatic disease, and severely impaired renal function. Of note, not all patients with comorbidities were excluded; patients with DM, asthma/COPD, non-major cardiac events, elevated liver enzymes, and mild-to-moderate renal dysfunction were included and well represented in the LEAP 1 and LEAP 2 trials.
Study outcomes
In both studies, the US Food and Drug Administration (FDA) primary efficacy endpoint was early clinical response (ECR) at 96 ± 24 h after first study drug dose in the intent-to-treat (ITT) population (all randomized patients). Patients were programmatically classified as ECR responders if they were alive, showed improvement in ≥ 2 CABP symptoms, had no CABP symptom worsening, and received no nonstudy antibiotic for CABP treatment. Achievement of ECR criteria was also assessed at each study day, end of treatment (EOT; within 2 days after last study drug dose), test of cure (TOC; 5‒10 days after last study drug dose), and late follow-up (LFU; days 27‒34).
Secondary endpoints (European Medicines Agency primary endpoints) were investigator assessment of clinical response (IACR) at TOC in the modified ITT (mITT) and clinically evaluable (CE) populations. The mITT population included all randomized patients who received any study drug. The CE population comprised patients with no indeterminate clinical response, ≥ 48 h of study drug (unless patient died before 48 h), receipt of no nonstudy antibacterial potentially effective against CABP pathogens (unless administered for clinical failure), and no additional efficacy confounding factors. Investigator assessment classified patient response as a success if CABP signs/symptoms were resolved or improved such that no additional antibiotic was administered for the current CABP episode or as a failure if nonstudy antibiotics were administered or patient died from any cause. IACR success rates were also assessed at EOT and LFU.
Additional analyses included ECR and IACR assessments in subgroups based on baseline demographics and disease characteristics (Additional file 2: Table 1). Safety was assessed in all randomized patients who received any amount of study drug (safety population). Treatment-emergent adverse events (TEAEs) were defined as adverse events (AEs) that started/worsened during or after first study drug administration and were monitored at all study visits and by patient reporting. Additional safety assessments included vital signs, laboratory tests, and triplicate 12-lead electrocardiograms, which were performed within a 5-min interval at screening and on days 1 and 3 (LEAP 1) or days 1 and 4 (LEAP 2) to capture changes at the estimated maximum observed plasma concentration of study drug.
Statistical analyses
Pooled ECR and IACR analyses were evaluated using a 10% noninferiority margin; lefamulin noninferiority versus moxifloxacin was concluded if the lower 95% CI limit for the treatment difference exceeded − 10%. Treatment differences were weighted by study. The 95% CI was calculated using the Miettinen-Nurminen method [24], adjusted for study (ECR and IACR) and receipt of a prior single-dose short-acting antibiotic (IACR only), with the inverse variance of the effect size used for stratum weights. For subgroup analyses, descriptive CIs were determined but no noninferiority conclusions were made. If the treatment difference and CI were not estimable using these methods, observed treatment differences were reported and 95% CIs were calculated via unadjusted continuity-corrected Z-test.
Results
Patients
The pooled ITT population included 1289 patients randomized to lefamulin (n = 646) or moxifloxacin (n = 643). Detailed patient dispositions have been published elsewhere [20, 21]. Baseline demographic and disease characteristics were generally well balanced between treatment groups and reflected the general patient population with CABP (Table 1). Overall, 40.1% of patients were aged ≥ 65 years, 55.6% were male, 51.4% had impaired renal function, and 70.8% had PORT risk class ≥ III. Common comorbidities included hypertension (38.9%), asthma/COPD (18.0%), DM (13.0%), and CHF (10.2%). As expected, patients with PORT risk class IV/V were older and more likely to have comorbidities than patients with PORT risk class III. Among PORT risk class III and IV/V patients, 16.3% and 42.0% were aged ≥ 75 years, respectively. Compared with PORT risk class III patients, more PORT risk class IV/V patients had comorbidities such as renal impairment (53.5% vs 73.9%, respectively), hypertension (41.5%, 52.1%), asthma/COPD (16.4%, 29.4%), and DM (12.1%, 22.7%).
Clinical response/success
In the pooled ITT population, ECR rates were high (lefamulin 89.3%; moxifloxacin 90.5%; difference − 1.1; 95% CI − 4.4 to 2.2), and lefamulin was noninferior to moxifloxacin (Fig. 1a). Most patients (> 60%) met ECR criteria by day 3, with > 80% of patients in both treatment groups meeting ECR criteria by day 4; further increases through day 7 and sustained efficacy through LFU were also observed (Fig. 1b). Similarly, proportions of patients with resolution of all baseline CABP signs and symptoms also increased over time in both treatment groups (Fig. 2).
a ECR response in the pooled ITT population, b patients meeting ECR criteria by visit in the pooled ITT population, and IACR success by visit in the pooled c mITT and d CE populations. CE clinically evaluable, ECR early clinical response, EOT end of treatment, IACR investigator assessment of clinical response, ITT intent to treat, LFU late follow-up, mITT modified ITT, TOC test of cure
Lefamulin was also noninferior to moxifloxacin for IACR success (mITT and CE populations), with high and similar rates at TOC (Fig. 1c, d) for both lefamulin and moxifloxacin. IACR success rates at EOT and LFU were similarly high (> 83%) and consistent between treatment groups.
Lefamulin and moxifloxacin demonstrated high and similar ECR rates across various baseline demographic and disease characteristics, including patients with advanced age or comorbidities (asthma/COPD, DM, hypertension, CHF, arrhythmia, elevated liver enzymes) and regardless of PORT risk class (Fig. 3a). IACR success rates at TOC for both treatment groups were similarly high across most subgroups (Fig. 3b, c).
Subgroup analysis of a ECR in the pooled ITT population and IACR at TOC in the pooled b mITT and c CE populations. See Table 1 footnotes for subgroup definitions. ATS American Thoracic Society, CE clinically evaluable, COPD chronic obstructive pulmonary disease, ECR early clinical response, IACR investigator assessment of clinical response, ITT intent to treat, mITT modified ITT, PORT Pneumonia Outcomes Research Team, SIRS systemic inflammatory response syndrome
Safety
Within the pooled safety population (n = 1282), mean (SD) study drug exposure was 4.9 (1.5) days for lefamulin (n = 641) and 6.8 (1.1) days for moxifloxacin (n = 641) overall. This included patients who received IV treatment only (LEAP 1 patients; mean duration of 5.9 [2.0] days with lefamulin [n = 273] and 5.4 [1.9] days for moxifloxacin [n = 273]) or oral treatment only (LEAP 2 patients; 4.7 [1.1] days with lefamulin [n = 472] and 5.9 (1.8) days with moxifloxacin [n = 489]).
Overall TEAE rates were similar with lefamulin (34.9%) and moxifloxacin (30.4%; Table 2); most TEAEs were mild to moderate in severity and few patients (< 5%) experienced severe TEAEs. Treatment-related TEAEs were reported in 15.4% (lefamulin) and 10.6% (moxifloxacin) of patients, serious TEAEs in 5.6% and 4.8%, and TEAEs leading to study drug discontinuation in 3.1% and 3.3%. Over the entire study duration, 19 patients experienced TEAEs leading to death (lefamulin n = 11, moxifloxacin n = 8; Table 2). Among patients with common comorbidities, lefamulin and moxifloxacin demonstrated overall similar TEAE profiles to the overall population (Additional file 2: Tables 1‒3). Regardless of treatment group, the percentage of patients with severe TEAEs, serious TEAEs, and TEAEs leading to death increased with advancing age or PORT risk class.
The most frequently reported TEAEs in the lefamulin (13.1% [84/641]) and moxifloxacin (10.1% [65/641]) groups were GI. The most common individual TEAEs were diarrhea (7.3% [lefamulin] and 3.9% [moxifloxacin]), nausea (4.2%, 2.0%), and vomiting (2.3%, 0.6%) (Table 2), and most were mild to moderate in severity. Differences between the 2 treatment groups were driven primarily by GI events associated with oral dosing in the LEAP 2 study. Few patients discontinued study drug because of GI TEAEs (lefamulin, 0.5% [3/641]; moxifloxacin, 0.2% [1/641]). One case of Clostridium difficile infection was reported in a LEAP 2 patient successfully treated with lefamulin; onset occurred ~ 1 week after completing 5 days of lefamulin treatment, patient remained hospitalized, and infection resolved after oral vancomycin treatment.
Treatment-emergent adverse events (TEAEs) in the Medical Dictionary for Regulatory Activities system organ class (SOC) of cardiac disorders occurred in 2.5% (lefamulin) and 3.1% (moxifloxacin) of patients (Additional file 2: Table 4). After dosing, mean QT intervals corrected according to Fridericia (QTcF) increased from baseline in both treatment groups, although the mean (SD) maximum change from baseline was numerically smaller with lefamulin (16.9 [16.9] ms) than moxifloxacin (19.3 [17.7] ms). No associated cardiac arrhythmias of concern were observed. Among patients with history of hypertension or arrhythmia and those aged ≥ 65 years, TEAEs in the cardiac disorders SOC were reported at similar and low (≤ 10%) incidences in both treatment groups. Patients who experienced an increase from baseline in QTcF > 60 ms or QTcF value > 500 ms were similarly few and more frequent with moxifloxacin than lefamulin.
Among patients with elevated baseline liver enzymes and those aged ≥ 65 years, TEAEs in the hepatobiliary disorders SOC were similarly infrequent in both treatment groups (Additional file 2: Table 5). Within these patient subgroups, postbaseline elevated liver enzymes occurred in few patients, were similar with lefamulin and moxifloxacin, and resolved upon treatment discontinuation.
Discussion
This pooled analysis confirmed lefamulin clinical efficacy and its noninferiority to moxifloxacin for treatment of adults with CABP. Outcome rates were high with lefamulin and moxifloxacin, with observed ECR rates (i.e., at 96 ± 24 h) of ~ 90% and IACR success rates at EOT, TOC, and LFU of 83.2%‒93.4%. Patients achieved ECR responder criteria early during treatment and maintained clinical response through LFU. Consistent with published literature [25,26,27], complete resolution of all CABP clinical signs and symptoms lagged noticeably behind ECR and cessation of antimicrobial therapy, which may be attributed to the inflammatory nature of CABP and exacerbation of preexisting conditions (e.g., asthma/COPD) or smoking-associated disability [26]. Despite this lag, however, hospitalized patients in the LEAP studies achieved clinical improvement and stability by treatment day 3 and were discharge-ready (ie, improved in ≥ 2 cardinal CABP symptoms) by day 4 [28].
Lefamulin and moxifloxacin demonstrated high and similar ECR and IACR success rates across almost all patient subgroups, with a few exceptions that may be due to small sample sizes (e.g., patients with bacteremia) or unadjusted confounders (e.g., aged < 65 years, meeting American Thoracic Society minor criteria) [29]. Complex cases of patients at risk for poor efficacy or safety outcomes due to age or comorbidity were well represented, and subpopulation analyses demonstrated high lefamulin efficacy similar to that with moxifloxacin. Similar results were observed among patients with more severe disease (i.e., PORT risk class III‒V), although clinical response rates were numerically higher in patients with PORT risk class III versus IV/V.
Lefamulin was generally well tolerated. Compared with moxifloxacin, lefamulin was associated with more frequent GI-related TEAEs; however, these were all nonserious, manageable, and rarely led to discontinuation. Patients aged ≥ 65 years or with hypertension, arrhythmia, or elevated liver enzymes are generally at greater risk of adverse safety outcomes, but these data demonstrate a safety profile for lefamulin in these patient subgroups comparable to that of the overall population. When stratified by PORT risk class, lefamulin and moxifloxacin had similar safety profiles, with higher TEAE and serious TEAE rates in patients with PORT risk class IV/V versus III, consistent with the older and more comorbid demographic of PORT risk class IV/V patients. Furthermore, the favorable safety profile observed in PORT risk class III patients suggests that they may be candidates for outpatient treatment, consistent with current consensus guidelines [30].
Extensive nonclinical testing of lefamulin suggested a potential for QT prolongation, and further assessment in phase 1 studies of healthy volunteers demonstrated dose/exposure-related QT interval effects [19]. Consistent with these findings, mild QT prolongation was seen with clinically relevant lefamulin doses in this analysis, but observed effects were consistently numerically smaller than with moxifloxacin, although the implications of QT prolongation with lefamulin should continue to be examined in clinical practice. Lefamulin is not recommended for patients taking other drugs with known QT effects [19], and experts on long QT syndrome recommend performance of an electrocardiogram before and after starting therapy with any drug(s) that has a probable or possible association with QT prolongation [31].
Potential liver injury is a concern with multiple antibiotic classes, and most (eg, cephalosporins, fluoroquinolones, macrolides, tetracyclines) list hepatic enzyme elevation and other hepatic AEs in their package inserts [32,33,34]. Consistent with extensive nonclinical evaluations suggesting lefamulin is unlikely to result in substantial hepatotoxicity [35], these data show a favorable lefamulin safety profile, with low frequencies of transient hepatic enzyme elevations and TEAEs. Because the liver is a major elimination route for lefamulin (primarily via CYP3A4) [35], dosage adjustment is required for IV lefamulin in patients with severe hepatic impairment; oral lefamulin has not been studied in subjects with hepatic impairment and, based on available data, is not recommended in patients with moderate or severe hepatic impairment [19].
Study findings may be limited in their generalizability, as enrollment criteria may have excluded some patients typically seen in clinical practice such as those at risk for major cardiac events or dysfunction, patients with significant hepatic disease, and patients with severely impaired renal function. However, comorbidities common in patients presenting with CABP such as age, DM, a history of cardiovascular diseases (e.g., hypertension, CHF, or arrhythmia) or chronic lung diseases (e.g., asthma or COPD), elevated liver enzymes, or mild-to-moderate renal dysfunction were well represented in our analysis. Each of these comorbidities would be important for clinicians to consider when determining the intensity of care that a given patient with CABP will require. Similar to most contemporary antimicrobial clinical trials [36, 37], enrollment in these studies was largely outside of the United States because of challenges associated with prestudy antibiotic treatment and hospitalization duration [38]. However, a recent FDA analysis of geographic differences across antimicrobial clinical trials from 2001 to 2017 indicated broad similarities in demographic, clinical, and microbiological characteristics, which lessens generalizability concerns for these trials [39]. Subgroup analysis findings are limited by relatively low sample size such that important but infrequent AEs may not have been detected and randomization may not have adequately balanced prognostic factors. Lastly, the data include some random variation owing to the number of subgroups examined.
Conclusions
In this pooled analysis of 2 pivotal CABP studies, clinical response rates were high and similar with lefamulin and moxifloxacin, achieving rapid clinical response that was sustained through LFU. Lefamulin was generally well tolerated regardless of administration route, suggesting a favorable benefit-risk profile. Subgroup analyses suggest lefamulin may be a promising empiric monotherapy option for both inpatients and outpatients with CABP, including patients presenting with advanced age or various comorbidities. In light of rising antibacterial resistance with macrolides, tolerability concerns with other antibiotic classes (eg, fluoroquinolones, beta-lactams), and/or failure of other antibiotic options, lefamulin may provide a much-needed IV/oral empiric monotherapy alternative.
Availability of data and materials
The datasets generated and analyzed during the current study were used under license and are therefore not publicly available. However, data are available from the authors upon reasonable request.
Abbreviations
- AE:
-
Adverse event
- ATS:
-
American Thoracic Society
- BMI:
-
Body mass index
- BUN:
-
Blood urea nitrogen
- CABP:
-
Community-acquired bacterial pneumonia
- CE:
-
Clinically evaluable
- CHF:
-
Congestive heart failure
- COPD:
-
Chronic obstructive pulmonary disease
- CrCl:
-
Creatinine clearance
- CURB-65:
-
Confusion of new onset, BUN > 19 mg/dL, respiratory rate ≥ 30 breaths/min, systolic blood pressure < 90 mm Hg or diastolic blood pressure ≤ 60 mm Hg, and age ≥ 65 years
- DM:
-
Diabetes mellitus
- ECR:
-
Early clinical response
- EOT:
-
End of treatment
- FDA:
-
US Food and Drug Administration
- GI:
-
Gastrointestinal
- IACR:
-
Investigator assessment of clinical response
- ITT:
-
Intent to treat
- IV:
-
Intravenous
- LEAP:
-
Lefamulin Evaluation Against Pneumonia
- LFU:
-
Late follow-up
- MedDRA:
-
Medical Dictionary for Regulatory Activities
- mITT:
-
Modified intent to treat
- MRSA:
-
Methicillin-resistant Staphylococcus aureus
- PORT:
-
Pneumonia Outcomes Research Team
- q12h:
-
Every 12 h
- q24h:
-
Every 24 h
- QTcF:
-
QT interval corrected according to Fridericia
- SIRS:
-
Systemic inflammatory response syndrome
- SOC:
-
System organ class
- TEAE:
-
Treatment-emergent adverse event
- TOC:
-
Test of cure
- WBC:
-
White blood cell
References
Peyrani P, Mandell L, Torres A, Tillotson GS. The burden of community-acquired bacterial pneumonia in the era of antibiotic resistance. Expert Rev Respir Med. 2019;13(2):139–52.
McDermott KW, Elixhauser A, Sun R. Trends in hospital inpatient stays in the United States, 2005–2014: statistical brief #225. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Rockville, MD: Agency for Healthcare Research and Quality; 2017.
Xu J, Murphy SL, Kochanek KD, Arias E. Mortality in the United States, 2018. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. https://www.cdc.gov/nchs/data/databriefs/db355-h.pdf. Accessed 16 Jan 2021.
Cavallazzi R, Furmanek S, Arnold FW, et al. The burden of community-acquired pneumonia requiring admission to an intensive care unit in the United States. Chest. 2020;158(3):1008–16.
Welte T, Torres A, Nathwani D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax. 2012;67(1):71–9.
File TM, Marrie TJ. Burden of community-acquired pneumonia in North American adults. Postgrad Med. 2010;122(2):130–41.
Aujesky D, Fine MJ. The pneumonia severity index: a decade after the initial derivation and validation. Clin Infect Dis. 2008;47(suppl 3):S133–9.
Amalakuhan B, Echevarria KL, Restrepo MI. Managing community acquired pneumonia in the elderly - the next generation of pharmacotherapy on the horizon. Expert Opin Pharmacother. 2017;18(11):1039–48.
Ishiguro T, Takayanagi N, Yamaguchi S, et al. Etiology and factors contributing to the severity and mortality of community-acquired pneumonia. Intern Med. 2013;52(3):317–24.
Luna CM, Palma I, Niederman MS, et al. The impact of age and comorbidities on the mortality of patients of different age groups admitted with community-acquired pneumonia. Ann Am Thorac Soc. 2016;13(9):1519–26.
Vardakas KZ, Kalimeris GD, Triarides NA, Falagas ME. An update on adverse drug reactions related to β-lactam antibiotics. Expert Opin Drug Saf. 2018;17(5):499–508.
Mason JW. Antimicrobials and QT prolongation. J Antimicrob Chemother. 2017;72(5):1272–4.
Postma DF, Spitoni C, van Werkhoven CH, et al. Cardiac events after macrolides or fluoroquinolones in patients hospitalized for community-acquired pneumonia: post-hoc analysis of a cluster-randomized trial. BMC Infect Dis. 2019;19(1):17.
US Food and Drug Administration. FDA drug safety communication: FDA reinforces safety information about serious low blood sugar levels and mental health side effects with fluoroquinolone antibiotics; requires label changes. https://www.fda.gov/downloads/Drugs/DrugSafety/UCM612834.pdf. Accessed 16 Jan 2021.
US Food and Drug Administration. FDA drug safety communication: FDA warns about increased risk of ruptures or tears in the aorta blood vessel with fluoroquinolone antibiotics in certain patients. https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-increased-risk-ruptures-or-tears-aorta-blood-vessel-fluoroquinolone-antibiotics. Accessed 27 Aug 2020.
Jones SC, Budnitz DS, Sorbello A, Mehta H. US-based emergency department visits for fluoroquinolone-associated hypersensitivity reactions. Pharmacoepidemiol Drug Saf. 2013;22(10):1099–106.
Eyal Z, Matzov D, Krupkin M, et al. A novel pleuromutilin antibacterial compound, its binding mode and selectivity mechanism. Sci Rep. 2016;6:39004.
Schlünzen F, Pyetan E, Fucini P, Yonath A, Harms JM. Inhibition of peptide bond formation by pleuromutilins: the structure of the 50S ribosomal subunit from Deinococcus radiodurans in complex with tiamulin. Mol Microbiol. 2004;54(5):1287–94.
Xenleta™ (lefamulin). Full prescribing information, Nabriva Therapeutics US, Inc., King of Prussia, PA; 2019.
File TM Jr, Goldberg L, Das A, et al. Efficacy and safety of intravenous-to-oral lefamulin, a pleuromutilin antibiotic, for the treatment of community-acquired bacterial pneumonia: the phase III Lefamulin Evaluation Against Pneumonia (LEAP 1) trial. Clin Infect Dis. 2019;69(11):1856–67.
Alexander E, Goldberg L, Das AF, et al. Oral lefamulin vs moxifloxacin for early clinical response among adults with community-acquired bacterial pneumonia: the LEAP 2 randomized clinical trial. JAMA. 2019;322(17):1661–71.
Paukner S, Gelone SP, Arends SJR, Flamm RK, Sader HS. Antibacterial activity of lefamulin against pathogens most commonly causing community-acquired bacterial pneumonia: SENTRY antimicrobial surveillance program (2015–2016). Antimicrob Agents Chemother. 2019;63(4):e02161-e2218.
Waites KB, Crabb DM, Duffy LB, et al. In vitro activities of lefamulin and other antimicrobial agents against macrolide-susceptible and macrolide-resistant Mycoplasma pneumoniae from the United States, Europe, and China. Antimicrob Agents Chemother. 2017;61(2):e02008–e2016.
Miettinen O, Nurminen M. Comparative analysis of two rates. Stat Med. 1985;4(2):213–26.
Wootton DG, Dickinson L, Pertinez H, et al. A longitudinal modelling study estimates acute symptoms of community acquired pneumonia recover to baseline by 10 days. Eur Respir J. 2017;49(6):1602170.
Wyrwich KW, Yu H, Sato R, Powers JH. Observational longitudinal study of symptom burden and time for recovery from community-acquired pneumonia reported by older adults surveyed nationwide using the CAP Burden of Illness Questionnaire. Patient Relat Outcome Meas. 2015;6:215–23.
Metlay JP, Atlas SJ, Borowsky LH, Singer DE. Time course of symptom resolution in patients with community-acquired pneumonia. Respir Med. 1998;92(9):1137–42.
Lodise T, Colman S, Stein DS, et al. Post hoc assessment of time to clinical response among adults hospitalized with community-acquired bacterial pneumonia who received either lefamulin or moxifloxacin in 2 phase III randomized, double blind, double-dummy clinical trials. Open Forum Infect Dis. 2020;7(5):ofaa145.
File TM, Gelone SP, Schranz J, Alexander E. Reply to Tang and Lai. Clin Infect Dis. 2020;71(6):1583.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia: an official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200(7):e45–67.
Al-Khatib SM, LaPointe NM, Kramer JM, Califf RM. What clinicians should know about the QT interval. JAMA. 2003;289(16):2120–7.
Avelox® (moxifloxacin hydrochloride). Full prescribing information. Bayer HealthCare Pharmaceuticals Inc., Whippany, NJ; 2019.
Zithromax® (azithromycin dihydrate). Full prescribing information, Pfizer Inc, New York, NY; 2019.
Teflaro® (ceftaroline fosamil). Full prescribing information, Allergan USA, Inc., Madison, NJ; 2019.
US Food and Drug Administration, Center for Drug Evaluation and Research. Xenleta NDA/BLA multi-disciplinary review and evaluation. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2019/211672Orig1s000,%20211673Orig1s000MultidisciplineR.pdf. Accessed 27 Aug 2020.
Kaye KS, Bhowmick T, Metallidis S, et al. Effect of meropenem-vaborbactam vs piperacillin-tazobactam on clinical cure or improvement and microbial eradication in complicated urinary tract infection: the TANGO I randomized clinical trial. JAMA. 2018;319(8):788–99.
Wagenlehner FM, Umeh O, Steenbergen J, Yuan G, Darouiche RO. Ceftolozane-tazobactam compared with levofloxacin in the treatment of complicated urinary-tract infections, including pyelonephritis: a randomised, double-blind, phase 3 trial (ASPECT-cUTI). Lancet. 2015;385(9981):1949–56.
Spellberg B, Marr KA, Brass EP. Regulatory pathways for new antimicrobial agents: trade-offs to keep the perfect from being the enemy of the good. Clin Pharmacol Ther. 2016;100(6):597–9.
Bart SM, Farley JJ, Bala S, Amini T, Cox E. Geographic shifts in antibacterial drug clinical trial enrollment: implications for generalizability. Clin Infect Dis. 2021;72(8):1422–8.
Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(suppl 2):S27–72.
Li HY, Guo Q, Song WD, et al. Modified IDSA/ATS minor criteria for severe community-acquired pneumonia best predicted mortality. Medicine (Baltimore). 2015;94(36):e1474.
Acknowledgements
Editorial and medical writing support for manuscript development was provided by Lauriaselle Afanador, Ph.D., and Morgan C. Hill, Ph.D., employees of ICON (North Wales, PA), and funded by Nabriva Therapeutics.
Funding
This work was funded by Nabriva Therapeutics. Nabriva Therapeutics was responsible for the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation and review of the manuscript. Nabriva Therapeutics did not have the right to veto or suppress publication.
Author information
Authors and Affiliations
Contributions
TMF: Formal Analysis, Investigation, Drafting—Review & Editing; EA: Conception, Methodology, Formal Analysis, Drafting—Review & Editing, Supervision; LG: Conception, Methodology, Formal Analysis, Drafting—Review & Editing; AFD: Formal Analysis, Drafting—Review & Editing; CS: Formal Analysis, Drafting—Review & Editing; SP: Conception, Methodology, Formal Analysis, Drafting—Review & Editing; GJ: Formal Analysis, Investigation, Drafting—Review & Editing. All authors had access to the data and a role in writing the manuscript, have approved the submitted version, and agree both to be personally accountable for their own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which they were not personally involved, are appropriately investigated and resolved and the resolution documented in the literature. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
These trials were compliant with the ethical principles of the Declaration of Helsinki, Good Clinical Practice guidelines, and local laws/regulations. All patients provided written informed consent. Before study initiation, participating centers for the LEAP 1 and 2 trials obtained study approval from 130 ethics committees/institutional review boards; 100 are listed here (please see Additional file 1: Appendices 1 and 2 for the full list and details): Copernicus Group IRB; Western Institutional Review Board (WIRB); Minneapolis Medical Research Foundation, Human Subjects Research Committee; Appalachian Regional Healthcare Inc., IRB; Louisiana State University Health Sciences Center-Shreveport; Summa Health Institutional Review Board; Human Research Protection Office, Washington University in St. Louis; Veterans Memorial Medical Center Institutional Review Board; Institutional Ethics Review Board (LCP-IERB) Lung Center of the Philippines; University of the Philippines Research Manila Ethics Board (UPMREB); St. Luke’s Institutional Ethics Review Committee; Unified Biomedical Research Ethics Review Committee, West Visayas State University; Institutional Review Board of Bamrasnaradura Infectious Diseases Institute; Comité Institucional de Ética de la Investigación en Salud del Adulto; CIEIS del Niño y del Adulto; Comite Institutional de Etica de Investigacion en Salud (CIEIS); Comité de Ética del Instituto Médico Platense (CEDIMP); Comité de Ética del Sanatorio Británico; Comité de Ética en Investigación Hospital Italiano de La Plata; Comissão Nacional de Ética em Pesquisa—CONEP; Comitȇ de Ética em Pesquisa da Faculdade de Medicina de São José do Rio Preto—FAMERP; Comitȇ de Ética em Pesquisa da Universidade de Passo Fundo; Comitȇ de Ética em Pesquisa—CEP da Pontificia Universidade Católica de Campinas—PUC/Campinas; Comitȇ de Ética em Pesquisa da Santa Casa de Misericórdia de Belo Horizonte; Comité Institucional de Etica en Investigación de la Asociación Benéfica Prisma; Comite Institucional de Etica en Investigacion del Hospital Nacional Arzobispo Loayza; Agency for Medicinal Products and Medical Devices; Ethics Committee of the University Clinical Center Sarajevo; Ethics Committee of the University Clinical Hospital Mostar; Ethics Committee for Multi-Centre Trials; LEC of LTD Diagnostic Services; LTD “Medulla”—Chemotherapy and Immunotherapy Clinic; LTD “Acad. Vakhtang Bochorishvili Center of Sepsis and Infection Pathology”; NCLE”Internal Medicine Clinic of Georgian Patriarchate (for indigents) and its Development Fund”; Local Ethics Committee of LTD Emergency Cardiology Center by Academician G. Chapidze; Local Ethics Committee of LTD National Center for Tuberculosis and Lung diseases”; Egészségügyi Tudományos Tanács Klinikai Farmakológiai Etikai Bizottság; Országos Gyógyszerészeti és Élelmezés-egészségügyi Intézet (OGYÉI); The Ethics Committee for Clinical Trials of Medicinal Products; METC Maxima Medisch Centrum; Komisja Bioetyczna przy Okregowej Izbie Lekarskiej w Lodzi; Beskidzka Izba Lekarska; National Bioethics Committee for Medicine and Medical Devices; The Russian Federation Ministry of Healthcare, Department of State Regulation of Circulation of Medicines, Ethics Council; Ethics Expert Council at St. Petersburg State Budget Healthcare Institution “City Hospital No. 40 of Kurortniy Administrative District; Ethics Committee at SBHI of Novosibirsk Region “City Clinical Hospital of Emergency Medicine No. 2”; Independent Ethics Committee at FSBMEI of HPE “Military Medical Academy n.a. S.M. Kirov” MD of RF; Ethics Committee at State Budgetary Health Institution “Regional Clinical Hospital #4”; Ethics Committee at State Budget Institution of Healthcare of Yaroslavl Region “Regional Clinical Hospital”; Ethics Committee at SBEI HPE “Smolensk State Medical University” of the MoH of RF; LEC of Clinical Centre Kragujevac; LEC of Clinical Centre Serbia; LEC of Clinical Centre Nis; LEC of Institute for Pulmonary Diseases of Vojvodina; Pharma-Ethics Independent Research Ethics Committee; Commission on Ethics Questions of Municipal Institution of Health Care Kharkiv City Clinical Hospital # 13; Commission on Ethics Questions of Nation Military and Medical Clinical Centre “Main Military Clinical Hospital”; Commission on Ethics Questions of MI “Chernivtsi Regional Clinical Hospital”; Local Commission on Bioethics Questions of Regional Centre of Phthisiology and Pulmonology; Commission on Ethics Questions of SI “National Institute of Phthisiology & Pulmonology n.a. F. G.Yanovskyi of NAMS of Ukraine”; Commission on Ethics Questions of Municipal Institution Central City Hospital #1 City of Zhytomyr; Commission on Ethics Questions of Municipal Institution of Sumy Regional Council Sumy Regional Clinical Hospital; Commission on Ethics Questions of Municipal Institution “Kherson City Clinical Hospital n.a. A. and O. Tropinykh”; Commission on Ethics Questions of Municipal Institution “City Hospital #7”; Commission on Ethics Questions of Municipal Institution Odesa Regional Clinical Hospital; Commission on Ethics Questions of Municipal Institute 6th City Clinical Hospital; Olive View-UCLA Education & Research Institute; University of Virginia Institutional Review Board for Health Sciences Research (UVA IRB-HSR); Chesapeake IRB; Community Medical Centers Institutional Review Board; St. Rita’s Health Partners (SRHP); UC Davis IRB; Biomedical Research Alliance of New York IRB; Comité de Ética en Investigación del Hospital Universitario “Dr. José Eleuterio González”; Comité de Ética en Investigación de Accelerium S. de R.L. de C.V.; Comité de Ética en Investigación de Promotora Médica Aquascalientes, S.A. de C.V.; Comité de Ética en Investigación del Hospital Civil Fray Antonio Alcalde; Manila Central University Filemon D. Tanchoco Sr. Medical Foundation Institutional Review Board (MCU-FDT IRB); Hospital Ethics Committee Quirino Memorial Medical Center; Chong Hua Hospital Institutional Review Board; Institutional Review Board of The Catholic University of Korea, St. Paul’s Hospital; Institutional Review Board of Ewha Womans University Mokdong Hospital; Institutional Review Board of Yeungnam University Hospital; Institutional Review Board of The Catholic University of Korea, Uijeongbu St. Mary’s Hospital; Institutional Review Board of Konkuk University Medical Center; Institutional Review Board of Korea University Guro Hospital; Institutional Review Board of The Catholic University of Korea, Bucheon St. Mary’s Hospital; Kaohsiung Medical University Chung-Ho Memorial Hospital Institutional Review Board; Institutional Review Board of the E-DA Hospital; China Medical University & Hospital Research Ethics Committee; National Taiwan University Hospital Research Ethics Committee; Research Ethics Review Committee, Far Eastern Memorial Hospital; Comité de Ética en Investigación de CEMIC; Comité de Etica San Isidro—Instituto Medico de Alta Complejidad San Isidro; Comité Independiente de Ética para Ensayos en Farmacología Clínica CIEFC; Comité de Ética em Pesquisa em Seres Humanos da Fundacão Universidade de Passo Fundo—VRPPG; Comité Institucional de Ética en la Investigación del Hospital Nacional Cayetano Heredia; Comité de Ética Hospital Carlos Alberto Seguín Escobedo—EsSalud; Comité de Ética en Investigación Biomédica del Hospital Nacional Dos de Mayo; Comité de Ética Científica Servicio de Salud Araucanía Sur.
Consent for publication
Not applicable.
Competing interests
TMF has served as a consultant for bioMérieux, Curetis, Merck, Motif BioSciences, Nabriva Therapeutics, Paratek, Pfizer, and Shionogi Inc. and received grants from Nabriva Therapeutics. SP is an employee of/stockholder in Nabriva Therapeutics plc. EA and LG were employees of/stockholders in Nabriva Therapeutics plc at the time of the analysis. AFD has served as a consultant for Achaogen, AntibioTx, Boston Pharmaceuticals, Cempra, ContraFect, IterumTx, Nabriva Therapeutics, Paratek, Tetraphase, Theravance, UTILITY, Wockhardt, and Zavante. CS has served as a consultant for Allergan and Nabriva Therapeutics, received grants from the National Institutes of Health and the Health Resources & Services Administration, and received nonfinancial support from the State of California. GJM has received grants from ContraFect and Nabriva Therapeutics.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Independent Ethics Committees and Institutional Review Boards.
Additional file 2.
Supplemental Tables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
File, T.M., Alexander, E., Goldberg, L. et al. Lefamulin efficacy and safety in a pooled phase 3 clinical trial population with community-acquired bacterial pneumonia and common clinical comorbidities. BMC Pulm Med 21, 154 (2021). https://doi.org/10.1186/s12890-021-01472-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-021-01472-z