Abstract
Background
Acute exacerbation (AE) of idiopathic pulmonary fibrosis (IPF) is devastating with no established treatment. This phenomenon involves disordered coagulation and excessive inflammatory reactions. As recombinant human soluble thrombomodulin (rhsTM) possesses anti-coagulative and anti-inflammatory properties, the medicine is expected to improve the prognosis of the disease. The aim of this study was to summarize current evidence regarding benefits and harms of rhsTM treatment for AE of IPF.
Method
Patients with AE of IPF were eligible for the review and all of the other types of interstitial pneumonias were excluded. The effect of rhsTM treatment on the outcomes such as all-cause mortality was estimated in comparison to conventional therapy. Primary studies of any design aside from a case report were reviewed. Electronic databases such as Medline and EMBASE were searched from 2002 through August 14, 2019. Two reviewers independently selected eligible reports and extracted relevant data. A risk of bias of individual studies was assessed similarly. Meta-analysis was conducted for univariate results if at least three studies were available for the same outcome.
Result
Out of a total of 390 records identified, eight studies were first deemed eligible and four of them were finally focused for the review. Only one study was a prospective trial and a historical control was employed in all studies. An overall risk of bias was rated as serious in three out of four studies. A total of 169 subjects were included. Two out of three studies that reported 3-month all-cause mortality by univariate analysis demonstrated beneficial effects of rhsTM treatment and a pooled analysis demonstrated that rhsTM treatment improved 3-month all-cause mortality with a risk ratio of 0.50 (95% confidence interval (CI): 0.35–0.72). All two studies reporting multivariate results demonstrated that rhsTM treatment improved 3-month all-cause mortality with odds ratios of 0.21 (95% CI: 0.05–0.91) and 0.25 (95% CI: 0.09–0.68), respectively. There were no serious adverse events.
Conclusion
The rhsTM treatment was demonstrated to improve 3-month all-cause mortality of AE of IPF with no serious adverse events. However, these findings should be interpreted with caution due to a small number of studies and serious risk of bias.
Similar content being viewed by others
Background
Idiopathic pulmonary fibrosis (IPF) is the most common type of interstitial pneumonia (IP) with unknown aetiology that is categorized as chronic fibrosing interstitial pneumonia (CFIP) alongside of idiopathic non-specific interstitial pneumonia (NSIP) [1]. IPF is a progressive disease and depicts the dismal clinical course with an estimated survival time of 2 to 3 years after its diagnosis [2]. The predominant cause of deaths of the disease is an acute exacerbation (AE), which is reported to be responsible for 40% of the cases [3]. AE of IPF was initially defined as acute respiratory worsening beyond its usually anticipated gradual progression triggered by no identifiable causes [4]. Subsequently, this overwhelming phenomenon was noted to be not unique to IPF but also complicate other types of IPs such as idiopathic NSIP, connective tissue disease-associated interstitial pneumonia (CTD-IP) and chronic hypersensitivity pneumonitis [5,6,7]. Although the frequency of AE and its prognosis varies depending on underlying IPs [5,6,7], IPF is the most prevalent among others [8], and the prognosis of AE of IPF is uniformly poor with 90-day mortality of 40 to 50% [9]. This devastating outcome is mostly because the pathogenesis of this phenomenon has yet to be fully elucidated and there is currently no established treatment that has been proved beneficial [10]. Therefore, it is urgent to develop a new therapeutic strategy to address substantial clinical burden caused by AE of IPF and improve the prognosis of the disease.
Recombinant human soluble thrombomodulin (rhsTM) is a relatively new medicine that uses the technology of cloning [11]. It consists of an extracellular domain of native thrombomodulin, a transmembrane glycoprotein expressed on the endothelial cell surface [12]. This rhsTM binds to thrombin to form a thrombin-thrombomodulin complex that activates protein C, which in turn, plays an important role in regulating both coagulation and inflammation [13]. Although it was first approved as a therapeutic agent for disseminated intravascular coagulation (DIC) in Japan [14], previous reports demonstrated that it could also improve respiratory indexes and the mortality of acute respiratory distress syndrome (ARDS) with DIC [15, 16]. There are pathophysiological similarities between AE of IPF and ARDS, which are characterized by a pathological pattern of diffuse alveolar damage (DAD), and disordered coagulative state and excessive inflammation [4, 17]. Although research on the potential of rhsTM treatment for AE of IPF has reported some promising results, the effect of rhsTM treatment on AE of IPF remains unclear. Therefore, the aim of this systematic review was to summarize current accumulating evidence regarding benefits and harms of rhsTM treatment for AE of IPF.
Methods
This study was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [18].
Eligibility criteria
Subjects
Patients with AE of IPF were eligible for the review. Idiopathic NSIP was not included in this study because there has been no clear evidence that the prognosis of AE of idiopathic NSIP is the same as that of AE of IPF although it constitutes CFIP alongside of IPF [19]. IPF was diagnosed based on previously published joint statement of American Thoracic Society/European Respiratory Society/Japanese Respiratory Society/Latin American Thoracic Association (ATS/ERS/JRS/ALAT) or its recent update [10, 20]. Other types of idiopathic interstitial pneumonias (IIPs) such as cryptogenic organizing pneumonia (COP) and unclassifiable interstitial pneumonia were also excluded as they are known to demonstrate a different clinical course or might include undiagnosed IPs [1]. Similarly, secondary IPs such as CTD-IP and chronic hypersensitivity pneumonitis were also excluded due to different disease entities although AE of these diseases may pathophysiologically be similar to that of IPF [6, 7]. AE of IPF was diagnosed based on the previous report by Idiopathic Pulmonary Fibrosis Clinical Research Network [4] or the guideline published by the Japanese Respiratory Society [21]. Specifically, it was defined as worsening or development of dyspnoea manifested within 30 days, which is accompanied by newly emerging bilateral ground glass opacities and/or consolidation superimposed on underlying usual interstitial pneumonia (UIP) on high resolution computed tomography (HRCT) scan. Although heart failure or volume overload needed to be excluded for the diagnosis of the disease, other causes such as infection, pulmonary thromboembolism and aspiration were accepted as the triggering factors of this condition complying with the recent update of the diagnostic criteria for AE of IPF by the international working group [22]. AE at the first visit without any prior information of chronic IP was accepted if chronic interstitial changes of UIP were confirmed radiologically and/or pathologically and there were no apparent causes. Only the first episode of AE was considered for the review.
Intervention
The rhsTM (Asahi Kasei Pharma Corporation, Tokyo, Japan) was administered at a dose of 0.06 mg/kg/day or 380 U/kg/day for 6 days based on the approved dosage of the medicine [14, 23]. Conventional therapy included all of the other therapeutic options aside from rhsTM treatment such as corticosteroid, immunosuppressive drugs and anti-fibrotic agents. There were no restrictions regarding baseline therapy and the usage of other anticoagulants.
Outcome
The primary outcome of interest was all-cause mortality. The secondary outcomes of interest were disease-related mortality, oxygenation, discharge from a medical institution, health-related quality of life and adverse events such as bleeding and other coagulative abnormalities. The mortality was determined at 1 month, 3 months, 6 months and 1 year after the diagnosis of the disease. The 28-day or 30-day mortality and the 90-day mortality were designated as the 1-month mortality and the 3-month mortality, respectively.
Study type
Primary studies of any design except for a case report were eligible for the review if it compared a group receiving rhsTM treatment with a control group receiving conventional therapy without rhsTM treatment. Study designs were not limited to randomized controlled trials (RCTs) but observational studies were also included. There were no restrictions as to the number of included subjects and follow-up periods. Editorials, letters, review articles and conference proceedings were not considered. No language restrictions were implemented.
Search strategy
Literature was searched through the following electronic databases, i.e., Medline (Ovid), EMBASE (Ovid), Science Citation Index Expanded (Web of Science), Cochrane Central Register of Controlled Trials (Cochrane Library), ClinicalTrials.gov, Google Scholar and ICHUSHI (the largest bibliographic database for medicine in Japan by Japan Medical Abstracts Society). Search was conducted on the 14th of August, 2019 and covered from 2002 as the current classification for IIPs was published in that year [24]. A string of search terms was constructed referring to previous reviews of the same topic [25, 26], which included ‘interstitial lung disease’, ‘acute exacerbation’ and ‘thrombomodulin’ (Additional file 1).
Study selection and data extraction
Two reviewers (HK and OMP) independently screened retrieved records by titles and abstracts as well as full-texts if needed to select eligible reports. The same reviewers extracted relevant data similarly referring to a previous review of a similar subject [27]. These data included the first author’s name and publication year, study location, number of subjects and their demographic features in each treatment group, prior therapy and conjunctive treatment for AE, outcomes, number of subjects who developed the outcome, summary statistics and adverse events related to rhsTM treatment. Any disagreement in the selection of articles and data extraction was resolved by discussion between the reviewers. Authors were contacted to request for additional information if there was missing data for relevant outcomes.
Risk of bias assessment
Two reviewers (HK and OMP) independently assessed risk of bias of individual studies using a tool called risk of bias in non-randomised studies of interventions (ROBINS-I) [28]. This tool is composed of 8 domains that are closely related to the bias of non-randomised studies. Each domain was rated as low, moderate, serious or critical and an overall risk of bias was determined based on the assessment of each domain.
Statistical analysis
For binary outcomes the effect of rhsTM treatment was estimated as a risk ratio (RR), which was calculated based on the absolute number of the outcomes in each treatment group while continuous outcomes were summarized by a mean difference (MD). The results were statistically combined if there were three or more studies available that reported the same outcome. Meta-analysis was conducted by Mantel-Haenszel method using a fixed effect model on statistical software, Review Manager (RevMan) Version 5.3 (Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014). Only univariate results were combined and multivariate results were reported qualitatively because variables in a multivariate model were to be diverse between studies. All results were reported with the 95% confidence interval (CI) and deemed statistically significant with p-value < 0.05. Heterogeneity between studies was estimated using the Q statistic and I2. Statistical significance of the test for heterogeneity was confirmed with p-value < 0.1 due to the low power of the test. I2 was interpreted as not important (< 30%), moderate (≥30 < 50%), substantial (≥50 < 70%) and considerable (≥70%) based on the Cochrane Handbook for Systematic Reviews of Interventions [29]. Subgroup analysis and sensitivity analysis were to be conducted focusing on study location (Asia/non-Asia) and studies with a similar risk of bias, respectively. Small study bias such as publication bias was to be examined graphically by a funnel plot and statistically by the Egger’s test if ten or more studies were available for meta-analysis [30].
Results
Selection of eligible studies
Out of a total of 390 records identified through a search of seven electronic databases, eight reports/studies were first deemed eligible after excluding 91 duplicates, 77 ineligible records, 198 irrelevant articles and 16 other reports (Fig. 1). Two out of eight studies (Isshiki 2015 [31], Sakamoto 2018 [32]) were conducted by the same research group. Because the latter study was an extension from the former study, only the result of the latter report was considered for further analysis. One study (Arai 2019 [33]), which was composed of a total of 100 subjects including both IPF and non-IPF, was excluded from further analysis because non-IPF group did not undergo pathological diagnosis although all cases in the group were non-IPF IIPs according to the authors (personal communication). Additionally, two studies (Abe 2015 [34], Abe 2016 [35]) were also not considered for further analysis because the former study included idiopathic NSIP in conjunction with IPF and the latter study included radiologically possible UIP, which was not confirmed by surgical lung biopsy. As a result, the remaining four studies were focused for the review.
Study flow diagram. Out of a total of 390 records identified through a search of seven electronic databases, 299 records after removing 91 duplicates were screened by titles and abstract, which identified 77 ineligible records (9 conference proceedings, 51 review articles, 10 case reports and 7 editorials or letters) and 198 irrelevant reports. Out of the remaining 24 records, 7 records were excluded, which were composed of 3 records that were retrieved through Google Scholar but unable to be identified due to unavailable links and unclear source information, 1 registered trial that was on-going without any result available and 3 non-English articles (1 German and 2 Bulgarian) that were unable to be interpreted due to lack of resources. The remaining 17 articles were retrieved as full-texts and 9 of them were excluded due to no description of a specific treatment in 6 articles and a different target disease in 3 articles. Finally, eight reports/studies were deemed eligible for the review
Characteristics of included studies
All of the included studies were conducted by Japanese research groups. One study was a prospective trial (Hayakawa 2016 [36]) whereas the other studies were retrospective observations. All studies compared a group with rhsTM treatment with a historical control without rhsTM treatment (Sakamoto 2018 [32], Hayakawa 2016 [36], Tsushima 2014 [37], Kataoka 2015 [38]) (Table 1). Out of a total of 169 subjects included in the review, 95 subjects were allocated to rhsTM treatment while 74 subjects received conventional therapy without rhsTM treatment. The mean or median age of the treatment group ranged from 73.2 to 76.2 years while that of the control group was between 69.7 and 75 years. Over 80% of subjects were men in both groups. Baseline therapy before AE was reported in three studies (Sakamoto 2018 [32], Hayakawa 2016 [36], Kataoka 2015 [38]). In the rhsTM treatment group an anti-fibrotic agent (pirfenidone) was prescribed to 16 patients, corticosteroid to 14 patients and immunosuppressive drugs to 6 patients while in the control group 9, 13 and 3 patients received these medicines, respectively. The rhsTM was administered at a dose of 0.06 mg/kg/day for 6 days in three studies (Sakamoto 2018 [32], Tsushima 2014 [37], Kataoka 2015 [38]) while a dose of 380 U/kg/day was administered for 7 days in the remaining study (Hayakawa 2016 [36]). In one study (Kataoka 2015 [38]) the rhsTM treatment group was followed by low molecular weight heparin (LMWH) treatment for the median duration of 8 days while the control group received only LMWH treatment for the median of 10 days. In another study (Sakamoto2018 [32]) only six patients in the control group received LMWH treatment with a dose of 75 IU/kg/day for 14 days (no comparative data available between rhsTM treatment and LMWT). Other conjunctive therapeutic agents administered for AE included steroid pulse therapy for all patients and immunosuppressive agents for a total of 112 patients (Table 1). There was no significant difference in distributions of potential prognostic factors for AE of IPF between rhsTM treatment group and control group (Table 2).
Risk of bias in individual studies
An overall risk of bias was deemed low in one study (Kataoka 2015 [38]) whereas that of the other three studies was rated as serious (Sakamoto 2018 [32], Hayakawa 2016 [36], Tsushima 2014 [37]). This different finding was largely due to the bias assessment of confounding domain, which was sufficiently addressed using a propensity score in the former study. However, it was inadequately explained or not considered at all in the other three studies (Table 3).
Effect of recombinant human soluble thrombomodulin (rhsTM) treatment
Univariate analysis
All four studies reported all-cause mortality using univariate analysis, which was described as 28-day mortality in two studies, 3-month mortality in three studies and 1-year mortality in one study (Table 4).
The 1-month all-cause mortality was significantly better in rhsTM treatment group than control group with an RR of 0.42 (95% CI: 0.21–0.84) in one study (Tsushima 2014 [37]) whereas there was no statistically significant difference with an RR of 0.65 (95%CI: 0.21–1.98) in the other study (Hayakawa 2016 [36]). The mortality was 35.0 and 30% in rhsTM treatment group whereas it was 83.0 and 46% in control group in these two studies, respectively (Table 4).
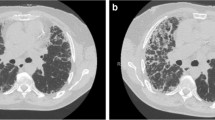
The 3-month all-cause mortality was significantly better in rhsTM treatment group than control group in two studies (Sakamoto 2018 [32], Kataoka 2015 [38]) whereas there was no statistically significant difference in the other study (Hayakawa 2016 [36]). The mortality ranged from 30.0 to 40% in rhsTM treatment group whereas it was between 62.9 and 85% in control group (Table 4). A pooled analysis of three studies yielded a statistically significant result with an RR of 0.50 (95% CI: 0.35–0.72) with no heterogeneity (chi2 = 0.12, df = 2, p = 0.94, I2 = 0) (Fig. 2).
3-month all-cause mortality. A total of three studies reported 3-month all-cause mortality using univariate analysis, which included 143 subjects. A total of 25 out of 75 patients (33.3%) in rhsTM treatment group died within 3 months while 46 out of 68 patients (67.6%) in control group died within the same period of time. A pooled analysis of three studies demonstrated that 3-month all-cause mortality was significantly better in rhsTM treatment group than control group with an RR of 0.50 (95% CI: 0.35–0.72) with no heterogeneity (chi2 = 0.12, df = 2, p = 0.94, I2 = 0)
There was no statistically significant difference of 1-year mortality between rhsTM treatment group and control group in one study (Hayakawa 2016 [36]). A total of 6 out of 10 patients (60%) in rhsTM treatment group died within 1 year whereas 92% of 13 patients died in control group, which yielded an RR of 0.65 (95% CI: 0.38–1.10) (Table 4).
Although subgroup analysis and sensitivity analysis could not be performed due to a small number of included studies, one study with low risk of bias demonstrated an improvement of 3-month all-cause mortality with an RR of 0.46 (95% CI: 0.22–0.97) (Kataoka 2015 [38]), which was similar to the results of the other two studies with serious risk of bias that demonstrated RRs of 0.53 (95% CI: 0.33–0.86) and 0.47 (95% CI: 0.21–1.05) (Sakamoto 2018 [32], Hayakawa 2016 [36]), respectively (Table 4).
Another outcome of interest reported was a change in the respiratory index in one study (Hayakawa 2016 [36]). There was a statistically significant difference of an improvement in the partial pressure of arterial oxygen to fraction of inspired oxygen (PaO2/FiO2) ratio on day 8 after commencing the rhsTM treatment with an MD of 21.0 (95% CI: 12.9–29.1) (Table 4).
Small study bias such as publication bias could not be evaluated due to a small number of included studies.
Multivariate analysis
Two studies reported all-cause mortality using multivariate analysis. A propensity score was employed to adjust for confounding factors in one study (Kataoka 2015 [38]) whereas there was no explanation of adjusted factors in another study (Sakamoto 2018 [32]). The rhsTM treatment significantly improved 3-month all-cause mortality with odds ratios (ORs) of 0.21 (95% CI: 0.05–0.91) and 0.25 (95% CI: 0.09–0.68) in these two studies (Kataoka 2015 [38], Sakamoto 2018 [32]), respectively (Table 4).
Adverse events
Adverse events related to rhsTM treatment were described in three studies including one study, in which no side effects were detected (Hayakawa 2016 [36]). There were one case each of haemosputum and deep venous thrombosis in one study (Kataoka 2015 [38]), both of which were improved after discontinuation or change of the treatment. Another study (Sakamoto 2018 [32]) reported a patient with both haemoptysis and haematuria, which resolved spontaneously. No severe bleeding or coagulopathy were reported (Table 4).
Discussion
This systematic review and meta-analysis demonstrated beneficial effects of rhsTM treatment on 3-month all-cause mortality of AE of IPF based on combined results of univariate analysis although its effect on 1-month mortality was inconsistent between studies. This finding was confirmed by the results of multivariate analysis in all studies that reported it. Furthermore, oxygenation was significantly improved after rhsTM treatment although it was reported in only one study. Finally, rhsTM treatment was considered safe and tolerable as only a few cases of minor bleeding and one thrombotic event were developed.
AE of IPF is characterised pathologically by damage to alveolar epithelial cells and surrounding capillary vasculature, i.e., DAD superimposed on chronic fibrotic interstitial changes [39]. DAD is not unique to AE of IPF but recognized as a common pathological finding manifested in severe respiratory illnesses resulting from intrinsic or extrinsic excessive insult to the lung such as ARDS [40]. Although the exact pathogenesis of AE of IPF remains unclear, it is reported to involve massive inflammatory reactions as well as disordered coagulation and fibrinolysis that lead to the characteristic hyaline membrane formation in DAD [39]. Thrombomodulin is a transmembrane glycoprotein present on the endothelial cell surface of the body and plays a pivotal role in regulating coagulation cascade [41]. It binds to thrombin to form thrombin-thrombomodulin complex in the blood vessel and enhances the activation of protein C, which in turn, suppresses the activated coagulation factor V and VIII with the aid of protein S and reduces further thrombin formation to control coagulative state [41]. As activated protein C possesses anti-inflammtory, cytoprotective and anti-apoptotic properties through the modulation of the transcription of pro-inflammatory mediators [42], thrombomodulin also indirectly involves host defence mechanism through this pathway [43]. Furthermore, thrombomodulin expresses anti-inflammation irrespective of the protein C pathway. It directly binds to high motility group box 1 (HMGB1) secreted by inflammatory cells and Lewis Y antigen in lipopolysaccharide on gram-negative bacteria [44], by which it prevents these molecules from interacting with their own receptors and suppresses the signal transduction to the down-stream pro-inflammatory pathway [45]. As an elevation of serum HMGB1 was noted in patients with acute lung injury [46] and a higher level of the molecule is reported to predict shorter survival of patients with AE of IPF [47], thrombomodulin, which plays a role in controlling the effect of HMGB1, may be essential in the pathogenesis of the disease.
Previous studies demonstrated that thrombomodulin is excessively secreted into bloodstream in severe illnesses such as sepsis and ARDS [48, 49]. Thrombomodulin was also reported to be elevated in bronchoalveolar lavage fluid (BALF) and shown to correlate with the prognosis of AE of IP [50]. This soluble thrombomodulin molecule detached from the endothelial cell surface may be unduly generated by proteolytic cleavage of the protein, which is mediated by a wide range of proteases augmented under these critical circumstances [48]. The soluble form of thrombomodulin may lack its full-brown property due to the breakdown of the molecule at various dimensional sites although some previous studies reported that it might remain functionally active [51]. However, at least the soluble thrombomodulin may insufficiently activate protein C due to little engagement of endothelial protein C receptor that is noted to boost the reaction on the endothelial cell surface [43]. Furthermore, it is reported that the transcription of thrombomodulin is suppressed and the expression of the molecule on the endothelium is reduced in severe clinical conditions such as ARDS and AE of IPF [48, 52]. As a result, accelerated inflammatory reactions in conjunction with unprotected thrombotic state would continue to injure respiratory system as well as other organs in these critical conditions.
The rhsTM was constructed through a cloning technique, which consists of extracellular domains of native thrombomodulin [12]. Since it carries anti-inflammatory and anti-coagulative property, it is expected to ameliorate both disintegrated inflammation and coagulation manifested in systemic inflammatory disorders and improve the prognosis of the disease [13]. The rhsTM treatment was first approved for clinical use in Japan based on the result of a small trial that depicted beneficial effects of rhsTM treatment on DIC triggered by hematologic malignancy and sepsis [14]. However, a similar efficacy of rhsTM treatment for sepsis-associated coagulopathy was not confirmed in a recent RCT that was conducted by international multi-institutions [53]. In addition, the latest systematic review and meta-analysis did not reveal the advantage of rhsTM treatment for sepsis-induced DIC [54]. Conversely, only a small number of studies reported the effect of rhsTM treatment on DIC complicated with ARDS. One study reported an improvement of lung injury score with rhsTM treatment [15] and another study demonstrated improved in-hospital mortality [16]. However, all of these studies were of retrospective design and no RCTs have been conducted to elucidate the efficacy of rhsTM treatment for ARDS. Although this current review demonstrated that rhsTM treatment could improve all-cause mortality of AE of IPF, it was based on a small number of low-quality studies. In short, a high-quality study reported non-significant results of rhsTM treatment for sepsis-associated coagulopathy [53] whereas a small number of low-quality studies demonstrated its possibly anecdotal beneficial effects on ARDS and AE of IPF [15, 16]. Therefore, clinicians should refrain from implementing rhsTM treatment in their daily practice. Furthermore, the recombinant human activated protein C (rhAPC), which formerly emerged as a promising medicine for sepsis or acute lung injury, was eventually removed from the market due to lack of beneficial effects confirmed by a large-scale RCT [55]. Biologically the mechanism of action of rhAPC constitutes the properties of rhsTM treatment [43]. Therefore, it may be too soon to be optimistic that rhsTM treatment is beneficial for AE of IPF although it seems to be a reasonable therapeutic option, in particular, under the current suffocating circumstances where there has been no established effective treatment for AE of IPF [10].
There are some of limitations that need to be kept in mind to appropriately interpret the findings of this review. Firstly, this review was composed of only four studies and most of these studies included a small sample with less than 50 subjects. Two studies (Arai 2019 [33], Abe 2016 [35]) were excluded from detailed analysis because both of these studies included IIPs with possible UIP pattern on HRCT without surgical lung biopsy, which possibly might have led to the inclusion of non-IPF cases. Therefore, the reports may be anecdotal and small study bias is likely to exist although it could not be evaluated due to a small number of included studies. However, prognosis of AE of non-IPF IIPs and AE of other fibrotic interstitial lung diseases is similarly poor to that of AE of IPF [19, 33]. The rhsTM treatment might be effective for AE of non-IPF IIP cases as was suggested in the report of Arai et al. [33] although additional trials are needed for a definitive conclusion. Secondly, only one study in this review was a prospective trial whereas the other studies were retrospective observations. In addition, the use of historical control employed in all studies is a major concern. Although a propensity score was introduced in one study to adjust for baseline differences, there remains a certain factor that may impact the prognosis of the disease but cannot be statistically handled, e.g., a change of care for patients with AE of IPF over time. In fact, the mortality of a control group in individual studies of this review was substantially high with 3-month mortality ranging from 62.9 to 85% in comparison to 40% in a recent report [9]. Therefore, a study design with a historical control may have distorted the true effect of rhsTM treatment. Thirdly, only two studies conducted multivariate analysis. As a result, most of the studies constituting this review were rated as serious in risk of bias assessment. Lastly, all studies in this review were conducted in Japan. As a result, the generalizability of the findings is limited. In particular, as Japanese patients are reported to be more susceptible to drug-induced IP [56] and other types of rapidly progressive IP [57], the effect of rhsTM treatment may vary depending on the ethnic background. Therefore, a large-scale international RCT is necessary to address these limitations and confirm the efficacy of rhsTM treatment for AE of IPF. To this end, one randomized placebo-controlled trial was undertaken in Japan and recently completed (NCT02739165) [58]. The result of this trial is expected to provide a conclusive finding. However, the true effect of rhsTM treatment may not be clarified due to its small sample size, i.e., only 74 subjects in total. In a previous trial of rhAPC for ARDS that enrolled around 70 subjects, the authors mentioned that underpowering could not be excluded to explain their negative result [59] and a larger trial with around 1600 subjects was required to obtain a definitive conclusion [55]. Therefore, whatever the result will be in this recent RCT, a larger-scale international trial will be required to confirm the finding.
Conclusion
In this systematic review and meta-analysis, the rhsTM treatment was demonstrated to improve 3-month all-cause mortality of AE of IPF. It was considered safe and tolerable with only minor adverse effects. However, these findings need to be interpreted with caution due to a small number of studies, serious risk of bias and limited generalizability.
Availability of data and materials
The dataset used and/or analyzed during the current study will be available from the corresponding author on a reasonable request after the final result is published in a journal.
Abbreviations
- AE:
-
Acute exacerbation
- ARDS:
-
Acute respiratory distress syndrome
- BALF:
-
Bronchoalveolar lavage fluid
- CFIP:
-
Chronic fibrosing interstitial pneumonia
- CI:
-
Confidence interval
- COP:
-
Cryptogenic organizing pneumonia
- CTD:
-
Connective tissue disease
- DAD:
-
Diffuse alveolar damage
- DIC:
-
Disseminated intravascular coagulation
- HMGB1:
-
High motility group box 1
- HR:
-
Hazard ratio
- HRCT:
-
High resolution computed tomography
- IIP:
-
Idiopathic interstitial pneumonia
- IP:
-
Interstitial pneumonia
- IPF:
-
Idiopathic pulmonary fibrosis
- LMWH:
-
Low molecular weight heparin
- MD:
-
Mean difference
- NSIP:
-
Non-specific interstitial pneumonia
- OR:
-
Odds ratio
- PaO2/FiO2:
-
Partial pressure of arterial oxygen to fraction of inspired oxygen
- PRISMA:
-
Preferred reporting items for systematic review and meta-analyses
- RCT:
-
Randomized controlled trial
- rhAPC:
-
Recombinant human activated protein C
- rhsTM:
-
Recombinant human soluble thrombomodulin
- ROBINS-I:
-
Risk of bias in non-randomised studies of interventions
- RR:
-
Risk ratio
- UIP:
-
Usual interstitial pneumonia
References
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188:733–48.
American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. International consensus statement. American Thoracic Society (ATS), and the European Respiratory Society (ERS). Am J Respir Crit Care Med. 2000;161:646–64.
Ley B, Collard HR, King TE Jr. Clinical course and prediction of survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2011;183:431–40.
Collard HR, Moore BB, Flaherty KR, et al. Acute exacerbations of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2007;176:636–43.
Park IN, Kim DS, Shiin TS, et al. Acute exacerbation of interstitial pneumonia other than idiopathic pulmonary fibrosis. Chest. 2007;132:214–20.
Suda T, Kaida Y, Nakamura Y, et al. Acute exacerbation of interstitial pneumonia associated with collagen vascular diseases. Respir Med. 2009;103:846–53.
Olson AL, Huie TJ, Groshong SD, et al. Acute exacerbations of fibrotic hypersensitivity pneumonitis: a case series. Chest. 2008;134:844–50.
Song JW, Hong SB, Lim CM, et al. Acute deterioration in idiopathic pulmonary fibrosis: causes, risk factors, and outcomes. Respirology. 2009;3:A167.
Suzuki A, Taniguchi H, Ando M, et al. Prognostic evaluation by oxygenation with positive end-expiratory pressure in acute exacerbation of idiopathic pulmonary fibrosis: a retrospective cohort study. Clin Respir J. 2018;12:895–903.
Raghu G, Collard HR, Egan JJ, et al. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183:788–824.
Gomi K, Zushi M, Honda G, et al. Antithrombotic effect of recombinant human thrombomodulin on thrombin-induced thromboembolism in mice. Blood. 1990;75:1396–9.
Nakashima M, Kanamaru M, Umemura K, et al. Pharmacokinetics and safety of a novel recombinant soluble human thrombomodulin, ART-123, in healthy male volunteers. J Clin Pharmacol. 1998;38:40–4.
Maruyama I. Recombinant thrombomodulin and activated protein C in the treatment of disseminated intravascular coagulation. Thromb Haemost. 1999;82:718–21.
Saito H, Maruyama I, Shimazaki S, et al. Efficacy and safety of recombinant human soluble thrombomodulin (ART-123) in disseminated intravascular coagulation: results of a phase III, randomized, double-blind clinical trial. J Thromb Haemost. 2007;5:31–41.
Ogawa Y, Yamakawa K, Ogura H, et al. Recombinant human soluble thrombomodulin improves mortality and respiratory dysfunction in patients with severe sepsis. J Trauma Acute Care Surg. 2012;72:1150–7.
Uba T, Nishi K, Takeshi O, et al. The influence of human soluble recombinant thrombomodulin on in-hospital mortality in patients with acute respiratory distress syndrome and disseminated intravascular coagulation: a retrospective multicenter study. J Intensive Crit Care. 2017;3:40.
Ware LB, Matthay MA. The acute respiratory distress syndrome. N Engl J Med. 2000;342:1334–49.
Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Suzuki A, Kondoh Y, Brown KK, et al. Acute exacerbations of fibrotic interstitial lung diseases. Respirology. 2019. https://doi.org/10.1111/resp.13682.
Raghu G, Remy-Jardin M, Myers JL, et al. Diagnosis of idiopathic pulmonary fibrosis: an official ATS/ERS/JRS/ALAT clinical practice guideline. Am J Respir Crit Care Med. 2018;198:e44–68.
Taniguchi H, Kondoh Y. Revised criteria for acute exacerbation of idiopathic pulmonary fibrosis. Annu Rep Study Group Minist Health Welf Diffuse Lung Dis. 2004:114–9.
Collard HR, Ryerson CJ, Corte TJ, et al. Acute exacerbation of idiopathic pulmonary fibrosis. An international working group report. Am J Respir Crit Care Med. 2016;194:265–75.
Hagiwara A, Tanaka N, Uemura T, et al. Can recombinant human thrombomodulin increase survival among patients with severe septic-induced disseminated intravascular coagulation: a single-Centre, open-label, randomised controlled trial. BMJ Open. 2016;6:e012850.
American Thoracic Society. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2002;165:277–304.
Qiu M, Chen Y, Ye Q. Risk factors for acute exacerbation of idiopathic pulmonary fibrosis: a systematic review and meta-analysis. Clin Respir J. 2017;23:23.
Yamakawa K, Aihara M, Ogura H, et al. Recombinant human soluble thrombomodulin in severe sepsis: a systematic review and meta-analysis. J Thromb Haemost. 2015;13:508–19.
Kamiya H, Panlaqui OM. A systematic review of the efficacy of direct hemoperfusion with a polymyxin B-immobilized fibre column to treat rapidly progressive interstitial pneumonia. SAGE Open Med. 2019;7:2050312119861821.
Sterne JA, Hernan MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration 2011. Available from: http://www.handbook.cochrane.org.
Egger M, Davey Smith G, Schneider M, et al. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Isshiki T, Sakamoto S, Kinoshita A, et al. Recombinant human soluble thrombomodulin treatment for acute exacerbation of idiopathic pulmonary fibrosis: a retrospective study. Respir. 2015;89:201–7.
Sakamoto S, Shimizu H, Isshiki T, et al. Recombinant human soluble thrombomodulin for acute exacerbation of idiopathic pulmonary fibrosis: a historically controlled study. Respir Investig. 2018;56:136–43.
Arai T, Kida H, Ogata Y, et al. Recombinant thrombomodulin for acute exacerbation in idiopathic interstitial pneumonias. Respirology. 2019;24:658–66.
Abe M, Tsushima K, Matsumura T, et al. Efficacy of thrombomodulin for acute exacerbation of idiopathic pulmonary fibrosis and nonspecific interstitial pneumonia: a nonrandomized prospective study. Drug Des Devel Ther. 2015;9:5755.
Abe T, Yokomura K, Goto A, et al. Efficacy of recombinant human thrombomodulin α in acute exacerbation of idiopathic pulmonary fibrosis. Nihon Kokyuki Gakkai Zasshi. 2016;5:57–63.
Hayakawa S, Matsuzawa Y, Irie T, et al. Efficacy of recombinant human soluble thrombomodulin for the treatment of acute exacerbation of idiopathic pulmonary fibrosis: a single arm, non-randomized prospective clinical trial. Multidscip Respir Med. 2016;11:38.
Tsushima K, Yamaguchi K, Kono Y, et al. Thrombomodulin for acute exacerbations of idiopathic pulmonary fibrosis: a proof of concept study. Pulm Pharmacol Ther. 2014;29:233–40.
Kataoka K, Taniguchi H, Kondoh Y, et al. Recombinant human thrombomodulin in acute exacerbation of idiopathic pulmonary fibrosis. Chest. 2015;148:436–43.
Churg A, Wright JL, Tazelaar HD. Acute exacerbations of fibrotic interstitial lung disease. Histopathol. 2011;58:525–30.
Parambil JG, Myers JL, Aubry MC, et al. Causes and prognosis of diffuse alveolar damage diagnosed on surgical lung biopsy. Chest. 2007;132:50–7.
Esmon CT. The regulation of natural anticoagulant pathways. Sci. 1987;235:1348–52.
Mosnier LO, Zlokovic BV, Griffin JH. The cytoprotective protein C pathway. Blood. 2007;109:3161–72.
Esmon CT. The interactions between inflammation and coagulation. Br J Haematol. 2005;131:417–30.
Li YH, Kuo CH, Shi GY, et al. The role of thrombomodulin lectin-like domain in inflammation. J Biomed Sci. 2012;19:34.
Okamoto T, Tanigami H, Suzuki K, et al. Thrombomodulin: a bifunctional modulator of inflammation and coagulation in sepsis. Crit Care Res Pract. 2012;2012:614545.
Ueno H, Matsuda T, Hashimoto S, et al. Contributions of high mobility group box protein in experimental and clinical acute lung injury. Am J Respir Crit Care Med. 2004;170:1310–6.
Yamaguchi K, Iwamoto H, Sakamoto S, et al. Serum high-mobility group box 1 is associated with the onset and severity of acute exacerbation of idiopathic pulmonary fibrosis. Respirology. 2020;25:275–80. https://doi.org/10.1111/resp.13634.
Faust SN, Levin M, Harrison OB, et al. Dysfunction of endothelial protein C activation in severe meningococcal sepsis. N Engl J Med. 2001;345:408–16.
Orwoll BE, Spicer AC, Zinter MS, et al. Elevated soluble thrombomodulin is associated with organ failure and mortality in children with acute respiratory distress syndrome (ARDS): a prospective observational cohort study. Crit Care. 2015;19:435.
Suzuki A, Taniguchi H, Kondoh Y, et al. Soluble thrombomodulin in bronchoalveolar lavage fluid is an independent predictor of severe drug-induced lung injury. Respirology. 2017;22:744–9.
Esmon CT. The roles of protein C and thrombomodulin in the regulation of blood coagulation. J Biol Chem. 1989;264:4743–6.
Ebina M, Taniguchi H, Miyasho T, et al. Gradual increase of high mobility group protein b1 in the lungs after the onset of acute exacerbation of idiopathic pulmonary fibrosis. Pulm Med. 2011;2011.
Vincent JL, Francois B, Zabolotskikh I, et al. Effect of a recombinant human soluble thrombomodulin on mortality in patients with sepsis-associated coagulopathy: the SCARLET randomized clinical trial. JAMA. 2019;321:1993–2002.
Yamakawa K, Murao S, Aihara M. Recombinant human soluble thrombomodulin in sepsis-induced coagulopathy: an updated systematic review and meta-analysis. Thromb Haemost. 2019;119:56–65.
Ranieri VM, Thompson BT, Barie PS, et al. Drotrecogin alfa (activated) in adults with septic shock. N Engl J Med. 2012;366:2055–64.
Inokuma S. Leflunomide-induced interstitial pneumonitis might be a representative of disease-modifying antirheumatic drug-induced lung injury. Expert Opin Drug Saf. 2011;10:603–11.
Koga T, Fujikawa K, Horai Y, et al. The diagnostic utility of anti-melanoma differentiation-associated gene 5 antibody testing for predicting the prognosis of Japanese patients with DM. Rheumatol. 2012;51:1278–84.
Clinical study of ART-123 for the treatment of acute exacerbation of idiopathic pulmonary fibrosis. http://clinicaltrials.gov/ct2/show/NCT02739165?cond =Thrombomodulin&rank=3. Accessed 23 September 2019.
Cornet AD, Groeneveld AB, Hofstra JJ, et al. Recombinant human activated protein C in the treatment of acute respiratory distress syndrome: a randomized clinical trial. PLoS One. 2014;9:e90983.
Acknowledgements
Not applicable
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HK planned the entire research project and analyzed data. He also summarized the result and wrote the manuscript. HK has full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the analysis.
OMP made contributions in conceiving the research project. He was also engaged in literature search, data extraction and risk of bias assessment. OMP provided thoughts and opinions to a draft paper and approved of the final version of the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
These were waived as this study was only based on the summary result of previously published articles and individual patient data was not obtained or accessed.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Search terms for each electronic database.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kamiya, H., Panlaqui, O.M. The efficacy of recombinant human soluble thrombomodulin (rhsTM) treatment for acute exacerbation of idiopathic pulmonary fibrosis: a systematic review and meta-analysis. BMC Pulm Med 20, 57 (2020). https://doi.org/10.1186/s12890-020-1092-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-020-1092-3