Abstract
Background
Since the beginning of SARS-CoV-2 outbreak in China, severe acute respiratory syndrome has been widely descripted. Hemoptysis has rarely been observed in SARS-CoV-2 infection.
We report here a case of severe hemoptysis in post-tuberculosis bronchiectasis precipitated by SARS-CoV-2 infection and managed in a referral center.
Case presentation
A 58-year-old man was admitted to our intensive care unit for severe hemoptysis with history of post-tuberculosis bronchiectasis. At ICU admission the patient had fever and severe acute respiratory failure requiring high flow oxygen therapy. Respiratory tract sampling was positive for SARS-CoV-2. Multi-detector computed tomography angiography pointed out localized bronchiectasis on the left lower lobe and enlarged left bronchial and phrenic arteries; bronchial arteriography with distal embolization was performed with favorable outcome and no bleeding recurrence.
Conclusions
To our knowledge, this is the first case of acute exacerbation of bronchiectasis related to SARS-CoV-2 infection and complicated by severe hemoptysis. Whether the virus may play a role in the dysregulation of airway haemostasis, and contribute to episodes of hemoptysis in patients with chronic pulmonary diseases and predisposing factors might be investigated.
Similar content being viewed by others
Background
Severe hemoptysis remains a challenging condition for physicians because of the variety of etiologies and a large panel of clinical presentation. Acute lower respiratory tract infection is one of the conditions of severe hemoptysis in chronic pulmonary disease, acting like an acute bronchial inflammation trigger. Since the beginning of SARS-CoV-2 outbreak in China, severe acute respiratory syndrome has been widely descripted [1,2,3] and hemoptysis has rarely been observed in this condition [1, 2, 4, 5].
We report here a case of acute exacerbation of post-tuberculosis bronchiectasis precipitated by SARS-CoV-2 infection complicated by severe hemoptysis and managed in a referral center.
Case presentation
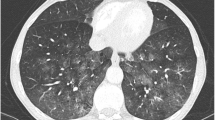
A 58-year-old man was admitted to our intensive care unit (ICU) for severe hemoptysis. He had a history of post-tuberculosis bronchiectasis responsible for several episodes of hemoptysis of low abundance 3 years ago that resolved with medical measures. He was treated by rivaroxaban for a pulmonary embolism diagnosed within the two preceding months. Three days before ICU admission, he presented fever, cough, increased expectoration, shortness of breath, myalgia and asthenia. He had not travelled in Asia, but reported a contact in the preceding week with a colleague who had been tested positive for SARS-CoV-2. He presented acute massive hemoptysis (> 200 ml) with increased dyspnea and was referred to the Emergency Department of our hospital. A multi-detector computed tomography angiography pointed out poorly defined disseminated centrilobular nodules associated with localized bronchiectasis in the left lower lobe, enlarged left bronchial (Fig. 1a) and phrenic (Fig. 1b) arteries. On ICU admission, the patient had fever (39 °C) and severe acute respiratory failure requiring high flow oxygen therapy. Respiratory tract sampling was positive for SARS-CoV-2, without any bacterial or viral co-infection. Respiratory tract culture was negative for Aspergillus sp and Mycobacterium tuberculosis. Fungal sensitization was also considered but serum Aspergillus-specific IgE level was low.
Other relevant biochemical parameters were assessed: CRP was measured at 256 mg/ L, lactate dehydrogenase level was low 237 UI/ L and D-Dimere level was 1228 ng/ mL.
The anti Xa activity was measured at 20 ng/ml. A bronchial arteriography with distal embolization of both left bronchial and phrenic arteries was performed, using micro coils. Bleeding did not recur thereafter, and the outcome was favorable with no complications of the vascular interventional procedure, and hospital discharge at D14.
Discussion and conclusions
Severe acute respiratory syndrome is known to be caused by SARS-CoV-2 since the beginning of the outbreak in December 2019 in China [1,2,3]. Hemoptysis has been rarely reported during SARS-CoV-2 infection [1, 2, 4, 5] (Table 1).
Acute lower respiratory tract infection related to bacteria or virus is one of the conditions of severe hemoptysis, and may threaten life. In our case, the radiological pattern of SARS-CoV-2 pneumonia was consistent with a viral bronchial and pulmonary involvement, as already described, and slightly differed from that of the typical bilateral multi-lobar ground glass opacities with peripheral or posterior distribution (see Figure in Electronic Supplemental Material, ESM).
The patient had a history of post-tuberculosis bronchiectasis, pulmonary embolism and oral anticoagulation: these are all common risk factors for hemoptysis.
In our case the clinical presentation was consistent with influenza-like illness and the high abundance of bleeding differed from patient’s previous bronchiectasis exacerbations: all these observations might suggest here the role of SARS-CoV-2 as precipitating but not coincidental factor in this exacerbation.
In our opinion and in accordance with recent studies [1, 2, 4, 5] (Table 1), SARS-CoV-2 infection should not been considered as a common general risk factor of hemoptysis but could be a precipitating factor of chronic pulmonary disease exacerbation with hemoptysis.
One may hypothesize that the virus may have triggered acute bronchial inflammation and exacerbation of the chronic bronchial disease, ultimately leading to the rupture of the regional hyper vascularization of enlarged systemic arteries associated with bronchiectasis.
To our knowledge, this is the first case reported of acute exacerbation of post-tuberculosis bronchiectasis precipitated by SARS-CoV-2 infection and complicated by severe hemoptysis. Whether the virus may play a role in the dysregulation of airway haemostasis, and contribute to episodes of hemoptysis in patients with chronic pulmonary diseases and predisposing factors might be investigated.
Availability of data and materials
All data are presented in the manuscript.
Abbreviations
- ICU:
-
Intensive care unit
- CRP:
-
C-reactive protein
References
Guan W-J, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020. https://doi.org/10.1056/NEJMoa2002032.
Huang C, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet Lond Engl. 2020;395:497–506.
Wang D, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA. 2020. https://doi.org/10.1001/jama.2020.1585.
Chen T, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ. 2020;368:m1091.
Xu X-W, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606.
Acknowledgements
Not applicable.
Patient data
Authors confirm that the patient has not been reported in any other submission.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
JL and GV had full access to all the data and take responsibility for the integrity of the data. JL and MT drafted the manuscript. AM participated in the image acquisition and interpretation. MF and GV revised the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Authors confirm that the patient gave oral and written consent for his personal and clinical details along with any identifying images to be published in this study.
Competing interests
Authors have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Figure Axial CT section showing localized bronchiectasis on the lower left lobe (blue arrow) and viral involvement with ground glass opacities (red arrow).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lopinto, J., Teulier, M., Milon, A. et al. Severe hemoptysis in post-tuberculosis bronchiectasis precipitated by SARS-CoV-2 infection. BMC Pulm Med 20, 244 (2020). https://doi.org/10.1186/s12890-020-01285-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12890-020-01285-6