Abstract
Background
Hypertension remains a major global health challenge, including in low- and middle-income countries. In Rwanda, a lack of adequate information and healthcare services impacts healthcare-seeking behaviors, contributing to undiagnosed hypertension in rural areas. Therefore, the need to determine its prevalence and associated factors.
Methods
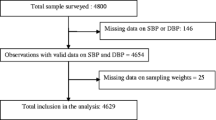
A cross-sectional study was conducted with 393 adults in the Ndera Sector, of Rwanda’s Gasabo District, through a multistage sampling technique. Data was gathered using the WHO STEP-wise approach to non-communicable disease risk factor surveillance (STEPS) questionnaire; physical examination was done to determine blood pressure and body-mass index (BMI), after which the data collected was analyzed using SPSS. Newly diagnosed hypertension was determined when on two different intervals, systolic blood pressure readings was > 140 mmHg, and/or the diastolic blood pressure readings was > 90 mmHg, in the absence of previous hypertension diagnosis.
Results
The overall prevalence of hypertension among patients at Ndera sector was 15%, all of which were newly diagnosed. The mean (SD) age of the participants was 37 (13.7) years and half (53%) were women. The mean systolic blood pressure for men was 124.3 mmHg compared to 120.9 mmHg for women (p = 0.043, 95%CI: 0.12–6.74). Women had a significantly higher mean BMI (26.0) compared to men (22.8) (p < 0.001, 95%CI: -4.18 - -2.31). Age (χ² = 37.400, p < 0.001), residence (χ² = 10.200, p < 0.001), BMI (χ² = 22.1, p < 0.001), and lack of knowledge about hypertension (χ² = 25.1, p < 0.001) were the factors with significantly undiagnosed hypertension.
Conclusions
The high prevalence of undiagnosed hypertension in Ndera Sector is linked to gender, older age, higher BMI, location, and lack of hypertension knowledge. These findings call for multifaceted approaches, combining educational initiatives, geographical targeting, lifestyle modifications, and policy implementations, all aimed at mitigating the burden of undiagnosed hypertension and enhancing community health within the Ndera Sector.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Non-communicable diseases (NCDs) are the leading cause of mortality worldwide and represent an emerging global health threat [1]. It is estimated that 41 million deaths are attributed to NCDs, which accounts for 71% of the annual global mortality rate [2]. Among these, hypertension is a major public health challenge and the most substantial risk for cardiovascular diseases (CVDs), affecting around one-billion people globally in 2008, with a projected increase to 1.5 billion by 2025 [3]. In 2021 ,approximately 1.3 billion people worldwide suffer from hypertension, with two-thirds living in low- or middle-income countries and 46% of these individuals are unaware of their condition [4] .
Hypertension, commonly known as high blood pressure, is diagnosed when systolic blood pressure readings are consistently ≥ 140 mmHg and/or the diastolic blood pressure readings is ≥ 90 mmHg at two different intervals [4]. The diagnosis of hypertension is made according to these standard measures, using a blood pressure monitor by a physician or other healthcare staff [5] .
In Africa, hypertension is the leading cause of cardiovascular disease deaths. Sub-Saharan Africa (SSA), which comprises low- and middle-income countries (except for high income Seychelles), is experiencing a double disease burden from both communicable diseases and NCDs like hypertension [6]. The prevalence of hypertension in SSA varies from 5 to 50%, depending on the country, with a significant increase observed over recent decades [7]. A systematic review and meta-analysis revealed a high prevalence of hypertension among individuals of 60 years and above in Africa, even in rural populations, contributing to 57% of overall prevalence [8] .
In Rwanda, the 2021 NCD STEP-wise survey reported that 16.2% of the population had hypertension, with an expected increase to 17.8% by the year 2025 due to factors such as imbalanced diets, physical inactivity, tobacco use, alcohol abuse, age and family history [9]. The Rwanda Biomedical Center (RBC) estimates that, of the over one million people with high blood pressure, only 8,000 (less than 1%) are enrolled in clinics, indicating that 99% of the population living with hypertension do not have access to diagnosis and treatment [10]. Almost all individuals with hypertension remain undiagnosed, untreated, or only partially treated, exacerbating the cardiovascular disease burden in the region [10]. For example, it is estimated that 46% of adults with hypertension in Ethiopia are undiagnosed [7] .
Undiagnosed hypertension is defined as having hypertension without being informed by health professionals [11]. Often termed the ‘‘silent killer,’’ hypertension typically presents symptoms only after causing permanent organ damage. This asymptomatic nature leads to a significant discrepancy between available community prevalence data and hospital based data [3] .
In rural parts of Rwanda, a study among 155 participants in 2019 found a high proportion (42%) of undiagnosed hypertension, with gender, age, and alcohol consumption being significantly associated factors [12]. The Ndera Sector is the third most populated sector in Kigali, is predominantly rural [13]. Urban residents have greater access to hypertension information through interventions like mass campaigns and free NCD risk factors screenings organized by the city of Kigali including car free days to encourage physical activity [14]. Conversely, rural areas like the Ndera Sector lack these opportunities [6] .
Despite the importance of determining the prevalence of undiagnosed hypertenion, there is a paucity of literature on undiagnosed hypertension among Rwandan’s 72.1% rural populations [13], .
This study aimed to determine the prevalence of undiagnosed hypertension and its associated factors in Ndera Sector, Gasabo District, Rwanda so as to inform the development of effective strategies for the prevention, early detection, management and monitoring of hypertension in Rwanda, ultimately improving public health outcomes.
Methods
Study site & population
A cross-sectional study was conducted in Bwiza Cell, Cyaruzinge Cell, and Kibenga Cell of Ndera Sector of Gasabo District, in Rwanda, in 2023, through a structured questionnaire and physical examination. Ndera Sector, largely a rural area, is the third most populated sector of 15 sectors in Kigali that make up Gasabo District, with a population of 95,164, as indicated by the Rwanda Population and Housing Census 2022 [13] .
Inclusion criteria
The study included participants aged 18 years and above with the following characteristics: not known to be hypertensive, voluntarily accepted to participate in the study, had no medical conditions such as gestational hypertension. In the last 30 min prior to the investigation, there should have been no physical activity, no caffeine or stimulant intake.
Exclusion criteria
The study excluded pregnant women above 20 weeks of gestation, those who had a diagnosed mental disorder and those with hearing and/or speaking disabilities due to either communication problems or incoherent answers to the eligibility criteria questionnaire.
Sample size calculation and sampling technique
The sample size was determined using Taro Yamane’s calculation formula [15]. Accordingly, the sample size drawn from the study population was 393 participants. A multistage sampling technique was then used to select three cells among six cells that make up Ndera Sector, which are Bwiza Cell, Cyaruzinge Cell, and Kibenga Cell. This is because Ndera Sector is a highly populated area. Thus, it was difficult and impractical to survey the entire population directly. In addition, Bwiza, Cyaruzinge, and Kibenga Cells are the most highly populated cells, with a population size of 22,001 adults aged 18 and above.
Where n = sample size,
N = population size = 22,001.
e = margin of error (0.05), and.
Reliability level is 95%,
In the first stage of the multistage sampling technique, a list of all the villages of the three selected cells of Ndera Sector was obtained from the National Institute of Statistics of Rwanda [15], and was used as a sampling frame for a random selection of enumeration areas (EAs) within each study cell. The Probability Proportional to Size (PPS) sampling method was also applied to select three EAs in each study cell randomly; thus, the selection was based on the size of EAs. In the second stage, the number of villages to be sampled in each EA was determined by dividing the total sample size by the total number of EAs selected. These villages were then selected from each of the identified EAs using a systematic random sampling method. Finally, in the third stage, all eligible participants aged 18 years and above were randomly selected from each cell and enrolled in the study.
Data collection
The standardized WHO STEP-wise approach V.3.2 tool designed for surveillance of non-communicable disease (WHO STEPS) [16], was used. The WHO STEPS for NCD risk factors surveillance consists of gathering information on socio-demographic characteristics and key risk factors using a set of questions, as well as physical measurements of blood pressure, height, and weight. The questionnaire was developed in English and was translated into the local language (Kinyarwanda).
A structured closed-ended questionnaire for socio-demographics and medical history was administered to participants, and a physical examination was performed to determine participants’ blood pressure and body-mass index (BMI). Participants’ information on sociodemographic variables (e.g. age, sex, marital status, cell of residence, education level), behavioural and lifestyle factors (e.g. physical activity, consumption of additional salt, smoking, alcohol consumption), and physical measurements (e.g. blood pressure, height, weight) was collected .
Before official data collection began, the structured questionnaire underwent a pilot test in one of the cells (Bwiza Cell) not included in the study to assess its psychometric properties. This pilot test was conducted to ensure the validity and reliability of the questionnaire. Content, construct, and face validity were evaluated through participant feedback and expert review. Subsequent necessary corrections were made to improve the questionnaire’s accuracy and consistency. This process ensured that the instrument was well-suited for the official data collection phase. Blood pressure was measured using an automated clinically validated blood pressure machine. Blood pressure measurements were taken at two separate time points and were performed by clinicians for validation. Participants were asked to rest (relax) in a chair for 30 min before measurement, with their legs not crossed and with their feet on the floor to support their back. Participants were also required to have an empty bladder, not to smoke, and not to drink coffee or tea. The upper arm was exposed two inches above the crease of the elbow. The blood pressure cuff was applied to the brachial artery on the upper arm. Two blood pressure measurements were taken three minutes apart in a sitting position; this is the standard practice in Rwanda. The mean of the two readings was taken to determine the blood pressure status of the participants.
Anthropometric measurements were performed using standard procedures (as prescribed by WHO STEPs ) and calibrated instruments (clinically validated machines to measure weight, height, and blood pressure). Participants’ weight was recorded to the nearest 0.1 kg, and the height was also measured using a portable stadiometer and recorded to the nearest 0.1 cm [17]. With this information, BMI was calculated using the height and weight measurements [18, 19].
Data analysis
Descriptive statistics were used to summarize the prevalence of undiagnosed hypertension and the sociodemographic characteristics of the study population. Namely, we summarised the frequency of individuals in our population that belonged to various age groups, sexes, marital statuses, cells of residence, education levels, physical activity level, consumption of additional salt, smoking, and alcohol consumption. SPSS (statistical package for the social science) program version 21 was used for data entry and analysis [20].
Several variables were included in subsequent bivariate analysis (Chi-squared) to understand the prevalence of undiagnosed hypertension and its association with socio-demographic factors (namely age groups, sexes, marital statuses, cells of residence, education levels, physical activity level, consumption of additional salt, smoking, and alcohol consumption). Chi-squared analysis was chosen to investigate associations between each aforementioned sociodemographic variable and the outcome of interest, separately.
In the data analysis process, the study employed a significance level, utilizing p-values, to determine the strength of associations between variables. During bivariate association calculations (Chi-square), a p-value cut-off of 0.05 was set to determine statistical significance. The utilization of this specific p-value cut-off contributed to the precision and reliability of the findings, allowing for the identification of meaningful patterns and associations in the context of undiagnosed hypertension prevalence.
Dependent variable
Newly diagnosed High Blood Pressure: This is the main outcome variable of the study, representing the proportion of individuals in the Ndera Sector with systolic blood pressure readings on two different intervals being > 140 mmHg, and / or the diastolic blood pressure readings being > 90 mmHg, but have not been previously diagnosed with hypertension. Undiagnosed hypertension was determined when someone met the aforementioned criteria for high blood pressure [21].
Independent variables (Associated Factors)
-
1.
Age: The age of the participants may influence the prevalence of undiagnosed hypertension, as hypertension is known to be more prevalent among older individuals.
-
2.
Gender: Gender differences might play a role in hypertension rates, and the study explored whether the prevalence varies between males and females.
-
3.
Marital Status: Marital status may have an influence on lifestyle habits and social support, potentially affecting hypertension prevalence.
-
4.
Lifestyle Factors: These may include variables such as smoking, alcohol consumption, self-reported regular physical activity, and dietary habits, which can influence hypertension rates.
-
5.
Body Mass Index (BMI): BMI could be relevant as obesity is a known risk factor for hypertension.
Ethical considerations
The research study adhered to the ethical principles [22]. Ethical approval was obtained from the Institutional Review Board (IRB) of the University of Rwanda and Kibagabaga District Hospital (Gasabo approval reference No: 1294/KBGH_EC/2023, UR CMHS reference No: CMHS/IRB/433/2023). The study followed the guidelines and regulations of these institutions, ensuring the protection of participants’ rights and confidentiality. Informed consent was obtained from all participants.
Results
The mean age of the participants was 36.8 years (SD = 13.7), with an age range from 18 to 82 years. The age distribution revealed that most participants were young adults, with 31.3% aged 25–34 years, followed by 26.2% aged 35–44 years. Participants aged 18–24 and 45–54 years each constituted 18.1% and 12.2% of the sample, respectively, while those aged 55 years and above also represented 12.2%. Regarding sex distribution, there was a higher representation of females (57.3%) compared to males (42.7%). Marital status data showed that over half of the participants (52.9%) were currently married, while 35.9% had never married. A smaller proportion of the sample were divorced (4.6%), separated (6.1%), or widowed (0.5%). The participants were distributed across three cells within the sector, with Bwiza hosting the largest share of the sample (36.6%), followed by Kibenga (34.1%) and Cyaruzinge (29.3%). Educational attainment among participants varied, with nearly half (49.4%) having completed primary school. Secondary school education was completed by 41.0% of the participants, while 5.3% had attained university education. A minority (4.3%) had no formal schooling (Table 1).
Table 2 provides the breakdown of behavioral patterns and dietary habits among the respondents within the study focused on undiagnosed hypertension in Ndera sector, Gasabo district, Rwanda. The data reveals that physical activity levels vary within the community, with 41% reporting engagement in regular physical activity, defined as exercise at least 3 times 30 min a week. Regarding salt consumption, there’s a notable variation in habits, with a significant portion (38.9%) reporting additional salt intake, followed by 31.3% who mention never adding extra salt to their meals. Smoking appears to be infrequent within this population, with only 2% reporting as smokers defined as smoking cigarettes every day. However, alcohol consumption is more prevalent, with 33.1% of respondents admitting to alcohol intake defined as drinking alcohol like beer, wine, and more over the past 12 months. These findings shed light on the diverse behavioral and dietary practices within the community of persons with undiagnosed hypertension, underscoring the need considering these varied habits when addressing undiagnosed hypertension.
Table 3 presents the bivariate analysis of blood pressure and BMI according to sex. The mean systolic blood pressure for men was 124.3 mmHg, compared to 120.9 mmHg for women, with a mean difference of 3.4 mmHg (p = 0.043, 95% CI: 0.12–6.74), indicating a statistically significant difference. Conversely, the mean diastolic blood pressure was slightly higher in women (80.1 mmHg) than in men (78.3 mmHg), but this difference was not statistically significant (mean difference = -1.8 mmHg, p = 0.101, 95% CI: -4.03–0.36). Regarding BMI, women had a significantly higher mean BMI (26.0) compared to men (22.8), with a mean difference of -3.2 (p < 0.001, 95% CI: -4.18 - -2.31). Age (χ² = 37.400, p < 0.001), residence (χ² = 10.200, p < 0.001), BMI (χ² = 22.1, p < 0.001), and lack of knowledge about hypertension (χ² = 25.1, p < 0.001) were the factors with significantly undiagnosed hypertension. However, the sex differential on diastolic blood pressure was not significant.
The bivariate analysis in Table 4 provides valuable insights into the association between various sociodemographic, behavioral, and diet-related factors with undiagnosed hypertension within the Ndera sector, Gasabo district of Rwanda. Among the factors examined, gender, age, BMI, knowledge on hypertension, and residence displayed significant associations with undiagnosed hypertension. Among women, 17% (39/225) had hypertension, compared to 13% (21/168) among men.
Among individuals aged 55 and above 43% (21/49) had undiagnosed hypertension compared to 7% (25/344) among younger age groups. Among individuals with obesity, 38% (18/48) had undiagnosed hypertension, compared to 12% (42/343) among individuals who were not obese.
Discussion
The study revealed a 15% prevalence of undiagnosed hypertension in the Ndera sector, Gasabo district, Rwanda, highlighting key risk factors such as age (particularly those 55 and older) and BMI, with obesity being notably associated with higher hypertension rates. A significant knowledge gap about hypertension was identified, emphasizing the need for health education to improve awareness and early detection. Geographic disparities were also evident, with higher prevalence in cells farther from Rubungo Health Centre, indicating the necessity for targeted interventions in these areas. Factors such as sex, marital status, physical activity, salt consumption, smoking, alcohol use, and education level showed no significant association with undiagnosed hypertension. These findings underscore the importance of tailored health education, weight management programs, and addressing geographic disparities to effectively combat undiagnosed hypertension in the community. However, physical activity, salt consumption, smoking, alcohol use are known to be risk factors for all NCDs and health promotion should address all risks.
This research in Ndera Sector aligns with regional and global findings regarding the impact of age, BMI, and health awareness on undiagnosed hypertension. Differences in significant factors across studies in Rwanda suggest that socio-demographic and lifestyle variations influence hypertension rates. These insights highlight the need for targeted interventions tailored to the specific needs of different communities.
Similarities exist between this study and a study conducted in Kirehe District, Rwanda. In the Kirehe study, 21.2% (n = 910) of the sampled population had elevated blood pressure at screening, with 18.7% (n = 752) of those individuals not previously diagnosed with hypertension. Both univariate and multivariate analyses showed that age, weight, smoking, and other factors were associated with elevated blood pressure [18]. Another study conducted in Rulindo District, rural Rwanda, assessed the prevalence and risk factors associated with undiagnosed hypertension. It revealed that 41.9% of the participants were hypertensive without a prior diagnosis [10]. Both studies identified age as a significant factor associated with hypertension, with older age groups exhibiting a higher likelihood of undiagnosed hypertension. The prevalence of undiagnosed hypertension was statistically significantly higher among older individuals. This finding aligns with the general physiological understanding that blood vessel walls lose elasticity with age, contributing to increased blood pressure [22].
Similar to our study findings, a systematic review and meta-analysis conducted in Ethiopia revealed a high pooled prevalence of undiagnosed hypertension, estimated at 23.7%. Risk factors identified included older age, BMI greater than 25 kg/m², and comorbidity with diabetes mellitus (DM) [5]. This suggests shared risk factors and the importance of awareness in managing hypertension across these African populations. The global context underscores lifestyle-related risk factors such as unhealthy diets, physical inactivity, tobacco and alcohol use, and obesity [5].
Conclusions
This study on undiagnosed hypertension in Ndera Sector, Gasabo District, Rwanda, highlights critical implications for public health interventions and targeted healthcare strategies. Addressing BMI through weight management programs is crucial to mitigate hypertension risk. Enhancing health awareness, particularly about hypertension, requires focused interventions to improve knowledge without inadvertently increasing undiagnosed hypertension rates among the well-informed. Addressing geographical disparities in hypertension prevalence calls for targeted healthcare initiatives to ensure equitable access to screenings. Tailored healthcare strategies for older age groups are essential due to their higher susceptibility to hypertension. These findings underscore the need for multifaceted approaches that address BMI, health awareness, geographical disparities, and age-related health concerns to effectively combat undiagnosed hypertension in the Ndera Sector community.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BMI:
-
Body Mass Index
- BP:
-
Blood Pressure
- CVD:
-
Cardiovascular diseases
- HTN:
-
Hypertension
- MmHg:
-
millimeter of mercury
- NCDs:
-
Non-communicable disease
- RBC:
-
Rwanda Biomedical Center
- WHO:
-
World Health Organization
- EA:
-
Enumerated Area
- PPS:
-
Probability proportional to size
- SPSS:
-
Statistical Package for the Social Sciences
References
Hendricks L, Uwimana-Nicol J, Young T. Decision makers perceptions and experiences of developing population-level interventions targeting risk factors for hypertension and diabetes in South Africa: a qualitative study. BMC Health Serv Res [Internet]. 2023 Dec 1 [cited 2023 May 31];23(1). https://doi.org/10.1186/s12913-023-09135-x
WHO. World health statistics 2023 – Monitoring health for the SDGs [Internet]. 2023 [cited 2023 Aug 9]. https://www.who.int/publications/i/item/9789240074323
Nahimana MR, Nyandwi A, Muhimpundu MA, Olu O, Condo JU, Rusanganwa A et al. A population-based national estimate of the prevalence and risk factors associated with hypertension in Rwanda: Implications for prevention and control. BMC Public Health [Internet]. 2017 Jul 10 [cited 2023 Aug 13];18(1). https://rdcu.be/djnHq
World Health Organization (WHO). Hypertension [Internet]. 2023 [cited 2023 Jul 9]. https://www.who.int/news-room/fact-sheets/detail/hypertension
Dissemination. and Implementation Program in Hypertension in Rwanda - PMC [Internet]. [cited 2024 Jun 19]. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6816501/
Elias S, Dadi TK. Prevalence of undiagnosed hypertension and Associated Factors among adults in Mizan-Aman Town, Bench Sheko Zone, Southwest Ethiopia: A Community-based cross-sectional study. Adv Med [Internet]. 2023 Jul 10 [cited 2024 Jun 19];2023:1–10. Available from: /pmc/articles/PMC10352527/.
Ambaw Kassie G, Alemu A, Yosef Gebrekidan A, Asmare Adella G, Eshetu K, Wolie Asres A et al. Undiagnosed hypertension and associated factors among adults in Ethiopia: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2023;23(1).
Bosu WK, Reilly ST, Aheto JMK, Zucchelli E. Hypertension in older adults in Africa: A systematic review and meta-analysis. PLoS One [Internet]. 2019 Apr 1 [cited 2024 Feb 16];14(4). https://doi.org/10.1371/journal.pone.0214934
Baumann AA, Mutabazi V, Brown AL, Hooley C, Reeds D, Ingabire C et al. Dissemination and Implementation Program in Hypertension in Rwanda: Report on Initial Training and Evaluation. Glob Heart [Internet]. 2019 Jun 1 [cited 2024 Jun 19];14(2):135. https://www./pmc/articles/PMC6816501/
Ministry of Health Rwanda, Rwanda Biomedical Center (RBC). The Nationwide Non-Communicable Diseases STEPwise survey 2021. [cited 2023 Aug 13]; https://www.moh.gov.rw/news-detail/rwanda-rolls-out-free-screening-exercise-to-mitigate-ncds
Dukunde A, Ntaganda JM, Kasozi J, Nzabanita J. Prediction of the Prevalence of Hypertension and Associated Risk Factors in Rwanda Using Gibbs Sampling Method. Diseases [Internet]. 2023 Jun 16 [cited 2023 Jun 27];11(2):87. https://www.mdpi.com/2079-9721/11/2/87
Mazimpaka C, Nsanzimana S, Logan J, Binagwaho A, Wong R. Assessing the magnitude and risk factors Associated with undiagnosed hypertension in Rural Rwanda. J Manage Strategy. 2019;10(2):3.
NISR. Population and Housing Census 5th Rwanda. 2022. [cited 2023 Aug 9]; https://www.statistics.gov.rw/publication/1975
Damascene Kabakambira J, Kabakambira J, Bitwayiki R, Mujawamariya G, Lucero-Prisno IIID, Mucumbitsi J. s)-CC BY-NC-ND Kigali Car Free Day: An Innovative Model in the Fight against Non-Communicable Disease Pandemics. Rwanda Medical Journal [Internet]. 2019 [cited 2024 Feb 16];76(3):1–5. http://www.bioline.org.br/pdf?rw19016
Determining Sample Size Degree Of Variability. [cited 2024 Jun 19]; https://www.tarleton.edu/academicassessment/wp-content/uploads/sites/119/2022/05/Samplesize.pdf
World Health Organization(WHO). STEPS-wise approach to NCD risk factor surveillance (STEPS) [Internet]. [cited 2023 Aug 13]. https://www.who.int/teams/noncommunicable-diseases/surveillance/systems-tools/steps
Li F, Wilkens LR, Novotny R, Fialkowski MK, Paulino YC, Nelson R et al. Anthropometric Measurement Standardization in the US-Affiliated Pacific: Report from the Children’s Healthy Living Program. Am J Hum Biol [Internet]. 2016 May 1 [cited 2024 Jun 19];28(3):364. https://www.pmc/articles/PMC4861683/
Obesity. preventing and managing the global epidemic : report of a WHO consultation [Internet]. [cited 2024 Jun 19]. https://iris.who.int/handle/10665/42330
Astrup A. Healthy lifestyles in Europe: prevention of obesity and type II diabetes by diet and physical activity. Public Health Nutr. 2001;4(2b):499–515.
SPSS Statistics 21. 0 Available for Download [Internet]. [cited 2024 Jun 19]. https://www.ibm.com/support/pages/spss-statistics-210-available-download
Mayo Clinic Staff. Mayo Clinic. 2024 [cited 2024 Jun 19]. High blood pressure (hypertension) - Diagnosis & treatment - Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/high-blood-pressure/diagnosis-treatment/drc-20373417#
Association WM. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull World Health Organ [Internet]. 2001 [cited 2024 Jun 19];79(4):373. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2566407/
Acknowledgements
This research project was accomplished in partnership with several people. We would like firstly to express our gratitude to the Government of Rwanda and the Ministry of Education for sponsoring our education. We appreciate the University Of Rwanda (UR), College of Medicine and Health Sciences (CMHS), and mostly the Department of Clinical Medicine and Community Health (CMCH) for arrangements and preparations of everything which was needed for these research projects to be carried out and end in the right time. We would also like to acknowledge the key input of the survey respondents and data from the KIBAGABAGA Hospital, without which this study would not have been possible.
Funding
Aashna Uppal acknowledges the receipt of studentship awards from the Health Data Research UK-The Alan Turing Institute Wellcome PhD Programme in Health Data Science (Grant Ref: 218529/Z/19/Z). The other authors do not have any funding sources to declare.
Author information
Authors and Affiliations
Contributions
OAA: Conception, design, data analysis, interpretation, project supervision, critical revision and writing of the manuscript JCH: Conception, design, data analysis, interpretation, and project supervision RM: Conception, design, data collection, data analysis, interpretation, critical revision and writing of the manuscript UM: Conception, design, data collection data analysis, and interpretation CM: Conception, design, data collection, data analysis, and interpretation SH: Conception, design, data collection, data analysis, interpretation, and critical revision MAG: Data analysis, and interpretation AU: Critical revision of the manuscript FPW: Conception, design, critical revision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research study adhered to rigorous ethical standards, aligning with the principles outlined in the Declaration of Helsinki. Prior to initiation, ethical approval was obtained from both the Institutional Review Board (IRB) of the University of Rwanda and Kibagabaga District Hospital. The study was conducted following the guidelines and regulations set forth by these institutions. The approval reference numbers, Gasabo approval reference No: 1294/KBGH_EC/2023, and UR CMHS reference No: CMHS/IRB/433/2023, signify the thorough ethical vetting undergone by the research protocol, ensuring the protection of participants’ rights, confidentiality, and the overall ethical integrity of the study. Finally, informed consent to participate was obtained from all participants in this study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Okesina, A.A., Habineza, J.C., Mbazumutima, R. et al. Prevalence of undiagnosed hypertension and associated factors in Ndera sector, Gasabo district of Rwanda: a cross-sectional study. BMC Public Health 24, 2495 (2024). https://doi.org/10.1186/s12889-024-19999-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19999-1