Abstract
Background
Although the Healthy Eating Index (HEI) is widely recommended to reduce the risk of cardiovascular disease and all-cause death, there are significant differences in physiological and nutritional factors between the sexes. The potential impact of sex on adult dietary health is still poorly understood. The study was designed to assess whether the health benefits of diet differed by sex.
Methods
In a prospective study of 39,567 U.S. adults (51.2% female, age 46.8 ± 17.6 years), we examined sex-specific, multivariable-adjusted associations of HEI with all-cause mortality and cardiovascular disease mortality. Restricted cubic splines (RCS), subgroup analysis, propensity score matching (PSM), random forest feature importance, and sensitivity analysis were also used.
Results
During 328,403 person-years of follow-up, a total of 4754 all-cause deaths were recorded, including 1481 cardiovascular deaths. Compared to the lowest quartile of HEI, the all-cause mortality rate of females and males in the highest quartile array decreased by 34% (HR 0.66 [95% CI 0.55–0.8]) and 15% (HR 0.85 [95% CI 0.73–0.99]), respectively. The restricted cubic spline showed a linear inverse association between baseline HEI and all-cause mortality and CVD mortality, with similar sex-specific results. Similarly, component scores were sex-specific for mortality risk, with females benefiting more from diet. The benefits of dairy products, vegetables, and sodium scores on the risk of all-cause death were higher in males and females. However, the benefits of vegetable, sodium, and fatty acid scores on the risk of cardiovascular death were different.
Conclusions
In the adult population of the U.S., there are more opportunities for females to reduce the risk of all-cause mortality and cardiovascular mortality from the same dose of healthy dietary intake than males. These findings could reduce the risk of death by motivating the population, especially females, to consume healthy dietary components, especially vegetables and dairy products.
Similar content being viewed by others
Introduction
It is well-known that cardiovascular disease is the leading cause of premature death worldwide [1]. More than 50% of global mortality is attributed to chronic diseases such as cardiovascular disease (CVD), diabetes, and certain types of cancer [2]. To this day, there are hundreds of risk factors beyond the “classic” risks considered in studies such as the Framingham Heart Study and the MONICA Project [3]. This includes psychosocial factors (including social gradients and status) as well as many environmental and occupational exposures and factors such as dietary composition. In recent years, people have been actively exploring essential factors that can be controlled, including poor diet, physical inactivity, and substance abuse [4].
Diet is a significant contributor to obesity and many chronic diseases such as cardiovascular disease, cancer, and type 2 diabetes. National Food-based Dietary Guidelines (FBDG) are designed to provide specific advice and recommendations on healthy eating and lifestyle [5]. A healthy diet can reduce the risk of chronic disease and death [6,7,8]. A meta-analysis study showed that high adherence to dietary quality measures such as the Alternative Healthy Eating Index (AHEI) and Dietary Approaches to Stop Hypertension (DASH) was associated with a 22% lower risk of all-cause death [9]. Associated with reduced morbidity and mortality from CVD[10] and cancer [11], these eating patterns have been widely disseminated to help people get more value out of their diets [12, 13]. Multiple studies have shown significant differences in the risk of cardiovascular disease (CVD) between the sexes [14, 15]. Among middle-aged population, the mortality of cardiovascular disease in men is 2–5 times higher than that in women [16]. Sex differences in CVD mortality cannot be fully explained by abnormal levels of conventional CVD risk factors such as hypertension, dyslipidemia, smoking, and obesity. These include a growing number of physiological risk factors that can also contribute to sex differences, such as changes in intermediate traits of blood pressure and serum cholesterol that may be the result of a range of behavioral factors, such as exercise and diet. In addition, persistent low-grade inflammation, including inflammation associated with infection, is associated with the supposed role of the gut microbiome, which in turn may be influenced by diet and biophysical environment [17, 18]. In recent years, researchers have increasingly focused on sex differences in the effects of diet. Similarly, the impact of sex-related nutritional status on the outcome of patients with CVD has been demonstrated [19, 20]. These differences are reflected in food choices, energy and nutrient intake, and attitudes toward diet [21,22,23,24,25,26,27]. However, it is unclear whether including sex differences affects the association between dietary factors and health outcomes. Therefore, the aim of this study was to assess the impact of the Healthy Eating Index (HEI) [28] on cardiovascular and all-cause mortality with respect to sex. Understanding this distinction could provide new insights into narrowing the “sex gap” in mortality risk rates and optimizing diet-related outcomes for all people.
Materials and methods
Data source
The National Health and Nutrition Examination Survey (NHANES) is a continuous, stratified, complex, multi-stage sampling survey conducted by the Centers for Disease Control and Prevention (CDC) in the United States. It collects nationally representative health and nutrition data from non-institutionalized individuals [29]. The research methodology and data collection process were previously reported. All databases can be accessed from the NHANES website (https://wwwn.cdc.gov/nchs/nhanes/Default.aspx). This study obtained approval from the CDC Institutional Review Board, and all participants provided written informed consent.
Study population
The study initially screened 80,312 participants from the NHANES 2003–2018 and linked their records to the National Death Index records. We excluded age younger than 18 years (n = 32,549), absence of daily dietary data (n = 5676), dietary energy intake of less than 800 or more than 4200 kcal per day for men, and dietary energy intake of less than 500 or more than 3500 kcal per day for women [30] (n = 1581), pregnancy (n = 861) or missing follow-up status data (n = 78). After exclusion, a total of 39,567 participants were included in our final analysis(Fig. S1).
Assessment of healthy eating index
The diet interview, titled “What We Eat in America” (WWEIA), is a collaboration between the U.S. Department of Agriculture (USDA) and the U.S. Department of Health and Human Services (DHHS). All NHANES participants underwent two 24-h dietary recall interviews, the first in a mobile test center (MEC) and the second in a telephone interview 3–10 days later. In this study, dietary intake was estimated using the average of two 24-h recall data. The USDA’s Dietary Research Food and Nutrition Database (FNDDS) calculates the composition of nutrients and food in all foods [31].
The HEI-2015 was calculated using the National Cancer Institute scoring algorithm [32]. The index has nine components associated with adequacy and four with moderation. First, Full ingredients include total fruit, whole fruit, total vegetables, greens and beans, total protein foods, seafood and plant proteins, whole grains, dairy, and fatty acids. Second, appropriate ingredients include sodium, refined grains, added sugars, and saturated fats. Total scores range from 0 to 100, with higher HEI-2015 scores indicating better diet quality. Supplementary materials Table S1 shows the scoring components of HEI-2015.
Assessment of covariates
We construct a directed acyclic graph (DAG) to ensure the causal relationship between HEI—2015 and mortality and identify the confounding factors (Fig. S2). Standardized questionnaires were used to collect information on age, sex, race/ethnicity, education level, household income, smoking status, etc. Race/ethnicity is divided into non-Hispanic white, non-Hispanic black, Mexican American, and the other four segments. The level of education was classified as less than a high school diploma, high school/equivalent, college, or above. Family income-to-poverty ratios were categorized as follows: ≤ 1.3, 1.3–3.5, and > 3.5. The higher the ratio, the better the family’s economic situation [33]. Smoking status was classified as never smokers, former smokers, and current smokers. BMI was divided into < 25.0, 25.0–29.9, or ≥ 30 kg/m2 [34], with BMI ≥ 30 was defined as obesity. Diabetes was defined as self-reported diagnosed diabetes, or the use of oral hypoglycemic agents or insulin, fasting blood glucose levels ≥ 126 mg/dL, or blood glucose levels ≥ 200 mg/dL after oral glucose tolerance tests, or hemoglobin A1c (HbA1c) levels ≥ 6.5%. Hypertension is defined as self-reported diagnosed hypertension, current use of antihypertensive medications, or mean systolic blood pressure (ASBP)/mean diastolic blood pressure (ADBP) ≥ 140/90 mmHg. Drinking status was defined as non-drinkers, moderate drinking (0.1–13.9 g/ day for women and 0.1–27.9 g/ day for men), and heavy drinking (≥ 14 g/ day for women and ≥ 28 g/ day for men).
Laboratory tests included total cholesterol (TC), triglycerides(TG), and HDL cholesterol. The estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [35].
Ascertainment of mortality
As of December 31, 2019, all-cause mortality and cardiovascular mortality were determined by association with National Death Index (NDI) records. The primary cause of death was identified according to the ICD-10 code. Cardiovascular deaths were defined as heart disease (I00-I09, I11, I13, I20-I51) and cerebrovascular disease (I60-I69).
Statistical analysis
As a result of NHANES’s review sampling design, sample weights, clustering, and stratification were included in all statistical analyses in this study, and a weighted estimate representing the non-institutional population of the United States for 2003–2018 was produced [29]. Continuous variables are reported as weighted mean ± standard deviation, and categorical variables are expressed as counts (percentages).
Participants’ baseline characteristics were described by sex and HEI(Q1-Q4) quartile, respectively. Kaplan–Meier curve analysis and log-rank test were used for primary outcome analysis to evaluate sex differences in overall survival. The association between HEI-2015 and all-cause mortality/cardiovascular mortality was examined using COX proportional hazard regression models. We first established three statistical models. Model 1: unadjusted variables; Model 2 was adjusted for age, sex (for all participants only), race/ethnicity, education, and family income-to-poverty ratios; Model 3 further adjusted smoking status, drinking status, BMI, hypertension, diabetes, HDL cholesterol, TG, TC, eGFR, energy intake, protein intake, and fat intake. We used the lowest quartile (Q1) of the HEI-2015 as the reference group and the median of each category as a continuous variable to calculate the linear trend. Estimated hazard ratio (HR) and 95% confidence interval (CI).
To explain the dose–response relationship between HEI-2015 and all-cause and cardiovascular death, a restricted cubic spline analysis was performed for the 5th, 35th, 65th, and 95th percentiles of the HEI-2015 distribution with the same variable adjustments as in Model 3. Sex differences between HEI-2015 and mortality were assessed using a likelihood ratio test.
Further, by age (18–40, 41–60, and > 60 years), race/ethnicity (non-Hispanic white, other), education level (less than high school diploma, high school/equivalent, college or above), income to poverty ratio (≤ 1.3, 1.3–3.5, > 3.5), BMI (< 25.0, 25.0–29.9, ≥ 30 kg/m2), hypertension (no or yes), diabetes (no or yes), smoking status (non-smokers, former smokers, current smokers), alcohol consumption (non-drinkers, moderate drinkers, heavy drinkers), and eGFR(< 60, ≥ 60 mL/min/1.73 m2) was stratified for analysis. Potential modifying effects were detected by detecting the corresponding multiplicative interaction terms. We then repeated the multivariate-adjusted COX model (Model 3), as described above, to examine the sex-specific association of HEI-2015 components with all-cause and cardiovascular death. Additionally, the random forest (RF) model will be used to evaluate the sex-related importance of features for predicting all-cause mortality and cardiovascular mortality based on HEI-2015 scores and components. All participants were divided into training and testing sets in a 7:3 ratio. Through the confusion matrix, the accuracy, the recall rate, and the F1 score are summarized as the performance index.
In order to better explain the sex differences in the benefit value of high HEI-2015, we performed some secondary analyses. First, in this study, using propensity score matching (PSM) was used. A 1:1 nearest neighbor matching algorithm with a caliper value of 0.1 matched participants with the lowest (Q1) and extreme quartile (Q4) HEI-2015, so as to eliminate bias and control for potential confounding variables. Confounding factors include age (continuous), race (non-Hispanic white, non-Hispanic black, Mexican Hispanic, and others), education (less than a high school diploma, high school/equivalent, college or above), household income to poverty ratio (≤ 1.3, 1.3–3.5, > 3.5), BMI(< 25.0, 25.0–29.9, ≥ 30 kg/m2), Smoking status (non-smoker, former smoker, and current smoker), alcohol consumption status (non-drinker, moderate drinker, heavy drinker), hypertension (no or yes), diabetes (no or yes), TC (quartile), TG (quartile), HDL-C(quartile),eGFR(< 60, ≥ 60 mL/min/1.73 m2). The absolute standardized mean difference (ASMD) of less than 0.1(dashed line) is considered to be negligible in the imbalance between the two groups. After matching, we reanalyzed sex differences between HEI-2015 scores and risk of all-cause mortality and cardiovascular disease mortality, as in the previous approach. Second, we examined sex differences between HEI-2015 and significant risk factors (diabetes, hypertension, malignancy, cardiovascular disease, obesity).
Finally, we also conducted some sensitivity analyses to check the robustness of the study results. First, we excluded participants with diabetes and malignancy at baseline to account for the effect of particular dietary differences on mortality risk. Second, to minimize the potential for reverse causality bias, we excluded participants who died within the first two years of follow-up and those with self-reported cardiovascular disease at baseline.
In order to minimize the sample size reduction caused by missing covariates, this study conducted multiple interpolations for all missing variables. Two-sided P < 0.05 was considered statistically significant. Statistical analysis was performed using Rv4.3.2.
Results
Baseline characteristics of study participants
The baseline demographic, lifestyle, and medical characteristics of this cohort are presented in Tables 1 and 2. Of 39,567 U.S. adults, 51.2% were female, and 67.8% were non-Hispanic white. The mean age at baseline was 46.8 ± 17.6 years. Participants with higher HEI-2015 levels were older, more likely to be non-Hispanic, female, had higher household income, higher levels of education, were less likely to be obese, had never smoked, were more likely to drink heavily, and were more likely to have high blood pressure, diabetes, higher HDL-C, TC, and lower TG and eGFR levels.
HEI-2015 and component distribution differences by sex
Overall, the distribution level of HEI-2015 in females was slightly higher than in males (Fig. S3). To further investigate the impact of dietary factors on the differences in HEI-2015 between males and females, we compared the scores of various components of HEI-2015, and the results are shown in Supplementary materials Table S2. The female population had higher HEI-2015 scores in fruits, vegetables, legumes, cereals, dairy products, seafood, fatty acids, and lower protein scores.
Sex differences in HEI-2015 associations with all-cause mortality and CVD mortality
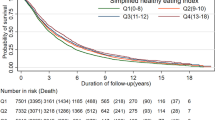
During 328,403 person-years of follow-up (median, 8.1 years) from the NHANES 2003–2018, we recorded 4754 deaths and identified 1481 cardiovascular deaths. Unadjusted Kaplan–Meier analysis showed that the cumulative incidence of all-cause and cardiovascular death was lower in women than in men, and this association was observed for any HEI-2015 score (Q1-Q2 or Q3-Q4) (Log-rank P < 0.001, Fig. 1). For all participants, the multivariate adjustment HRs for all-cause mortality in the highest quartile was 0.76 (95% CI 0.68 to 0.85), and the multivariate adjustment HRs for cardiovascular disease mortality was 0.69 (95% CI 0.55 to 0.85) compared to the lowest quartile in the fully adjusted model. For females, the highest quartile had a 34% lower risk of all-cause mortality (P trend < 0.001) and a 38% lower risk of cardiovascular death (P trend = 0.006) compared to the lowest quartile. For males, there was a 15% reduction in all-cause mortality in the highest quartile compared to the lowest quartile (P trend < 0.001). However, this relationship was not observed in cardiovascular mortality, and this benefit was significantly smaller than in females (Table 3).
Kaplan–Meier Survival Curves for All-cause Mortality and CVD Mortality According to HEI-2015. Kaplan–Meier survival curves for all-cause mortality (A) and cardiovascular mortality (B) were based on participants with HEI-2015 < 48.4. Kaplan–Meier survival curves for all-cause mortality (C) and cardiovascular mortality (D) were based on participants with HEI-2015 ≥ 48.5
In addition, multivariate-adjusted RCS analysis shows a significant dose–response relationship between HEI-2015 and all-cause death (P non-linearity = 0.562, Fig. 2A) and cardiovascular death (P non-linearity = 0.93, Fig. 2B). Meanwhile, the same trend is observed after sex grouping, with linear relationship after multi-factor adjustment (P linearity < 0.001, Fig. 2C, D).
Association between HEI-2015 and all-cause and CVD mortality among participants in NHANES 2003–2018. Multivariate adjusted associations of HEI-2015 with all-cause mortality (A) and CVD mortality (B) were shown for all participants. Multivariable-adjusted association of HEI-2015 with all-cause mortality (C) and CVD mortality (D) were shown by sex overall. HRs were adjusted for age, sex (for all participants only), race/ethnicity, education, and family income-to-poverty ratios, smoking status, drinking status, BMI, hypertension, diabetes, HDL cholesterol, TG, TC, eGFR, energy intake, protein intake, and fat intake. The solid red/blue/orange lines correspond to the estimates, and the shaded regions indicate the 95% confidence intervals
Stratified analysis of the association of HEI-2015 with all-cause mortality and CVD mortality by sex
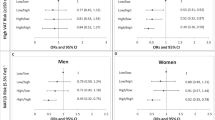
Based on age (18–40, 41–60, and > 60 years), race/ethnicity (non-Hispanic white and other), education level (less than a high school diploma, high school/equivalent, college or above), income to poverty ratio (≤ 1.3, 1.3–3.5, > 3.5), BMI (< 25.0, 25.0–29.9, ≥ 30 kg/m2), hypertension (no or yes), diabetes (no or yes), smoking status (never, former, current), drink status (never, moderate, heavy), and eGFR level (< 60, ≥ 60 mL/min/1.73 m2) stratified analysis was conducted. The results showed that the survival advantages of different sexs were consistent in different subgroups, as shown in Fig. 3. In the female population, we found significant interactions between HEI-2015 and all-cause mortality by age (P for interaction = 0.033) and smoking status (P for interaction = 0.039). At the same time, there was a significant interaction between HEI-2015 and CVD mortality by education level (P for interaction = 0.022) and eGFR (P for interaction = 0.006).
Stratified analyses for the associations of HEI-2015 with all-cause mortality and CVD mortality among participants in NHANES 2003–2018. A All-cause mortality; B CVD mortality. Adjusted for age, sex (for all participants only), race/ethnicity, education, and family income-to-poverty ratios, smoking status, drinking status, BMI, hypertension, diabetes, HDL cholesterol, TG, TC, eGFR, energy intake, protein intake, and fat intake. When analyzed stratified, stratified variables were not included in the model. Abbreviations: BMI, body mass index; TG, triglycerides; TC, total cholesterol
Sex differences in HEI-2015 components associations with all-cause mortality and CVD mortality
Further, we examined sex differences in associations between HEI-2015 component scores and all-cause mortality and CVD mortality. The Results are summarized in Fig. 4. Overall, HEI-2015 scores of fruits, vegetables, legumes, dairy products, fatty acids, and saturated fatty acids were significantly associated with mortality. For men, higher HEI-2015 scores for vegetables, legumes, dairy products, fatty acids, and saturated fatty acids reduced the risk of death, and the benefit was significantly smaller than that of women. Dose-dependent analysis of HEI-2015 component scores and risk of all-cause death and cardiovascular death suggested higher benefits for women in HEI-2015 scores (Figs. 5 and 6).
Associations of HEI-2015 components with All-cause and CVD mortality among participants in NHANES 2003–2018. HEI-2015 components were modeled as continuous (per 1-unit increase). HRs were adjusted for age, sex (for all participants only), race/ethnicity, education, and family income-to-poverty ratios, smoking status, drinking status, BMI, hypertension, diabetes, HDL cholesterol, TG, TC, eGFR, energy intake, protein intake, and fat intake
Association between HEI-2015 components (A-M) and all-cause mortality among participants. HRs were adjusted for age, race/ethnicity, education, and family income-to-poverty ratios, smoking status, drinking status, BMI, hypertension, diabetes, HDL cholesterol, TG, TC, eGFR, energy intake, protein intake, and fat intake. The solid blue/orange lines correspond to the estimates, and the shaded regions indicate the 95% confidence intervals
Association between HEI-2015 components (A-M) and CVD mortality among participants. HRs were adjusted for age, race/ethnicity, education, and family income-to-poverty ratios, smoking status, drinking status, BMI, hypertension, diabetes, HDL cholesterol, TG, TC, eGFR, energy intake, protein intake, and fat intake. The solid blue/orange lines correspond to the estimates, and the shaded regions indicate the 95% confidence intervals
Figure 7 shows the features of an essential analysis of HEI-2015 and the component scores used to assess all-cause and cardiovascular mortality. Overall, the RF model accurately predicted cardiovascular mortality on independent test data with accuracy of 0.99 (men and women), recall rates of 0.68 (women) and 0.69 (men), and F1 scores of 0.80 (women) and 0.81 (men). The RF model predicted all-cause mortality with relatively low accuracy on independent test data, with accuracy of 0.92 (women) and 0.89 (men), recall rates of 0.22 (women) and 0.21 (men), and F1 scores of 0.37 (women) and 0.34 (men). HEI-2015 score remained the most critical factor in assessing the risk of death, and its importance score was significantly higher than other factors of each HEI-2015 component. In addition, for men, dairy products, vegetables, saturated fatty acids, and fatty acid scores were essential factors in determining the risk of death from both all-cause and cardiovascular death. In the female population, dairy, vegetable, sodium, and fatty acid scores were significant determinants of all-cause mortality. The scores of dairy products, sodium, saturated fatty acids, and added sugars were essential in determining cardiovascular death.
Secondary analyses
First, we performed PSM on participants with the lowest and highest HEI-2015 quartile, and a total of 12,558 participants were matched, including 6,279 participants with the lowest HEI-2015 quartile and 6,279 participants with the highest HEI-2015 score. Supplementary materials Table S3 shows the weighted baseline characteristics after PSM. Participants in both groups were well-balanced on all baseline covariates; The standardized mean difference for all covariates is 0.1 (Fig. S4). When considering only the ultimate HEI-2015 score group, we found that in the female population, the risk of all-cause mortality was reduced by 27% in the Q4 group compared to the Q1 group. This association was not found in males. However, we could still observe a trend of women benefiting more, even if it was not statistically significant in the male population (Supplementary materials Table S4). Second, in a cross-sectional analysis of the HEI-2015 score and traditional risk factors for cardiovascular disease, we found similar sex specificity.
Interestingly, in terms of the prevalence of hypertension and obesity, the highest quartile, HEI-2015, was associated with a significantly lower risk of disease compared to the lowest quartile, HEI-2015. However, the relative magnitude of the risk–benefit for women was consistently higher than for men (Supplementary materials Table S5,S6). HEI-2015 with malignant tumor and cardiovascular disease prevalence is only such a negative correlation observed among women (Table S7,S8). There was no significant correlation between the prevalence of diabetes in females and males (Supplementary materials Table S9). Despite the limitations of the cross-sectional analysis, these findings suggest that women benefit more from HEI-2015 scores than men.
Sensitivity analysis
In sensitivity analyses, after excluding participants who died in the first two years of follow-up and had CHD at baseline, the relative magnitude of survival benefits in terms of all-cause mortality and cardiovascular mortality was consistently higher in females than in males (Supplementary materials Table S10,S11). Similarly, we observed the same sex differences after excluding participants with diabetes and malignancy at baseline (Supplementary materials Table S12,S13).
Discussion
In the nationally representative large-scale study, we observed evidence of significant sex differences between self-reported dietary intake and survival benefits. This association was independent of demographic characteristics, lifestyle, cardiovascular risk, and diet-related factors. Multiple sensitivity analyses and stratified analyses demonstrate the robustness of these results. Both sexes showed a significant linear negative association in the dose–response relationship between HEI-2015 and mortality risk. Of these, women had reductions of 34% in all-cause mortality and 38% in cardiovascular mortality.
In contrast, males obtained 15% reductions in all-cause mortality and 23% reductions in cardiovascular mortality from the same degree of high diet quality. Interestingly, this association was also found for each component, but this sex specificity was slightly attenuated compared to the HEI-2015 score. These findings can be used to motivate more people to eat healthily, especially females.
Although a large number of epidemiological studies have shown that healthy dietary patterns are significantly negatively associated with cardiovascular disease events and mortality [36,37,38]. These reports are generally consistent with our results. However, previous data on sex differences in the benefits of dietary patterns have been limited. A large prospective cohort study investigated the dose-dependent relationship between HEI-2015, Alternative Mediterranean Diet (AMED), Healthy Plant-based Diet Index (HPDI), and overall mortality. Subgroup analysis showed that HEI-2015 reduced the risk of death by 24% in women and 12% in men [39]. Consistent with previous results, our findings also show that this sex specificity is also present for the 13 component scores in HEI-2015, although there is no clear trend in some components. It is reasonable to infer that these foods are composed of a combination of multiple nutrients and phytochemicals that may have additive and synergistic effects.
There are several possible explanations for the sex differences in the effect of diet quality on all-cause mortality and cardiovascular mortality. From a biological perspective, hormones and gut microbiota may be essential causes of sex differences. Estrogen may protect women from heart disease by reducing circulating levels of bad cholesterol [40], while testosterone increases LDL-cholesterol and inflammatory marker levels, thereby driving the progression of atherosclerosis and stroke in men [41, 42]. In addition, women’s serum leptin levels are 3–4 times higher than that of men, which may be related to women’s body fat distribution and hormone levels [43]. The increased levels of leptin suppress appetite, making it easier for women to feel satiated [44], and more inclined to choose healthy foods rich in fiber and nutrients. Moreover, women have different hormone changes and nutritional needs during pregnancy and lactation compared to men, which requires them to pay more attention to healthy diets to meet their own and fetal needs. Previous studies have also observed differences in gut microbiota between sexes [45], which may play different roles in their dietary intake and nutrient absorption to some extent. In addition to the physiological differences mentioned above, there are also sex differences in food choices and health attitudes [25]. Sweets have been shown to be culturally associated with femininity, whereas meat is generally associated with masculinity. Females consume more sweets and less red meat than men [26]. The intake of soft drinks is even lower. Additionally, previous studies have shown that women consume more fruits and vegetables than men. These results are consistent with the findings of this study. Moreover, these foods were negatively associated with CVD [46] and stroke [47]. The sex differences in food choices can be partially attributed to women’s firm beliefs in health [48, 49]. In terms of the effectiveness of health communication, recipients with high self-efficacy were more persuasive about health messages, especially in a negative framework [50]. This means that women generally have a higher level of participation in health education, and are more willing to listen to information about healthy eating, make healthier dietary choices, and cook healthier meals. From a socio-cultural perspective, women are often expected to present the image of a slim figure and take responsibility for family health, including dietary planning and cooking, which makes them more focused on weight management and healthy eating practices, and often feel guilty about carbohydrates and saturated fatty acids. In contrast, the social restrictions on men’s body image are less stringent [27]. In addition, the sex differences in the association of eating patterns with health outcomes are also related to the definition of social sex roles or the freedom of individuals to express their sex roles. Hopwood CJ et al. found that sex differences are more significant in countries with higher levels of human development and sex equality [51]. This means that in these countries, there are more opportunities for expressing sex roles, resulting in more pronounced sex differences. This discovery supports the hypothesis of the sex equality paradox’.
The sex difference in prognosis caused by the difference in HEI-2015 components further indicated the need to consider the superposition and synergistic effects of nutrition. When we analyzed each component, there were differences in the contribution of each component to the risk of death. In addition, dairy products, vegetables, and fat scores showed higher benefits. Although the benefits varied slightly between the sexes, these represented the highest benefits for both sexes overall.
Dietary guidelines generally recommend low-fat diets, while high-fat diets are, especially saturated fatty acids, associated with coronary heart disease and obesity complications [52]. In recent years, Dehghan et al. have shown that higher total dairy intake (> 2 servings per day compared with no intake) is inversely associated with mortality risk and non-cardiovascular mortality [53]. This is consistent with the results of this study. A meta-analysis showed that fruit and vegetable consumption, alone or in combination, was associated with reductions in all-cause mortality and cardiovascular mortality [54]. However, more recent studies have shown that mixed fruit and vegetable consumption and vegetable consumption alone are linked to lower all-cause mortality in women but not in men [55]. In this study, we observed a significant negative association between vegetable intake and risk of death in both men and women. Fruit consumption was found to be only negatively associated with the risk of death in women, not men.
Among these components, we noted a sex-specific association between sodium intake and mortality risk rates. Previous studies have shown a U-shaped association between high sodium intake and cardiovascular disease and overall mortality [56,57,58]. In another UK Biobank study, which measured 24-h urinary sodium excretion in more than 390,000 participants, the researchers did not observe a significant association between sodium intake and CVD events. Still, they did find a J-shaped relationship with all-cause mortality [59]. However, the Health ABC Study with 2,642 older adults aged 70–79 years showed that FFQ-based sodium intake was not associated with an increased 10-year mortality risk [60]. The results are generally consistent with current data, although this study was based on a one-unit increase in sodium scores, which may have significantly weakened the association. However, it is essential to note that we also found that reducing sodium intake had a higher benefit to total mortality risk reduction in women, providing additional strong support for the association between high sodium intake and increased risk of cardiovascular disease.
When analyzing the relationship between HEI-2015 and all-cause mortality and cardiovascular death in the female population, we found that age, smoking status, education level, and eGFR, four potential confounding factors, have significant interactions with these associations. Females of different age groups have varying responses to healthy diets due to differences in hormone levels, metabolic rates, nutritional needs, health awareness, and so on. Smoking, as a known risk factor for cardiovascular diseases, may have a negative impact on health due to harmful substances in tobacco, thereby reducing the potential benefits of a healthy diet. In addition, education level may affect individuals’ acquisition and understanding of health information, which in turn affects their dietary choices. Women with higher levels of education are more likely to follow healthy eating guidelines. Finally, impaired kidney function can also affect the processing and metabolism of nutrients, so women with lower eGFR may not receive the same cardiovascular benefits from a healthy diet as those with normal kidney function. In summary, these confounding factors may affect the relationship between HEI-2015 and health outcomes through different mechanisms, needing to be adjusted and considered in further research to more accurately assess the impact of a healthy diet on women’s health.
The study has several advantages. The large sample size and number of events, as well as long-term follow-up, provided enough power to reveal a modest association between HEI-2015 and the risk of death. Although HEI-2015 has been proven to benefit both sexes, we categorized the diet by component importance to maximize the survival benefits. However, some limitations of this study need to be mentioned. First, all dietary data collected was self-reported. Although a standardized questionnaire was used, the report was calculated based on self-reported 24-h food recall data, which may not be representative of habitual eating behavior and may have recall bias. Eating habits, in particular, may vary depending on occupation, recall time, weekends, etc. Moreover, because of the simplicity of our scoring algorithm, it was challenging to completely eliminate the effects of differences between people based on just two days of intake. Second, given the observational design of this study, causality cannot be inferred, and the results should be interpreted with caution. Again, these results are based on U.S. adult participants, which may limit generalizations to populations in other countries. Then, to mitigate the impact of potential confounding factors on the results. Sensitivity analyses were performed to exclude participants who died during the first two years of follow-up and who had self-reported diabetes, hypertension, CVD, or malignancy at baseline. However, unknown confounding factors that may have influenced the results cannot be completely ruled out, including reports of differences between men and women and sex-related effects of dietary habits on outcome events over time. Given that death is a complex, multi-factorial end event involving multiple genetic, behavioral, and environmental causes, there are still some unknown or unidentified confounding factors. Finally, genetic risk factors affecting dietary metabolism were not analyzed. Therefore, in future studies, it would be interesting to investigate the sex correlation of potential interactions between diet and genes on cardiovascular mortality and all-cause mortality.
Conclusion
In summary, we found evidence of sex differences between diet and all-cause and cardiovascular deaths in this nationally representative cohort of U.S. adults. Overall, women obtained a more significant reduction in risk of all-cause death and cardiovascular death from HEI-2015 compared to men. Recognizing the limitations of a one-size-fits-all approach to health, increasing attention to sex differences in diet-related benefits could increase the perspective of personalized medicine to improve health outcomes for all. Nevertheless, the impact of HEI-2015 and its components on cardiovascular disease mortality and all-cause mortality relative to sex requires further research.
Availability of data and materials
All data can be obtained from NHANES in this study. This data is available from the NHANES database, https://www.cdc.gov/nchs/nhanes (accessed on 7 April 2024).
References
Ahmadijoo P, Eftekhari MH, Masoumi SJ, Zahedani MR, Mohammadi F. The possible relationship between the healthy eating index-2015 and the 10-year risk of cardiovascular diseases. BMC Nutr. 2023;9(1):76. https://doi.org/10.1186/s40795-023-00735-8.
GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
Ezzati M, Obermeyer Z, Tzoulaki I, Mayosi BM, Elliott P, Leon DA. Contributions of risk factors and medical care to cardiovascular mortality trends. Nat Rev Cardiol. 2015;12(9):508–30. https://doi.org/10.1038/nrcardio.2015.82.
Meléndez-Fernández OH, Walton JC, DeVries AC, Nelson RJ. Clocks, Rhythms, Sex, and Hearts: How Disrupted Circadian Rhythms, Time-of-Day, and Sex Influence Cardiovascular Health. Biomolecules. 2021;11(6):883. https://doi.org/10.3390/biom11060883. Published 2021 Jun 14.
Herforth A, Arimond M, Álvarez-Sánchez C, Coates J, Christianson K, Muehlhoff E. A Global Review of Food-Based Dietary Guidelines. Adv Nutr. 2019;10(4):590–605. https://doi.org/10.1093/advances/nmy130.
Li Y, Zhong X, Cheng G, et al. Hs-CRP and all-cause, cardiovascular, and cancer mortality risk: A meta-analysis. Atherosclerosis. 2017;259:75–82. https://doi.org/10.1016/j.atherosclerosis.2017.02.003.
Aune D, Sen A, Prasad M, et al. BMI and all cause mortality: systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. BMJ. 2016;353:i2156. https://doi.org/10.1136/bmj.i2156.
English LK, Ard JD, Bailey RL, et al. Evaluation of Dietary Patterns and All-Cause Mortality: A Systematic Review. JAMA Netw Open. 2021;4(8): e2122277. https://doi.org/10.1001/jamanetworkopen.2021.22277.
Schwingshackl L, Schwedhelm C, Hoffmann G, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2017;105(6):1462–73. https://doi.org/10.3945/ajcn.117.153148.
Belin RJ, Greenland P, Allison M, et al. Diet quality and the risk of cardiovascular disease: the Women’s Health Initiative (WHI). Am J Clin Nutr. 2011;94(1):49–57. https://doi.org/10.3945/ajcn.110.011221.
Wirt A, Collins CE. Diet quality–what is it and does it matter? Public Health Nutr. 2009;12(12):2473–92. https://doi.org/10.1017/S136898000900531X.
Fung TT, McCullough M, van Dam RM, Hu FB. A prospective study of overall diet quality and risk of type 2 diabetes in women. Diabetes Care. 2007;30(7):1753–7. https://doi.org/10.2337/dc06-2581.
Chiuve SE, Fung TT, Rimm EB, et al. Alternative dietary indices both strongly predict risk of chronic disease. J Nutr. 2012;142(6):1009–18. https://doi.org/10.3945/jn.111.157222.
Thom TJ, Epstein FH. Heart disease, cancer, and stroke mortality trends and their interrelations. An international perspective Circulation. 1994;90(1):574–82. https://doi.org/10.1161/01.cir.90.1.574.
Tunstall-Pedoe H, Kuulasmaa K, Amouyel P, Arveiler D, Rajakangas AM, Pajak A. Myocardial infarction and coronary deaths in the World Health Organization MONICA Project. Registration procedures, event rates, and case-fatality rates in 38 populations from 21 countries in four continents. Circulation. 1994;90(1):583–612. https://doi.org/10.1161/01.cir.90.1.583.
Jousilahti P, Vartiainen E, Tuomilehto J, Puska P. Sex, age, cardiovascular risk factors, and coronary heart disease: a prospective follow-up study of 14 786 middle-aged men and women in Finland. Circulation. 1999;99(9):1165–72. https://doi.org/10.1161/01.cir.99.9.1165.
Howitt MR, Garrett WS. A complex microworld in the gut: gut microbiota and cardiovascular disease connectivity. Nat Med. 2012;18(8):1188–9. https://doi.org/10.1038/nm.2895.
Tremaroli V, Bäckhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489(7415):242–9. https://doi.org/10.1038/nature11552.
Kwaśny A, Uchmanowicz I, Juárez-Vela R, Młynarska A, Łokieć K, Czapla M. Sex-related differences in the impact of nutritional status on in-hospital mortality in heart failure: a retrospective cohort study. Eur J Cardiovasc Nurs. 2024;23(2):176–87. https://doi.org/10.1093/eurjcn/zvad050.
Kwaśny A, Łokieć K, Uchmanowicz B, Młynarska A, Smereka J, Czapla M. Sex-related differences in the impact of nutritional status on in-hospital mortality in acute coronary syndrome: A retrospective cohort study. Nutr Metab Cardiovasc Dis. 2023;33(11):2242–50. https://doi.org/10.1016/j.numecd.2023.06.010.
Bates CJ, Prentice A, Finch S. Gender differences in food and nutrient intakes and status indices from the National Diet and Nutrition Survey of people aged 65 years and over. Eur J Clin Nutr. 1999;53(9):694–9. https://doi.org/10.1038/sj.ejcn.1600834.
Cavazza N, Guidetti M, Butera F. Portion size tells who I am, food type tells who you are: Specific functions of amount and type of food in same- and opposite-sex dyadic eating contexts. Appetite. 2017;112:96–101. https://doi.org/10.1016/j.appet.2017.01.019.
Kang M, Park SY, Boushey CJ, et al. Portion Sizes from 24-Hour Dietary Recalls Differed by Sex among Those Who Selected the Same Portion Size Category on a Food Frequency Questionnaire. J Acad Nutr Diet. 2018;118(9):1711–8. https://doi.org/10.1016/j.jand.2018.02.014.
Lim EX, Sim AY, Forde CG, Cheon BK. The role of perceived stress and gender on portion selection patterns. Physiol Behav. 2018;194:205–11. https://doi.org/10.1016/j.physbeh.2018.05.031.
Wardle J, Haase AM, Steptoe A, Nillapun M, Jonwutiwes K, Bellisle F. Gender differences in food choice: the contribution of health beliefs and dieting. Ann Behav Med. 2004;27(2):107–16. https://doi.org/10.1207/s15324796abm2702_5.
Wansink B, Cheney MM, Chan N. Exploring comfort food preferences across age and gender. Physiol Behav. 2003;79(4–5):739–47. https://doi.org/10.1016/s0031-9384(03)00203-8.
Nicolaou M, Doak C, Dam Rv, Hosper K, Seidell J, Stronks K. Body size preference and body weight perception among two migrant groups of non-Western origin. Public Health Nutr. 2008;11(12):1332–41. https://doi.org/10.1017/S1368980008002966.
Reedy J, Lerman JL, Krebs-Smith SM, et al. Evaluation of the Healthy Eating Index-2015. J Acad Nutr Diet. 2018;118(9):1622–33. https://doi.org/10.1016/j.jand.2018.05.019.
CDC. The National Health and Nutritional Examination Survey (NHANES) Analytic and Reporting Guidelines. Atlanta: CDC; 2006.
Hou W, Han T, Sun X, et al. Relationship Between Carbohydrate Intake (Quantity, Quality, and Time Eaten) and Mortality (Total, Cardiovascular, and Diabetes): Assessment of 2003–2014 National Health and Nutrition Examination Survey Participants. Diabetes Care. 2022;45(12):3024–31. https://doi.org/10.2337/dc22-0462.
Chen F, Du M, Blumberg JB, et al. Association Among Dietary Supplement Use, Nutrient Intake, and Mortality Among U.S. Adults: A Cohort Study. Ann Intern Med. 2019;170(9):604–13. https://doi.org/10.7326/M18-2478.
National Cancer Institute. Overview & background of the healthy eating index; 2021. https://epi.grants.cancer.gov/hei/.
Johnson CL, Paulose-Ram R, Ogden CL, et al. National health and nutrition examination survey: analytic guidelines, 1999–2010. Vital Health Stat 2. 2013;(161):1–24.
Dreimüller N, Lieb K, Tadić A, Engelmann J, Wollschläger D, Wagner S. Body mass index (BMI) in major depressive disorder and its effects on depressive symptomatology and antidepressant response. J Affect Disord. 2019;256:524–31. https://doi.org/10.1016/j.jad.2019.06.067.
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12. https://doi.org/10.7326/0003-4819-150-9-200905050-00006.
Liese AD, Krebs-Smith SM, Subar AF, et al. The Dietary Patterns Methods Project: synthesis of findings across cohorts and relevance to dietary guidance. J Nutr. 2015;145(3):393–402. https://doi.org/10.3945/jn.114.205336.
Akbaraly TN, Ferrie JE, Berr C, et al. Alternative Healthy Eating Index and mortality over 18 y of follow-up: results from the Whitehall II cohort. Am J Clin Nutr. 2011;94(1):247–53. https://doi.org/10.3945/ajcn.111.013128.
Ha K, Kim K, Sakaki JR, Chun OK. Relative Validity of Dietary Total Antioxidant Capacity for Predicting All-Cause Mortality in Comparison to Diet Quality Indexes in US Adults. Nutrients. 2020;12(5):1210. https://doi.org/10.3390/nu12051210. Published 2020 Apr 25.
Shan Z, Wang F, Li Y, et al. Healthy Eating Patterns and Risk of Total and Cause-Specific Mortality. JAMA Intern Med. 2023;183(2):142–53. https://doi.org/10.1001/jamainternmed.2022.6117.
Yang XP, Reckelhoff JF. Estrogen, hormonal replacement therapy and cardiovascular disease. Curr Opin Nephrol Hypertens. 2011;20(2):133–8. https://doi.org/10.1097/MNH.0b013e3283431921.
Wang X, Smith GI, Patterson BW, et al. Testosterone increases the muscle protein synthesis rate but does not affect very-low-density lipoprotein metabolism in obese premenopausal women. Am J Physiol Endocrinol Metab. 2012;302(6):E740–6. https://doi.org/10.1152/ajpendo.00533.2011.
Engström G, Hedblad B, Rosvall M, Janzon L, Lindgärde F. Occupation, marital status, and low-grade inflammation: mutual confounding or independent cardiovascular risk factors? Arterioscler Thromb Vasc Biol. 2006;26(3):643–8. https://doi.org/10.1161/01.ATV.0000200100.14612.bb.
Belin de Chantemèle EJ. Sex Differences in Leptin Control of Cardiovascular Function in Health and Metabolic Diseases. Adv Exp Med Biol. 2017;1043:87–111. https://doi.org/10.1007/978-3-319-70178-3_6.
Lombardo M, Feraco A, Armani A, et al. Gender differences in body composition, dietary patterns, and physical activity: insights from a cross-sectional study. Front Nutr. 2024;11:1414217. https://doi.org/10.3389/fnut.2024.1414217. Published 2024 Jul 11.
Mueller S, Saunier K, Hanisch C, et al. Differences in fecal microbiota in different European study populations in relation to age, gender, and country: a cross-sectional study. Appl Environ Microbiol. 2006;72(2):1027–33. https://doi.org/10.1128/AEM.72.2.1027-1033.2006.
Dauchet L, Amouyel P, Hercberg S, Dallongeville J. Fruit and vegetable consumption and risk of coronary heart disease: a meta-analysis of cohort studies. J Nutr. 2006;136(10):2588–93. https://doi.org/10.1093/jn/136.10.2588.
Shiferaw B, Verrill L, Booth H, et al. Sex-based differences in food consumption: Foodborne Diseases Active Surveillance Network (FoodNet) Population Survey, 2006–2007. Clin Infect Dis. 2012;54(Suppl 5):S453–7. https://doi.org/10.1093/cid/cis247.
Egele VS, Stark R. Specific health beliefs mediate sex differences in food choice. Front Nutr. 2023;10:1159809. https://doi.org/10.3389/fnut.2023.1159809. Published 2023 Jun 5.
Grzymisławska M, Puch EA, Zawada A, Grzymisławski M. Do nutritional behaviors depend on biological sex and cultural gender? Adv Clin Exp Med. 2020;29(1):165–72. https://doi.org/10.17219/acem/111817.
Werrij MQ, Ruiter RA, Van ‘t Riet J, De Vries H. Self-efficacy as a potential moderator of the effects of framed health messages. J Health Psychol. 2011;16(2):199–207. https://doi.org/10.1177/1359105310374779.
Hopwood CJ, Zizer JN, Nissen AT, et al. Paradoxical gender effects in meat consumption across cultures. Sci Rep. 2024;14(1):13033. https://doi.org/10.1038/s41598-024-62511-3. Published 2024 Jun 13.
World Health Organization. Diet, Nutrition, and the Prevention of Chronic Diseases: Report of a Joint WHO/FAO Expert Consultation, vol. 916. Geneva, Switzerland: World Health Organization; 2003.
Dehghan M, Mente A, Rangarajan S, et al. Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (PURE): a prospective cohort study. Lancet. 2018;392(10161):2288–97. https://doi.org/10.1016/S0140-6736(18)31812-9.
Wang X, Ouyang Y, Liu J, et al. Fruit and vegetable consumption and mortality from all causes, cardiovascular disease, and cancer: systematic review and dose-response meta-analysis of prospective cohort studies. BMJ. 2014;349:g4490. https://doi.org/10.1136/bmj.g4490. Published 2014 Jul 29.
Nguyen B, Bauma A, Gale J, Banks E, Kritharides L, Ding D. Fruit and vegetable consumption and all-cause mortality: evidence from a large Australian cohort study. Int J Behav Nutr Phys Act. 2016;13:9. https://doi.org/10.1186/s12966-016-0334-5. Published 2016 Jan 25.
Mente A, O’Donnell M, Rangarajan S, et al. Associations of urinary sodium excretion with cardiovascular events in individuals with and without hypertension: a pooled analysis of data from four studies. Lancet. 2016;388(10043):465–75. https://doi.org/10.1016/S0140-6736(16)30467-6.
O’Donnell M, Mente A, Rangarajan S, et al. Joint association of urinary sodium and potassium excretion with cardiovascular events and mortality: prospective cohort study. BMJ. 2019;364:l772. https://doi.org/10.1136/bmj.l772. Published 2019 Mar 13.
Wuopio J, Orho-Melander M, Ärnlöv J, Nowak C. Estimated salt intake and risk of atrial fibrillation in a prospective community-based cohort. J Intern Med. 2021;289(5):700–8. https://doi.org/10.1111/joim.13194.
Elliott P, Muller DC, Schneider-Luftman D, et al. Estimated 24-Hour Urinary Sodium Excretion and Incident Cardiovascular Disease and Mortality Among 398 628 Individuals in UK Biobank. Hypertension. 2020;76(3):683–91. https://doi.org/10.1161/HYPERTENSIONAHA.119.14302.
Kalogeropoulos AP, Georgiopoulou VV, Murphy RA, et al. Dietary sodium content, mortality, and risk for cardiovascular events in older adults: the Health, Aging, and Body Composition (Health ABC) Study. JAMA Intern Med. 2015;175(3):410–9. https://doi.org/10.1001/jamainternmed.2014.6278.
Acknowledgements
We thank the staff of the National Center for Health Statistics of the Centers for Disease Control for building and maintaining the NHANES database. Thank you to all the volunteers and participants
Funding
This work was supported by the Key Research and Development Project of Jiangsu Province (Grant Nos. BE2022780); the National Natural Science Foundation of China (Grant Nos. 82070455, 82370457).
Author information
Authors and Affiliations
Contributions
Zhongqun Wang,Haipeng Yao,and Xiabo Wang designed the research. Haipeng Yao, Xunan Wu,Lifeng Li, and Jingzheng Chen collected, analyzed the data, and drafted the manuscript. Xiabo Wang,Yi Liu, and Yiliu Chen reviewed and revised the manuscript. All authors critically revised manuscripts of significant intellectual content. All authors contributed to the article and approved the submitted version. Haipeng Yao,and Xiabo Wang contributed equally to this work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The National Center for Health Statistics (NCHS) Institutional Review Board has approved the NHANES research plan. All information was publicly available, so the consent of the medical ethics committee was not required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yao, H., Wang, X., Wu, X. et al. Sex differences in association of healthy eating pattern with all-cause mortality and cardiovascular mortality. BMC Public Health 24, 2363 (2024). https://doi.org/10.1186/s12889-024-19883-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19883-y