Abstract
Background
Currently, obesity has been recognized to be an independent risk factor for osteoarthritis (OA), and the Metabolic Score for Visceral Fat (METS-VF) has been suggested to be potentially more accurate than body mass index (BMI) in the assessment of obesity. Nevertheless, the correlation of METS-VF with OA has not been obviously revealed yet. Therefore, this study aimed to delve into the potential relationship between METS-VF and OA.
Methods
By examining data from the NHANES (2009–2018), weighted multivariate logistic regression analyses were used for assessing the correlation between METS-VF and OA. Subgroup analyses were then performed to validate the findings. Moreover, the nonlinear relationship between the two was assessed by restricted cubic spline (RCS). Receiver operating characteristic (ROC) curves were plotted to examine the diagnostic accuracy of METS-VF versus previous obesity index for OA.
Results
This study involved 7639 participants. According to our results, METS-VF was notably related to an elevated risk of OA, regardless of the METS-VF and the trend of positive association was more pronounced with the elevating METS-VF level (p for trend < 0.05). Subgroup analyses showed that the positive association between METS-VF and prevalence of osteoarthritis persisted in all populations with different characteristics, confirming its validity in all populations. Besides, RCS results showed a significant non-linear relationship between METS-VF and OA (p-non-linear < 0.05). As indicated by the ROC curve analysis results, METS-VF was a superior predictor of OA to BMI and HC.
Conclusions
This study finds a possible nonlinear positive correlation between METS-VF and the risk of OA. In addition, METS-VF may serve as an indicator for the more accurate diagnosis of OA and provide a new way to further evaluate the relationship between visceral fat and OA.
Similar content being viewed by others
Background
Osteoarthritis (OA) refers to a chronic disease that affects joint cartilage, resulting in damage to the subchondral bones, meniscus, ligaments, moreover, it often involves the knees, hips, hands and feet [1]. It is a clinical condition characterized by progressive joint pain, swelling, stiffness, and dysfunction. The prevalence and disability rate of OA are increasing year by year, and OA has been the second most prevalent and disabling disease after heart disease [2]. According to Cross M, the OA-related disability cases elevated from 10.5 million in 1990 to 17.1 million in 2010 [3]. Globally, the disease affects about 18% of women and 10% of men aged 60 years and over. About 80% of these patients have limited mobility, while one in four affects daily life [4, 5].
In recent studies, OA is recognized as a multifaceted disease affected by a number of causative factors. Senescence, genetics, obesity, and imbalance of metabolic homeostasis have been identified as the potential risk factors for OA [6,7,8]. Currently, with population aging and the rising obesity rate, the risk of obesity-induced OA, type 2 diabetes mellitus, hypertension, cardiovascular disease, sleep disorders, and premature death is also on the increase [9]. Internationally, the body mass index (BMI) has been widely applied in assessing weight status and health risks associated with obesity in an individual. However, despite its widespread use as a simple clinical indicator, BMI has several limitations and may not provide a full and accurate picture of an individual’s overall health status [10]. As reported in some studies, there may be significant differences in the amounts of visceral adipose and muscular tissues and in metabolic profiles among individuals with the same BMI [11, 12].Currently, waist circumference (WC), hip circumference (HC), and waist-to-hip ratio (WHR) have been gradually used as the predictors of obesity in OA [13]. However, similar to BMI, they are associated with certain drawbacks. Meanwhile, magnetic resonance imaging (MRI), the gold indicator for evaluating visceral adipose tissue, has limited the researchers’ discussion on the relationship between visceral adiposity and OA due to its high cost [8]. Therefore, a more reliable approach is to identify indicators that can more accurately reflect the level of visceral adiposity for predicting OA.
In recent years, the Metabolic Score for Visceral Fat (METS-VF) has been reported to be highly efficiently assess a variety of diseases [14, 15]. However, the accuracy of using METS-VF as an indicator of OA has not been explored until now. In order to explore the relationship between METS-VF and OA, this cross-sectional study was conducted based on data from the National Health and Nutrition Examination Survey (NHANES).
Materials and methods
Data sources and study population
NHANES is a deinstitutionalized two-year survey of samples of the U.S. population held by the Centers for Disease Control and Prevention (CDC), hoping to assess the health and dietary status of the U.S. population. It incorporates multiple face-to-face interviews, physical examinations, questionnaires, and laboratory tests, and data are obtained through a multistage probability sampling design. Participants are provided with the institutional informed consent prior to both the interview and examination phases. All procedures are standardized by the NCHS Research Ethics Review Board according to the U.S. Department of Health and Human Services (HHS) Policy for the Protection of Human Research Subjects. For a detailed description of the NHANES survey methodology and data sources, please access the website (http://www.cdc.gov/nchs/nhanes/index.htm).
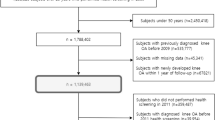
Based on pertinent questionnaires and laboratory examination results, a cross-sectional study was conducted in this work using five individual NHANES survey cycles (2009–2018). A total of 49,693 individuals participated in this survey, and participants with the following missing information were excluded, including METS-VF (n = 35301), OA (n = 4103), age < 20 years (n = 233), total energy deficit (n = 558), and total energy intake extremes < 500 or > 5,000 kcal/day in females, and < 500 or > 8,000 kcal/day in male individuals (n = 57), level of education (n = 6), poverty income ratio (n = 834), smoking (n = 10), alcohol consumption (n = 650), hypertension (n = 13), diabetes (n = 224), coronary heart disease (n = 17), and serum calcium (n = 48). Finally, 7639 participants were enrolled in this study for final analysis (Fig. 1).
Assessment of osteoarthritis
OA was assessed using a NHANES codebook questionnaire in the form of “Has a doctor or other health professional ever told you that you have arthritis?“. The response options were “yes” or “no”. Those who chose “yes” went on to the next round of the questionnaire with the question “What type of arthritis is this?” Those who selected the option of OA were included in the study.
Assessment of visceral fat metabolic score
The METS-VF is an index which can be adopted for assessing the visceral fat accumulation and associated metabolic health of an individual. In this study, METS-VF was calculated using the following formula: METS-VF = 4.466 + 0.011[(Ln (METS-IR))3] + 3.239[(Ln (WHtR))3] + 0.319(Sex) + 0.594(Ln (Age)) (“male” = 1, “female” = 0). The metabolic insulin resistance score (METS-IR) was calculated with the formula: METS-IR = Ln [(2 × fasting glucose) + fasting triglycerides) × BMI] / [Ln (high-density lipoprotein cholesterol)]. In addition, waist-to-height ratio (WHtR) was calculated by WHtR = WC / HT.
Covariates
In addition to the variables of OA and METS-VF in the questionnaire, a number of potential confounders were investigated, including age, gender, race, education level, poverty-to-income ratio, alcohol intake (Categorized as whether they consume at least 12 alcoholic beverages per year), smoking status (Categorization is determined by whether or not you have “smoking at least 100 cigarettes in your life” and whether or not you smoke now), work intensity, recreational intensity, serum calcium level (mg/dL), vitamin D (nmol/L) level, hypertension, diabetes, and coronary heart disease, dietary intake factors (containing energy intake, fat intake, protein intake, carbohydrate intake, total saturated fatty acid intake, total monounsaturated fatty acids intake, and polyunsaturated fat intake). All of the participants underwent two 24-hour dietary recalls. As shown in this particular analysis, the average consumption of the two recalls was used as a dietary intake factor for inclusion in the study.
Statistical analysis
Statistical analyses were conducted with Stata 17.0 and R (version 4.3.1), with two-sided p < 0.05 being considered of statistical significance. Considering the complex sampling design and ensuring the nationally representative estimates, all analyses were adjusted for the survey design and weighting variables, for which a simple linear scaling of the 2-year weights (the original 2-year sample weights divided by 2) was performed. In this study, continuous variables were shown to be weighted survey means and standard deviations and analyzed by survey-weighted linear regression, and categorical variables were indicated by weighted survey ratios (%) and 95% confidence intervals (CIs) and analyzed by survey-weighted chi-square tests. Besides, the association of OA with quartiles of the METS-VF index was examined using the multivariable-adjusted logistic regression models. According to the guidelines [16], three models were developed to explore the association between METS-VF and OA. Model 1 was unadjusted for variables, Model 2 was adjusted for age and sex, while Model 3 was adjusted for all the covariates. Thereafter, the four categorical variables of METS-VF were transformed into continuous variables and incorporated into a weighted multivariate logistic regression model to identify the potential linear trends in the association. Next, subgroup analyses stratified by age, gender, race, education, household income poverty, smoking, alcohol consumption, blood pressure, and blood glucose were also conducted. Furthermore, dose-response relationships in the logistic regression model 3 were assessed with restricted cubic spline (RCS) strips located at the 4 nodes of the exposure distribution at the 25, 50, 75, and 95th percentiles, and the median METS-VF was used as the reference value for odds ratio (OR) = 1. Finally, the predictive effects of METS-VF and BMI on OA were assessed by receiver operating characteristic (ROC) curve and the area under the curve (AUC).
Results
The characteristics of OA in the study population are presented in Table 1. Ultimately, totally 7639 participants were included for final analysis. Overall, there existed significant differences (p < 0.05) in the characteristics of the study variables, except for total monounsaturated fatty acids and polyunsaturated fat. The results in Table 1 showed that participants who developed OA tended to be older, females, non-Hispanic white, consumed alcohol, high vitamin D, low energy, high serum calcium, had ever smoked cigarettes, engaged in moderate physical activity and moderate recreation, and had moderate percentage of income from poverty, compared with those who did not develop OA, received education beyond high school, had high blood pressure, and no diabetes. To further supplement the information in Table 1, the METS-VF index was categorized by quartiles and all variables (Supplementary Table 1) were recounted. According to the results of Supplementary Table 1, with the increasing METS-VF, age, percentage of males, percentage of education higher than high school, and percentage of people with diabetes, hypertension, and OA were significantly higher. The overall trend and percentage were consistent with the findings in Table 1. A weighted multivariate logistic regression analysis was carried out on the three models, revealing a positive correlation between METS-VF and the prevalence of OA relative to the reference level (Q1). Notably, this positive correlation persisted after adjusting for all covariates (Q2: OR = 1.14, 95% CI: 1.02−2.02; Q3: OR = 1.93, 95% CI: 1.39−2.69; Q4: OR = 2.33, 95% CI: 1.65−3.28), and became more pronounced with the increase of METS-VF in Table 2 (p for trend < 0.01). Meanwhile, the METS-VF index was also transformed from a categorical variable to a continuous variable and incorporated into three models for weighted multivariate logistic regression analysis. The final results were consistent with those mentioned above. As revealed by the findings of model 3, the risk of developing OA increased by 23% for each unit increase in the METS-VF index (OR = 1.23, 95% CI: 1.14−1.33) (p < 0.01) (Supplementary Table 2). To further evaluate the robustness of the association between the METS-VF index and OA, subgroup analyses were later performed on age, sex, race, education, household income poverty, smoking, alcohol consumption, blood pressure, and blood glucose and the final results are presented in a forest plot (Fig. 2). As a result, a positive association between METS-VF and the prevalence of OA persisted across all different population characteristics (Table 3). Typically, the more significant population characteristics were 40−59 years (OR = 1.24, 95% CI: 1.10−1.39), female (OR = 1.26, 95% CI: 1.14−1.40), Non-Hispanic White (OR = 1.21, 95% CI: 1.10−1.32), and less than high school (OR = 1.32, 95% CI: 1.16−1.50), high poverty of family income (OR = 1.26, 95% CI:1.11−1.43), non-smoking (OR = 1.23, 95% CI: 1.10−1.38), alcohol consumption (OR = 1.23, 95% CI: 1.12−1.34), non-hypertension (OR = 1.24, 95% CI:1.11−1.38) and non-diabetes (OR = 1.24, 95% CI: 1.14−1.34). To elucidate whether there existed a nonlinear relationship between METS-VF and the prevalence of OA, the findings were tested by RCS. The findings showed that there existed a significant nonlinear relationship between METS-VF and OA (p-non-linear < 0.05) (Fig. 3). Ultimately, we utilized the AUC values of ROC curves and the cut-off to evaluate the diagnostic potential of METSVF, BMI and hip circumference (HC) for OA. As a result, the AUC value of METS-VF (0.6241) was significantly higher than those of BMI (0.5874) and HC (0.512), and the corresponding cut-off values were 9.552, 29.695, and 32.850, respectively, suggesting that METS-VF might be superior to BMI and HC in the diagnosis of OA (Fig. 4).
Subgroup analysis of the association between METS-VF and osteoarthritis. All the covariates in Table 1 were adjusted
The RCS plot between METS-VF and osteoarthritis. All the covariates in Table 1 were adjusted. The area enclosed by the solid red line and the transparent purple line represents the estimated ORs and its 95%confidence intervals. (OR, odds ratio)
Discussion
By utilizing the large sample size of the NHANES database, this study indicated a nonlinear positive association between METS-VF and the prevalence of OA. Besides, our results demonstrated a gradually increasing trend of the prevalence of OA with the increasing METS-VF levels, and the relationship persisted after adjusting for all variables. In addition, compared with BMI and HC, METS-VF was more sensitive in predicting the risk of OA.
OA is a disease characterized by degenerative changes in the joints, usually resulting in damage to articular cartilage. With the continuous progress in medical technology, significant advancement has been made in the study on the causes and treatments of OA. However, the prevalence and global health burden of OA continue to increase year by year [17]. Obesity, which has been a vital public health challenge worldwide, is recognized to be a vital risk factor for the development and progression of OA. Internationally, BMI is commonly adopted as an indicator for assessing the risk of obesity and OA. However, an increasing number of researchers have started to question the accuracy of BMI in assessing the risk of OA and its limitations in accurately assessing an individual’s true obesity status [18]. This is because that BMI does not accurately reflect adipose and muscle tissues, nor does it accurately reflect the differences in fat distribution by age and sex [19]. METS-VF, a new indicator for evaluating visceral obesity, has been demonstrated to be potentially superior to BMI in the diagnosis of various systemic disorders [8, 20], consistent with the results in our study (Fig. 3). This is associated with the fact that METS-VF contains several indicators responsive to the influences on disease progression, such as age, gender, blood glucose, and METS-IR. With age, visceral fat usually accumulates in the waist and abdomen, resulting in the so-called “central obesity”. “Central obesity” often influences the development of OA due to factors such as inflammation, oxidative stress, joint loading, and changes in hormone levels [17]. The high visceral fat levels have been suggested to lead to an overall decrease in androgen production [21]. While such decrease in the androgen level diminishes the protective effect of articular cartilage, reduces the attachment of periarticular muscle strength, and increases the localized joint inflammation [22]. When men enter the middle age, they are more probably to develop a higher level of visceral adiposity than those who are more likely to be obese. Moreover, as men enter the middle age and beyond, the testosterone levels decline, leading to more fat deposition in the visceral fat storage reservoirs, while the subcutaneous fat decreases significantly after the age of 50 years [23]. This phenomenon also explains the greater concentration of age in the mid-50s in the age means of METS-VF after four classifications and in the subgroup analyses. According to our study, OA patients were more likely to develop vascular disease and diabetes, and the risk of vascular disease and diabetes increased progressively with the increasing METS-VF levels, which may be related to insulin resistance. In some studies, insulin resistance has been demonstrated as a major factor influencing the relationship of diabetes with OA [24]. METS-IR has been widely used in the assessment of diseases including cardiovascular disease and diabetes, and exhibits significant advantages in assessing type 2 diabetes and reflecting the degree of insulin resistance [25]. The amount of visceral adiposity is a key factor influencing the changes in insulin sensitivity. Generally, smaller adipocytes are more sensitive to insulin, whereas larger adipocytes may probably be insulin-resistant [26]. Visceral fat contains more large adipocytes with insulin resistance, hyper-lipolysis, and resistance to the anti-lipolytic effects of insulin [27]. Visceral cells with insulin-resistant properties are more likely to contribute to the decreased bone density, lipid metabolic disturbance, and enhanced inflammation levels, which can hasten the development of OA. Unfortunately, the statistical results for the hypertensive and diabetic subgroups differed from the results of previous studies after considering a wide range of specific characteristics.
We also observed that some participants with specific characteristics were more likely to exhibit a correlation between METS-V and OA. For instance, the high-intensity recreational and work activities might reduce the risk of OA, which might be related to weight reduction due to the high intensity exercises [28]. Body weight loss is one of the effective ways to lower the risk of METS-VF on OA. As reported in some studies, weight loss can help reduce the prevalence of diabetes, OA, and other diseases. Also, visceral fat is more sensitive to weight loss, and all forms of exercises have a greater impact on visceral fat than on subcutaneous fat. In furthermore, the non-Hispanic white group exhibited a higher risk of OA compared to the other population. This may be related to the relatively higher risk of obesity in the non-Hispanic white group [29], which exacerbates the METS-VF risk associated with OA. Studies have shown that non-Hispanic individuals tend to consume more energy [30], which may contribute to their increased risk of OA. Based on the above, we suggest that the non-Hispanic white population should reduce their energy intake, especially fat intake; meanwhile, the other population should enhance their health education in order to work together to prevent the occurrence of OA. In addition, the higher levels of vitamin D are related to a higher risk of OA [31], consistent with our findings (Table 1). As pointed out in previous studies (HuangHanRozi et al., 2024), there is a curvilinear positive correlation between lipid accumulation products and OA, conforming to our findings. The difference is that our study included age factors affecting the occurrence of OA, waist-to-height ratio indexes that reflected obesity, and metabolic scores of insulin resistance affecting the occurrence of diabetes and other metabolic diseases, which also provided more accurate indicators for subsequent in-depth exploration of the relationship between visceral adiposity and OA.
Although the precise mechanisms linking visceral fat and the development of OA remain elusive, the recognized mechanisms probably fall into three categories, namely, mechanical, inflammatory, and metabolic factors. With the accumulation of visceral fat, the increased mechanical loading, particularly on weight-bearing joints, places a greater stress on articular cartilage, thereby accelerating cartilage wear and degradation, while stimulating subchondral bone proliferation and sclerosis [32]. Additionally, the excessive mechanical loading may lead to an elevation in the levels of inflammatory factors IL-1β and TNF-α and the activation of associated channels [33]. Biomechanics also supports the above view. Furthermore, studies have indicated that visceral fat is metabolically active and often impacts the progression of certain metabolic diseases including type II diabetes to affect OA. It is attributed to the fact that the high blood glucose levels accelerate oxidative stress in chondrocytes and the formation of glycosylation end-products (AGEs) in the cartilage [34]. Besides, visceral fat is more susceptible to infiltration by inflammatory cells, and has a greater ability to produce proteins such as TNF-a, CRP, and IL-6 [35, 36]. Finally, reactive adipokines induced by abnormal visceral adiposity can also affect OA through exacerbating inflammation, affecting insulin sensitivity, and activating the cartilage degradation mechanisms [37, 38].
Certain significant strengths and drawbacks should be noted in this study. Firstly, the NHANES database, which has an adequate and representative sample size, was selected in the study, which contributes to the statistical efficacy and credibility of the results. Secondly, this is the first cross-sectional study to explore the correlation between visceral fat metabolism and the prevalence of OA, providing a foundation for future studies on visceral fat and OA. Finally, the study also identified a nonlinear relationship between METS-VF and the risk of OA, providing additional support for a threshold effect. Nonetheless, there are still some limitations in this study. First of all, we were unable to determine the causality or completely exclude possible bias from confounding factors owing to the cross-sectional study nature, which is one of the main drawbacks of the study. Therefore, future cohort studies are needed to validate the results. Second, although the study included as many relevant covariates as possible, the effects of other potential covariates could not be completely excluded. In addition, many of the key variables including OA were determined by questionnaires, which might induce recollection bias in the results. Moreover, imaging materials supporting the determination of visceral fat and OA are lacking. So, further validation of the results using imaging modalities such as CT and MRI are warranted.
Conclusion
In this study, a possible nonlinear positive relationship between METS-VF and the risk of OA is detected using NHANES data. In addition, METS-VF may serve as a more accurate diagnostic marker of OA and provide a new avenue for further evaluation of the relationship between visceral fat and OA.
Data availability
https://www.cdc.gov/nchs/nhanes/.
Abbreviations
- METS-VF:
-
Metabolic Score for Visceral Fat
- OA:
-
Osteoarthritis
- NHANES:
-
National Health and nutrition examination survey
- RCS:
-
restricted cubic spline
- ROC:
-
receiver operating characteristic
- BMI:
-
Body mass index
- HC:
-
hip circumference
- OR:
-
Odds ratio
- CI:
-
Confidence interval
References
Hunter DJ, Felson DT, Osteoarthritis. BMJ. 2006;332:639–42.
Liu Q, Niu J, Li H, Ke Y, Li R, Zhang Y, et al. Knee symptomatic osteoarthritis, walking disability, NSAIDs use and all-cause Mortality: Population-based Wuchuan Osteoarthritis Study. Sci Rep. 2017;7:3309.
Cross M, Smith E, Hoy D, Nolte S, Ackerman I, Fransen M, et al. The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Ann Rheum Dis. 2014;73:1323–30.
Ma VY, Chan L, Carruthers KJ. Incidence, prevalence, costs, and impact on disability of common conditions requiring rehabilitation in the United States: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, rheumatoid arthritis, limb loss, and back pain. Arch Phys Med Rehabil. 2014;95:986–e9951.
Woolf AD, Pfleger B. Burden of major musculoskeletal conditions. Bull World Health Organ. 2003;81:646–56.
Bruyère O, Cooper C, Arden N, Branco J, Brandi ML, Herrero-Beaumont G, et al. Can we identify patients with high risk of osteoarthritis progression who will respond to treatment? A focus on epidemiology and phenotype of osteoarthritis. Drugs Aging. 2015;32:179–87.
Deveza LA, Loeser RF. Is osteoarthritis one disease or a collection of many? Rheumatology (Oxford). 2018;57:iv34–42.
Kapoor N, Jiwanmall SA, Nandyal MB, Kattula D, Paravathareddy S, Paul TV, et al. Metabolic score for visceral Fat (METS-VF) Estimation - A Novel cost-effective obesity Indicator for visceral adipose tissue estimation. Diabetes Metab Syndr Obes. 2020;13:3261–7.
Godziuk K, Hawker GA. Obesity and body mass index: past and future considerations in osteoarthritis research. Osteoarthritis Cartilage. 2024;S1063-4584(24)00042 – 6.
Gutin I. Body mass index is just a number: conflating riskiness and unhealthiness in discourse on body size. Sociol Health Illn. 2021;43:1437–53.
Gonzalez MC, Correia MITD, Heymsfield SB. A requiem for BMI in the clinical setting. Curr Opin Clin Nutr Metab Care. 2017;20:314–21.
Rask-Andersen M, Johansson Å. Illuminating the healthy obese phenotype. Nat Metab. 2023;5:193–4.
Lyu L, Cai Y, Xiao M, Liang J, Zhang G, Jing Z, et al. Causal relationships of General and Abdominal Adiposity on Osteoarthritis: a two-sample mendelian randomization study. JCM. 2022;12:320.
Bello-Chavolla OY, Antonio-Villa NE, Vargas-Vázquez A, Viveros-Ruiz TL, Almeda-Valdes P, Gomez-Velasco D, et al. Metabolic score for visceral Fat (METS-VF), a novel estimator of intra-abdominal fat content and cardio-metabolic health. Clin Nutr. 2020;39:1613–21.
Ogden CL, Carroll MD, Fakhouri TH, Hales CM, Fryar CD, Li X, et al. Prevalence of obesity among youths by Household Income and Education Level of Head of Household - United States 2011–2014. MMWR Morb Mortal Wkly Rep. 2018;67:186–9.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The strengthening the reporting of Observational studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Bull World Health Organ. 2007;85:867–72.
Park D, Park Y-M, Ko S-H, Hyun K-S, Choi Y-H, Min D-U, et al. Association of general and central obesity, and their changes with risk of knee osteoarthritis: a nationwide population-based cohort study. Sci Rep. 2023;13:3796.
Huang J, Han J, Rozi R, Fu B, Lu Z, Liu J, et al. Association between lipid accumulation products and osteoarthritis among adults in the United States: a cross-sectional study, NHANES 2017–2020. Prev Med. 2024;180:107861.
Hildebrand S, Stümer J, Pfeifer A. PVAT and its relation to Brown, Beige, and White Adipose tissue in development and function. Front Physiol. 2018;9:70.
Feng Y, Yang X, Li Y, Wu Y, Han M, Qie R, et al. Metabolic score for visceral Fat: a novel predictor for the risk of type 2 diabetes mellitus. Br J Nutr. 2022;128:1029–36.
Freedland ES. Role of a critical visceral adipose tissue threshold (CVATT) in metabolic syndrome: implications for controlling dietary carbohydrates: a review. Nutr Metab (Lond). 2004;1:12.
Freystaetter G, Fischer K, Orav EJ, Egli A, Theiler R, Münzer T, et al. Total serum testosterone and Western Ontario and McMaster universities osteoarthritis Index Pain and function among older men and women with severe knee osteoarthritis. Arthritis Care Res (Hoboken). 2020;72:1511–8.
Ibrahim MM. Subcutaneous and visceral adipose tissue: structural and functional differences. Obes Rev. 2010;11:11–8.
Zaharia OP, Pesta DH, Bobrov P, Kupriyanova Y, Herder C, Karusheva Y, et al. Reduced muscle strength is Associated with insulin resistance in type 2 diabetes patients with osteoarthritis. J Clin Endocrinol Metab. 2021;106:1062–73.
Stolar MW. Insulin resistance, diabetes, and the adipocyte. Am J Health-Syst Pharm. 2002;59:S3–8.
Salans LB, Cushman SW, Weismann RE. Studies of human adipose tissue. Adipose cell size and number in nonobese and obese patients. J Clin Invest. 1973;52:929–41.
Frayn KN. Visceral fat and insulin resistance–causative or correlative? Br J Nutr. 2000;83(Suppl 1):S71–77.
Elmaleh-Sachs A, Schwartz JL, Bramante CT, Nicklas JM, Gudzune KA, Jay M. Obesity Management in adults: a review. JAMA. 2023;330:2000–15.
Xie L, Kim J, Almandoz JP, Clark J, Mathew MS, Cartwright BR, et al. Anthropometry for predicting cardiometabolic disease risk factors in adolescents. Obesity (Silver Spring). 2024;32:1558–67.
Williams MS, McKinney SJ, Cheskin LJ. Social and Structural Determinants of Health and Social Injustices Contributing to Obesity Disparities. Curr Obes Rep. 2024;
Nielsen RL, Monfeuga T, Kitchen RR, Egerod L, Leal LG, Schreyer ATH, et al. Data-driven identification of predictive risk biomarkers for subgroups of osteoarthritis using interpretable machine learning. Nat Commun. 2024;15:2817.
Robling AG, Castillo AB, Turner CH. Biomechanical and molecular regulation of bone remodeling. Annu Rev Biomed Eng. 2006;8:455–98.
Yao Q, Wu X, Tao C, Gong W, Chen M, Qu M, et al. Osteoarthritis: pathogenic signaling pathways and therapeutic targets. Signal Transduct Target Ther. 2023;8:56.
Courties A, Sellam J. Osteoarthritis and type 2 diabetes mellitus: What are the links? Diabetes Res Clin Pract. 2016;122:198–206.
Pepys MB, Hirschfield GM. C-reactive protein: a critical update. J Clin Invest. 2003;111:1805–12.
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW. Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest. 2003;112:1796–808.
Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320:C375–91.
Tu C, He J, Wu B, Wang W, Li Z. An extensive review regarding the adipokines in the pathogenesis and progression of osteoarthritis. Cytokine. 2019;113:1–12.
Acknowledgements
We would like to thank all NHANES participants and staff.
Funding
The funding support from the National Natural Science Foundation of China (Grant no. 82374489) for this work is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
H.X., C.Z. designed the research. H.X., L.Z., K.L., J.X., and L.J. collected, analyzed the data, and drafted the manuscript. H.X., C.Z., S.Y., interpreted the data and revised the manuscript. All authors contributed to the article and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was reviewed and approved by the NCHS Ethics Review Board. The participants provided written informed consent to participate in this study.
Consent for publication
Before participating in the study, all participants signed up with informed permission.
Competing interests
The authors declare no competing interests.
Institutional review board statement
There was no requirement for institutional review board permission since the NHANES database was open to the public.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xue, H., Zhang, L., Xu, J. et al. Association of the visceral fat metabolic score with osteoarthritis risk: a cross-sectional study from NHANES 2009–2018. BMC Public Health 24, 2269 (2024). https://doi.org/10.1186/s12889-024-19722-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19722-0