Abstract
Background
Low income communities are vulnerable to non-communicable diseases (NCDs), which affect their economy and disability status. An effective approach to address the NCD burden is through the multidimensional concept of health-promoting lifestyle. Another preferred approach by the population worldwide for NCD treatment is natural health product (NHP). Studies on NHP and health-promoting lifestyle among this vulnerable population, specifically the low-income urban community, are limited. Therefore, this study, aimed at investigating the NHP knowledge and health-promoting lifestyle, and to determine the factors associated with health-promoting lifestyle in a low income urban community in Cheras, Kuala Lumpur. This study has focused on sociodemographic characteristics, annual health monitoring activities, and health status, which are modifiable and non-modifiable factors.
Methods
Phase 1 of the study involves developing the Malay-version NHP knowledge questionnaire, whereas Phase 2 involves a cross-sectional study of 446 randomly selected low-income respondents to determine their level of health-promoting lifestyle and the associated factors. The respondents’ sociodemographic, socioeconomic, health monitoring activity, health status, and NHP knowledge data were obtained using the newly developed Malay-version NHP questionnaire and the Health-Promoting Lifestyle Profile II (HPLP II) questionnaire. The independent variables include sociodemographic status, annual health monitoring activities, health status and NHP knowledge were analysed using simple and multiple linear regression.
Results
In this study, the 10-item NHP knowledge questionnaire developed in the Malay version contains two domains [safe use (eight items) and point of reference (two items)] (total variance explained: 77.4%). The mean of NHP knowledge score was 32.34 (standard deviation [SD] 7.37). Meanwhile, the mean score of health-promoting lifestyle was 109.67 (SD 25.01). The highest and lowest scores of health-promoting lifestyles are attributed to spiritual growth and physical activity, respectively. Ethnicity is associated with a higher health-promoting lifestyle level, same goes to the occupational status − NHP knowledge interaction. “Unclassified” education status and annual blood glucose level monitoring are associated with a lower level of health-promoting lifestyle.
Conclusion
A new questionnaire in Malay version was developed to measure NHP knowledge. Compared to other subpopulations, the respondents’ health-promoting lifestyle levels in this study were low, associated with ethnicity, education status, and health monitoring activities. The findings provided insight into the interaction between NHP knowledge and occupational status, which is associated with a higher health-promoting lifestyle level. Accordingly, the future health-promoting lifestyle intervention programmes in healthcare delivery should target these factors.
Similar content being viewed by others
Introduction
Rapid urbanisation and increased population density is a worsening scenario among urban low-income communities [1]. Such communities are vulnerable to non-communicable diseases (NCDs), which are a major public health concern due to their influence on economic growth, disability, and premature death [2,3,4]. Health-promoting lifestyle is one of the best approaches to reduce the NCD burden on these vulnerable populations [5, 6].
Health-promoting lifestyle is a multidimensional concept in which self-initiated action, behaviour, and perception contribute to maintaining and improving self-actualisation and wellness. The health-promoting lifestyle is based on the behaviour, health beliefs, and Pender’s health promotion model [7]. Different populations record varying health-promoting lifestyle scores. For example, the mean of health-promoting lifestyle score among low-income Polish men was 70.98 (standard deviation, SD = 16.38) [8], while those of Iranian and Turkish women were 112.2 (SD = 16.1) [9] and 126.81 (SD = 19.2) [10], respectively. These differences are attributed to the different study populations and instruments used to measure the health-promoting lifestyle level.
The most widely applied health-promoting lifestyle instrument is the Health-Promoting Lifestyle Profile II (HPLP II), which uses a holistic and multidimensional approach [11,12,13,14,15,16]. HPLP II comprises a set of questionnaires that cover six scales (health responsibility, physical activity, nutrition, spiritual growth, interpersonal relations, and stress management) [17, 18]. Understanding of these factors is crucial to plan for targeted health programmes to improve the health-promoting lifestyle. Many factors are associated with the practice of health-promoting lifestyle, such as sociodemographic factors, namely age [13, 18], gender [11, 13], marital status [9, 13], education status [9, 13, 18], and socioeconomic status [2]. The health-promoting lifestyle is significantly associated with the presence of comorbidities such as cardiocerebrovascular disease [13].
Health monitoring activities involve any behaviours related to individual monitoring of health parameters, encompassing physical activity, dietary intake, blood glucose, and blood pressure [19,20,21]. Health monitoring activity is associated with a higher level of health-promoting lifestyle [19, 20]. Natural health products (NHPs) are defined as “naturally occurring substances that are used to restore or maintain good health and must be licensed for use”. For example, NHPs include probiotics, herbal remedies, vitamins and minerals, homoeopathic medicines, traditional medicines, as well as amino acids and essential fatty acids [22]. Up to 70 − 80% of the worldwide population prefer NHPs as the prime source of healthcare and alternative for NCD treatment [23,24,25]. The usage of NHPs is significantly associated with health-promoting lifestyle [26] and stress management [27], while safe usage of NHPs is associated with the user’s knowledge level [23, 24].
In Malaysia, the low-income community is defined as those with monthly earnings < RM4850 [28]. Although only 14.1% of Malaysians are considered having low-income, almost 90% of them live in urban areas [29, 30]. Furthermore, 8.1% of Malaysians have at least three lifestyle-related NCDs (hypertension, diabetes, and high cholesterol), which are the leading cause of death among Malaysians [31]. Thus, the health-promoting lifestyle approach is essential to reduce the NCD burden in Malaysia. Moreover, understanding of the health-promoting lifestyle and associated factors among urban low-income communities is crucial in the planning of health programme targeting this subpopulation.
HPLP II has been used to examine undergraduates [11, 12, 14, 32], elderly people [13], women [15, 16], and a low-income community at a suburban community health centre [18]. However, local studies assessing the health-promoting lifestyle-associated factors are limited. In this study, it is postulated that NHP knowledge is associated with health-promoting lifestyle, but questionnaires to measure NHP knowledge in the local setting are limited. Accordingly, we developed a Malay-version NHP knowledge questionnaire to investigate the NHP knowledge and health-promoting lifestyle among low-income community. This study also aimed at measuring the health-promoting lifestyle level and its associated factors in this study population.
Materials and methods
Study phase and design
Phase 1 of the study involved developing an NHP knowledge questionnaire, while Phase 2 involved a cross-sectional study to determine the level of health-promoting lifestyle and the associated factors in a low-income urban community in Cheras, Kuala Lumpur. The Universiti Kebangsaan Malaysia (UKM) Medical Research Ethics Committee approved this study (project code: FF-2021-497), and all respondents had been informed and they provided written consent.
Study setting and population
The study was conducted in Kuala Lumpur, a city that has experienced rapid economic development and population growth with a 100% urban community. Kuala Lumpur is made up of 11 districts [33, 34]. Cheras District had been selected due to convenience as it features numerous low-cost flats housing Malaysians of many ethnicities [34, 35]. A list of Cheras low-cost flats was obtained from the Kuala Lumpur City Hall, and Flat Sri Kota was selected via a simple random sampling. The inclusion criteria are age ≥ 18 years, Malaysian citizen, and able to read and understand Malay. The exclusion criteria are monthly income > RM4849 and being dependent on daily living activities.
Development of NHP knowledge questionnaire
The preliminary questionnaire was developed in English based on the literature [24, 36]. Ten items were developed with scores using the 5-point Likert scale – 1 (very little knowledge), 2 (little knowledge), 3 (medium knowledge), 4 (much knowledge), and 5 (very much knowledge). The content validity was examined by five experts (public health specialists and pharmacists) through discussion until they reach the consensus. The simplicity, validity, and sentence structure of the items were reviewed via professional evaluation. Then, the preliminary questionnaire underwent forward (English-to-Malay) and backward (Malay-to-English) translations.
A pre-test was conducted for face validity, involving five respondents from Flat Sri Kota. The respondents were asked to answer and give comments on the wording used in the questionnaire. There was no modification needed. Subsequently, a pilot study was conducted with a preliminary questionnaire involving 40 respondents from Flat Sri Kota via systematic random sampling [37]. The respondents involved in the pre-test and pilot study were excluded from the sample frame in the field study. The questionnaire validity was examined using the exploratory factor analysis (principal component extraction with Varimax rotation). Retained factors are determined based on the Kaiser criterion with eigenvalue > 1, while the determination of retained items is based on factor loading > 0.40. A Kaiser-Meyer-Olkin (KMO) value > 0.50 indicates adequate sample size, while a significant Bartlett’s value < 0.05 is accepted for the sphericity valuation test [38]. The questionnaire reliability is evaluated using Cronbach’s alpha to assess the internal consistency of all items and each domain. An acceptable value of α ≥ 0.50 is set for this study [39, 40].
Health-promoting lifestyle level and the associated factors
A cross-sectional study was conducted involving the Flat Sri Kota residents. The respondents were selected via a systematic random sampling from the list of residents provided by the residents’ Joint Management Board (JMB). A minimum sample size of 382 was calculated based on the previous study [18] using the two-means formula for continuous outcome [41]. Considering a 20% non-response rate, 446 respondents were recruited to reach a minimum sample size for this study. The health-promoting lifestyle was measured using the validated Malay-version HPLP II questionnaire [17]. The translation from English to Malay was conducted using standard forward and backward translation procedures [17]. The content validity was done by five experts and face validity was conducted with 10 undergraduate students [17].
The validated Malay-version HPLP II questionnaire consists of 50 items, with two items with the factor loading of less than 0.40 (0.339 and 0.373) were removed as compared to the original version with 52 items. [17]. These two removed items measure the interpersonal relationship and nutrition domain. However, this study used the 52 items of the Malay-version HPLP II questionnaire as per the original version [42]. It consists of six domains - (i) health responsibility, (ii) physical activity, (iii) nutrition, (iv) spiritual growth, (v) interpersonal relations, and (vi) stress management. Each domain is scored on four-point Likert scale and scores from these six domains are then combined to calculate the total HPLP II score [17]. The HPLP II score provides a comprehensive assessment of an individual’s health-promoting lifestyle [17].
Data collection
Data were collected from December 2021 to February 2022 using a self-administered questionnaire that was distributed by hand to the respondents. The completion of the questionnaire was assessed upon collection from the respondents. The questionnaire contains five sections − i) sociodemographic and socioeconomic characteristics, ii) health monitoring activity, iii) health status, iv) NHP knowledge, and v) health-promoting lifestyle. The sociodemographic and socioeconomic characteristics are age, gender, ethnicity, marital status, education status, occupational status, and monthly income. The health monitoring activity was measured by four questions with “yes” or “no” responses. The questions are based on annual activity of (i) blood pressure monitoring, (ii) weight measurement, and (iii) blood glucose level monitoring.
Meanwhile, health status was measured by four questions based on: (i) presence of comorbidities (“yes” or “no” responses − diabetes mellitus, hypertension, heart disease, stroke, asthma, arthritis, tuberculosis, dengue fever, chronic skin diseases, anaemia, kidney disease, eye diseases affecting vision except refractive error, congenital disorder, and cancer), (ii) duration of comorbidities, (iii) the personnel who had diagnosed the comorbidities, and (iv) treatment visit frequency. NHP knowledge was measured as a continuous variable (mean of total score), where a higher score indicates a higher knowledge level. The health-promoting lifestyle was measured using the validated Malay-version HPLP II questionnaire of 52 items [17] as a continuous variable (mean of total score), and a higher score indicates a higher health-promoting lifestyle level. Each item is scored using the 4-point Likert scale: 1 (never), 2 (sometimes), 3 (often), and 4 (routinely) [17].
Statistical analyses
The data were analysed using SPSS version 26. Categorical data are described as the frequency (n) and percentage (%), while continuous data are described in the form of mean and SD. The associations between the independent variables and the mean of health-promoting lifestyle scores were determined using simple and multiple linear regression analyses. Multivariable analysis has a significant role in controlling confounders such as socio-demographic factors [43]. Interaction analyses were carried out to demonstrate synergy between factors and enhance the model’s predictive power [44]. The significance level was set at p < 0.05.
Results
Development of NHP knowledge questionnaire
The mean respondent age was 50.35 (SD 16.40) years. There was almost equal distribution between the 18–39-year (32.5%), 40–59-year (30.0%), and ≥ 60-year (37.5%) age groups. The majority of the respondents are female (62.5%), Malay (90.0%), married (62.5%), self-employed (20.0%) and worked in the private sector (20.0%). Almost half of them were with secondary education (47.5%). The construct validity analysis demonstrated that the KMO value was 0.85 and the Bartlett’s test score was χ² = 364.09 (p < 0.001). Factor numbers were extracted based on eigenvalues ≥ 1 and scree plots. Two-factor numbers were obtained with a total variance explained of 77.4% (Table 1). All 10 items have factor loading > 0.40. Reliability analysis demonstrated that Cronbach’s alphas for the total items, first domain, and second domain were 0.93, 0.95, and 0.55, respectively. The pilot study developed the final questionnaire with two domains: (i) safe use (eight items), and (ii) point of reference (two items).
Health-promoting lifestyle level and the associated factors
A total of 446 Flat Sri Kota residents were selected in the study (response rate: 100%). Table 2 depicts the respondents’ sociodemographic characteristics. The mean respondent age was 49.02 (SD 16.34) years. There was almost equal distribution between the 18–39-year (32.3%), 40–59-year (34.5%), and ≥ 60-year (33.2%) age groups. Up to 41.3% of the respondents are female and the majority are Malay (92.6%). A total of 64.6% of respondents were married and 55.8% had secondary education. Up to 28.9% of the respondents were unemployed while 25.8% worked in the private sector (25.8%). Most respondents underwent an annual health monitoring activity such as blood pressure monitoring (88.6%), weight measurement (91.5%), and blood glucose level monitoring (71.1%).
A total of 41.5% of respondents had underlying comorbidities and 34.3% had been diagnosed with a comorbidity for ≥ 12 months. Meanwhile, 25.1% of the respondents had been diagnosed by a medical practitioner and 17.7% had 3 − 6 treatment visits per year. The mean of NHP knowledge score was 32.34 (SD 7.37), where the lowest and highest scores were 10 and 50, respectively. The mean of health-promoting lifestyle score was 109.67 (SD 25.01), where the lowest and highest scores were 52 and 187, respectively. The highest and lowest mean of health-promoting lifestyle scale scores are for spiritual growth [20.36 (SD 4.68)] and physical activity [14.79 (SD 5.63)], respectively (Table 3).
The simple linear regression analysis demonstrated that the significant factors are (i) age, (ii) ethnicity (others), (iii) marital status (married, widowed/divorced), (iv) education status (primary, higher education, unclassified), (v) occupation (self-employed, private employment, homemaker, government employment), (vi) annual health monitoring activity (blood pressure monitoring, weight measurement, blood glucose level monitoring), (vii) presence of comorbidity, (viii) duration of comorbidity (≥ 12 months), (ix) diagnosis personnel (self-diagnosed, a combination of self-diagnosis with a medical practitioner, and x) treatment visit frequency (3 − 6 times per year) (Table 4).
Meanwhile, the multiple linear regression analysis demonstrated that five factors are significantly associated with health-promoting lifestyle, namely (i) ethnicity (others), (ii) education status (unclassified), (iii) occupational status (self-employed), health monitoring activity which includes annual blood glucose level monitoring, and v) NHP knowledge. The respondents who are of “others” ethnicity obtained the mean scores of health-promoting lifestyle that were higher by 28.00 (95% confidence interval [CI] 10.81, 45.21, p = < 0.001). Respondents with “unclassified” educational status had the mean scores of health-promoting lifestyle that were lower by 12.20 (95% CI -18.67, -5.73, p = < 0.001). For health monitoring activity, respondents who underwent annual blood glucose level monitoring had the mean scores of health-promoting lifestyle that were lower by 15.01 (95% CI -19.10, -10.93, p < 0.001). Further analysis demonstrated the presence of interaction between the occupational status of self-employed and NHP knowledge score (Table 5).
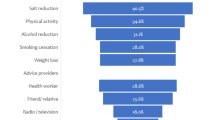
Figure 1 depicts the significant interaction between occupational status and NHP knowledge. The unemployed respondents who had the NHP knowledge score that was higher by 1 also had the mean scores of health-promoting lifestyle that were higher by 1.20 (95% CI -1.28, -0.28, p < 0.001). The self-employed respondents who had the NHP knowledge score that was higher by 1 also had the mean scores of health-promoting lifestyle that were higher by 0.53 (95% CI 0.07, 1.00, p = 0.026). This model contains five significant factors that explained 42.1% of the variation of the mean scores of health-promoting lifestyle in the study sample (R² = 0.421).
Discussion
Development of NHP knowledge questionnaire
The usage of NHP is ubiquitous and expanding worldwide. The major concern is the NHP knowledge in relation to the user’s health-promoting lifestyle [26, 46, 47]. In general, NHP knowledge is measured with various questionnaires in multiple languages [23, 24, 48]. However, the validated Malay versions of such questionnaires are limited. Certain questionnaires are developed for specific populations [49] or diseases [50] but less for the healthy community setting. To date, few studies specifically assessed the association between NHP knowledge and the health-promoting lifestyle in low-income populations.
The Malay-version NHP knowledge questionnaire developed in this study is deemed valid and reliable. The questionnaire contains 10 items in the domains of safe use and point of reference. These two domains are valuable as NHP usage is significant among low-income communities as an alternative approach to NCD treatment [51]. All 10 items have good loading factors > 0.40, which are deemd acceptable [40]. The overall questionnaire and safe use domain recorded good Cronbach α values. Cronbach’s α of the point of reference domain has fulfilled the 0.50 value (acceptable) in this study [39, 40]. Nevertheless, this may be deemed low in some studies due to the lower number of items in this domain [52, 53]. Despite the point of reference domain containing only two items, previous reports stated that there is no definitive rule on the number of items [54]. The low number of items could benefit the respondents in terms of the time required to complete the questionnaire [54], which is supported by another study that used a questionnaire with a 2-item domain [55].
Health-promoting lifestyle level and the associated factors
Health-promoting lifestyle studies have been conducted among various populations, such as low-income adults [18], adolescents [56], men [8], and undergraduates [17, 32, 57,58,59]. In Malaysia, health-promoting lifestyle studies that used the HPLP II mostly involve medical and nursing undergraduates [17, 57, 59]. The present study recorded a relatively lower mean score of health-promoting lifestyle as compared to the previous studies [11, 18, 58], where the difference could be attributed to different study populations.
This study demonstrated that the spiritual growth recorded the highest score among the six health-promoting lifestyle scales. Spiritual growth refers to “the ability to develop one’s inner self to the fullest potential” and is not confined to religious practices [60]. Instead, spiritual growth measures the personal capabilities to attain personal peace [18]. Other studies reported similar findings to ours [11, 18, 61]. However, this study recorded a lower spiritual growth score compared those studies [11, 18, 61]. This difference is attributed to the study population, cultural, and regional differences.
In this study, three scales recorded low scores, which are (i) physical activity (any regular body movement, which includes recreational activities and exercise [62]), (ii) health responsibility (the individual’s wellbeing and ability to seek treatment when needed [11, 18]), and (iii) stress management (the individual’s ability to handle stress [11, 18]). In this study, the physical activity recorded the lowest score, which resemble other studies [11, 18, 61]. The barriers to physical activity are because of limitation of resources, social influence, willpower, skill [63], and time [64]. Density is the main issue in the low-cost residential areas, and inadequate exercise infrastructure is the main factor that prevents the respondents from performing regular physical activity. Furthermore, leisure time among the low-income community are limited because their time tends to be occupied by extra work to ensure financial survival [64].
Health responsibility focuses on actions related to the individual’s health, of being educated about health, and seeking professional assistance when indicated [62]. Among low-income communities, limited healthcare accessibility [65], low-risk perception regarding health problems [65], and financial burden from out-of-pocket payment for medical treatment contribute to low health responsibility [66, 67]. Stress management incorporates an individual’s sleep and stress-handling mechanism about health [62]. Low-income communities face higher stress level in terms of finances, unmet social needs, and asset quality [67, 68]. Other studies reported that low-stress management among low-income communities is due to low family income and low education status [69, 70]. Therefore, public health intervention programmes need to focus on these three aspects to improve the health-promoting lifestyle among low-income communities.
The sociodemographic factors indicate a significant association between ethnicity and education status with health-promoting lifestyle. There is limited information from pthe revious studies to enable further discussion on the association between ethnicity and health-promoting lifestyle. In this study, the “others” ethnic group contributed to the significant association between ethnicity and the health-promoting lifestyle. In Malaysia, the major ethnicities are Malay, Chinese, and Indian [71], whereas other non-major ethnicities such as Kadazan, Bidayuh, and Iban are categorised as “others”. Thus, further studies are needed to clarify this association.
This study highlighted that “unclassified” education is significantly associated with a lower health-promoting lifestyle level. Unclassified education refers to a structured traditional education programme that focuses on spiritual growth. This could be due to education status that demonstrates a significant but weak correlation with health-promoting lifestyle [18]. It is also postulated that unclassified education does not have a structured syllabus on some of the health-promoting lifestyle scales such as physical activity and health responsibility. In the formal primary and secondary school syllabuses, the compulsory subjects of physical and moral education cover the health, spiritual, and stress components [72, 73]. This explains the association between the unclassified education scale and the lower health-promoting lifestyle level recorded in this study.
Of the three annual health monitoring activities, only blood glucose level monitoring is significantly associated with the health-promoting lifestyle. Respondents who underwent blood glucose level monitoring have a lower health-promoting lifestyle level. Initially, we postulated that there could be an interaction between the frequency of blood glucose monitoring and the status of comorbidities leading to this finding [74]. Individuals who were recently diagnosed with diabetes mellitus tend to have more frequent clinic follow-up and blood glucose monitoring [75]. For example, among diabetic patients, the recommended blood glucose level monitoring frequency is based on the disease severity and medication types, whereas a diabetic patient on insulin therapy requires more frequent blood glucose level monitoring [76]. Nevertheless, this study does not reflect any significant interaction between these factors towards health-promoting lifestyle.
This finding needs to be explored further because monitoring the frequency was only measured on an annual basis. The financial burden from out-of-pocket medical monitoring leads to the limitation of blood glucose self-monitoring among low-income communities despite such monitoring does not requires a medical doctor’s prescription [66, 67]. Apart from blood glucose monitoring frequency, an assessment demonstrated a significant effect of the association between blood glucose level, rather than annual monitoring activity and the health-promoting lifestyle [77].
Our study recorded an increase in the health-promoting lifestyle level with increased NHP knowledge score among unemployed and self-employed respondents. Other studies reported that the leisure time of unemployed respondents in low-income communities enable them the opportunity to improve their NHP knowledge, which results in higher health-promoting lifestyle levels [36, 78]. Furthermore, our findings suggested that the unemployed respondents have higher health-promoting lifestyle level than the self-employed respondents. This was supported by another study that found self-employed participants has to encounter higher job demand and stress compared to unemployed participants [79].
The strengths of this study are the development of the new Malay-version NHP knowledge questionnaire and its application to the health-promoting lifestyle among the low-income community. However, usage of the Malay-version HPLP II questionnaire in vulnerable communities in a local setting is limited. The study findings could be generalised to the low-income residents of Cheras flats, but not to all low-income residential communities in Kuala Lumpur. The limitation of this study is the cross-sectional design that is unable to establish the cause-effect relationship. Future studies could be conducted to validate the NHP knowledge questionnaire in the general population. Furthermore, future studies that explore the association between ethnicity and the health-promoting lifestyle would aid in understanding this issue. Lastly, future research could focus on the effect of blood glucose levels on the health-promoting lifestyle rather than only blood glucose monitoring frequency.
Conclusion
A new Malay-version questionnaire has been developed to measure NHP knowledge. Compared to other subpopulations, the low-income urban community in Cheras has a low health-promoting lifestyle level, which is associated with ethnicity, education status, and health monitoring activities. The findings of this study provide new insight into the interaction between NHP knowledge and occupational status, which is associated with a higher health-promoting lifestyle level. Therefore, future health-promoting lifestyle intervention programmes in healthcare delivery among the low-income urban community should target these factors.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Junaidi J. The impact of the COVID-19 pandemic on socio-economic conditions for households in Jambi city, Indonesia. Silpakorn university journal of social sciences, humanities, and arts. 2022;22(2).
Geyer S. Social inequalities in the occurrence of chronic diseases. Fed Health Gaz. 2016;59:181–7.
Arun R, Stanly AM. A review of risk factors for non-communicable diseases among Bus drivers. Natl J Community Med. 2022;13(06):404–10.
Tumas N, Rodríguez López S, Bilal U, Ortigoza AF, Diez Roux AV. Urban social determinants of non-communicable diseases risk factors in Argentina. (1873–2054 (Electronic)).
Goetzel RZ. Ten Modifiable Health risk factors and employees’ medical costs. Sage Journals. 2020;34(5).
Tavakkoli Oskuei M, Barzanjeh Atri S, Davoodi A, Van Son C, Asghari-Jafarabadi M, Hosseinzadeh M. Evaluation of a self-care education program for older adults in Iran using a lifestyle improvement model. Int J Older People Nurs. 2022;17(1):e12419.
Carole Edelman ECK. Health Promotion Throughout The Lifespan. tenth ed. Missouri2002.
Hildt-Ciupińska K, Pawłowska-Cyprysiak K. Positive Health Behaviors and their determinants among men active on the Labor Market in Poland. Am J Men’s Health. 2020;14(1).
Mirghafourvand M, Baheiraei A, Nedjat S, Mohammadi E, Charandabi SM-A, Majdzadeh R. A population-based study of health-promoting behaviors and their predictors in Iranian women of reproductive age. Health Promot Int. 2014;30(3):586–94.
Sonmezer H, Cetinkaya F, Nacar M. Healthy life-style promoting behaviour in Turkish women aged 18–64. Asian Pac J Cancer Prev. 2012;13(4):1241–5.
Alzahrani SH, Malik AA, Bashawri J, Shaheen SA, Shaheen MM, Alsaib AA, et al. Health-promoting lifestyle profile and associated factors among medical students in a Saudi university. SAGE Open Med. 2019;7:2050312119838426.
Bayati R. The Health-promoting Lifestyle Assessment among nursing students in East Kalimantan. Jurnal Ilmu Kesehatan Masyarakat. 2022;13:163–79.
Chen L, Gong Y, Yuan L. Health behaviour and its determinants in elderly patients with chronic diseases: evidence from Jiangsu Province, China. BMC Geriatr. 2022;22(1):297.
Enríquez-Reyna MC, Peche Alejandro P, Ibarra González ÁD, Gómez Infante EA. Villarreal Salazar AdC, Medina Rodríguez RE. Propiedades psicométricas de la versión en español del instrumento health-promoting Lifestyle Profile-II en universitarios mexicanos. Enfermería Global. 2022;21(2).
Rathnayake N, Alwis G, Lenora J, Lekamwasam S. Impact of Health-Promoting Lifestyle Education Intervention on Health-Promoting Behaviors and Health Status of Postmenopausal women: a quasi-experimental study from Sri Lanka. Biomed Res Int. 2019;2019:4060426.
Yusefi AR, Barfar E, Daneshi S, Bayati M, Mehralian G, Bastani P. Health literacy and health promoting behaviors among inpatient women during COVID-19 pandemic. BMC Womens Health. 2022;22(1):77.
Kuan G, Kueh YC, Abdullah N, Tai ELM. Psychometric properties of the health-promoting lifestyle profile II: cross-cultural validation of the malay language version. BMC Public Health. 2019;19(1):751.
Maglione JL. Health-promoting behaviors of low-income adults in a Community Health Center. J Community Health Nurs. 2021;38(2):61–72.
Goodyear VA, Kerner C, Quennerstedt M. Young people’s uses of wearable healthy lifestyle technologies; surveillance, self-surveillance and resistance. Sport Educ Soc. 2017;24(3):212–25.
Rippe JM. Lifestyle Medicine: the health promoting power of Daily habits and practices. Am J Lifestyle Med. 2018;12(6):499–512.
Vatanparast H, AJL, Whiting SJ. Socio-economic status and vitamin or mineral supplement use in Canada. Canadianpeer-reviewed J Popul Health Health Serv Res. 2010;21(4):19–26.
Health Canada. Natural health products: Government of Canada. 2023 [ https://www.canada.ca/en/health-canada/services/drugs-health-products/natural-non-prescription.html
Abdelmola AO, Bahri A, Abuallut I, Refaei BA, Hakami WK, Abutaleb AK, et al. Prevalence, knowledge, and perception about the use of herbal medicines jazan - Saudi Arabia. J Family Med Prim Care. 2021;10(6):2386–93.
Catublas HAL. Knowledge, attitudes and practices in the use of herbal medicine. Mahidol Univ J Pharm Sci. 2016;43(1):1–16.
Islahudin F, Shahdan IA, Mohamad-Samuri S. Association between belief and attitude toward preference of complementary alternative medicine use. Patient Prefer Adherence. 2017;11:913–8.
Sanchez-Ortuno MM, Belanger L, Ivers H, LeBlanc M, Morin CM. The use of natural products for sleep: a common practice? Sleep Med. 2009;10(9):982–7.
Ravindran AV, Lam RW, Filteau MJ, Lesperance F, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and anxiety treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. V. complementary and alternative medicine treatments. J Affect Disord. 2009;117(Suppl 1):S54–64.
Department of Statistics Malaysia. Household Income and Basic amenities Survey Report 2019. Malaysia: Department of Statistics; 2020.
Mayan SNA, Challenges to the household income, class b40 increase in developed country towards 2020 case study:Penang. Int J Environ Soc Space. 2017;5(2):35–41.
Wahab SNA, Urban, poor: evidence of barriers in accessing public clinics in Kuala Lumpur. Malaysia Malaysian J Public Health Med. 2022;22(1):193–204.
NHMS. Non-communicable diseases, Healthcare Demand and Health Literacy. MOH; 2019.
Bhuiyan M, Wong KS, Ghazali FH, Ali FG, Arnous MK, Maziz MNH, et al. Health-promoting Lifestyle habits among Preclinical Medical Students. Pakistan J Med Health Sci. 2017;11:490–5.
Murad W, Hasan M, Islam S, Alam MM. Socio-Economic Profile of the Low Income and Poor communities in Kuala Lumpur City, Malaysia. Int J Ethics Social Sci. 2019;2(1).
DBKL, Senarai, PPR dan PA di Bawah Seliaan DBKL Secara Sewa dan Jual Kuala Lumpur: DBKL. ; 2021 [ https://www.data.gov.my/data/ms_MY/dataset/ppr-pa-sewa-jual
DOSM, MyParlimen. 2022 [ https://www.mycensus.gov.my/index.php/census-product/publication/census-2020/myparlimen
Tengku Mohamad TAS, Islahudin F, Jasamai M, Jamal JA. Preference, perception and predictors of Herbal Medicine use among malay women in Malaysia. Patient Prefer Adherence. 2019;13:1829–37.
Perneger TV, Courvoisier DS, Hudelson PM, Gayet-Ageron A. Sample size for pre-tests of questionnaires. Qual Life Res. 2015;24(1):147–51.
Kaiser HF. An index of factorial simplicity. Psychometrika. 1974;39(1).
Gliem JA, Gliem RR. Calculating, Interpreting, and Reporting. 2003.
Taber KS. The use of Cronbach’s alpha when developing and reporting research instruments in science education. Reasearch Sci Educ. 2018;48:1273–96.
Dhand N, Khatkar M, Statulator. An online statistical calculator. Sample Size Calculator for Estimating a Single Proportion; 2014.
Kline P. An easy guide to factor analysis. Routledge; 2014.
Katz MH. Multivariable analysis: a primer for readers of medical research. Ann Intern Med. 2003;138(8):644–50.
Li X, Li B, Wang G, Zhan X, Holyoak M. Deeply digging the interaction effect in multiple linear regressions using a fractional-power interaction term. MethodsX. 2020;7:101067.
Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17.
Wiwanitkit V. Herbal medicines: knowledge, perception, and usage. Med J Dr DY Patil Univ. 2017;10(3).
Awad A, Al-Shaye D. Public awareness, patterns of use and attitudes toward natural health products in Kuwait:a cross-sectional survey. BMC Complement Altern Med Volume. 2014;14(105):1–11.
Danesh K, DS, Karimzade I, Mohagheghzadeh A. Knowledge, attitude, and practice (KAP) of pharmacists about Natural products used for Urolithiasis in Shiraz, Iran. Res J Pharmacognosy. 2023;10(1):5–14.
Muhammed Taher MI, Ibrahim RH. Knowledge, attitudes, and practice of university’s employees about complementary and alternative medicine (CAM). Inf Med Unlocked. 2023;37.
Gutierrez E, Silbert-Flagg J, Vohra S. Natural health product use and management in pediatrics: an integrative review. Eur J Integr Med. 2014;6(2):226–33.
Palileo-Villanueva LM, Palafox B, Amit AML, Pepito VCF, Ab-Majid F, Ariffin F, et al. Prevalence, determinants and outcomes of traditional, complementary and alternative medicine use for hypertension among low-income households in Malaysia and the Philippines. BMC Complement Med Ther. 2022;22(1):252.
Tavakol M, Dennick R. Making sense of Cronbach’s alpha. Int J Med Educ. 2011;2:53–5.
University BC. Advice on exploratory factor analysis. 2017:1–7.
Eisinga R, Grotenhuis M, Pelzer B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? Int J Public Health. 2013;58(4):637–42.
Cuijpers P, Smits N, Donker T, ten Have M, de Graaf R. Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Res. 2009;168(3):250–5.
Rahman ZA. View of Translation, Validity, and Reliability of the Malay Version of the Adolescent Healthy Lifestyle Questionnaire. 2023;31:132 – 51.
Lim BC, Kueh YC, Arifin WN, Ng KH. Validation of health promoting lifestyle profile-II: a confirmatory study with a Malaysian undergraduate students sample. Educ Med J. 2016;8(2).
Nacar M, Baykan Z, Cetinkaya F, Arslantas D, Ozer A, Coskun O, et al. Health promoting lifestyle behaviour in medical students: a multicentre study from Turkey. Asian Pac J Cancer Prev. 2014;15(20):8969–74.
Soh KG. Physical activity and health promoting lifestyle among diploma nursing students in Malaysia. Res J Pharm Technology_. 2018;11:1–12.
Murdaugh CL, Parsons M, Pender NJ. Health promotion in nursing practice. 8th ed. Pearson; 2019.
Bhandari P, Kim M. Predictors of the Health-promoting behaviors of Nepalese migrant workers. J Nurs Res. 2016;24(3):232–9.
Walker SN, Sechrist KR, Pender NJ. The Health-promoting Lifestyle Profile: development and psychometric characteristics. Nurs Res. 1987;36(2):76–81.
Al Salim ZA. Barriers to physical activity participation among University students in Saudi Arabia. Inform Sci Lett. 2023;12(1):353–60.
Darroch FE, Oliffe JL, Montaner GG, Webb JM. Barriers to physical activity for father’s living in marginalising conditions. Health (London). 2023;27(1):147–66.
Lazar M, Davenport L. Barriers to Health Care Access for low income families: a review of literature. J Community Health Nurs. 2018;35(1):28–37.
Evaluation ASfPa. Financial Condition and Health Care Burdens of People in Deep Poverty2015. https://aspe.hhs.gov/reports/financial-condition-health-care-burdens-people-deep-poverty-0
Anderson NB, Belar CD, Breckler SJ, Nordal KC, Ballard DW, Bufka LF et al. Stress in America: Paying with our health. 2015:1–19.
Garg R, McQueen A, Wolff JM, Skinner KE, Kegler MC, Kreuter MW. Low housing quality, unmet social needs, stress and depression among low-income smokers. Prev Med Rep. 2022;27:101767.
Upchurch DM, Stein J, Greendale GA, Chyu L, Tseng CH, Huang MH, et al. A Longitudinal Investigation of Race, Socioeconomic Status, and Psychosocial mediators of allostatic load in midlife women: findings from the study of women’s Health across the Nation. Psychosom Med. 2015;77(4):402–12.
Rothwell DW, Han C-K. Exploring the relationship between assets and family stress among low-income families. Fam Relat. 2010;59(4):396–407.
Kamaruddin AR, Kamaruddin K. Malay culture and consumer decision-making styles-an investigation on religious and ethnic dimensions. J Kemanusiaan. 2009;14:37–50.
Balakrishnan V. The development of moral education in Malaysia. Asia Pac J Educators Educ. 2010;25:89–101.
Salamuddin N, Harun MT. Facilitating the process of learning social skills through humanistic physical education. Procedia - Social Behav Sci. 2010;9:223–7.
Urina-Jassir M, Herrera-Parra LJ, Hernández Vargas JA, Valbuena-García AM, Acuña-Merchán L, Urina-Triana M. The effect of comorbidities on glycemic control among Colombian adults with diabetes mellitus: a longitudinal approach with real-world data. BMC Endocr Disorders. 2021;21(1):128.
Mathew TK, Zubair M. P. T. Blood Glucose Monitoring: StatPearls Publishing; 2023.
Renard E. Monitoring glycemic control: the importance of self-monitoring of blood glucose. Am J Med. 2005;118(Suppl 9A):S12–9.
Yoshimura E, Hamada Y, Hatanaka M, Nanri H, Nakagata T, Matsumoto N, et al. Relationship between intra-individual variability in nutrition-related lifestyle behaviors and blood glucose outcomes under free-living conditions in adults without type 2 diabetes. Diabetes Res Clin Pract. 2023;196:110231.
Ahmed M, Hwang JH, Hasan MA, Han D. Herbal medicine use by pregnant women in Bangladesh: a cross-sectional study. BMC Complement Altern Med. 2018;18(1):333.
Nikolova M. Switching to self-employment can be good for your health. J Bus Ventur. 2019;34(4):664–91.
Acknowledgements
This programme was supported by the SULAM@UKM 2021 Project (CH-H-FFF 1001-00-1002003). The authors thank the Secretariat of SULAM@UKM 2021, Doctor of Public Health Programme students (Cohort XIII), Department of Public Health Medicine, Faculty of Medicine, UKM, and UKM staff for their commitment. The authors are also grateful to the Flat Sri Kota Joint Management Board and Kuala Lumpur City Hall for their support, and the respondents who participated in this study. Lastly, the authors thank the Cheras District Health Office staff and the Malaysian Civil Defence Force team for their contributions to this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
N.A., I.B.I., A.N.A., R.I. and W.M.D. conceptualized, visualized and supervised the research. N.A., W.M.D. and S.M.S.S. done the formal analyses. N.A., W.M.D., I.H.K., M.R.A.R, S.W. and Q.M.G. done the methodology and investigation of the research. W.M.D. and S.M.S.S. wrote the original draft of the manuscript. N.A., W.M.D. and A.N.A. reviewed and edited the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All the study methods were carried out based on the guidelines and regulations under the UKM Medical Research Ethics Committee approval (FF-2021-497) on 16th December 2021. The consent for participation and publication was obtained from the respondents through the consent form that was distributed prior to the questionnaire.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Syed Shamsuddin, S.M., Ahmad, N., Idris, I.B. et al. Natural health product knowledge as a significant factor associated with health-promoting lifestyle in a low-income urban community in Kuala Lumpur. BMC Public Health 24, 2146 (2024). https://doi.org/10.1186/s12889-024-19601-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19601-8