Abstract
Background
Effective education is considered by the American Heart Association (AHA) as a vital variable in improving outcomes of cardiac arrest. Studies have shown that the level of knowledge and attitude of non-healthcare providers towards resuscitation training varies widely across the globe. While some training methods and barriers to training have been discussed, the literature is still quite vague and unclear regarding resuscitation training, particularly in the Middle East. This study’s focus on the efficacy of resuscitation training in this region of the world may help dictate how to better implement education initiatives aimed towards non-healthcare providers in developing countries.
Methodology
A systematic review and meta-analysis were conducted on studies published from inception until March 2023. Observational studies assessing CPR knowledge and skills among non-healthcare workers in Arab countries were included. Data were extracted from PubMed, Cochrane Library, EMBASE, Web of Science, and Scopus. Data analysis was performed using Rstudio with a random effects model.
Results
50 studies were included in this review and meta-analysis, revealing that 55% of participants had prior knowledge of CPR, while only 28% considered their knowledge sufficient. The majority (76%) supported mandatory CPR training, and 86% were willing to attend training if offered. This study found that prior knowledge of cardiopulmonary resuscitation (CPR) varied among populations. This meta-analysis also compiled results regarding CPR technique defined by correct compression to ventilation ratio, compression depth, compression rate, location of chest compression, and correct sequence. The overall results from this meta-analysis showed that, of these factors, compression rate and depth were the two factors that were most often administered incorrectly. In all, the results from this study demonstrated that CPR training in Arab countries was favorably viewed overall, with the majority of participants indicating both support for mandatory CPR training and general willingness to attend training if offered the opportunity.
Conclusion
Given the overall positive view and willingness to learn CPR skills, healthcare policy makers should adopt a more comprehensive focus on strategies that enhance the accessibility and opportunity for CPR training for non-healthcare populations in Arab countries. Future training programs should implement strategies to highlight the ideal combination of compression rates and depth to learners to ensure correct and efficacious delivery of CPR with increased focus on the practical portion during refresher courses to promote retention.
Similar content being viewed by others
Background
Worldwide, cardiovascular diseases are the number one cause of death, causing 32% of all global deaths according to the World Health Organization (WHO) [1]. Sequalae of cardiovascular diseases, such as respiratory failure and circulatory shock, are reversible, yet cause millions of deaths globally. There is a disproportionate number of such deaths in developing countries [2]. In fact, the American Heart Association (AHA) has noted that the administration of cardiopulmonary resuscitation (CPR) and defibrillation within the first three to five minutes of collapse can yield survival rates ranging from 49% to as high as 75% [3, 4]. Not only that, CPR has also been shown to double or triple survival from the time of witnessed sudden cardiac arrest [4]. Implementation of effective resuscitation training is critical to improving survival rates and outcomes.
Effective education is considered by the AHA as a vital variable in improving outcomes of cardiac arrest [5]. Resuscitation training programs aim to provide evidence-based knowledge and skills to reduce the morbidity and mortality of reversible life-threatening conditions. Such training is necessary to allow for lay persons and healthcare providers alike to consistently apply this evidence-based approach [5]. It has been reported that resuscitation teams one or more members trained in advanced cardiovascular life support (ACLS) have better outcomes [5].
Although morbidity and mortality related to cardiovascular diseases have been decreasing, the prognosis of out-of-hospital cardiac arrest (OHCA) remains the same [6]. OHCA is defined as the cessation of cardiac mechanical activity that takes place outside hopitals. Importantly, OHCA is considered a potentially reversible event through the activation of chain of early CPR and proper care. The survival rate of OHCA could be two to three times higher if bystander CPR is performed in a timely manner. While healthcare professionals are expectedly aware of of CPR, adequate awareness of CPR among the general population is still lacking as many studies have reported poor knowledge among laypersons [7].
In Arab countries, first aid education and CPR training are often provided through schools, community centers, and healthcare institutions. However, the extent and quality of this training can vary widely. For example, in countries like Lebanon and the UAE, CPR training is integrated into school curricula, whereas in others, it is offered sporadically through community initiatives [8, 9].
The rationale for this systemic review originates from the paucity of literature covering this specific topic. As discussed previously, cardiovascular diseases are a leading cause of death worldwide and its sequelae, such as respiratory failure and circulatory shock, can be reversible. The burden on the healthcare system increases dramatically due to increased morbidity and mortality that could have been mitigated with evidence-based application of resuscitation measures. While the awareness and knowledge of CPR among healthcare providers are a popular concern worldwide, awareness of CPR among the general public represents an equally crucial objective in order to enhance the prognosis of OHCA. The aim of this study is to systematically review and analyze the level of CPR knowledge and skills among non-healthcare providers in Arab countries, identifying key areas for improvement and providing recommendations for future training programs.
Methods
We followed the PRISMA statement guidelines when conducting this systematic review and meta-analysis [8]. All steps were done per the Cochrane Handbook of Systematic Reviews and Meta-analysis of Interventions [9]. Based on the PRISMA guidelines, investigators (MA and MSA) created the review protocol and the search strategy. Our research question was developed following the key elements of the PICO framework: Participants, Interventions, Comparison, and Outcomes [10, 11]. The protocol (CRD42023399328) was registered in PROSPERO (International Prospective Register of Systematic Reviews) 2023.
Inclusion and selection criteria
Using predefined keywords, databases were searched from inception through August 2023 for studies that assessed the knowledge, attitude, and perceptions (KAP) towards Basic Life Support (BLS) among non-healthcare workers in Arab/Middle Eastern countries. In the case of studies which included both healthcare and non-healthcare workers, we included the study only when there were separable data for the non-healthcare workers eligible per our criteria; otherwise, we excluded the studies. In this meta-analysis, we included observational studies such as cross-sectional studies that assessed CPR knowledge and skills. For specific outcomes like previous knowledge, only cross-sectional studies were used to ensure consistency in the analysis. Reviews, abstracts, editorials, conference papers, and non-English studies were excluded. We removed the duplicates using Endnote 8 software. Then, we screened the titles and abstracts, followed by full-text screening to identify the relevant studies.
Information sources and search strategy
To identify studies to be included in this review, the databases PubMed, Cochrane Library, EMBASE, Web of Science, and Scopus were searched for keywords related to CPR, knowledge, skill, Middle East, Arab, Arabian Gulf (see Table 1. in appendix) from inception until August 2023. Additionally, we manually searched the references of the included studies, Google Scholar, and Research Gate for additional articles of interest.
Study selection
Following the database searches, all of the citations were imported into EndNote X9 Windows version. Duplicate references resulting from the overlap of database content were identified and removed. Two independent reviewers (MSZ and AAE) screened the titles and abstracts of all unique citations against the predefined inclusion and exclusion criteria. Any disagreements between the two reviewers at this stage were resolved through discussion; if necessary, a third reviewer (MA) was consulted. Studies that appeared to meet the inclusion criteria, or for which there was insufficient information in the title and abstract to make a clear decision, were advanced to full-text review. Again, two independent reviewers (MSZ and AAE) assessed each full-text article to determine its eligibility. Disagreements at this stage were resolved through consultation with a third reviewer (MA). The reference lists of all included studies were scanned to identify additional studies that might have been missed during the initial database searches. Any potentially relevant studies identified through this process were subjected to a full-text review and included if they met the criteria.
Data extraction and synthesis
The data analysis in this study was performed using Rstudio (Version 4.2.2). We performed subgroup analysis according to the study group (e.g., university students, parents, etc.). To calculate the pooled proportion along with its corresponding 95% confidence interval (CI) for all the analyzed outcomes, a random effects model was employed. This statistical approach was implemented using the “meta prop” function, which is a part of the “meta” library available within the Rstudio environment. We assessed the prevalence of the different indices of CPR knowledge among all studies with higher prevalence (percentage %) indicating higher number of participants being aware or proficient in each index. The assessment of heterogeneity among the included studies was a crucial aspect of this analysis. To quantify heterogeneity, the I^2 statistic was computed, and its associated p-value was determined. A p-value < 0.1 indicated statistically significant heterogeneity. The meta-analytical method utilized in this study involved the application of a random intercept logistic regression model, employing maximum-likelihood estimation to determine tau^2. To establish random effects confidence intervals, the t-distribution was utilized, and a logit transformation was applied to the data.
Quality assessment
We employed an adapted version of the Newcastle–Ottawa quality assessment scale (NOS) for cross-sectional studies. The scale has three main domains with seven items for quality assessment. We included the detailed guidelines for NOS risk of bias assessment in our supplementary material. While the maximum points a study can score is up to 9 points, studies were deemed to be of good quality if they scored 5 points or more [12].
To assess the quality of experimental and quasi-experimental studies, we used the AHA guideline’s definitions for the level of evidence and class of recommendation of the CPR training. The following are the definitions: ‘LOE A’ represents high-quality evidence based on two or more randomized controlled trials (RCTs); ‘LOE B’ is intermediate level of evidence based on one RCT or more; ‘LOE B-NR’ level is based on strong observational or nonrandomized studies; ‘LOE C-LD’ has evidence from weak or limited observational studies; ‘LOE C-EO’ is the weakest level of evidence which is based only on experts’ opinion [13].
In terms of class of recommendation (COR) in CPR training, the strength of training is stratified as follows:
-
1.
When benefit is three-fold the risks of intervention A compared to intervention B, the training is considered “class I (strong).”
-
2.
When benefit is two-fold the risks of intervention A compared to intervention B, the training is considered “class IIa (moderate).”
-
3.
When benefit is thought to be equal or more than the risks of intervention A compared to intervention B, the training is considered “class IIb (weak).”
-
4.
When benefit of intervention A equals intervention B, the training is considered “class III (no benefit/moderate).”
-
5.
When intervention A has risks higher than those of intervention B the training is considered “class III (harm/strong).” [14].
Results
Literature search
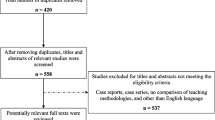
The initial search identified a total of 4573 records from five different databases. Following the removal of duplicates, 3705 records remained. Through the title and abstract screening, we excluded 3512 records. Moreover, following the full-text screening, there were 40 included studies. Additionally, we included 10 through manual screening (Fig. 1),
Characteristics of the included studies and population
50 studies [15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64] were included in the meta-analysis. A summary of the characteristics of the included studies is provided in Table 1. Regarding the populations of included studies, 14 studies enrolled health colleges students, 12 studies enrolled university students, 5 studies enrolled teachers, 5 studies enrolled secondary school students and 14 studies enrolled patricipants of the general population. Our quantitative analysis included a total number of 30,308 participants. Subgroup analyses were performed on several groups of participants: health colleges students (n = 7,420), university students (n = 9,802), school students (n = 3,256), teaching staff (n = 1,389), and the general population (n = 8,441).
Previous knowledge
In the meta-analysis of 13 studies [19,20,21,22, 26, 29, 31, 37, 38, 43, 45, 57, 58] on “Previous Knowledge” (9,343 observations, 5,226 events), 55% of participants were found to have previous knowledge regarding CPR (95% CI: 43% to 66%). Heterogeneity analysis showed substantial variability among the included studies, with an I^2 value of 98.7% (p < 0.01). Subgroup analysis demonstrated significant differences in previous knowledge among various groups of participants: secondary school students (47%, 95% CI: 33% to 61%), the general population (61%, 95% CI: 51% to 71%), health college students (59%, 95% CI: 30% to 83%), and teachers (11%, 95% CI: 9% to 13%). (Fig. 2 A). The meta-analysis revealed significant variations in CPR knowledge and skills. The prevalence of prior knowledge was 55%, while the correct compression rate was only 26%. Figures 2 and 3 illustrate the distribution of knowledge and skills, respectively.”
Consider their knowledge sufficient
The meta-analysis of 9 studies [18, 19, 22, 25, 31, 33, 40, 52, 60] (7,188 observations, 1,608 events) revealed that 28% of paricipants consider their knowledge sufficient (95% CI: 14% to 48%). Heterogeneity was substantial with an I^2 of 99.1% (p < 0.01). Subgroup analysis indicated differences among groups of participants regarding whether they consider their knowledge sufficient, including teachers (35%, 95% CI: 30% to 41%), secondary school students (13%, 95% CI: 1% to 62%), health college students (48%, 95% CI: 41% to 54%), university students (19%, 95% CI: 9% to 35%), and the general population (84%, 95% CI: 81% to 88%).(Fig. 2 B).
CPR training should be mandatory
The meta-analysis of 14 studies [18,19,20, 25, 26, 28, 30, 31, 39, 40, 50, 59,60,61] (11,974 observations, 7,937 events) revealed that 76% of participants think that CPR training should be mandatory (95% CI: 62% to 86%). Heterogeneity was substantial with an I^2 of 99.3% (p < 0.01). Subgroup analysis revealed variations in responses among different groups of participants, including teachers (70%, 95% CI: 39% to 90%), secondary school students (38%, 95% CI: 25% to 54%), the general population (89%, 95% CI: 67% to 97%), university students (66%, 95% CI: 15% to 95%), and health college students (88%, 95% CI: 41% to 99%).(Fig. 2 C).
Encountered a case that needed CPR
The meta-analysis of 14 studies [19, 26, 29, 31,32,33, 38, 40, 42, 52, 53, 57, 60, 64] (11,685 observations, 2,068 events) estimated that 18% of participants encountered a case that needed CPR (95% CI: 14% to 22%). Heterogeneity was substantial with an I^2 of 96.4% (p < 0.01). Subgroup analysis showed varying results concerning this question among different groups of participants, including secondary school students (14%, 95% CI: 0.5% to 84.7%), teachers (19%, 95% CI: 14.7% to 24.9%), the general population (18%, 95% CI: 10.7% to 28.7%), university students (17%, 95% CI: 9.8% to 29.1%), and health college students (26%, 95% CI: 23.8% to 28.7%).(Fig. 2 D).
Willingness to attend CPR training if offered
The meta-analysis of 13 studies [17, 18, 20, 24, 25, 28, 30, 38, 45, 50, 52, 61] (7,622 observations, 6,396 events) estimated that 86% of participants ar willing to attend CPR training if offered (95% CI: 81% to 90%). Heterogeneity was present with an I^2 of 95.0% (p < 0.01). Subgroup analysis showed variations in responses to this question among different groups of participants, including teachers (85%, 95% CI: 49% to 97%), the general population (88%, 95% CI: 77% to 94%), university students (85%, 95% CI: 74% to 92%), and health college students (89%, 95% CI: 87% to 90%).( Fig. 3 A).
Activate emergency medical services (EMS) when encountering an unresponsive person
The meta-analysis of 7 studie [22, 24, 25, 28, 30, 31, 60] (3,321 observations, 1,020 events) estimated that 34% of patricipants would activate EMS when encountering an unresponsive person (95% CI: 15% to 60%). Heterogeneity was substantial with an I^2 of 99.0% (p < 0.01). Subgroup analysis revealed differences in responses among various groups of participants, including health college students (29%, 95% CI: 0% to 100%), university students (38%, 95% CI: 0% to 100%), teachers (55%, 95% CI: 49% to 60%), secondary school students (52%, 95% CI: 48% to 56%), and the general population (12%, 95% CI: 9% to 15%).( Fig. 3 B).
Awareness of EMS number
Meta-analysis across 10 studies [16, 26, 28, 30, 38, 45, 50, 58, 60, 63] revealed that 66% of participants are aware of the EMS number (95% CI: 56% to 74%). Significant heterogeneity was observed (I^2 = 97.0%, p < 0.0001). Subgroup analysis showed varying responses concerning the awareness of the EMS number among different groups of participants, with university students having the lowest awareness (48%, 95% CI: 31% to 66%), while health college students demonstrated the highest awareness (72%, 95% CI: 67% to 76%). (Fig. 3 C).
Correct CPR ratio (Compression to ventilation)
In the meta-analysis of 14 studies [23, 30,31,32,33, 39, 44, 45, 50, 53, 55, 58, 59, 63] 32% of participants were found to know the correct CPR ratio (95% CI: 22% to 43%). Substantial heterogeneity was observed (I^2 = 99.1%, p < 0.0001). Subgroup analysis indicated significant variations among different groups of participants, with university students showing the lowest correct CPR ratio (35%, 95% CI: 6% to 82%) and health college students having the highest (36%, 95% CI: 20% to 56%). ( Fig. 3 D).
Correct compression rate for adults
Meta-analysis 11 studies [23, 30, 32, 33, 39, 44, 50, 53, 55, 59, 63] revealed that 26% of participants were found to know the correct compression rate for adults (95% CI: 19% to 35%). Considerable heterogeneity was observed (I^2 = 98.3%, p < 0.0001). Subgroup analysis demonstrated variations among different groups of participants, with university students having the lowest correct compression rate (27%, 95% CI: 7% to 65%), while health college students exhibited the highest (25%, 95% CI: 14% to 40%). (Fig. 4 A).
Correct compression depth for adults
Meta-analysis across 10 studies [23, 30, 33, 39, 44, 50, 55, 58, 59, 63] 34% of participants were found to know the correct compression depth for adults (95% CI: 22% to 47%). Significant heterogeneity was observed (I^2 = 98.9%, p < 0.0001). Subgroup analysis revealed variations among different groups of participants, with university students showing the lowest correct compression depth (40%, 95% CI: 13% to 74%) and health college students having the highest (31%, 95% CI: 17% to 56%). (Fig. 4 B).
Correct location for chest compression
Meta-analysis of 13 studies [16, 23, 30, 32, 33, 39, 44, 50, 53,54,55, 59, 63] revealed that 50% of participants know the correct location for chest compression across (95% CI: 39% to 61%). Significant heterogeneity was observed (I^2 = 98.7%, p < 0.0001). Subgroup analysis indicated variations among different groups of participants, with university students having the lowest prevelance (55%, 95% CI: 31% to 76%), while health college students exhibited the highest (44%, 95% CI: 27% to 63%). (Fig. 4 C).
Knowledge of what the abbreviation of BLS stands for
Meta-analysis of 4 studies [23, 44, 50, 63] revealed that 69% of patricipants know what the abbreviation of BLS stands for (95% CI: 24% to 94%). Substantial heterogeneity was observed (I^2 = 99.5%, p < 0.0001). Subgroup analysis showed variations among different groups of participants, with university students having a prevelance of 67% (95% CI: 0% to 100%), while health college students exhibited 70% (95% CI: 0% to 100%). (Fig. 4 D).
Correct sequence for CPR
Meta-analysis of 3 studies [38, 55, 58] showed that 54% of participants know the correct sequence for CPR (95% CI: 23% to 82%). Significant heterogeneity was observed (I^2 = 96.2%, p < 0.0001). Subgroup analysis revealed variations among different groups of participants, with health college students having the highest prevelance (62%, 95% CI: 3% to 99%). (Fig. 4 E).
Quality assessment of included studies
Overall, the quality of cross-sectional questionnaire studies was good with score ranging between 5 and 8, with only two of them scoring 8 and twenty-two studies scoring 7. All studies, except for Al Harbi et al. [66], Alghamdi et al. [67], Aloraibi et al. [68], Alshehri et al. [69] and Awadallah et al. [70] scored zero in the ‘Non-Response Rate’ in the selection domain. Table 2 presents the details of the quality assessment thoroughly.
Furthermore, we stratified seven experimental and quasi-experimental studies according to the AHA level of evidence and class of recommendation classification as summarized in Table S2. Evidence level ‘LOE B-R’ was given to four studies, ‘LOE B-NR’ to two studies and ‘LOE C-LD’ to one study. Only Abbas et al. [65] Hassan et al. [71], Majid et al. [72] were considered to have moderate (class IIa) evidence, while the remainder of the studies were deemed to have weak (class IIb) evidence.
Discussion
The results from this study demonstrated that CPR training in Arab countries was favorably viewed overall with the majority of participants indicating both support for mandatory CPR training and general willingness to attending training if offered the opportunity. Public awareness is of great importance as the success rate of BLS can be ameliorated when lay persons initiate life-saving techniques before arrival of healthcare professionals. Given the overall positive view and willingness to learn CPR skills, there should be increased focus on strategies that increase accessibility and opportunity for CPR training in Arab countries. One country that has recognized the importance of this notion is Lebanon, as evidenced by the position statement published by the Lebanese Society of Cardiology and the Lebanese Society of Emergency Medicine [15]. In this statement, the launching of a campaign raising public awareness of CPR and automated external defibrillator (AED) use through videos, messages, and educational material was recommended to demonstrate the importance of early recognition of signs of cardiac arrest and factors impacting survival outcomes. This statement also discussed mandating of CPR training including the use of AEDs in high schools, in addition to training of lay people in the community. In a Slovenian study on CPR training in school children, the youngest age group (12.5 years) made the most progress in CPR knowledge, thus highlighting the value of starting training and instilling a sense of social responsibility early [16]. This is comparable to several other countries such as Japan, Austria, Hong Kong, Singapore, and Norway where CPR and AED courses are integrated into secondary school curricula [17].
As expected, prior knowledge of CPR varied among populations. This can be explained by differing stages of life and variations in work, school, and living environments that result in different levels of exposure to information about CPR. Compared to the proportion of participants who reported prior knowledge of CPR, the proportion of those who considered their knowledge sufficient was roughly half; this is consistent with multiple studies. For instance, in a study conducted at a medical school in Oman, 53.6% and 64.5% of 304 medical students had insufficient knowledge and no previous BLS training, respectively [18]. In another observational study, comprised of 121 participants including nurses, dental personnel, and house officers, it was found that the average health care worker lacked sufficient BLS and CPR knowledge [19]. This may be remedied by providing initial training and refresher programs with strategies that promote knowledge retention. Recent studies have highlighted the importance of high-quality resuscitation training. For example, Dudziński et al. [20] analyzed the quality of CPR performed by firefighters and found significant insights into compression quality under physical strain. Leszczyński et al. [21] evaluated the use of virtual environments for CPR training, demonstrating the potential of multimedia methods. Sholokhova et al. [22] examined CPR knowledge among pedagogy students, providing valuable data on the effectiveness of training programs for non-healthcare professionals. A prospective study conducted in Slovenia on schoolchildren demonstrated a more marked drop in retention of practice CPR skills compared to theoretical knowledge; they recommended putting a greater emphasis on practical training combined with a quick theoretical overview on repeat courses [23]. This can be implemented to empower individuals following initial training to be able to initiate CPR measures as a bystander.
In our review, we found that 13 included studies have organized their questionnaires in line with the American Heart Association (AHA) guidelines and one study in line with the European Resuscitation Council (ERC) guidelines. While the AHA guidelines are often referenced due to their global influence, the ERC guidelines are also significant in this region. Studies have shown that the adoption of resuscitation guidelines in the Middle East can be influenced by regional collaborations and the availability of training resources [24, 25].
Another finding in this meta-analysis was that 66% of participants over 10 studies reported knowledge of the EMS contact number, with only 34% over 7 studies activating EMS when encountering an unconscious person. One factor that may be contributing to this difference may be that participants simply had never found themselves in such a situation; for instance, in our study, only 18% of individuals over 14 studies had encountered a case requiring CPR. However, it is alarming that there is not a larger proportion of the population is aware of the EMS number. This is unfortunately consistent with other studies conducted in the area. A study in Saudi Arabia conducted on security personnel in shopping malls showed that more than half of the participants (54.1%) did know the correct EMS number in Saudi Arabia [17]. A study in Iran in non-institutionalized older adults demonstrated that 47% were not familiar with the EMS system and thus, how to implement it [26]. They cited a low public awareness and high rate of illiteracy as contributing factors. Given that recognition and subsequent activation of the emergency response system is the first step of the chain of survival, knowledge of the EMS number and how to activate the response is imperative. Future endeavors should focus on increasing public awareness of the role, availability, and contact of local EMS.
Several studies have discussed the outcomes and modifying factors of OHCA in Middle Eastern countries. Ethnicity has been evaluated by Awad et al. [27] in a Qatari population as a possible influencing factor on the prognosis of OHCA cases and they found that North African patients had lower risk factors, more favorable rhythms and better survival rates as they were more likely to receive advanced cardiac life support (ACLS) interventions. On the other hand, another study found sex-based difference in the outcomes of OHCA cases with lower incidence of OHCA in public places among female patients; moreover, female patients were less likely to receive bystander CPR compared to male patients [28]. Alqahtani et al. [29] performed a prospective observational study of OHCA cases that were treated by the ambulance services in United Arab Emirates; they reported low bystander response rate -with only half of OHCA cases being recognized- and low AED usage rate.
This meta-analysis compiled results regarding CPR technique defined by correct compression to ventilation ratio, compression depth, compression rate, location of chest compression, and correct sequence. The overall results from this meta-analysis showed that, of these factors, compression rate and depth were the two factors that were most often administered incorrectly. This is supported by a study conducted in Saudi Arabia in which participants’ most common misconceptions included the adult compression rate (90.8%) and the compression depth (84.5%) [17]. This represents an area for improvement as these two factors, when within target ranges, are correlated with recovery with good neurologic function after OHCA [30]. The AHA recommends a target compression rate of 100–120 per minute and a depth of at least 5 cm for adult patients [31]. However, it is important to note that these factors affect one another; for instance, a faster compression rate can compromise the compression depth. Furthermore, it has been postulated that the recommended depth is too high and that maximal survival is at a depth of 45.6 mm [32]. A study in 2019 sought to find an ideal combination target for these two factors and recommended a combination of 107 compressions per minute and a depth of 4.7 cm [30]. In a prospective study on school children examining retention of CPR skills, hand location was well adapted as were the depth and release of the compressions, but compression rate was noted to be most out of the desired range, too slow on average [16]. With this information in mind, future training programs should implement strategies to highlight the ideal combination of compression rates and depth to learners to ensure correct and efficacious delivery of CPR.
Limitations
This study has several limitations. Many included studies were cross-sectional and relied on self-reported data, which may introduce bias as individuals may not accurately report their own knowledge and proficiency in CPR. The exclusion of studies without separable data for non-healthcare workers might limit the comprehensiveness of our analysis. Additionally, the variations in first aid education programs across different countries may impact the generalizability of our findings. Future studies should aim to include a broader range of data sources and consider longitudinal designs to better assess the impact of CPR training over time [33, 34]. Another limitation may stem from the fact that all the studies included in this meta-analysis were conducted in Arab countries; as such, this may limit the generalizability of the results to the rest of the world, given that several cultural and demographic factors might influence the results.
Future direction
We are encourage future studies to assess the knowledge, awareness, and perception (KAP) before and after CPR training, including long-term follow-up, and to investigate possible associated factors that impact BLS KAP and CPR performance. This information will aid in identifying lapses and areas for improvement to ensure better performance – and outcomes – following CPR training. In addition to this, we are shedding a spotlight on the importance of adoption of national policies that should prioritize the quality and accessibility of BLS education, not only to healthcare providers, but to the general population.
Conclusion
As expected, prior knowledge of CPR varied between different groups of participants. This can be explained by differing stages of life and variations in work, school, and living environments that result in different levels of exposure to information about CPR. This meta-analysis also compiled results with regards to CPR technique defined by correct compression to ventilation ratio, compression depth, compression rate, location of chest compression, and correct sequence. The overall results from this meta-analysis showed that, of these factors, compression rate and depth were the two factors that were most often administered incorrectly. future training programs should implement strategies to highlight the ideal combination of compression rates and depth to learners to ensure correct and efficacious delivery of CPR with increased focus on the practical portion during refresher courses to promote retention. In all, the results from this study demonstrated that CPR training in Arab countries was favorably viewed overall with the majority of non-healthcare participants indicating both support for mandatory CPR training and general willingness to attending training if offered the opportunity. Given the overall positive view and willingness to learn CPR skills, healthcare policy makers should adopt a more comprehensive focus on strategies that enhance the accessibility and opportunity for CPR training for non-healthcare populations in Arab countries.
Availability of data and materials
The datasets generated or analyzed in this manuscript are provided either in the main text of the article or the supplementary file.
Abbreviations
- CPR:
-
Cardiopulmonary resuscitation
- AHA:
-
American Heart Association
- ACLS:
-
Advanced cardiovascular life support
- KAP:
-
Knowledge, attitude, and perceptions
- BLS:
-
Basic Life Support
- NOS:
-
Newcastle–Ottawa quality assessment scale
- CI:
-
Confidence interval
References
World Health Organization. Cardiovascular diseases (CVDs). World Health Organization; 2021. https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds).
Meaney PA, Topjian AA, Chandler HK, Botha M, Soar J, Berg RA, Nadkarni VM. Resuscitation training in developing countries: a systematic review. Resuscitation. 2010;81(11):1462–72.
American Heart Association. 2005 American Heart Association (AHA) guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care (ECC) of pediatric and neonatal patients: pediatric advanced life support. Pediatrics. 2006;117(5):e1005–28.
Alkubati SA, McClean C, Yu R, Albagawi B, Alsaqri SH, Alsabri M. Basic life support knowledge in a war-torn country: a survey of nurses in Yemen. BMC Nurs. 2022;21(1):1–7.
CPR and ECC Guidelines | American Heart Association CPR & First. [Internet]. [cited 2024 Jul. 29]. https://cpr.heart.org/en/resuscitation-science/cpr-and-ecc-guidelines.
Song J, Guo W, Lu X, Kang X, Song Y, Gong D. The effect of bystander cardiopulmonary resuscitation on the survival of out-of-hospital cardiac arrests: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med. 2018;26(1):86. https://doi.org/10.1186/s13049-018-0552-8.
Mani G, Annadurai K, Danasekaran R. Bystander cardiopulmonary resuscitation in out of hospital cardiac arrest: need of the hour. Afr Health Sci. 2015;15(1):307–9. https://doi.org/10.4314/ahs.v15i1.43.
Sharma SK, et al. First aid and CPR training in schools: a regional perspective from the Middle East. Int J Public Health. 2017;62(1):101–10.
Ibrahim M, et al. Community-based CPR training in the UAE: challenges and successes. J Community Health. 2019;44(4):700–8.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.2 [updated February 2021]. Cochrane Handbook for Systematic Reviews of Interventions. 2021.
Wells GA, Shea B, O’connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Hospital Research Institute. Clinical Epidemiology. 2014.
Bhanji F, Donoghue AJ, Wolff MS, Flores GE, Halamek LP, Berman JM, Sinz EH, Cheng A. Part 14: education: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18):S561–73. https://doi.org/10.1161/CIR.0000000000000268.
Finn JC, Bhanji F, Lockey A, Monsieurs K, Frengley R, Iwami T, Lang E, Ma MHM, Mancini ME, McNeil MA, Greif R, Billi JE, Nadkarni VM, Bigham B, Billi JE, Bray JE, Breckwoldt J, Brooks SC, Cheng A, et al. Part 8: education, implementation, and teams. 2015 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation. 2015;95:e203–24. https://doi.org/10.1016/j.resuscitation.2015.07.046.
Isma’eel H, Noureddine S, Mohammad M, Zgheib A, Abou Arbid S, Njeim M, et al. Out-of-hospital cardiopulmonary resuscitation: a position statement of the Lebanese Society of Cardiology and the Lebanese Society of Emergency Medicine. Cardiovascular diagnosis and therapy. 2019;9(6):609.
Pivač S, Gradišek P, Skela-Savič B. The impact of cardiopulmonary resuscitation (CPR) training on schoolchildren and their CPR knowledge, attitudes toward CPR, and willingness to help others and to perform CPR: mixed methods research design. BMC Public Health. 2020;20:1–11.
Al Haliq SA, Khraisat OM, Kandil MA, Al Jumaan MA, Alotaibi FM, Alsaqabi FS, et al. Assessment on CPR knowledge and AED availability in Saudi malls by security personnel: public safety perspective. J Environ Pub Health. 2020;2020:7453027.
Albadi S, Al-Hadi H, Nadar SK. Knowledge and attitudes toward basic life support among medical students in Oman. Indian Journal of Critical Care Medicine: Peer-reviewed, Official Public Indian Soc Crit Care Med. 2020;24(7):599.
Roshana S, Batajoo KH, Piryani RM, Sharma MW. Basic life support: knowledge and attitude of medical/paramedical professionals. World J Emerg Med. 2012;3(2):141.
Dudziński Ł, et al. Quality analysis of chest compression during cardiopulmonary resuscitation performed by firefighters with physical effort. Kardiol Pol. 2021;79(6):690–2. https://doi.org/10.33963/KP.15992.
Leszczyński P, et al. Evaluation of virtual environment as a form of interactive resuscitation exam. J New Rev Hypermed Multimedia. 2017;23(4):265–76. https://doi.org/10.1080/13614568.2017.1421717.
Sholokhova D, et al. Knowledge of CPR and first aid for children among pedagogy students. Crit Care Innov. 2023;6(4):23–33. https://doi.org/10.32114/CCI.2023.6.4.23.33.
Borovnik Lesjak V, Šorgo A, Strnad M. Retention of knowledge and skills after a basic life support course for schoolchildren: a prospective study. Inquiry. 2022;59:00469580221098755.
Brazier J, et al. Resuscitation guidelines in the Middle East: adoption and adaptation. J Emerg Med. 2017;53(3):320–7.
Böttiger BW, et al. Implementation of resuscitation guidelines in Europe: a comparison between the European resuscitation council and american heart association guidelines. Resuscitation. 2019;138:142–50.
Ghafouri RR, Araj-Khodaei M, Abbasian M, Sahebihagh MH, Mohammadpoorasl A, Parsian Z, et al. Challenges of emergency medical services utilization by older adults in Tabriz, Iran: data from Health Status of Aged People in Tabriz (HSA-T Study). Int J. 2023;1:2.
Awad E, Alinier G, Farhat H, Rumbolt N, Azizurrahman A, Mortada B, Shami R. Provision of bystander CPR for out-of-hospital cardiac arrest in the Middle East: a retrospective gender-based analysis. Int J Emerg Med. 2023;16(1):63. https://doi.org/10.1186/s12245-023-00537-6.
Irfan FB, Castren M, Bhutta ZA, George P, Qureshi I, Thomas SH, Pathan SA, Alinier G, Shaikh LA, Suwaidi JA, Singh R, Shuaib A, Tariq T, McKenna WJ, Cameron PA, Djarv T. Ethnic differences in out-of-hospital cardiac arrest among Middle Eastern Arabs and North African populations living in Qatar. Ethn Health. 2021;26(3):460–9. https://doi.org/10.1080/13557858.2018.1530736.
Alqahtani SE, Alhajeri AS, Ahmed AA, Mashal SY. Characteristics of out of hospital cardiac arrest in the United Arab Emirates. Heart views : the official journal of the Gulf Heart Association. 2019;20(4):146–51. https://doi.org/10.4103/HEARTVIEWS.HEARTVIEWS_80_19.
Duval S, Pepe PE, Aufderheide TP, Goodloe JM, Debaty G, Labarère J, et al. Optimal combination of compression rate and depth during cardiopulmonary resuscitation for functionally favorable survival. JAMA cardiology. 2019;4(9):900–8.
Meaney PA, Bobrow BJ, Mancini ME, Christenson J, De Caen AR, Bhanji F, et al. Cardiopulmonary resuscitation quality: improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128(4):417–35.
Stiell IG, Brown SP, Nichol G, Cheskes S, Vaillancourt C, Callaway CW, et al. What is the optimal chest compression depth during out-of-hospital cardiac arrest resuscitation of adult patients? Circulation. 2014;130(22):1962–70.
Smith GD, et al. Longitudinal studies in CPR training: assessing knowledge retention over time. J Med Educ. 2020;55(2):145–52.
Patel R, Green M. Challenges in assessing the effectiveness of community-based CPR training programs. Resuscitation. 2018;127:102–8.
Ahmad A, Akhter N, Mandal RK, Areeshi MY, Lohani M, Irshad M, et al. Knowledge of basic life support among the students of Jazan University, Saudi Arabia: is it adequate to save a life? Alexandria journal of medicine. 2018;54(4):555–9.
Akhagbaker JM, Aziz KF. Teachers, knowledge and attitudes regarding basic life support atprimary schools in Erbil city. NeuroQuantology. 2022;20(12):970.
Al Enizi BA, Saquib N, Zaghloul MSA, Alaboud MSA, Shahid MS, Saquib J. Knowledge and attitudes about basic life support among secondary school teachers in Al-Qassim, Saudi Arabia. Int J Health Sci. 2016;10(3):415.
Alamri S, Khan M, Jarad M, Almalki A, Alotaibi T, Ahmed A, Alraddadi M, Albalwi Z, Altemani O, Alswayed S. Public knowledge, attitudes and practice toward bystander cardiopulmonary resuscitation in Saudi Arabia, a cross-sectional study. Med Sci. 2021;25(118):3392–9.
Alanazi A, Bin-Hotan A, ALhalyabah H, Alanazi A, Al-oraibi S. Community awareness about cardiopulmonary resuscitation among secondary school students in Riyadh. World J Med Sci. 2013;8(3):186e9.
Alazmi A, Al Salem AH, et al. Knowledge and attitudes towards cardiopulmonary resuscitation among dental students in Abha, Saudi Arabia. J Res Med Dent Sci. 2021;9(3):59–63.
Albazee E, Alnifise M, Almahmoud L, Alsaeedi A, Al-balawi M, Alotaibi T, Al Sharei A. Basic life support awareness level among medical students in Jordan: a cross-sectional study. Front Emergency Med. 2022;6(1):e1–e1.
Alfakey M, Alkarani A. Students’ knowledge and attitudes toward basic life support. Int J Evaluat Res Educ. 2021;10(3):871–7.
Alharbi MM, Horaib YF, Almutairi OM, Alsuaidan BH, Alghoraibi MS, Alhadeedi FH, Alrowithi AS. Exploring the extent of knowledge of CPR skills among school teachers in Riyadh, KSA. J Taibah University Med Sci. 2016;11(5):497–501.
Alhasan D, Fakhraldeen M, Alqabandi S, Alajmi M. High school student CPR training in Kuwait: a cross-sectional study of teacher perspectives, willingness, and perceived barriers. Open Access Emergency Med. 2022;14:639–48.
Alhejaili AS, Alghamdi RA, Al-Dubai SA. Knowledge and attitude of basic life support skills among female school teacher in Al-Madinah, Saudi Arabia. J Family Med Primary Care. 2020;9(5):2281.
Alhussein RM, Albarrak MM, Alrabiah AA, Aljerian NA, Bin Salleeh HM, Hersi AS, et al. Knowledge of non-healthcare individuals towards cardiopulmonary resuscitation: a cross-sectional study in Riyadh City, Saudi Arabia. Int J Emergency Med. 2021;14(1):1–9.
Al-Mohaissen MA. Knowledge and attitudes towards basic life support among health students at a Saudi women’s university. Sultan Qaboos Univ Med J. 2017;17(1):e59.
Almojarthe B, Alqahtani S, AlGouzi B, Alluhayb W, Asiri N. Awareness of Secondary School Students regarding Basic Life Support in Abha City, Southern Saudi Arabia: A Cross-Sectional Survey. Sci World J. 2021;2021:4878305. https://doi.org/10.1155/2021/4878305.
Almulhim N, Al-Mulhim F, Al-Hassan H, Aldamigh O, Al-Hussain R, Alkhalifah A, Alarab Z, Al-Nasser A. Knowledge and attitude of non-healthcare providers towards cardiopulmonary resuscitation in the eastern province of Saudi Arabia. Medical Science. 2022;26:ms245e2328.
Alnajjar H, Hilal RM, Alharbi AJ, Alharthi OH, Batwie RA, AlShehri RM, Algethami MR. Evaluation of awareness, knowledge, and attitudes towards basic life support among non-medical students at two academic institutions in Jeddah, Saudi Arabia. Adv Med Educ Pract. 2020;11:1015–21.
Aloush SM, Al Sabah A, Abu Sumaqa Y, Halabi M, Al Bashtawy M, Suliman M, Abdelkader FA. Cardiopulmonary resuscitation training for undergraduates from nonmedical majors: effectiveness of the three tiers model. Nursing Forum. 2018;53(4):585–91.
Aloush S, Tubaishat A, ALBashtawy M, Suliman M, Alrimawi I, Al Sabah A, Banikhaled Y. Effectiveness of basic life support training for middle school students. J School Nurs. 2019;35(4):262–7.
Alquwaiay FK, Alshammari FA, Alshammari MS, Alquwaiay DA, Alabdali NAN, Elkandow AE, Ahmed HG. Assessment of the levels of awareness toward cardiopulmonary resuscitation: a community-based study in Northern Saudi Arabia. J Educ Health Promot. 2018;7:167.
Owaid Alsharari A, Alduraywish A, Ali Al-Zarea E, Ibrahim Salmon N, Ali Sheikh MS. Current Status of Knowledge about Cardiopulmonary Resuscitation among the University Students in the Northern Region of Saudi Arabia. Cardiol Res Pract. 2018;2018:3687472. https://doi.org/10.1155/2018/3687472.
Al-Turki YA, Al-Fraih YS, Jalaly JB, Al-Maghlouth IA, Al-Rashoudi FH, Al-Otaibi AF, et al. Knowledge and attitudes towards cardiopulmonary resuscitation among university students in Riyadh, Saudi Arabia. Saudi med J. 2008;29(9):1306–9.
Aqel AA, Ahmad MM. High-fidelity simulation effects on CPR knowledge, skills, acquisition, and retention in nursing students. Worldviews on Evidence-Based Nursing. 2014;11(6):394–400.
Gaafar RM, Khan AS, Elmorsy S. Knowledge and attitude of young population toward CPR training, results from largest training session in an official attempt to enter Guinness Book of Records: a cross-sectional study from Saudi Arabia. J Family Med Primary Care. 2022;11(2):531.
Ghanem E, Elgazar M, Oweda K, Tarek H, Assaf F, El-Husseny MWA, et al. Awareness of basic life support among Egyptian medical students; a cross-sectional study. Emergency. 2018;6(1):e36.
Hamadneh S, Raffee L, Hamadneh J, Kassab M, Almomani F, Obeidat RA, Almazloom O. Knowledge and attitudes toward infant BLS among babysitters and nursemaids working in rural northwest Jordan. J Emergency Med Trauma & Acute Care. 2020;2020(1):7.
Jarrah S, Judeh M, AbuRuz ME. Evaluation of public awareness, knowledge and attitudes towards basic life support: a cross-sectional study. BMC Emerg Med. 2018;18(1):1–7.
Kasem A, Abuhammad S. Pediatric Basic Life Support among Nursing Students in Jordan: Stimulation-Based Education. Open Nurs J. 2022;16(1).
Mansour A, Alsager AH, Alasqah A, Altamimi AS, Alsuhaibani A, Aljabr AA, et al. Student’s knowledge, attitudes, and practices related to cardiopulmonary resuscitation at Qassim University, Saudi Arabia. Cureus. 2019;11(11):e6169.
Oteir AO, Almhdawi KA, Kanaan SF, Alwidyan MT, Williams B. Cardiopulmonary resuscitation level of knowledge among allied health university students in Jordan: a cross-sectional study. BMJ Open. 2019;9(11):e031725.
Oteir A, Mhdawi K, Kanaan S, Alwidyan M, Williams B. Attitudes towards CPR among allied health students in Jordan: a cross-sectional study. Austral J Paramed. 2020;17:1–8.
Abbas F, Sawaf B, Hanafi I, Hajeer MY, Zakaria MI, Abbas W, Alabdeh F, Ibrahim N. Peers versus professional training of basic life support in Syria: a randomized controlled trial. BMC Med Educ. 2018;18:1–9.
Al Harbi N, Afifi A, Alateeq M, Tourkmani A, Alharbi T, Albattal S. Awareness of basic life support and cardiopulmonary resuscitation among female secondary school students in government schools in Riyadh city, KSA. J Family Med Prim Care. 2018;7(6):1493.
Alghamdi YA, Alghamdi TA, Alghamdi FS, Alghamdi AH. Awareness and attitude about basic life support among medical school students in Jeddah University, 2019: a cross-sectional study. J Family Med Primary Care. 2021;10(7):2684.
Aloraibi S. Community awareness about cardiopulmonary resuscitation among secondary school students in Riyadh. World J Med Sci. 2013;8:186–9.
Alshehri MH, Alqahtani MA, Alshehri SM, Alturki RI, Alshiha KA, Alqahtani MA, Alshehri SM. Knowledge and attitude of basic life support among medical students at Al-Imam Muhammad Ibn Saud Islamic University in Riyadh, Saudi Arabia. Middle East J Family Med. 2021;7(10):47.
Awadalla NJ, Al Humayed RS, Mahfouz AA. Experience of basic life support among King Khalid University health profession students, Southwestern Saudi Arabia. Int J Environ Res Public Health. 2020;17(13):4822.
Hassan EA, Elsaman SEA. The effect of simulation-based flipped classroom on acquisition of cardiopulmonary resuscitation skills: a simulation-based randomized trial. Nurs Crit Care. 2022;28(3):344–52.
Majid A, Jamali M, Ashrafi MM, Haq ZU, Irfan R, Rehan A, et al. Knowledge and attitude towards cardiopulmonary resuscitation among doctors of a tertiary care hospital in Karachi. Cureus. 2019;11(3):e4182.
Qara FJ, Alsulimani LK, Fakeeh MM, Bokhary DH. nowledge of nonmedical individuals about cardiopulmonary resuscitation in case of cardiac arrest: a cross-sectional study in the population of Jeddah, Saudi Arabia. Emergency Med Int. 2019;2019:3686202.
Shams A, Raad M, Chams N, Chams S, Bachir R, El Sayed MJ. Community involvement in out of hospital cardiac arrest: a cross-sectional study assessing cardiopulmonary resuscitation awareness and barriers among the Lebanese youth. Medicine. 2016;95(43):e5091.
Srinivasan AP, Albalawe MA, Issrani R, Patil SR, Prabhu N, Siddanna S. Awareness, knowledge, and attitude of Saudi students towards basic life support: a cross-sectional study. Pesquisa Brasileira em Odontopediatria e Clínica Integrada. 2021;21:43.
Subki AH, Mortada HH, Alsallum MS, Alattas AT, Almalki MA, Hindi MM, et al. Basic life support knowledge among a nonmedical population in Jeddah, Saudi Arabia: cross-sectional study. Int J Med Res. 2018;7(2):e10428.
Zakirulla M, Faden R, Al Hadhir A, Alqahtani A, Abu-Hawi R, Asiri A, Alqahtani N, Alqahtani R, Alfaifi O, Al-Salem A, Almalki M, Al-Zabin H, Alshehri D, Abu Msmar S, Otudi A. Knowledge and attitudes towards cardiopulmonary resuscitation among parents in Abha, Saudi Arabia. J Res Med Dent Sci. 2021;9(12):184–7.
Alhakamy NA, Zamzami AM, Bukhari FA, Bukhari FA, Almash OA, Madkhali MA, et al. Knowledge and attitude about basic life support and emergency medical services among pharmacy students at King Abdulaziz University, Jeddah, Saudi Arabia. Saudi J Emergency Med. 2020;1(2):70–70.
Alkarrash MS, Shashaa MN, Kitaz MN, Rhayim R, Ismail M, Swed S, et al. Basic life support awareness among medical undergraduate students in Syria, Iraq, and Jordan: a multicenter cross-sectional study. Int J Emergency Med. 2023;16(1):44.
Khashaba A, Alharbi M, Alghunaim M, Alsemari L, Almohaimeed W. Knowledge and awareness of basic life support among nonhealth-care providers in Riyadh. Saudi J Oral Sci. 2021;8(1):38–38.
Al-Riyami H, Al-Hinai A, Nadar SK. Determinants of provision of bystander cardiopulmonary resuscitation among the general public in Oman. Sultan Qaboos Univ Med J. 2020;20(4):e380.
Alrasheedi SM, Alrashdi MN, Almutairi KF, Alruways AF, Almutairi IN, Alfehaid SN, et al. Awareness, knowledge, and attitudes regarding basic life support among the population with relatives suffering from heart diseases in the Al-Qassim Region, Saudi Arabia. Cureus. 2022;14(11):e31530.
Alavudeen S, Basharat V, Khaled Bahamdan A, Easwaran V, Khaled Bahamdan G, Akhtar MS, et al. Knowledge, attitude and preparedness of healthcare students toward basic life support at King Khalid University, Abha, Kingdom of Saudi Arabia. Clin Experiment Hyperten. 2022;44(7):634–40.
Aljewayed BH, Albaik NZ, Aljuwayed HS, Aljewayed FHS, Albaik SZ, AlQarous MA, Alshorafa JM. Knowledge, attitude, and practice about CPR and associated factors among laypersons in Dammam, Riyadh, and Jeddah. Indian J Sci Technol. 2019;12:47.
Acknowledgements
None.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
Mohammed Alsabri Hussein (MA) along with Basel F. Alqeeq (BA) are considered as the first authors as they participated in the screening and the selection of the studies, contributed to the conception, formulation, drafting of the article, reviewed and revised the manuscript. MA* is the corresponding author who proposed the project and wrote the study protocol. Mohamed Sayed Zaazouee (MSZ) assisted with writing the protocol, conducted the literature search, and helped with data analysis. MSZ and Alaa Ahmed Elshanbary (AAE) participated in the screening of the studies. BA and YS (Youssef Soliman) helped with the data extraction, quality assessment of the included studies, and critical revision. YS conducted the data analysis, and participated in writing and revison the final manuscript. Rebecca Yu (RY) participated in writing and revision of the final manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alsabri, M.A.H., Alqeeq, B.F., Elshanbary, A.A. et al. Knowledge and skill level among non-healthcare providers regarding cardiopulmonary resuscitation (CPR) training in the Middle East (Arab countries): a systematic review and meta-analysis. BMC Public Health 24, 2081 (2024). https://doi.org/10.1186/s12889-024-19575-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19575-7