Abstract
Background
Too much sedentary behavior (SB) and too little physical activity (PA) place adult workers at risk for chronic illness. It remains unclear which occupations and subgroups within occupations have the highest and lowest SB and PA, and little is known about the effects of organizational factors on these behaviors and metrics. Thus, our main aims were to review and summarize evidence describing daily SB and PA collected using accelerometry across various occupations and to identify organizational factors influencing SB and PA.
Methods
A literature search of six databases was performed for relevant studies published through March 2023. Eligible studies were in English, targeted working populations, had a sample size > 75, and objectively measured both SB and PA for seven consecutive days using accelerometers. Following PRISMA guidelines, 5,197 studies were identified, and 19 articles met our inclusion criteria. Five of these studies were included in a meta-analysis comparing time spent in SB, light PA (LPA), and moderate to vigorous PA (MVPA) across occupations. Methodological quality was assessed using a Joanna Briggs Institute tool.
Results
We found that 63% of the studies reported daily time spent in SB and in MVPA, but fewer reported LPA, moderate PA, and vigorous PA. The average time spent in SB was 553.34 min/day, in LPA was 299.77 min/day, and in MVPA was 33.87 min/day. In occupational subgroup analysis, we observed that office workers had 2.3 h more SB, 2.4 less hours LPA, and 14 min less MVPA per day than nurses. However, most studies either did not specify workers’ occupations or grouped occupations. Shift work and workplace facilities significantly influenced SB and PA, but organizational factors affecting these behaviors were not sufficiently investigated (e.g., occupation type, work environment and workplace facilities, and shift work).
Conclusions
More research is needed to explore SB and PA patterns within occupational subgroups. Additionally, it is important to explore work-related individual (e.g., job task), interpersonal (e.g., social support from colleagues), organizational (e.g., work policy), and environmental factors influencing SB and PA. Future studies should also investigate the association of these factors with SB and PA.
Similar content being viewed by others
Introduction
Too much sedentary behavior (SB) and too little physical activity (PA) place adult workers at risk for chronic illness [1,2,3]. SB is defined as “any waking behavior characterized by an energy expenditure ≤ 1.5 metabolic equivalents (METs), while in a sitting, reclining or lying posture [4], and PA is defined as body movements facilitated by skeletal muscles that lead to energy expenditure [5]. High SB is positively associated with all-cause mortality, including death from cancer and other chronic disease [6], while PA provides health benefits to reduce mortality [7]. Nevertheless, 46% of U.S. adults aged 18 to 64 years did not meet aerobic-activity or muscle-strengthening PA guidelines for Americans in 2020 [8]. Also, a recent U.S. Centers for Disease Control and Prevention report showed that over 25% of Americans aged ≥ 18 years were physically inactive [9]. Because adult workers spend a significant amount of time working, work-related patterns of SB and PA contribute significantly to total SB and PA [10, 11], but the relationship between work related SB and PA and total SB and PA is complex. People with physically active occupations can be highly sedentary during non-working hours, thereby offsetting the potential health benefits derived from the PA accumulated during working hours, the PA paradox [12]. Thus, the combined patterns of SB and PA must be understood to better manage workers’ health.
Sedentary work is on the rise, contributing to increased SB among workers and reduced overall PA levels [10, 13]. For occupational settings, there is currently no standard definition of sedentary work based on energy expenditure [14, 15]. In addition, SB and PA are often considered polar opposites [5], but this is not reflected by studies. For example, occupation types with the lowest reported SB are food preparation and sewing and farming, fishing, and forestry, but working groups showing the highest moderate to vigorous physical activity (MVPA) are healthcare support and community and social service [16]. Thus, it remains unclear which occupations and subgroups within occupations have the highest and lowest SB and PA, and how organizational factors affect these measures. To address this gap, our review focuses on studies that capture both measures.
Office work is generally classified as sedentary [13, 16] and is considered a high-SB occupation; however, the occupational groups with the highest PA levels have varied in different studies [13, 16]. In addition, only a few organizational factors that influence SB and PA have been identified, namely the work environment [17], benefits of social support in workplace [18], worksite culture [19], and worker characteristics. This lack of information makes it difficult to understand whether workers’ lifestyles, workplace behaviors, and environments are barriers or motivators for SB and PA.
Although previous studies have described SB and PA in adult workers, most of their results have been based on self-reported measures or on measurement of SB or PA but not both [11, 17]. Moreover, the accelerometry studies that have been conducted had challenges in terms of being representative of each occupation due to a small sample size [20]. Because estimates of SB and PA have differed significantly depending on whether they were self-reported or accelerometer-measured [21], we focused our study on SB and PA outcomes measured in larger samples by accelerometry only to maximize the accuracy of our findings. The aims of this review were as follows:
-
1.
Summarize the evidence of daily SB and PA measured by accelerometry for different occupations in large-scale studies.
-
2.
Identify organizational factors influencing SB and PA
Methods
Search strategy
The comprehensive literature search for this systematic review and meta-analysis followed Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) guidelines [22]. Through April 25, 2024, six databases were searched for relevant literature: Cumulative Index of Nursing and Allied Health Literature (CINAHL) Complete EBSCO, Excerpta Medica Database (Embase), PubMed, Scopus, SPORTDiscus EBSCO, and Web of Science. Search terms were selected to focus on studies addressing exercise or SB and PA in working populations (see Appendix A). A reference librarian was consulted for the selection of databases and the development of search terms. In addition to the database search, we manually reviewed the reference lists of the included studies in an attempt to identify other relevant studies.
Study selection and data extraction
The inclusion criteria were as follows: (a) primary research published in English in peer-reviewed journals, (b) studies specifically targeting the working population, and (c) sample sizes > 75, (d) objective measurement of both SB and PA for seven consecutive days using accelerometry following National Health and Nutrition Examination Survey PA monitoring guidelines [19, 20], (d) inclusion of at least 3 valid days of accelerometer data, and I reporting of time spent in SB and PA as means with standard deviations (SDs) or confidence intervals (CIs) to allow consistent comparison of outcome variables.
Because appropriate sample sizes for feasibility and pilot studies range from 10 to 75 [23], our review targeted studies with samples > 75 to obtain reliable and valid results that would adequately reflect variations across occupational groups. We chose the sample threshold of 75 to capture studies that potentially had more heterogeneous samples within occupational groups; this choice was based on Teresi et al.’s (2023) recommendation that sample sizes of 70 to 100 per group should be required for detection of group differences in pilot studies [24]. Also, although 4 valid days of accelerometer data are desirable [25], we set our inclusion criterion at 3 valid days to maximize the number of large-sample studies included [26].
We excluded studies of the general population when working status was only described as part of the demographic characteristics; measured only SB or PA because there is a known strong negative relationship between SB and LPA [27]; reported outcomes as percentages, METs, or step-counts; or reported outcomes as median and/or interquartile range.
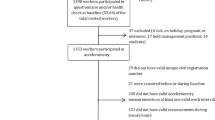
This review was prospectively registered with the PROSPERO database of systematic and meta-analysis reviews (CRD42022374343). The search yielded 682 articles in CINAHL, 1,164 in Embase, 931 in PubMed, 1,297 in Scopus, 384 in SPORTDiscus EBSCO, and 1,318 in Web of Science (Fig. 1). We removed 2,831 duplicates using EndNote 20 [28]. The first author screened titles and abstracts using EndNote, and 2,492 articles were excluded. The remaining 171 articles were independently examined by three authors (SP, SL, KW) [29] and 19 articles met criteria for inclusion (see Fig. 1). We extracted publication information, sample characteristics, research design, measurements of the two main outcomes (i.e., total time/day in SB and in PA), and relevant findings (see Supplementary Table 1). Completeness and accuracy of the data extracted were assessed and double-checked by four authors (SP, SL, SW, KW). The corresponding/first authors of three articles were contacted for additional information, and two responded. All main outcomes were reported as min/day.
Risk of bias in selected studies
The risk of bias in the selected studies was assessed using the Joanna Briggs Institute’s (JBI) critical appraisal tools. We used the appropriate JBI tool for each research design (see Fig. 2): cohort (11 questions) [30], cross-sectional (8 questions) [30], quasi-experimental (9 questions), and randomized controlled trial (13 questions) [32]. Each question was rated using four categories: “Yes,” “No,” “Unclear,” or “Not applicable.”
Two authors (SL and SW) independently assessed the quality of the selected studies and resolved any disagreements through discussion. If disagreements remained unresolved, a third author (SP) was consulted to reach a consensus. There is no established guideline for determining scoring values using the JBI tool [30,31,32]. Therefore, we calculated the proportion of “Yes” divided by the total number of questions excluding “Not applicable” in each study. We evaluated the degree of risk (i.e., low, moderate, and high risk of bias) [33, 34].
Meta-analysis
For the meta-analysis, two authors (SP and KW) prepared a coding list of variables of interest based on Supplementary Table 1 (i.e., study number, publication year, sample size, occupation, SB, and PA levels). Given that most study designs were cross-sectional, we selected the baseline outcome values for studies with multiple outcomes at various time points [35, 36]. After double-checking the variables for consistency, a senior biostatistician (PV) verified the list [37]. Ten studies examined time spent in both SB and PA across the total study sample using a combination of working days and non-working days [38,39,40,41,42,43,44,45,46,47]. For studies reporting multiple outcomes at various time points, we selected the baseline outcome values for consideration. [45, 47]. Seven of the 10 studies were included in the meta-analysis; they all used hip/waist-mounted Actigraph accelerometers. The other three were excluded because one reported data from a wrist-worn device that produces higher estimates of PA [44] and the others used an accelerometer (Actical [48] and AX3 [46]) that does not produce data comparable to Actigraph data [49, 50].
We used Stata version 18.0 for the meta-analysis [51], employing the mean values and standard errors (SEs) for daily SB and daily PA. SDs and CIs were converted into SEs [52]. Based on Cochrane’s guideline [52], SDs were calculated using the formula SE\(\times \sqrt{sample size}\), and CIs were calculated using the formula SD\(= \sqrt{sample size} \times (upper limit-lower limit)/ 3.92\) (given the 95% CI range). To calculate the pooled SD for two groups [45, 47], we used the formula [53] SDpooled\(=\sqrt{\frac{\left(n1-1\right)\left(SD1\right)({\text{SD}}1)+\left(n2-1\right)\left(SD2\right)(SD2)}{n1+n2-2}}\). A random-effects model was applied for the analysis due to expected variations across occupational groups in the meta-analysis [54].
Results
The research purpose, design, sample size and characteristics, measures, main outcomes (i.e., time spent in daily SB and daily PA [min/day]), and other relevant findings for each selected study are summarized in Supplementary Table 1. Of the 19 selected studies, 14 were cross-sectional, two were quasi-experimental, two were randomized controlled trials (RCTs), and one was a cohort study. The sample size varied from 78 to 3,513 workers, and mean ages ranged from the mid-30s to early 50s. Four studies were conducted in Japan, and three studies each in the USA, and Canada. Two studies were conducted in Finland and one study each in Sweden, New Zealand, the UK, Thailand, Taiwan, South Africa, and Singapore. During our review, we classified the occupation types reported in the studies into four groups: (1) office workers [36, 41, 42, 45,46,47, 55], (2) occupation not specified (typically referred to only as “worker/employee”) [38, 48, 56,57,58,59], (3) grouped occupations (combinations of several occupations such as workers in banking services and at amusement parks) [35, 39, 44, 60], and (4) nurses [40, 43]. These classifications are further discussed under “Organizational Factors Related to SB and PA” below.
Most of the 19 studies reviewed were conducted prior to the COVID-19 pandemic, but data were collected for three studies [45, 46, 60] during the pandemic. Among these three studies [45, 46, 60], only Fujii et al.’s study compared SB and PA before and during COVID-19; they reported that office workers showed increased SB and reduced PA both on weekdays and weekends after the pandemic compared to before it [60].
Regarding measurement devices for SB and PA, 10 studies used the ActiGraph (53%); four [55, 56, 58, 60] used the Active style Pro HJA; and one each used the Fitbit [44], Actical [48], AX3 [46], Hookie AM [35], and UKK RM42 [59]. Two studies [36, 42] that applied the ActiGraph also used the activPAL to assess SB in greater detail. The device wear location was most commonly the waist or hip (79%; 15 of 19 studies); three [44, 46, 57] studies employed a wrist-worn device, and one [56] did not identify the wear location. Twelve studies [35, 36, 38, 39, 41, 42, 46,47,48, 56, 57, 59] reported 7 consecutive days of monitoring. Of 19 studies, the number of required valid days of data varied: ≥ 4 days in 10 studies [38, 40, 41, 43, 46,47,48, 57,58,59], ≥ 3 days in one study [39], and 14 days in one study [44]. Additional seven studies included data for a mix of working and weekend days such as 3 working days and 1 non-working day [36, 56], 2 working days and 1 non-working day [42, 55, 60], and 3 working days only [35, 45]. Most studies reported using 60-s epochs [36, 38, 39, 41, 42, 44, 45, 47, 48, 55, 57, 60].
No studies showed a high risk of bias. Most studies had a low risk (16 of 19 studies) [35, 36, 38, 39, 41,42,43,44, 46,47,48, 55, 57,58,59,60], and three [40, 45, 56] had a moderate risk of bias (see Fig. 2– Figs. 2a-d). Two of the studies [40, 56] with a moderate risk of bias were cross-sectional and raised concerns related to a lack of clear selection criteria. In addition, one RCT study [45] posed concerns regarding the blind assignment of treatment; it was unclear how blinding could have been maintained for each participant and researcher and how to avoid cross-contamination between control and intervention groups.
Profiles of total daily SB and PA time
Both daily SB and MVPA during waking hours were reported in 12 (63%) of the 19 studies [38,39,40,41,42,43,44,45,46,47,48, 57]. For profile calculations, we excluded Hajo et al.’s study [40] because it employed the same dataset as was used in Reed et al.’s study [40]. Across seven of these studies employing a waist-worn ActiGraph and a total of 3,176 workers [38, 39, 41,42,43, 45, 47], the mean SB time was 553.34 min/day (SD 91.54 min/day), and the mean MVPA time was 33.87 min/day (SD 21.68 min/day) [38, 39, 41,42,43, 47]. Also, our review revealed that relatively low proportions of studies reported LPA, moderate PA, and vigorous PA: only 42% [40,41,42,43,44,45,46, 57] reported LPA, and 16% [40, 43, 44] reported both moderate PA and vigorous PA. Across four studies with waist-worn ActiGraph and a total of 957 workers, the mean LPA was 299.77 min/day (SD 74.96 min/day) [41,42,43, 45].
The main outcomes, time in daily SB and PA, were not consistently reported (Supplementary Table 1). Studies reported results based on commute mode [39], work shifts [48, 57], or sample characteristics [36, 41, 47, 59], such as sex.
SB and PA by specific timeframe
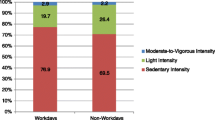
Eight of 19 studies reported SB and PA according to specific timeframes such as working days, working hours during working days, and non-working days (see Supplementary Table 2) [35, 36, 42, 45, 55, 56, 58, 60], but results were inconsistently reported across those studies. Only one [42] reported detailed outcomes for all three categories: working days (also addressing working vs non-working hours), non-working days, and mixed days (encompassing both working and non-working days). An additional seven studies addressed only one or two of these categories in their outcomes (see Supplementary Table 2).
During our review, we observed no consistent trends in SB or PA intensity between working days and non-working days across studies. For example, in two studies [36, 42], detailed SB and PA outcomes for a total of 158 workers were obtained using both the activPAL (for SB) and ActiGraph (for PA). In those studies [36, 42], workers showed more SB and less PA on working days. Specifically, they had 49 min/day more SB, 29 min/day less LPA, and 3.34 min/day less MVPA on working days than on non-working days [36, 42]. However, different outcomes were reported by three studies [55, 56, 58] using an HJA device; those studies involved totals of 629 workers on working days [56, 58] and 1,663 workers on non-working days [55, 56]. Across these studies [55, 56, 58], workers had 1,019.5 min/day less SB on working days but were more physically active on non-working days, showing 149.95 min/day more LPA and 19.3 min/day more MVPA than on working days.
Meta-analysis of SB and PA
Seven studies with a total of 3,176 workers were included in the meta-analysis [38, 39, 41,42,43, 45, 47]. Occupation type was the only common factor among them, and so we conducted a subgroup analysis by occupation (see Fig. 3). Workers studied included nurses in one study (n = 410) [43], office workers in four studies (n = 913) [41, 42, 45, 47], workers with occupation not specified in one study (n = 1,313) [38], and workers with grouped occupations in one study (n = 540) [39].
The time spent in SB across all seven studies [38, 39, 41,42,43, 45, 47] averaged 553.34 min/day (95% CI 505.63 – 601.05., p < 0.001., Fig. 3-a). Based on subgroup analysis, nurses [43] had the lowest SB (mean = 445 min/day, 95% CI 433.77 – 456.22), followed by workers with occupation not specified [38] (mean = 507.20 min/day, 95% CI 501.59 – 512.81), and workers with grouped occupations [39] (mean = 580.60 min/day, 95% CI 574.48 – 586.72). Office workers [41, 42, 45, 47] had the highest SB (mean = 585.33 min/day, 95% CI 528.02 – 642.64., p < 0.001).
As shown in Fig. 3-b, the mean time spent in LPA was 299.77 min/day (95% CI 218.63 – 380.90., p < 0.001) [41,42,43, 45]. For subgroup analysis, only two occupations were used: Office workers [41, 42, 45] had lower LPA (mean = 263.86 min/day, 95% CI 215.76—311.96., p < 0.001) than nurses [43] (mean = 408 min/day, 95% CI 400.35—415.65). In addition to all workers, the average time spent in MVPA [38, 39, 41,42,43, 45, 47] was 33.87 min/day (95% CI 25.49 – 42.25., p < 0.001., see Fig. 3-c). Office workers had the lowest MVPA (mean = 26.72 min/day, 95% CI 21.15 – 32.30., p < 0.001), followed by those with occupation not specified (mean = 32.80 min/day, 95% CI 31.57 – 34.03) and nurses (mean = 41.10 min/day, 95% CI 39.13 – 43.07). Workers with grouped occupations had the highest MVPA (mean = 52.90 min/day, 95% CI 50.48 – 55.32). Compared to office workers (lowest MVPA), workers with grouped occupations (highest MVPA) had 26.18 min/day higher MVPA.
Organizational factors related to SB and PA
Organizational factors influencing SB and PA were insufficiently addressed in the 19 studies, as the only organizational factor considered in every study was occupation type. The most common occupation type was office workers [36, 41, 42, 45,46,47, 55]. Other occupation types were nurses [40, 43], workers with occupations not specified [38, 48, 56,57,58,59], and workers with grouped occupations [35, 39, 44, 60].
The organizational factors most commonly found to influence SB and PA were on-site work environment and facilities [35, 38, 43, 47] and shift work [40, 43, 48, 57]. Regarding on-site work environment and facilities [35, 38, 43, 47], two studies [35, 47] involved interventions that adjusted the work environment to promote decreased SB and increased PA. For instance, Deery et al. [46] reported that PA calorie expenditure labels implemented in worksite cafeterias slightly reduced SB and increased PA [47]. As for shift work, shift work type [43, 48, 57], shift length [43], and shift work disorders [40] were reported as influencing SB and PA, and specific shift conditions influenced SB and PA differently. For example, rotating shift workers had less SB and more LPA than day shift workers [57]. In addition, other organizational factors influencing SB and PA were absenteeism [40], work performance efficiency [58], and commute mode and commute distance [39]. Although unit-peer support was included as one component of the intervention addressed by Aitassalo et al., [35] no significant influence of social support on SB or PA was reported in their study or in any others.
Discussion
Having estimated daily SB and PA using accelerometry, our review indicates that adult workers average 9.22 h per day in SB, 5 h per day in LPA, and 0.56 h per day in MVPA. Also, our review revealed that the only common organizational factor influencing SB and PA was occupation type. Notably, we found that insufficient organizational factors were examined in terms of their influence on SB and PA.
Our review highlighted two specific occupations (nurses and office workers), suggesting that estimating SB and PA based on workers’ individual characteristics, such as occupation and age, helps capture these parameters more meaningfully than estimating them for working adults as a whole. Compared to a previous review [13] that included studies employing a combination of various devices to measure SB and PA and varied sample sizes of working adults, our waist-worn Actigraph-derived SB and PA estimates were based on larger samples. However, we obtained similar findings: a 12.46-min lower SB and a 9.53-min lower LPA, but a 19-min greater MVPA. In addition, we compared our outcomes with previous studies [64, 65] examining a large sample of the general adult population included in the U.S. National Health and Nutrition Examination Survey, which like our study employed waist-worn Actigraph data. In comparison with those studies [64, 65], we found that workers (in our review) had more SB, less LPA [64], and more MVPA than in Kim and Kang’s [64] study [65] but less MVPA than in Fishman et al.’s [63] study [64]. These differences in outcomes may be due to the age range of the sample. Previous studies [64, 65] included older adults aged 65 or more. Approximately 50% of the studies (10 of 19) either did not clearly classify occupations within groups or used workers whose occupations could not be differentiated when reporting SB and PA. Despite these limitations, our review highlighted findings for two specific occupations: office workers and nurses. For office workers, our results support previous studies’ [13, 16] findings that office workers had the highest SB. With respect to PA, however, we found that office workers showed the lowest MVPA, whereas a prior review [13] reported that office workers had more MVPA than other occupations. Notably, the term “office worker” was typically not defined in past studies [66,67,68,69]. To better understand the profiles of office workers and create tailored strategies to increase their PA and decrease their SB, subgroups of office workers need to be defined and classified. One way to do so is to use occupational codes such as the Standard Occupational Classification System (e.g., 43–0000 for Office and Administrative Support Occupations) [70] and/or the North American Industry Classification System (e.g., 561,110 for Office Administrative Services) [71]. To achieve greater consistency in research reporting, these occupational codes can be converted using “autocoder” software applications [72]. As for the nursing occupation, a previous study targeting nurses [73] has reported findings similar to ours. In that research, nurses showed lower SB (mean = 445 min/day) [73] and higher MVPA compared to other healthcare occupations. To better understand the facets of multiple occupations across industries, we recommend that future studies investigate specific occupations and groups of occupations and measure each outcome for different occupations within specific industries.
Moreover, our review did not find sufficient organizational factors that influence SB and PA, with our key findings being limited to the effects of shift work and onsite-work facilities on work performance and benefits to the company (e.g., work performance efficiency, absenteeism). In general, the reviewed studies neglected to examine social organizational factors such as social support and workplace climate, workplace benefits (e.g., a PA work wellness program), mental stress caused by the job, and individual organizational factors (e.g., job task and home office work environment). Nevertheless, we did find that a few studies reported on partial organizational factors such as workplace facilities. The dominant organizational factors that we identified as influencing SB and PA, namely occupation types, may not fully capture the evolving nature of how job tasks are impacted by technological advancement [74]. Therefore, it is essential that more studies explore diverse occupational changes (e.g., job characteristics [job task] and workplace [home-office]) and micro–macro level factors that influence SB and PA. Such studies may eventually enhance work climate and policy support, thereby reducing SB and increasing PA for workers.
Following the COVID-19 pandemic, workers have reported increased SB and reduced PA [75], with remote workers in particular having experienced a significant increase in SB and decrease in PA [76, 77]. However, those studies were based on self-reported data. Brusaca et al.’s [77] study, which used accelerometry, supported the finding that sitting time was higher in remote workers than in on-site workers [78]. There findings were also supported by our review: among the 19 studies we reviewed, Fujii et al.’s [59] study [60] reported that office workers had more SB and less PA after the pandemic than before. To mitigate these negative trends in SB and PA, a combination of home working environment modifications and behavior-changing strategies have been recommended. Indeed, these changes have proven effective in improving remote workers’ mental health, reducing their SB, and enhancing their work performance [79]. These outcomes reflect the importance of designing workplaces, be it remote or traditional, that promote worker health and well-being. They also highlight the growing need to facilitate healthy remote work environments and establish a supportive organizational culture [77]. On the whole, future research should comprehensively examine the impact of home and traditional work arrangements and their associated environments on SB and PA.
Strengths and limitations
One of the strengths of this review is its emphasis on objectively measured SB and PA using accelerometry. It helps to overcome the inherent bias in self-reported SB and PA, overestimation of PA and under-estimation of SB [21]. In addition, our meta-analysis compared SB and PA in four working groups (i.e., workers with grouped occupations, nurses, office workers, and workers with occupation not specified), thereby supporting results from the systematic review and enhancing the rigor and validity of our findings.
The study findings are subject to a number of limitations. First, due to our stringent inclusion and exclusion criteria, our study could not capture SB and PA across the range of occupations. For example, in the meta-analysis, we could compare only two identifiable occupation types—office workers and nurses. For studies that aggregated data and grouped results for multiple groups, we were unable to separate results by occupation. However, we believe that our approach was justified in providing a synthesis of the most reliable data available. Second, although most of the reviewed studies showed a low risk of bias, our findings regarding factors significantly influencing SB and PA should be interpreted with caution because several of the studies were cross-sectional, and we included those outcomes. Third, methodological differences among the reviewed studies made it challenging to synthesize their results. Studies used different devices; different device placements (waist/hip vs wrist); and different timeframes such as working days, non-working days, and a combination of the two. As an example of the issues arising from these differences, we did not include results based on data from wrist-worn devices [44, 57] because they have no standard cut points [80, 81]. To minimize outcome variances, our meta-analysis results for SB and PA are based solely on data generated by ActiGraph devices worn on the waist/hip [38, 39, 41,42,43]. Finally, because the aim of the review was to assess evidence regarding total daily SB and PA, we did not explicitly consider posture-specific accelerator measurements such as standing vs. sitting.
Conclusion
Our review indicates that adult workers average 9.22 h per day in SB, 5 h per day in LPA, and 0.56 h per day in MVPA. Our review supports earlier reports of office workers having higher SB and lower PA than other groups of workers. Nurses had the lowest SB and highest PA. To better detect occupational subgroup differences using accelerometry, we suggest that future studies specify outcomes from grouped occupations and/or specific occupations from different industry categories.
There is limited evidence identifying organizational factors that influence SB and PA along with SB and PA outcomes. To more comprehensively understand SB and PA in working adults, it is essential to explore work-related individual (e.g., job task), interpersonal (e.g., social support from colleagues), organizational (e.g., work policy and work culture), and environmental factors (e.g., office facilities) influencing SB and PA and their associations with SB and PA outcomes. Specifically, we suggest that future studies investigate the impact of redesigning workplaces, as social support and interaction at work have been shown to influence SB and PA.
Availability of data and materials
No datasets were generated or analysed during the current study.
Abbreviations
- CI:
-
Confidential intervals
- CINAHL:
-
Cumulative index of nursing and allied health literature complete EBSCO
- Embase:
-
The excerpta medica database
- JBI:
-
Joanna Briggs Institute
- LPA:
-
Light physical activity
- METs:
-
Metabolic equivalents
- MVPA:
-
Moderate to vigorous physical activity
- PA:
-
Physical activity
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- RCT:
-
Randomized controlled trial
- SB:
-
Sedentary behavior
- SD:
-
Standard deviation
- SE:
-
Standard error
References
Smith L, McCourt O, Sawyer A, et al. A review of occupational physical activity and sedentary behaviour correlates. Occup Med (Lond). 2016;66(3):185–92. https://doi.org/10.1093/occmed/kqv164.
Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA. 2018;320(19):2020–8. https://doi.org/10.1001/jama.2018.14854.
U.S. Center for Disease Control and Prevention (CDC). Brief Summary of Findings on The Association between Physical Inactivity And Severe COVID-19 Outcomes. Accessed May 10, 2023. https://www.cdc.gov/coronavirus/2019-ncov/downloads/Brief-Summary-of-Findings-on-the-Association-Between-Physical-Inactivity-and-Severe-COVID-19-Outcomes.pdf
Tremblay MS, Aubert S, Barnes JD, et al. Sedentary Behavior Research Network (SBRN) – Terminology consensus project process and outcome. Int J Behav Nutr Phys Act. 2017;14(1):75. https://doi.org/10.1186/s12966-017-0525-8.
Thivel D, Tremblay A, Genin PM, Panahi S, Rivière D, Duclos M. Physical activity, inactivity, and sedentary behaviors: definitions and implications in occupational health. Front Public Health. 2018;6:288. https://doi.org/10.3389/fpubh.2018.00288.
Powell KE, King AC, Buchner DM, et al. The scientific foundation for the physical activity guidelines for Americans, 2nd edition. J Phys Act Health. 2018:1–11. https://doi.org/10.1123/jpah.2018-0618
Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Washington, DC: U.S. Department of Health and Human Services; 2018.
Elgaddal N, Kramarow EA, Reuben C. Physical activity among adults aged 18 and over: United States, 2020. NCHS Data Brief, no 443. Hyattsville: National Center for Health Statistics; 2022. https://doi.org/10.15620/cdc:120213.
U.S. CDC.. Adult Physical Inactivity Outside of Work. U.S. Center for Disease Control and Prevention. Updated 2024 February 1. Accessed May 30, 2024. https://www.cdc.gov/physical-activity/php/data/inactivity-maps.html
Lusa S, Punakallio A, Mänttäri S, et al. Interventions to promote work ability by increasing sedentary workers’ physical activity at workplaces - a scoping review. Appl Ergon. 2020;82:102962. https://doi.org/10.1016/j.apergo.2019.102962.
Prince SA, Rasmussen CL, Biswas A, et al. The effect of leisure time physical activity and sedentary behaviour on the health of workers with different occupational physical activity demands: a systematic review. Int J Behav Nutr Phys Act. 2021;18(1):100. https://doi.org/10.1186/s12966-021-01166-z.
van Tienoven TP, Deyaert J, Harms T, Weenas D, Minnen J, Glorieux I. Active work, passive leisure? Associations between occupational and non-occupational physical activity on weekdays. Soc Sci Res. 2018;76:1–11. https://doi.org/10.1016/j.ssresearch.2018.08.012.
Prince SA, Elliott CG, Scott K, Visintini S, Reed JL. Device-measured physical activity, sedentary behaviour and cardiometabolic health and fitness across occupational groups: a systematic review and meta-analysis. Int J Behav Nutr Phys Act. 2019;16(1):30. https://doi.org/10.1186/s12966-019-0790-9.
Labor Do. Division of Federal Employees' Compensation Procedure Manual. Accessed June 1, 2023. https://www.dol.gov/agencies/owcp/FECA/regs/compliance/DFECfolio/FECA-PT2/group3
Bull FC, Al-Ansari SS, Biddle S, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Steeves JA, Tudor-Locke C, Murphy RA, et al. Daily physical activity by occupational classification in US adults: NHANES 2005–2006. J Phys Act Health. 2018;15(12):900–11. https://doi.org/10.1123/jpah.2017-0465.
Zhu X, Yoshikawa A, Qiu L, Lu Z, Lee C, Ory M. Healthy workplaces, active employees: a systematic literature review on impacts of workplace environments on employees’ physical activity and sedentary behavior. Build Environ. 2020;168:106455. https://doi.org/10.1016/j.buildenv.2019.106455.
Lafrenz A, Lust T, Cleveland M, et al. Association between psychosocial and organizational factors and objectively measured sedentary behavior in desk-dependent office workers. Occup Health Sci. 2018;2(4):323–35. https://doi.org/10.1007/s41542-018-0028-2.
Mullane SL, Toledo MJL, Rydell SA, et al. Social ecological correlates of workplace sedentary behavior. Int J Behav Nutr Phys Act. 2017;14(1):117. https://doi.org/10.1186/s12966-017-0576-x.
Gilson ND, Hall C, Holtermann A, et al. Sedentary and physical activity behavior in “Blue-Collar” workers: a systematic review of accelerometer studies. J Phys Act Health. 2019;16(11):1060–9. https://doi.org/10.1123/jpah.2018-0607.
Tucker JM, Welk GJ, Beyler NK. Physical activity in U.S. adults: compliance with the physical activity guidelines for Americans. Am J Prev Med. 2011;40(4):454–61. https://doi.org/10.1016/j.amepre.2010.12.016.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. https://doi.org/10.1136/bmj.n71.
Lewis M, Bromley K, Sutton CJ, McCray G, Myers HL, Lancaster GA. Determining sample size for progression criteria for pragmatic pilot RCTs: the hypothesis test strikes back! Pilot Feasibility Stud. 2021;7(1):40. https://doi.org/10.1186/s40814-021-00770-x.
Teresi JA, Yu X, Stewart AL, Hays RD. Guidelines for designing and evaluating feasibility pilot studies. Med Care. 2022;60(1):95–103. https://doi.org/10.1097/mlr.0000000000001664.
Shim J, Fleisch E, Barata F. Wearable-based accelerometer activity profile as digital biomarker of inflammation, biological age, and mortality using hierarchical clustering analysis in NHANES 2011–2014. Sci Rep. 2023;13(1):9326. https://doi.org/10.1038/s41598-023-36062-y.
Migueles JH, Cadenas-Sanchez C, Ekelund U, et al. Accelerometer data collection and processing criteria to assess physical activity and other outcomes: a systematic review and practical considerations. Sports Med. 2017;47(9):1821–45. https://doi.org/10.1007/s40279-017-0716-0.
Mansoubi M, Pearson N, Biddle SJH, Clemes S. The relationship between sedentary behaviour and physical activity in adults: a systematic review. Prev Med. 2014;69:28–35. https://doi.org/10.1016/j.ypmed.2014.08.028.
EndNote [Computer software]. Version: 20. Philadelphia: Clarivate; 2013.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5(1):210. https://doi.org/10.1186/s13643-016-0384-4.
Moola S, Munn Z, Tufanaru C, et al. Chapter 7: systematic reviews of etiology and risk. In: Aromataris E, Munn Z, eds. JBI Manual for evidence synthesis. JBI; 2020. https://synthesismanual.jbi.global
Barker TH, Habibi N, Aromataris E, et al. The revised JBI critical appraisal tool for the assessment of risk of bias for quasi-experimental studies. JBI Evid Synth. 2024;22(3):378–88. https://doi.org/10.11124/jbies-23-00268.
Barker TH, Stone JC, Sears K, et al. The revised JBI critical appraisal tool for the assessment of risk of bias for randomized controlled trials. JBI Evid Synth. 2023;21(3):494–506.
Munn Z, Barker TH, Moola S, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth. 2020;18(10):2127–33. https://doi.org/10.11124/jbisrir-d-19-00099.
Fernandez R, Sikhosana N, Green H, et al. Anxiety and depression among healthcare workers during the COVID-19 pandemic: a systematic umbrella review of the global evidence. BMJ Open. 2021;11(9):e054528. https://doi.org/10.1136/bmjopen-2021-054528
Aittasalo M, Livson M, Lusa S, et al. Moving to business - changes in physical activity and sedentary behavior after multilevel intervention in small and medium-size workplaces. BMC Public Health. 2017;17(1):319. https://doi.org/10.1186/s12889-017-4229-4.
Bergman F, Wahlström V, Stomby A, et al. Treadmill workstations in office workers who are overweight or obese: a randomised controlled trial. Article. Lancet Public Health. 2018;3(11):e523–35. https://doi.org/10.1016/S2468-2667(18)30163-4.
Cooper H. Research synthesis and meta-analysis: A step-by-step approach. 5th ed. Inc.: SAGE Publications; 2017.
Crespo NC, Sallis JF, Conway TL, et al. Worksite physical activity policies and environments in relation to employee physical activity. Am J Health Promot. 2011;25(4):264–71. https://doi.org/10.4278/ajhp.081112-QUAN-280.
Ferrer HB, Cooper A, Audrey S. Associations of mode of travel to work with physical activity, and individual, interpersonal, organisational, and environmental characteristics. J Transp Health. 2018;9:45–55. https://doi.org/10.1016/j.jth.2018.01.009.
Hajo S, Reed JL, Hans H, Tulloch HE, Reid RD, Prince SA. Physical activity, sedentary time and sleep and associations with mood states, shift work disorder and absenteeism among nurses: an analysis of the cross-sectional champlain nurses’ study. Peerj. 2020;8:e8464. https://doi.org/10.7717/peerj.8464.
Huang WC, Chang SH, Hsueh MC, Liao Y. Relationship of sleep regularity with device-based sedentary behavior time and physical activity time in working adults. Article. Sleep Health. 2023;9(1):86–92. https://doi.org/10.1016/j.sleh.2022.10.002.
Keown MK, Skeaff CM, Perry TL, Haszard JJ, Peddie MC. Device-measured sedentary behavior patterns in office-based university ennployees. J Occup Environ Med. 2018;60(12):1150–7. https://doi.org/10.1097/JOM.0000000000001467.
Reed JL, Prince SA, Pipe AL, et al. Influence of the workplace on physical activity and cardiometabolic health: results of the multi-centre cross-sectional champlain nurses’ study. Int J Nurs Stud. M 2018;81:49–60. https://doi.org/10.1016/j.ijnurstu.2018.02.001.
Rykov Y, Thach TQ, Dunleavy G, et al. Activity tracker-based metrics as digital markers of cardiometabolic health in working adults: cross-sectional study. JMIR Mhealth Uhealth. 2020;8(1):e16409.https://doi.org/10.2196/16409.
Akksilp K, Koh JJE, Tan V, et al. The physical activity at work (PAW) study: a cluster randomised trial of a multicomponent short-break intervention to reduce sitting time and increase physical activity among office workers in Thailand. Lancet Reg Health Southeast Asia. 2023;8:100086. https://doi.org/10.1016/j.lansea.2022.100086.
Phaswana M, Gordon NF, Gradidge PJL. Sedentary behavior, physical activity patterns, and cardiometabolic risk factors in South African office-based workers. Am J Lifestyle Med. 2023. https://doi.org/10.1177/15598276231210479.
Deery CB, Hales D, Viera L, et al. Physical Activity Calorie Expenditure (PACE) labels in worksite cafeterias: effects on physical activity. BMC Public Health. 2019;19(1):1596. https://doi.org/10.1186/s12889-019-7960-1.
Neil-Sztramko SE, Gotay CC, Demers PA, Campbell KL. Physical activity, physical fitness, and body composition of Canadian shift workers. Article. J Occup Environ Med. 2016;58(1):94–100. https://doi.org/10.1097/JOM.0000000000000574.
Duncan S, Stewart T, Bo Schneller M, Godbole S, Cain K, Kerr J. Convergent validity of ActiGraph and Actical accelerometers for estimating physical activity in adults. PLoS ONE. 2018;13(6):e0198587. https://doi.org/10.1371/journal.pone.0198587.
De Craemer M, Verbestel V. Comparison of outcomes derived from the ActiGraph GT3X+ and the Axivity AX3 accelerometer to objectively measure 24-hour movement behaviors in adults: a cross-sectional study. Int J Environ Res Public Health. 2022;19(1):271.
Stata Statistical Software. Release 18. College Station, TX: StataCorp LLC.; 2023.
Higgins JP LT, Deeks JJ (editors). Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT TJ, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). ed. Cochrane Handbook for Systematic Reviews of Interventions version 63 (updated February 2022). Cochrane; 2022 updated February 2022.
Chi K-Y, Li M-Y, Chen C, Kang E, Cochrane T. Ten circumstances and solutions for finding the sample mean and standard deviation for meta-analysis. Syst Rev. 2023;12(1):62. https://doi.org/10.1186/s13643-023-02217-1.
Dettori JR, Norvell DC, Chapman JR. Fixed-effect vs Random-effects models for meta-analysis: 3 points to consider. Glob Spine J. 2022;12(7):1624–6. https://doi.org/10.1177/21925682221110527.
Kitano N, Kai Y, Jindo T, Fujii Y, Tsunoda K, Arao T. Association of domain-specific physical activity and sedentary behavior with cardiometabolic health among office workers. Scand J Med Sci Sports. 2022;32(8):1224–35.
Kurosawa S, Shibata A, Ishii K, Koohsari MJ, Oka K. Accelerometer-measured diurnal patterns of sedentary behavior among Japanese workers: a descriptive epidemiological study. Int J Environ Res Public Health. 2020;17(11):3814. https://doi.org/10.3390/ijerph17113814.
Loprinzi PD. The effects of shift work on free-living physical activity and sedentary behavior. Prev Med. 2015;76:43–7. https://doi.org/10.1016/j.ypmed.2015.03.025.
Ma J, Ma D, Kim J, Wang Q, Kim H. Effects of substituting types of physical activity on body fat mass and work efficiency among workers. Article. Int J Environ Res Public Health. 2021;18(10):5101. https://doi.org/10.3390/ijerph18105101.
Husu P, Tokola K, Vähä-Ypyä H, Sievänen H, Vasankari T. Accelerometer-measured physical behavior and cardiorespiratory fitness as indicators of work ability. Int J Environ Res Public Health. 2023;20(7)https://doi.org/10.3390/ijerph20075414
Fujii Y, Kitano N, Kai Y, Jindo T, Arao T. Changes in accelerometer-measured physical activity and sedentary behavior from before to after COVID-19 outbreak in workers. J Epidemiol. 2023. https://doi.org/10.2188/jea.JE20230023.
Clemes SA, O’Connell SE, Edwardson CL. Office workers’ objectively measured sedentary behavior and physical activity during and outside working hours. J Occup Environ Med. 2014;56(3):298–303. https://doi.org/10.1097/jom.0000000000000101.
Wu Y, Petterson JL, Bray NW, Kimmerly DS, O’Brien MW. Validity of the activPAL monitor to measure stepping activity and activity intensity: a systematic review. Gait Posture. 2022;97:165–73. https://doi.org/10.1016/j.gaitpost.2022.08.002.
Veronica V-M, Orlagh OS, James AK, et al. Cross-sectional surveillance study to phenotype lorry drivers’ sedentary behaviours, physical activity and cardio-metabolic health. BMJ Open. 2017;7(6):e013162. https://doi.org/10.1136/bmjopen-2016-013162.
Fishman EI, Steeves JA, Zipunnikov V, et al. Association between objectively measured physical activity and mortality in NHANES. Med Sci Sports Exerc. 2016;48(7):1303–11. https://doi.org/10.1249/mss.0000000000000885.
Kim H, Kang M. Sedentary behavior and metabolic syndrome in physically active adults: national health and nutrition examination survey 2003–2006. Am J Hum Biol. 2019;31(2):e23225. https://doi.org/10.1002/ajhb.23225.
World Health Organization. Health Topics. Accessed September 27, 2023. https://www.who.int/health-topics/
Internationl Labour Organization. Topics. Accessed September 27, 2023. https://www.ilo.org/global/topics/lang--en/index.htm
U.S. National Institute for Occupational Safety and Health (NIOSH). Accessed Sepember 27, 2023. https://www.cdc.gov/niosh/index.htm
U.S Department of Labor. Accessed September 27, 2023. https://www.dol.gov/
U.S. Bureau of Labor Statistics. Standard Occupational Classification. Accessed September 27, 2023. https://www.bls.gov/soc/
U.S. Census Bureau. North American Industry Classification System. Accessed September 27, 2023. https://www.census.gov/naics/
U.S. NIOSH. Collecting and Using Industry and Occupation Data. Accessed November 11, 2023. https://www.cdc.gov/niosh/topics/coding/code.html
Prince SA, Reid RD, Bernick J, Clarke AE, Reed JL. Single versus multi-item self-assessment of sedentary behaviour: a comparison with objectively measured sedentary time in nurses. J Sci Med Sport. 2018;21(9):925–9. https://doi.org/10.1016/j.jsams.2018.01.018.
Peng G, Wang Y, Han G. Information technology and employment: the impact of job tasks and worker skills. J Ind Relat. 2018;60(2):201–23. https://doi.org/10.1177/0022185617741924.
Ráthonyi G, Kósa K, Bács Z, et al. Changes in workers’ physical activity and sedentary behavior during the COVID-19 pandemic. Sustainability. 2021;13(17):9524.
Wilms P, Schröder J, Reer R, Scheit L. The impact of "Home Office" work on physical activity and sedentary behavior during the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. 2022;19(19)https://doi.org/10.3390/ijerph191912344
Tomonaga R, Watanabe Y, Jiang Y, Nakagawa T, Yamato H. Comparison of physical activity and sedentary behavior between work-in-office and work-from-home: a self-controlled study. Journal of Occupational and Environmental Medicine. 9900:https://doi.org/10.1097/JOM.0000000000003061. https://doi.org/10.1097/jom.0000000000003061
Brusaca LA, Hallman DM, Januario LB, Gupta N, Oliveira AB, Mathiassen SE. Working at the office or from home during the COVID-19 pandemic: a cross-sectional study of temporal patterns of sitting and non-sitting among normal-weight and overweight Brazilian office workers. J Act Sedentary Sleep Behav. 2023;2(1):28. https://doi.org/10.1186/s44167-023-00038-0.
Falk GE, Mailey EL, Okut H, et al. Effects of sedentary behavior interventions on mental well-being and work performance while working from home during the COVID-19 pandemic: a pilot randomized controlled trial. Int J Environ Res Public Health. 2022;19(11)https://doi.org/10.3390/ijerph19116401
U.S. CDC. 2013-2014 Examination Data - Continuous NHANES. Accessed September 27, 2023. https://wwwn.cdc.gov/nchs/data/nhanes/2013-2014/manuals/2014-Physicial-Activity-Monitor-Procedures-Manual-508.pdf
Liu F, Wanigatunga AA, Schrack JA. Assessment of physical activity in adults using wrist accelerometers. Epidemiol Rev. 2022;43(1):65–93. https://doi.org/10.1093/epirev/mxab004.
Acknowledgements
The authors express their thanks to Mr. Jon Mann, Academic Specialist, University of Illinois at Chicago, for his editorial contributions to the paper, and to Dr. Richard Neitzel, the Director for Center for Occupational Health and Safety Engineering, University of Michigan (UM), for his valuable insights in defining the terminologies used. Also, we appreciate Ms. Kate Saylor, a health sciences informationist at UM, for her help in building the rigorous search terms in each database.
Funding
This study was supported by the first author (SP)’s research fund from the start-up fund from the School of Nursing, University of Michigan. KW was supported by NIH T32 NR018407.
Author information
Authors and Affiliations
Contributions
SP and JL conceptualized and designed the study. SP, SL, SW, and KW participated in the data screening procedure. SP, SL, and SW conducted the risk of bias. SP, KW, and PV were participated in the meta-analysis procedure. SP drafted the manuscript under the guidance of JL. SP prepared all figures and supplementary files. All authors contributed to reviewing the manuscript and editing the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Park, S., Lee, S., Woo, S. et al. Sedentary behaviors and physical activity of the working population measured by accelerometry: a systematic review and meta-analysis. BMC Public Health 24, 2123 (2024). https://doi.org/10.1186/s12889-024-19449-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19449-y