Abstract
Background
The combined association of physical activity (PA) and alcohol use (AU) with long-term mortality is yet to be investigated.
Methods
For the current study, 12,621 participants aged ≥ 20 years were enrolled from the National Health and Nutrition Examination Survey (1999–2004). The study endpoint was all-cause mortality. Cox proportional hazards regression models were used to examine the combined effect of PA and AU on long-term mortality.
Results
The study population was divided into young (< 60 years, N = 8,258) and old (≥ 60 years, N = 4,363) groups. The median follow-up time was 203 months. In both young and old group, sedentary lifestyle combined with even minimal AU were associated with elevated risk of death (all P < 0.05). In young group, the integration of high volume AU with any degree of PA, including sedentary PA (HR = 2.35, 95% CI 1.24–4.44, P = 0.009), low PA (HR = 1.64, 95% CI 1.01–2.68, P = 0.047), and moderate-to-vigorous PA (HR = 1.99, 95% CI 1.03–3.84, P = 0.041), was associated with an increased risk of mortality. This relationship persisted as significant after adjusting for potential confounders (all P < 0.05). In old group, combining moderate-to-vigorous PA and low volume AU (HR = 0.59, 95% CI 0.37–0.94, P = 0.027) was associated with a reduction in mortality. After adjustment, the combination of moderate-to-vigorous PA and low volume AU was independently associated with favorable prognostic outcomes (all P < 0.05).
Conclusions
In both age groups, combining sedentary lifestyle with even minimal AU was a risk factor for death. In young group, combining any level of PA with high volume AU was associated with increased mortality. In old group, combining moderate-to-vigorous PA with low volume AU was related to reduced mortality.
Similar content being viewed by others
Background
Modifiable lifestyle factors are closely associated with life expectancy and the incidence of chronic disease [1,2,3]. Advocating for a combination of healthy lifestyle factors is a fundamental aspect of public health strategies aimed at minimizing early mortality [4]. Physical activity (PA) intensity is correlated with better outcomes. Engaging in regular exercise that meets or surpasses the current PA guidelines is linked to a reduced risk of all-cause mortality [5,6,7,8]. Alcohol use (AU), on the other hand, exhibited a J-shaped curve in its association with adverse clinical outcomes [9,10,11].
The behavior of PA and AU are positively correlated, suggesting that higher levels of PA are often associated with greater AU, and vice versa. Physically active individuals that engage in problematic drinking might appear “healthy”, masking alcohol-related issues and precipitating future personal and societal risks [12]. Previous research has examined the interplay between PA and AU, concentrating primarily on AU’s impact on exercise performance [13,14,15], and the influence of exercise on alcohol dependency and various mental health disorders [16,17,18,19]. However, the combined effect of PA and AU on clinical outcomes is yet unknown. Besides, age-stratified analysis is necessary, given the significantly different mortality risks faced by young and old populations [20, 21]. Therefore, this study was designed to explore the combined association of PA and AU on long-term, all-cause mortality, with a novel stratification by age groups.
Methods
Study design and population
The National Health and Nutrition Examination Survey (NHANES) is a program conducted every 2 years and employs a complex, multistage probability sampling design to select participants representative of the civilian, non-institutionalized population of the United States to assess the health and nutritional status of adults and children. Sample weights are assigned to all NHANES participants, accounting for the probability of selection, nonresponse adjustments, and post-stratification adjustments. NHANES is conducted by the Centers for Disease Control and Prevention and the National Center for Health Statistics (NCHS). The NCHS Research Ethics Review Committee reviewed and approved the NHANES study protocol.
For the current study, data from three cycles, 1999–2000, 2001–2002, and 2003–2004, were merged (available at: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx). For the 1999–2000 and 2001–2002 cycle, the dietary day one 4-year sample weight was applied. For the 2003–2004 cycle, the dietary day one sample weight was applied. There were 31,126 participants in NHANES 1999–2004. After excluding age < 20 years (N = 15,794), missing questionnaire data of PA (N = 5), missing dietary data of AU (N = 1,886), missing questionnaire data of education (N = 6), missing questionnaire data of marital status (N = 543), missing questionnaire data of smoking (N = 8), and missing examination data of body mass index (BMI, N = 1,621), 12,621 participants were included in the final analysis (Fig. 1).
Data collection and definition
Demographic data were extracted including age, sex, race, education, marital status, and smoking status. In addition, examination and laboratory data were extracted including height, weight, BMI, systolic and diastolic blood pressure, white blood cell count, hemoglobin, lymphocyte count, platelet count, high-density and low-density lipoprotein cholesterol, total cholesterol, serum creatinine, total bilirubin, albumin, and glycohemoglobin. Furthermore, questionnaire data were extracted including PA, and past medical history of congestive heart failure, coronary heart disease, angina, myocardial infarction, stroke, cancer, hypertension, hypercholesterolemia, diabetes mellitus, and chronic kidney disease. Eventually, dietary data were extracted including AU.
The participants’ daily PA levels were classified as sedentary, low, moderate, or vigorous according to the questionnaire data. Participants were assumed to have a sedentary life if they sat during the day and did not walk about very much. Participants were assumed to have low PA if they walked a lot during the day but did not carry or lift things very often. Participants were assumed to have moderate PA if they lifted light loads or climbed stairs or hills often. Participants were assumed to have vigorous PA if they did heavy work or carried heavy loads.
The participants’ AU levels were classified based on the dietary intake of alcohol per day. Occasional drinkers had < 1.3 g AU, low-volume drinkers had 1.3–24.0 g AU, medium-volume drinkers had 25.0–44.0 g AU, and high-volume drinkers had ≥ 45.0 g AU [11].
Follow-up and study endpoints
The NHANES participants were followed up for mortality until 31 December 2019. The follow-up time was calculated using person months from the date of interview to the date of death or the end of the follow-up period. The median follow-up time was 203 months (or ~ 16.9 years). The endpoint of the current study was all-cause mortality. Death data were extracted from public-use linked mortality files in the NHANES database (available at: https://www.cdc.gov/nchs/data-linkage/mortality-public.htm).
Statistical analysis
All statistical analyses were conducted in accordance with guidelines from the Centers for Disease Control and Prevention (available at: https://wwwn.cdc.gov/nchs/nhanes/tutorials/default.aspx). Sample weights were assigned to participants as recommended by NCHS. The baseline characteristics of the study population are presented as weighted samples. The continuous variables are presented as weighted mean (standard deviation). The categorial variables are presented as unweighted number (survey-weighted percentages).
The study population was categorized into young (< 60 years) and old (≥ 60 years) groups, and the baseline characteristics of each group were subclassified by PA and AU levels. The continuous variables were compared using the weighted linear regression models and the categorial variables were compared using the weighted chi-square tests. Bar charts were used to show all-cause mortality per 100,000 person-years in various levels of PA and AU combinations. Univariate Cox proportional hazard regression analysis was conducted to explore the potential risk factors for all-cause mortality. Possible confounding factors (age, race, education, marital status, BMI, smoking status, congestive heart failure, myocardial infarction, stroke, cancer, hypertension, hypercholesterolemia, and diabetes mellitus) were incorporated into multivariate Cox proportional hazard regression models to evaluate the independent effect of PA and AU on all-cause mortality, as well as the combined association of PA and AU with all-cause mortality. The selection of confounding factors was based on clinical relevance and the univariate association with outcomes. Statistical data were analyzed using R statistical software version 4.3.1. Two-tailed P values < 0.05 were considered statistically significant.
Results
Baseline characteristics for total population
Overall, 12,621 participants were included in this study. The baseline clinical characteristics of the weighted samples are displayed in Table 1. Generally, the mean age of weighted sample was 46.17 (16.96) years, and 48.0% were male. The median BMI was 28.14 (6.36) kg/m2. Non-Hispanic white participants accounted for the majority (72.2%) of the population, followed by participants who were non-Hispanic black (10.8%), Mexican American (7.3%), other Hispanic (5.1%), and other races (4.5%). In terms of education and marital status, 53.9% of the participants had attained an education level beyond high school, and 57.5% of the participants reported being married. Never smokers comprised 50.0% of the population, former smokers accounted for 25.6%, and current smokers made up 24.4%. About half of the participants had a low daily PA and occasional AU.
The study population was divided into young (< 60 years, N = 8,258) and old (≥ 60 years, N = 4,363) groups (Fig. 1). Relative to the younger group, the older group exhibited a higher prevalence of chronic diseases, and reduced engagement in moderate-to-vigorous PA and medium-to-high AU.
The baseline characteristics of young and old group by PA and AU levels were presented in Supplementary Tables 1–4. For different PA levels, both young and old participants with moderate-to-vigorous PA tended to be male, had higher proportion of high volume AU, lower proportion of chronic medical disease, lower BMI and glycohemoglobin (all P < 0.05). For different AU levels, both young and old participants with high volume AU tended to be male, had higher proportion of current smoker, never married and divorced. (all P < 0.05).
The association between PA and AU with all-cause mortality for age < 60 years
For the younger participants, there were no significant difference for the all-cause mortality per 100,000 person-years among AU levels (P for trend in PA = 0.163, P for trend in AU = 0.109; Fig. 2).
The Cox regression analyses between PA and AU with all-cause mortality for age < 60 years were summarized in Table 2.
Univariate Cox regression analyses showed that low PA (hazard ratio [HR] = 0.53, 95% confidence interval [CI] 0.42–0.66, P < 0.001), and moderate-to-vigorous PA (HR = 0.54, 95% CI 0.41–0.72, P < 0.001) acted as protective factors for mortality, while high-volume AU was a risk factor for mortality (HR = 1.45, 95% CI 1.10–1.93, P = 0.010. After adjustment for possible confounding factors, the correlation remained significant (all P < 0.05).
The integration of high volume AU with any degree of PA, including sedentary PA (HR = 2.35, 95% CI 1.24–4.44, P = 0.009), low PA (HR = 1.64, 95% CI 1.01–2.68, P = 0.047), and moderate-to-vigorous PA (HR = 1.99, 95% CI 1.03–3.84, P = 0.041), was associated with an increased risk of mortality. This relationship persisted as significant after adjusting for potential confounders (all P < 0.05). Additionally, occasional AU (HR = 2.07, 95% CI 1.42–3.03, P < 0.001) or medium volume AU (HR = 2.57, 95% CI 1.14–5.79, P = 0.023), when combined with sedentary lifestyle was also associated with increased mortality risk. After adjustment of possible confounding factors, the association remained significant (all P < 0.05).
The association between PA and AU with all-cause mortality for age ≥ 60 years
For the older participants, the all-cause mortality per 100,000 person-years varied significantly among different PA levels, but no significant difference among different AU levels (P for trend in PA = 0.013, P for trend in AU = 0.246; Fig. 2).
The Cox regression analyses between PA and AU with all-cause mortality for age ≥ 60 years were summarized in Table 3.
Similar to young participants, maintaining physically active lifestyle, including low PA (HR = 0.57, 95% CI 0.51–0.64, P < 0.001), and moderate-to-vigorous PA (HR = 0.52, 95% CI 0.45–0.61, P < 0.001), was correlated with lower death risk in old population. After adjustment, the beneficial effect for prognosis remained significant (P < 0.05). In regards to alcohol consumption, low volume AU were related to lower risk of death (HR = 0.81, 95% CI 0.68–0.97, P = 0.020). The significance of this relationship dissipated after adjusting for confounders, including demographic variables and medical conditions (P > 0.05).
In addition, the combination of a sedentary lifestyle with either occasional AU (HR = 1.83, 95% CI 1.54–2.18, P < 0.001), or low AU (HR = 1.91, 95% CI 1.38–2.64, P < 0.001) was associated with an increased risk of mortality in old people, which remained significant after adjustment (P < 0.05). Finally, it is noteworthy that, combining moderate-to-vigorous PA and low volume AU (HR = 0.59, 95% CI 0.37–0.94, P = 0.027) in old participants was associated with a reduction in mortality. After adjustment, the combination of moderate-to-vigorous PA and low volume AU was independently associated with favorable prognostic outcomes (all P < 0.05).
Discussion
Physically active individuals report higher frequency and quantity of alcohol consumption [12]. Dodge et al. conducted a systemic review on the relationship between PA and AU among adults in the United States and concluded that they were positively correlated [22]. Studying the combined effects of PA and AU is crucial for understanding their influence on long-term mortality and providing evidence for public health promotion that targets PA and AU, but research in this field is scarce. To the best of our knowledge, this study is the first to explore the combined association of PA and AU with long-term mortality. The major findings of our study revealed that, across both young and old populations, being physically active consistently contributed to positive health outcomes. A sedentary lifestyle combined with even low levels of AU was associated with higher mortality risk. Specifically, among young adults, the combination of any level of PA with high volume AU was linked to unfavorable outcomes. For old participants, engaging in moderate-to-vigorous PA while low volume AU emerged as a beneficial practice.
The effect of PA on mortality
The current PA guidelines for young and old populations are similar. They recommend at least 150–300 min per week of moderate PA, or at least 75–150 min per week of vigorous PA, or an equivalent combination of both [5,6,7, 23]. An inverse curvilinear dose–response relationship is observed between weekly PA level and the reduction of mortality risk [24]. A prospective cohort study conducted by Lee et al. demonstrated a 19% risk reduction for all-cause mortality for participants with vigorous PA, and a 20% risk reduction for those with moderate PA, over a median follow-up of 26 years [25]. Consistent with previous studies, our study found that PA, even at low level, correlated with decreased long-term all-cause mortality, with adjustments for confounders.
The effect of AU on mortality
Recommendations for alcohol consumption have not reached a consensus opinion. Evidence from observational and prospective studies have consistently shown a lower risk of mortality in people with low-volume AU when compared with abstainers or individuals with high volume AU, in a J-shaped curve relationship [26,27,28,29]. First, compared with high volume AU, low-to-medium volume AU may prevent the development of heart failure [30, 31], coronary artery disease, myocardial infarction, peripheral arterial disease, and stroke [32]. Second, high volume AU is associated with chronic liver disease [33], atrial fibrillation [34], dilated cardiomyopathy [35], and cancer [36, 37]. However, the threshold at which the volume of AU shifts from being beneficial to detrimental for health is not clearly defined [38]. Additionally, many confounding factors could affect the relationship between AU and outcomes. A meta-analysis showed a non-significant reduction in mortality risk in people with low-volume AU, probably because of the abstainer bias, that is to say, the abstainers with whom they were compared quitted drinking because of pre-existing medical conditions caused by prior high volume AU [39, 40]. In our study, low volume AU was associated with survival benefit; however, after adjustment, the beneficial effect disappeared.
The combined association of PA and AU with mortality
Our results demonstrated a lower mortality risk for old participants who had moderate-to-vigorous PA and low volume AU, and a higher mortality risk for young participants who had moderate-to-vigorous PA and high volume AU. The underlying mechanism is yet unclear, but several possible explanations exist.
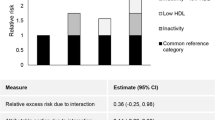
Firstly, exercise benefits clinical outcomes irrespective of traditional risk factors. Regular exercise facilitates cardiac parasympathetic regulation, generates a healthy anti-inflammatory environment, increases circulating angiogenic cells, and protects the gut barrier [41]. By contrast, sarcopenia, defined as the loss of muscle strength, mass, and function, is related to a higher risk of mortality, falls, and compromised quality of life [42]. Secondly, low volume AU can contribute to an increase in high-density lipoprotein, fibrinolysis, and endothelial function, and a decrease in platelet aggregation and plasma viscosity [26, 43]. These factors might account for the net decrease in mortality risk observed in old participants when moderate-to-vigorous PA and low volume AU were combined.
Nevertheless, we saw an increased risk of mortality in young participants when moderate-to-vigorous PA was combined with high volume AU. The equilibrium of skeletal muscle protein synthesis and degradation is partially regulated by the rapamycin complex 1 (mTORC1) signaling pathway [44, 45]. Alcohol and exercise could independently influence this pathway, but in opposite directions; that is, alcohol generally has a suppressive effect on this pathway and causes muscle losses, while exercise has a stimulatory effect and leads to muscle gains [15, 46,47,48]. Therefore, the harmful effect of chronic high volume AU might initially antagonize and gradually override the beneficial effect associated with regular exercise, such as increases in mTORC1 pathway signaling, gains in muscle size and decrease in long term mortality [14].
Our study had several limitations. First, this study was an observational cohort study. Though multivariate hazard regression models were used, residual confounding factors may exist. Randomized controlled trials are required to testify our results. Second, the evaluation of PA and AU was not comprehensive because of limited variables. Future studies could involve information on the intensity and type of PA, or the timing and frequency of AU. Third, while our study revealed the combined effect of PA and AU on mortality, the underlying biological process driving the association are as yet unknown. Further experimental studies are necessary to elucidate the mechanisms.
Conclusions
As compared to sedentary lifestyle, being physically active decreases mortality in both young and old populations. Combining sedentary lifestyle with even minimal alcohol consumption correlated with elevated risk of death. In young group, combining any level of PA with high volume AU was associated with increased mortality. In old group, combining moderate-to-vigorous PA with low volume AU was related to reduced mortality. These findings demonstrated the possible relationships between different levels of PA and AU and long-term mortality, which may provide guidance for public health promotion strategies that target PA and AU.
Data availability
The NHANES datasets are available online at: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx. Death data were extracted from public-use linked mortality files in the NHANSE database, which is available at: https://www.cdc.gov/nchs/data-linkage/mortality-public.htm.
Abbreviations
- PA:
-
Physical activity
- AU:
-
Alcohol use
- BMI:
-
Body mass index
- mTORC1:
-
Rapamycin complex 1
- HR:
-
Hazard ratio
- CI:
-
Confidential interval
References
Chudasama YV, Khunti K, Gillies CL, Dhalwani NN, Davies MJ, Yates T, et al. Healthy lifestyle and life expectancy in people with multimorbidity in the UK Biobank: a longitudinal cohort study. PLoS Med. 2020;17(9):e1003332.
Li Y, Schoufour J, Wang DD, Dhana K, Pan A, Liu X, et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ. 2020;368:l6669.
Li Y, Pan A, Wang DD, Liu X, Dhana K, Franco OH, et al. Impact of healthy lifestyle factors on life expectancies in the US Population. Circulation. 2018;138(4):345–55.
Li K, Husing A, Kaaks R. Lifestyle risk factors and residual life expectancy at age 40: a German cohort study. BMC Med. 2014;12:59.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62.
Tucker WJ, Fegers-Wustrow I, Halle M, Haykowsky MJ, Chung EH, Kovacic JC. Exercise for primary and secondary Prevention of Cardiovascular Disease: JACC Focus Seminar 1/4. J Am Coll Cardiol. 2022;80(11):1091–106.
Piercy KL, Troiano RP, Ballard RM, Carlson SA, Fulton JE, Galuska DA, et al. The physical activity guidelines for americans. JAMA. 2018;320(19):2020–8.
Moore SC, Patel AV, Matthews CE, Berrington de Gonzalez A, Park Y, Katki HA, et al. Leisure time physical activity of moderate to vigorous intensity and mortality: a large pooled cohort analysis. PLoS Med. 2012;9(11):e1001335.
Moissl AP, Delgado GE, Kramer BK, Dawczynski C, Stojakovic T, Marz W, et al. Alcohol consumption and mortality: the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Atherosclerosis. 2021;335:119–25.
Ronksley PE, Brien SE, Turner BJ, Mukamal KJ, Ghali WA. Association of Alcohol Consumption with selected cardiovascular disease outcomes: a systematic review and meta-analysis. BMJ. 2011;342:d671.
Zhao J, Stockwell T, Naimi T, Churchill S, Clay J, Sherk A. Association between Daily Alcohol Intake and Risk of all-cause mortality: a systematic review and Meta-analyses. JAMA Netw Open. 2023;6(3):e236185.
French MT, Popovici I, Maclean JC. Do alcohol consumers exercise more? Findings from a national survey. Am J Health Promot. 2009;24(1):2–10.
Wynne JL, Wilson PB. Got Beer? A systematic review of Beer and Exercise. Int J Sport Nutr Exerc Metab. 2021;31(5):438–50.
Levitt DE, Luk HY, Vingren JL, Alcohol. Resistance Exercise, and mTOR pathway signaling: an evidence-based narrative review. Biomolecules. 2022;13(1).
Duplanty AA, Budnar RG, Luk HY, Levitt DE, Hill DW, McFarlin BK, et al. Effect of Acute Alcohol Ingestion on Resistance Exercise-Induced mTORC1 Signaling in Human muscle. J Strength Cond Res. 2017;31(1):54–61.
Leasure JL, Neighbors C, Henderson CE, Young CM. Exercise and Alcohol Consumption: what we know, what we need to know, and why it is important. Front Psychiatry. 2015;6:156.
Ashdown-Franks G, Firth J, Carney R, Carvalho AF, Hallgren M, Koyanagi A, et al. Exercise as Medicine for Mental and Substance Use disorders: a Meta-review of the benefits for neuropsychiatric and cognitive outcomes. Sports Med. 2020;50(1):151–70.
Hallgren M, Vancampfort D, Hoang MT, Andersson V, Ekblom O, Andreasson S, et al. Effects of acute exercise on craving, mood and anxiety in non-treatment seeking adults with alcohol use disorder: an exploratory study. Drug Alcohol Depend. 2021;220:108506.
Gunillasdotter V, Andreasson S, Hallgren M, Jirwe M. Exercise as treatment for alcohol use disorder: a qualitative study. Drug Alcohol Rev. 2022;41(7):1642–52.
Collaborators GBDA. Population-level risks of alcohol consumption by amount, geography, age, sex, and year: a systematic analysis for the global burden of Disease Study 2020. Lancet. 2022;400(10347):185–235.
Angus C. Harms of alcohol in different age groups. BMJ. 2022;378:o1979.
Dodge T, Clarke P, Dwan R. The relationship between physical activity and alcohol use among adults in the United States. Am J Health Promot. 2017;31(2):97–108.
Izquierdo M, Merchant RA, Morley JE, Anker SD, Aprahamian I, Arai H, et al. International Exercise recommendations in older adults (ICFSR): Expert Consensus guidelines. J Nutr Health Aging. 2021;25(7):824–53.
Eijsvogels TM, Molossi S, Lee DC, Emery MS, Thompson PD. Exercise at the extremes: the amount of Exercise to Reduce Cardiovascular events. J Am Coll Cardiol. 2016;67(3):316–29.
Lee DH, Rezende LFM, Joh HK, Keum N, Ferrari G, Rey-Lopez JP, et al. Long-term leisure-time physical activity intensity and all-cause and cause-specific mortality: a prospective cohort of US adults. Circulation. 2022;146(7):523–34.
Fernandez-Sola J. Cardiovascular risks and benefits of moderate and heavy alcohol consumption. Nat Rev Cardiol. 2015;12(10):576–87.
Goel S, Sharma A, Garg A. Effect of Alcohol Consumption on Cardiovascular Health. Curr Cardiol Rep. 2018;20(4):19.
O’Keefe EL, DiNicolantonio JJ, O’Keefe JH, Lavie CJ. Alcohol and CV Health: Jekyll and Hyde J-Curves. Prog Cardiovasc Dis. 2018;61(1):68–75.
Xi B, Veeranki SP, Zhao M, Ma C, Yan Y, Mi J. Relationship of Alcohol Consumption to All-Cause, Cardiovascular, and Cancer-related mortality in U.S. adults. J Am Coll Cardiol. 2017;70(8):913–22.
Di Castelnuovo A, Costanzo S, Bonaccio M, Rago L, De Curtis A, Persichillo M, et al. Moderate alcohol consumption is Associated with Lower risk for heart failure but not atrial fibrillation. JACC Heart Fail. 2017;5(11):837–44.
Goncalves A, Claggett B, Jhund PS, Rosamond W, Deswal A, Aguilar D, et al. Alcohol consumption and risk of heart failure: the atherosclerosis risk in communities Study. Eur Heart J. 2015;36(15):939–45.
Bell S, Daskalopoulou M, Rapsomaniki E, George J, Britton A, Bobak M, et al. Association between clinically recorded alcohol consumption and initial presentation of 12 cardiovascular diseases: population based cohort study using linked health records. BMJ. 2017;356:j909.
Aberg F, Byrne CD, Pirola CJ, Mannisto V, Sookoian S. Alcohol consumption and metabolic syndrome: clinical and epidemiological impact on liver disease. J Hepatol. 2023;78(1):191–206.
Csengeri D, Sprunker NA, Di Castelnuovo A, Niiranen T, Vishram-Nielsen JK, Costanzo S, et al. Alcohol consumption, cardiac biomarkers, and risk of atrial fibrillation and adverse outcomes. Eur Heart J. 2021;42(12):1170–7.
Andersson C, Schou M, Gustafsson F, Torp-Pedersen C. Alcohol intake in patients with cardiomyopathy and heart failure: Consensus and controversy. Circ Heart Fail. 2022;15(8):e009459.
Rumgay H, Murphy N, Ferrari P, Soerjomataram I. Alcohol and Cancer: Epidemiology and Biological mechanisms. Nutrients. 2021;13(9).
Suter F, Pestoni G, Sych J, Rohrmann S, Braun J. Alcohol consumption: context and association with mortality in Switzerland. Eur J Nutr. 2023;62(3):1331–44.
Day E, Rudd JHF. Alcohol use disorders and the heart. Addiction. 2019;114(9):1670–8.
Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T. Do moderate drinkers have reduced mortality risk? A systematic review and Meta-analysis of Alcohol Consumption and all-cause mortality. J Stud Alcohol Drugs. 2016;77(2):185–98.
Krittanawong C, Isath A, Rosenson RS, Khawaja M, Wang Z, Fogg SE, et al. Alcohol Consumption and Cardiovascular Health. Am J Med. 2022;135(10):1213–30. e3.
Fiuza-Luces C, Santos-Lozano A, Joyner M, Carrera-Bastos P, Picazo O, Zugaza JL, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat Rev Cardiol. 2018;15(12):731–43.
Damluji AA, Alfaraidhy M, AlHajri N, Rohant NN, Kumar M, Al Malouf C, et al. Sarcopenia Cardiovasc Dis Circulation. 2023;147(20):1534–53.
Piano MR. Alcohol’s effects on the Cardiovascular System. Alcohol Res. 2017;38(2):219–41.
Bodine SC, Stitt TN, Gonzalez M, Kline WO, Stover GL, Bauerlein R, et al. Akt/mTOR pathway is a crucial regulator of skeletal muscle hypertrophy and can prevent muscle atrophy in vivo. Nat Cell Biol. 2001;3(11):1014–9.
Drummond MJ, Fry CS, Glynn EL, Dreyer HC, Dhanani S, Timmerman KL, et al. Rapamycin administration in humans blocks the contraction-induced increase in skeletal muscle protein synthesis. J Physiol. 2009;587(Pt 7):1535–46.
Parr EB, Camera DM, Areta JL, Burke LM, Phillips SM, Hawley JA, et al. Alcohol ingestion impairs maximal post-exercise rates of myofibrillar protein synthesis following a single bout of concurrent training. PLoS ONE. 2014;9(2):e88384.
Steiner JL, Lang CH. Alcohol impairs skeletal muscle protein synthesis and mTOR signaling in a time-dependent manner following electrically stimulated muscle contraction. J Appl Physiol (1985). 2014;117(10):1170–9.
Steiner JL, Lang CH. Alcohol intoxication following muscle contraction in mice decreases muscle protein synthesis but not mTOR signal transduction. Alcohol Clin Exp Res. 2015;39(1):1–10.
Acknowledgements
The authors thank to all of the NHANES participants who gave freely of their time to make this and other studies possible.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
BQF and WH were involved in designing the study. Data collection and cleaning were carried out by BQF, YY, SJC, HH, TXL, JWY, CC, MG, and HXN. The statistical analysis was conducted by BQF and YY. BQF drafted the manuscript. All authors reviewed, revised, and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The NHANES is conducted by the Centers for Disease Control and Prevention and the National Center for Health Statistics (NCHS). The NCHS Research Ethics Review Committee reviewed and approved the NHANES study protocol. All participants signed written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fu, B., Yu, Y., Cheng, S. et al. The combined association of physical activity and alcohol use with long-term mortality: an age-stratified analysis. BMC Public Health 24, 1817 (2024). https://doi.org/10.1186/s12889-024-19326-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19326-8