Abstract
Background
Hookworm infection and schistosomiasis are two of sub-Saharan Africa's most common neglected tropical diseases. An annual mass drug administration (MDA) program against schistosomiasis and soil-transmitted helminths (STHs), including hookworm, has been implemented in Mayuge district, Uganda, since 2003 to date. However, hookworm and schistosomiasis remain prevalent in Mayuge district. Understanding the factors that predispose children to these infections in the context of MDA could inform interventions to reduce prevalence in Uganda and similar settings.
Method
This cross-sectional study took place in 33 randomly selected primary schools in the Mayuge district from January to February 2022. Children in primary classes 4 or 5, in the selected schools provided single stool samples and completed questionnaires. Stool specimens were examined using the Kato-Katz method to determine the prevalence of hookworm and schistosomiasis. We performed univariable and multivariable logistic regression to assess the associations of each infection with potential risk factors.
Result
A total of 1,617 students (mean age 12.1 years, 50.1% male) were enrolled. The prevalence of hookworm infection and schistosomiasis was 21.8% (95% confidence interval (CI): 19.8–23.9%) and 18.7% (95% CI: 16.8–20.7%), respectively. In multivariable analysis, longer water fetching time (over 30 min versus less than 30 min) and working daily in the soil were associated with increased odds of hookworm infection (adjusted odds ratio (AOR): 1.49, 95% CI: 1.13–1.96 and 1.37, 95% CI: 1.03–1.82, respectively). Higher odds of schistosomiasis were linked to proximity to water bodies within a one-hour walking distance (AOR: 1.84, 95% CI: 1.35–2.50), and not always washing hands before eating (AOR: 2.00, 95% CI: 1.50–2.67). Swimming, bathing, or washing in water bodies twice a week, compared to never, also increased schistosomiasis odds (AOR: 2.91, 95% CI: 1.66–5.13).
Conclusion
Consistent with the mechanisms of acquisition, hookworm infection increased with exposure to soil, and schistosomiasis increased with exposure to unclean water. Our findings highlight the importance of Water, Sanitation, and Hygiene programs and strategies aimed at reducing exposure within the framework of Neglected Tropical Disease elimination programs.
Similar content being viewed by others
Background
Hookworm is the commonest soil-transmitted helminth (STH), affecting 500 million people globally [1] and contributing to an estimated 4 million Disability-Adjusted Life Years (DALYs) worldwide annually [2]. Schistosomiasis affects more than 250 million people worldwide, with approximately 800 million, mainly children, being at risk [3, 4]. Schistosomiasis is associated with 1.4 million lost DALYs annually and with 280,000 deaths per year globally [5].
Adult hookworms residing in the host's gastrointestinal tract instigate blood loss, thereby giving rise to iron-deficiency anaemia and hookworm disease. Consequently, the severity of blood loss is directly proportional to the worm burden [6]. Persistent and chronic blood loss resulting from hookworm infection can contribute to long-term health consequences, manifesting as growth retardation, and mental and cognitive impairment [7, 8]. Also, hookworm infection in pregnant women can lead to adverse birth outcomes, including reduced birth weight and increased infant mortality rates [7, 9, 10]. Schistosoma mansoni infection causes intestinal schistosomiasis, producing severe sequelae such as hepatosplenomegaly with periportal liver fibrosis and portal hypertension, which progress from abdominal pain and bloody diarrhoea [11, 12]. Urogenital schistosomiasis caused by Schistosoma haematobium leads to haematuria, dysuria, hydronephrosis, female genital schistosomiasis and calcification of the bladder [13].
Hookworm infection and schistosomiasis are the two most common neglected tropical diseases (NTDs) in sub-Saharan Africa [14]. While not causing immediate fatal outcomes, these NTDs give rise to persistent and chronic health burdens that together contribute to combined DALYs due to hookworm and schistosomiasis higher than that of HIV/AIDS or malaria [3].
In Uganda, the estimated nationwide prevalence of hookworm infection and schistosomiasis is 7.7% and 25.6% respectively [15, 16], but schistosomiasis, as a consequence of Schistosoma mansoni infection, in particular is highly focal, over a third of the population are affected in several Ugandan districts [16]. Mayuge district is one such area and as a consequence of the high prevalence in this district, an annual mass drug administration (MDA) program against STH and schistosomiasis targeting school-aged children has been implemented since 2003. In addition, World Vision, funded by Korea International Cooperation Agency (KOICA), implemented the Mayuge NTDs Elimination (MANE) project between 2019 and 2022, a comprehensive NTD elimination program targeting STHs and schistosomiasis in Mayuge district. The MANE project involved annual MDA, water, sanitation and hygiene (WASH), and awareness increasing programs for community members and health workers.
In the MANE baseline survey, a total of 1,123 school-aged children (SAC) were enrolled in July 2019, the prevalence of hookworm and Schistosoma mansoni infection was 15.1% and 27.2% respectively, whereas other STHs were less than 1% [17]. The cure rate (CR) for hookworm by single-dose albendazole was approximately 78% [18] and CR for schistosomiasis by standard praziquantel (PZQ) dose of 40 mg/kg was over 70% [19], and there has been high program coverage of MDA for STH (77%, 81%, and 75% in 2012, 2014, and 2016 respectively) and for schistosomiasis (85%, 65%, and 72% in 2012, 2014, and 2016), respectively. As such, the continued burden of hookworm and Schistosoma mansoni in Mayuge district suggests that important gaps exist which are weakening the effectiveness of the MDA campaigns. One possible explanation for persistently high prevalence is re-infection among treated people. Several risk factors for hookworm [20,21,22,23,24,25] and schistosomiasis [26,27,28] infection/re-infection have been identified. These include gender, age, temperature, raising animals, WASH, exposure to contaminated environment, and lack of knowledge of parasitic infections. However, studies have presented conflicting results regarding risk factors for hookworm and schistosomiasis. There is also a lack of data in the context of MDA. This study sought to investigate whether hookworm and schistosomiasis are still prevalent in the context of > 15 years of an annual MDA program and additional NTD elimination programs, and to determine risk factors for prevalent infections.
Methods
Study area
This study was conducted in Mayuge district located in south-eastern Uganda, next to the shores of Lake Victoria and 146 km from Uganda’s capital, Kampala. Mayuge district has 14 sub-counties, including five lakeshore sub-counties: Bukabooli, Bukatube, Malongo, Wairasa, and Jaguzi. In a census conducted in 2020, as part of the MANE project, Mayuge’s population was 509,118, with 95,418 children under five and 156,182 children between five and 14 years old. As of January 2022, there were 504 primary schools, 41 health centres and one hospital.
Study design and population
This was a cross-sectional study involving SAC from randomly selected primary schools in Mayuge district. A two-stage random sampling technique was used. In the first stage, the 504 schools in Mayuge district were listed by sub-county, and 33 were selected using probability proportional to size (PPS) [29], so that each school in a larger sub-county had a higher probability of selection, and each school in a smaller sub-county a lower probability of selection.
In the second stage, within each selected school, a class (40–50 children) was selected among the primary four and five classes (targeting nine to ten-year-old schoolchildren) using a table of random numbers. If only one class of this age group was present, that class was selected by default. All children in the selected classes were eligible for inclusion. Information about the study was provided to children and their parents/guardians in the local language, with the information for children adapted to ensure understanding. Children who signed the child assent form and whose parents/guardian provided written informed consent were included.
Sample size
Sample size determination for the survey was based on the comparison of the prevalence of STH and schistosomiasis in Mayuge district in 2019 with the anticipated prevalence of STH and schistosomiasis after three years of project implementation. The baseline prevalence of STHs in 2019 was 15.8%, and it was anticipated that MANE program activities would reduce the prevalence of STHs to 12% by the time of the 2022 survey. For schistosomiasis, the prevalence was 27.2% in 2019, and it was estimated that MANE program activities would reduce schistosomiasis prevalence to 18% by the time of the 2022 survey.
Assuming the above changes in prevalence, a target sample size for the 2022 prevalence survey of at least 1,300 participants would be required for 80% power to detect a difference between 2019 and 2022 STH prevalence at 5% significance level. Assuming that each class contained at least 40 children, the number of selected schools (n = 33) was chosen in order to achieve the required sample size..
Data collection and laboratory procedures
Field workers performing stool sample collection and survey questionnaires (supplementary file 1) were comprehensively trained before data collection, with training for standardised approaches to obtaining informed consent and assent, interviewing techniques, recording of responses, probing, and data handling/management. The research questionnaires were pre-tested and amended accordingly if necessary. Laboratory staff working at the public health centres in Mayuge district participated as field workers. Two field workers visited each school and conducted survey questionnaires with enrolled participants, entering data on assigned mobile phones.
The lead field worker cross-checked the completed questionnaires and wrote notes at the end of each day to ensure that all relevant questions had been asked and the responses adequately recorded. Field workers used mobile phones to record the data through the KoBoToolbox system and automatically saved and stored the data in the system when completing the questionnaire. The designated MANE project staff ensured appropriate supervision of the entire data collection process.
Each child was given a pre-labelled sterile stool container to collect a single stool sample and these were collected on the same day as the questionnaires were completed. These containers were then securely stored in cool boxes, which field workers transported to the district central laboratory at Kigandalo Health Centre IV, where the Kato-Katz examination method was employed [30]. Within 24 h of arrival at the laboratory, two slides were prepared from each stool sample. In cases where stool samples were not examined with the Kato-Katz method on the same day they were received, they were kept refrigerated at 4 °C overnight for examination the next day.
Examiners from the Vector-borne and Neglected Tropical Diseases Control Division (VCD) within the Ministry of Health of Uganda examined the prepared slides. Furthermore, a supervisor from the VCD double-checked 5% of the slides to confirm the accuracy and reliability of the results obtained from the initial examination.
Potential risk factors
The following data on sociodemographic, lifestyle and environmental characteristics collected with the questionnaire were assessed as potential risk factors of interest: age, sex, location of school, household assets, type of latrine, open defecation (i.e. defecation in open fields/bush land etc.), water source for drinking, water source for other purposes (i.e. other than for drinking, such as bathing and washing clothes), water fetching time (time taken for round trip to water source from household: ≤ 30 min or > 30 min), household water facilities, hand-washing behaviour, soil contact, history of anthelminthic treatment, distance to and frequency of contact with freshwater, and knowledge of how hookworm and schistosomiasis can be acquired.
Participants’ school location was categorised into two groups: those who attended a school in a lakeshore sub-county and those who attended school in a non-lakeshore sub-county.
For water source variables, piped water connected to the dwelling or within the compound, piped water to neighbours, piped water to public places, boreholes, tube wells, protected dug wells, and protected springs were considered improved water sources. Unprotected dug wells, unprotected springs, lake water, river water, rainwater and unidentified water sources were considered unimproved. We categorised rainwater as a not-improved water source because rainwater in Mayuge district is usually harvested through gutters attached to roofs and house walls and exposed to contaminated soil.
For household assets, study participants were asked about types of home ownership and the possession of various household amenities, including cars, motorbikes, mobile phones, televisions, radios, access to electricity, and the availability of latrine facilities. We categorised participants into three groups based on their household assets: the "low" category was assigned to those with up to three household assets, the "moderate" category included those with four to five household assets, and the "high" category encompassed individuals with six to eight household assets.
Statistical analysis
Data saved in the KoBoToolbox system were exported into Microsoft Office Excel, and checked for errors, missing values, and extreme values. The cleaned data were exported to Stata SE version 18.0 (Stata Corp; College Station, TX, USA) for statistical analysis.
The prevalence of STHs and schistosomiasis with a 95% confidence interval (CI) was calculated. The arithmetic egg count was obtained through the microscopic examination of slides prepared by applying the Kato-Katz method. A multiplication factor of 24 was applied to calculate eggs per gram since the stool quantity in a slide prepared with the Kato-Katz method contains 41.7 mg of stool (24 × 41.7 mg ≈ 1 g). The intensity of infection was categorised according to WHO guidelines [31].
The chi-square (χ2) test or Fisher’s exact test was applied to assess associations between categorical variables and the presence versus absence of hookworm infection and schistosomiasis. χ2 test for trend was used for evaluating associations with ordered categorical variables. Univariable logistic regression analysis was conducted to estimate crude odds ratios (OR) and 95% CI for the association between potential risk factors and hookworm infection and schistosomiasis. Multivariable logistic regression analysis was used to determine the association of risk factors with the prevalence of hookworm and schistosomiasis after controlling for confounders. In addition to age and sex, variables were selected for inclusion in the multivariable analysis based on the following criteria: 1) p-value for association with the outcome less than 0.1 in the univariable analysis; 2) biological plausibility for an association between an independent variable and the outcome.; 3) representative variable considering collinearity with similar variables.
The following variables were included in the multivariable analysis of risk factors for hookworm infection: sex, age, open defecation, water source used for non-drinking purposes, water fetching time, working in the soil, frequency of water-associated activities, and knowledge of skin penetration as a cause of parasite infection. The variable “water source used for drinking purposes” was not included in the multivariable analysis due to the possibility of collinearity with water sources used for non-drinking purposes.
For multivariable analysis of schistosomiasis, the following variables were included: sex, age, living near the lake or river, handwashing before eating, utilising improved water sources for other purposes, and the frequency of swimming, bathing, and washing clothes in risky environments. The variable “always handwashing after defecation” was excluded from the multivariable analysis due to collinearity with the variable of handwashing before eating. After completing the multivariable analysis, variables that exhibited a p-value ≤ 0.05 were regarded as statistically significant.
Results
Participant characteristics
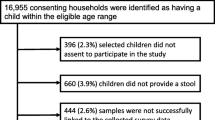
A total of 1,617 students from 33 schools (Fig. 1) were enrolled into the study, 632 (39%) from schools in lakeshore sub-countries. The mean age was 12.1 years (range 7.1–21.4 years), and 810 (50.1%) were male. Some respondents used more than one water source for drinking and other purposes; 9.2% (149) of all respondents used unimproved water sources for drinking, while 14.5% (234) used unimproved water sources for non-drinking purposes (Table 1). Borehole water was the primary source for drinking and other purposes in both lakeshore sub-counties and non-lakeshore sub-counties (supplementary Table 1). Of the study participants, 69.9% (1130) reported having hand-washing facilities at home. Among this group, 54.5% (616) had access to a fixed water facility within their homes.
Prevalence results
Of 1,617 students, 361 (22.4%) were diagnosed with soil-transmitted helminth (STH) infection: 352 (21.8%) had hookworm infection, three (0.2%) had Ascaris lumbricoides infection, and six (0.4%) had Trichuris trichiura infection. The prevalence of hookworm infection by sub-county ranged from 8 to 39% (supplementary Table 2). Additionally, 302 students were found to be infected with S. mansoni, representing 18.7% of the students in the study (Table 1). The prevalence of schistosomiasis by sub-county ranged from 2 to 68% (supplementary Table 2). The prevalence of hookworm and S. mansoni co-infection was 5.8% (n = 94).
Infection intensity was categorized according to WHO definitions of light, moderate or heavy. Among the hookworm-positive cases, 338 children (95.9%) had mild-intensity, 11 (3.1%) had moderate-intensity, and three (0.9%) had heavy-intensity infection. On the other hand, among the S. mansoni-positive cases, 177 (58.6%) had mild-intensity, 69 (22.8%) had moderate-intensity, and 56 (18.5%) had heavy-intensity infection.
Demographic characteristics, geological factors, WASH factors, and knowledge associated with hookworm infection and schistosomiasis
Crude associations with hookworm infection
There was no difference in hookworm prevalence between boys (184/810) and girls (168/807, OR: 0.89, 95% CI: 0.71–1.13, p = 0.35), and prevalence was similar across the different age groups. Hookworm infection was crudely associated with several WASH factors. Those using unimproved water sources, either for drinking purposes (OR: 1.58, 95% CI: 1.10–2.30, p = 0.02) or non-drinking purposes (OR: 1.43, 95% CI: 1.04–1.96, p = 0.03), had elevated hookworm prevalence. Other associated factors included extended water fetching time (> 30 min versus ≤ 30 min) (OR: 1.51, 95% CI: 1.16–1.97, p = 0.002), increased frequency of partaking in water-related activities, such as swimming, bathing, and washing clothes in lakes, rivers, and swamps (Trend OR: 1.27, 95% CI: 1.11–1.48, p = 0.001), and daily exposure to contaminated soil (working in the soil every day) (OR: 1.35, 95% CI: 1.03–1.77, p = 0.03). No significant associations were observed between hookworm infection status and other factors, including school location (lakeshore-locating vs. non-lakeshore-locating), household possession of appropriate latrines, handwashing practices, household assets, animal contact, deworming history, or knowledge regarding parasite infection.
Crude associations with schistosomiasis
The prevalence of schistosomiasis was slightly higher in boys (165/810) than in girls (137/807, OR: 0.80, 95% CI: 0.62–1.03, p = 0.08), and decreased somewhat with increasing age category (trend OR: 0.93, 95% CI: 0.86–1.00; p = 0.05).
Schistosomiasis was crudely associated with several environmental and behavioural factors. Students attending schools located along lakeshores had substantially higher odds of schistosomiasis (OR: 6.80, 95% CI: 5.01–9.24, p = 0.001). Additionally, utilising unimproved water sources for non-drinking purposes (OR: 1.62, 95% CI: 1.17–2.25, p = 0.01), not always washing hands after defecation (OR: 1.38, 95% CI: 1.08–1.78, p = 0.01), and before eating (OR: 1.74, 95% CI: 1.33–2.27, p = 0.001), were associated with having schistosomiasis. Frequency of partaking in water-related activities, such as swimming, bathing, and washing clothes in lakes, rivers, and swamps, was associated with schistosomiasis (Trend OR: 1.50, 95% CI: 1.29–1.75, p = 0.001) as was residing within one hour of water sources (OR: 1.92, 95% CI: 1.46–2.53, p = 0.001). However, no significant associations were observed between schistosomiasis and the use of appropriate latrines, open defecation behaviours, household assets, exposure to soil, or knowledge regarding parasite infections (Table 2).
Multivariable logistic regression analysis for hookworm infection
In the multivariable analysis for hookworm infection (Table 3), children who reported that the journey time for fetching water was longer than 30 min had higher odds of hookworm infection compared to the ≤ 30 min group (AOR: 1.49, 95% CI: 1.13–1.96, p = 0.01). Those who reported working in the soil every day had increased odds of hookworm infection compared to those who did not (AOR: 1.36, 95% CI: 1.03–1.81, p = 0.03). Increased frequency of doing a water-associated activity was associated with higher odds of hookworm infection (AOR: 1.37, 95% CI: 1.01–1.86 and 1.67, 95% CI: 0.93–2.99 for once a week and twice a week, respectively, versus none) (Table 3).
Multivariable logistic regression analysis for schistosomiasis
In the multivariable analysis for schistosomiasis (Table 4), as age increased, the odds of schistosomiasis decreased somewhat (AOR: 0.93, 95% CI: 0.86–1.00, p = 0.05). Increased frequency of engaging in swimming, bathing, and washing activities in lakes, rivers, or swamps was associated with higher odds of schistosomiasis compared to those who never engaged in such activities (e.g. AOR: 2.91, 95% CI: 1.66–5.13 for twice a week versus none). Additionally, those not always washing hands before eating had higher odds of having schistosomiasis than those who always washed hands before eating (AOR: 2.00, 95% CI: 1.50–2.67, p = 0.001). Finally, those who lived within one hour by foot from a river, lake, or swamp had higher odds of schistosomiasis (AOR: 1.84, 95% CI: 1.35–2.50, p = 0.001) (Table 4).
Discussion
This study focused on factors influencing hookworm and schistosomiasis infection among SAC in Mayuge district, Uganda. Despite high program coverage of MDA for STH and schistosomiasis during the MANE project period (2019–2021), hookworm and schistosomiasis prevalence in 2022 remained high at 21.8% and 18.7%, respectively, compared to 15.1% and 27.2% in 2019. The study's findings improve understanding of the behavioural factors, environmental elements and sociodemographic traits that contribute to the pervasive presence of hookworm and schistosomiasis infections. These results may inform the interventions required for mitigating hookworm and schistosomiasis infections. As expected, activities associated with soil exposure, such as prolonged water fetching and frequent soil work, increased the likelihood of hookworm infection [32, 33]. Frequent engagement in water-related activities and poor hand-washing behaviour heightened the risk of schistosomiasis [32], whereas living farther away from water sources decreased the risk of contracting schistosomiasis [34].
The WHO recommends targeting SACs aged 9 to 10 years when conducting surveys to assess STH prevalence and schistosomiasis at the community level [31]. We adopted this approach in our study, so our findings do not necessarily represent all-age community prevalence. It is notable that in this SAC age group, the proportion of moderate to heavy schistosomiasis was higher than that of moderate to severe hookworm infection. This suggests that breaking the morbidity pattern for schistosomiasis when implementing WASH intervention may be more challenging than for hookworm infection.
Longer water fetching time was associated with hookworm infection, as found in an Ethiopia study [32]. We also found that daily work with exposure to soil was associated with hookworm infection. These findings are consistent with known mechanisms of infection. Hookworm prevalence increases in warm and moist soil and infective hookworm larvae can penetrate human skin directly, particularly the hands and feet [35]. In Mayuge District, SAC often engage in water-fetching practices without wearing footwear, heightening their vulnerability to hookworm larvae exposure during these activities. Therefore, this exposure can increase the likelihood of contracting hookworm infections among this age group.
The prevalence of schistosomiasis was lower for those who lived over an hour's walk from a river or lake and were attending schools in non-lakeshore sub-counties. This is because individuals who are not in close proximity to water bodies are less likely to come into contact with contaminated surface water where schistosomiasis-causing parasites may be present.[36]. Activities in the lake, river, and swamps, such as bathing, washing, and swimming, were associated with an increased risk of schistosomiasis, emphasising the well-established link between contaminated water and schistosomiasis infection [37].
Good hand hygiene practices in our study, specifically during pivotal daily activities—such as after defecation and before eating—were associated with reduced schistosomiasis. However, establishing a definitive cause-and-effect relationship between handwashing and schistosomiasis remains unclear. While schistosoma eggs in human excreta can release miracidia into freshwater, this parasite stage does not directly infect humans [38]. Similarly, the reasoning behind the association of schistosomiasis with handwashing before eating is difficult to explain. Further investigation is warranted to ascertain whether these factors causally contribute to schistosomiasis or if other unmeasured confounding variables influenced the observed association between handwashing behaviours and schistosomiasis.
We found no evidence of an association between hookworm infection and age, likely because our study focused on children attending school. Other researchers have indicated a discernible pattern of increasing hookworm infection rates with age, reaching a plateau typically observed in individuals in their thirties or forties [39, 40], which is different from other STHs. Studies that have examined the factors contributing to increased hookworm infection intensity with advancing age suggest that hookworms employ strategies to evade or suppress the host's immune response as individuals age [41, 42]. We observed a slight decline in schistosomiasis prevalence with increasing age in contrast to other studies, which have reported an increasing trend in schistosomiasis prevalence up to adolescence [16] or early adulthood followed by a decline in older age [43, 44].
We found no evidence of association between sex and helminth infections in our study, in contrast to multiple studies conducted in Africa (Ethiopia [45], Tanzania [46], Mali, Burkina Faso, Ghana [47], Cote d’Ivoire [47]) and Asia (Sri Lanka [48], Laos PDR [49]) that have identified higher prevalence of hookworm in males than females, predominantly due to greater exposure to soil among males [50, 51]. Similarly, schistosomiasis prevalence in Africa [52] generally shows male predominance, but this can be attributed to the gender disparity with water exposure, which may be less relevant among school-aged children. In some contexts, prevalence was higher in men due to activities such as swimming, farming, and fishing [50,51,52,53]; in others, prevalence was higher in women primarily due to contact with contaminated water for household chores [53].
Compared to the MANE 2019 baseline survey estimate of 27%, the prevalence of schistosomiasis decreased to 19%. However, contrary to the working hypothesis, the prevalence of hookworm increased slightly, from 16 to 22%. There are multiple possible explanations for this. First, we prepared two slides per stool sample for examination, aiming to enhance the detection yield of parasite eggs. However, in the prevalence survey conducted in 2019, only one slide per stool sample was examined. Consequently, the relatively increased prevalence of hookworm in this study compared to 2019 might have been influenced by this discrepancy in the number of slides per stool sample and greater detection in the follow-up relative to the baseline survey. Additionally, during the COVID-19 pandemic, the two-year closure of schools nationwide in Uganda resulted in increased participation of school-aged children residing in rural areas in labour alongside their parents [54, 55]. Male students became more involved in agricultural activities, while female students engaged more in domestic chores. These shifts in their daily routines likely led to increased exposure to contaminated soil, potentially contributing to the rise in hookworm infections in the 2022 prevalence survey compared to the hookworm prevalence in 2019. Therefore, the increase in the number of slides prepared per sample for examination and the increased exposure of school-aged children to contaminated soil due to the COVID-19 pandemic might explain the rise in hookworm infection prevalence despite the ongoing efforts of the MANE project.
Limitation
Our study may have been subject to selection bias, due to the fact that only children attending school were eligible for inclusion, and they may not be representative of non-school attending children. Although every attempt was made to collect information on anticipated confounders, we cannot rule out the possibility of residual confounding. The study's respondents participated by responding in a self-reporting format, which could entail reliance on memory or reflect social desirability bias. As mitigation, when survey interviewers were trained, they were instructed to conduct one-on-one interviews with the interviewees and not to be subject to peer pressure. Additionally, standardised questions were posed to the interviewees, and interviewers recorded responses directly into standardised templates using mobile phones. This approach aimed to mitigate the limitations associated with self-reporting.
Conclusions
Longer water fetching times and daily work in the soil are identified as common risk factors for hookworm infection. The association between water fetching time and hookworm infection underscores the importance of efficient water supply systems to minimise exposure to contaminated environments. Daily soil work highlights the need for protective measures, such as appropriate footwear, to reduce the risk of hookworm infection.
Schistosomiasis is associated with exposure to contaminated water sources, emphasising the critical role of access to safe and clean water in preventing the disease. Inadequate handwashing behaviours are linked to an increased risk of schistosomiasis, which needs further investigation to identify a cause-and-effect relationship between handwashing and schistosomiasis.
The study underscores the significance of effective water supply systems and protective measures in reducing hookworm infection risks, as well as the critical role of safe water access in preventing schistosomiasis. Further investigation is needed to understand the relationship between handwashing practices and schistosomiasis risk. These findings emphasise the importance of Water, Sanitation, and Hygiene (WASH) interventions in addressing both hookworm and schistosomiasis. Integrated neglected tropical disease elimination programs should prioritise WASH improvements to reduce exposure to contaminated soil and water, highlighting the interconnected nature of environmental factors, hygiene behaviours, and disease transmission..
Availability of data and materials
Data is provided as a supplementary file.
Abbreviations
- AOR:
-
Adjusted Odds Ratio
- CI:
-
Confidence Interval
- CR:
-
Cure rate
- DALY:
-
Disability-adjusted life years
- HC:
-
Health centre
- KOICA:
-
Korean International Cooperation Agency
- MANE project:
-
Mayuge NTDs Elimination project
- MDA:
-
Mass drug administration
- NTDs:
-
Neglected tropical diseases
- OR:
-
Odds Ratio
- PPS:
-
Probability proportional to size
- PSAC:
-
Preschool-aged children
- PZQ:
-
Praziquantel
- STH:
-
Soil-transmitted helminth
- VCD:
-
Vector-borne and NTD control division
- WASH:
-
Water, sanitation, and hygiene
- WHO:
-
World Health Organization
References
Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386(9995):743–800.
Bartsch SM, Hotez PJ, Asti L, Zapf KM, Bottazzi ME, Diemert DJ, et al. The global economic and health burden of human hookworm infection. PLoS Negl Trop Dis. 2016;10(9):e0004922.
Hotez PJ, Bethony JM, Diemert DJ, Pearson M, Loukas A. Developing vaccines to combat hookworm infection and intestinal schistosomiasis. Nat Rev Microbiol. 2010;8(11):814–26.
Rojo JU, Melkus MW, Kottapalli KR, Okiya OE, Sudduth J, Zhang W, et al. Sm-p80-based schistosomiasis vaccine mediated epistatic interactions identified potential immune signatures for vaccine efficacy in mice and baboons. PLoS One. 2017;12(2):e0171677.
Tsuji N. Schistosomiasis and hookworm infection in humans: disease burden, pathobiology and anthelmintic vaccines. Parasitol Int. 2020;75:102051.
Loukas A, Hotez PJ, Diemert D, Yazdanbakhsh M, McCarthy JS, Correa-Oliveira R, et al. Hookworm infection. Nat Rev Dis Prim. 2016;2(1):16088 Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JSandPAGE=referenceandD=med13andNEWS=NandAN=27929101 .
Brooker S, Albonico M, Bethony J, Geiger SM, Loukas A, Diemert D, et al. Soil-transmitted helminth infections: ascariasis, trichuriasis, and hookworm. Lancet. 2006;367(9521):1521–32 Available from: http://www.journals.elsevier.com/the-lancet/ .
Stephenson LS, Latham MC, Adams EJ, Kinoti SN, Pertet A. Physical fitness, growth and appetite of Kenyan school boys with hookworm, Trichuris trichiura and Ascaris lumbricoides infections are improved four months after a single dose of albendazole. J Nutr. 1993;123(6):1036–46.
Hotez PJ, Brindley PJ, Bethony JM, King CH, Pearce EJ, Jacobson J. Helminth infections: the great neglected tropical diseases. J Clin Invest. 2008;118(4):1311–21.
Aderoba AK, Iribhogbe OI, Olagbuji BN, Olokor OE, Ojide CK, Ande AB. Prevalence of helminth infestation during pregnancy and its association with maternal anemia and low birth weight. Int J Gynecol Obstet. 2015;129(3):199–202.
Colley DG, Bustinduy AL, Secor WE, King CH. Human schistosomiasis. Lancet. 2014;383(9936):2253–64.
Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. Lancet. 2006;368(9541):1106–18.
Rollinson D. A wake up call for urinary schistosomiasis: reconciling research effort with public health importance. Parasitology. 2009;136(12):1593–610.
Hotez PJ, Kamath A. Neglected tropical diseases in sub-Saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Negl Trop Dis. 2009;3(8):e412.
Adriko M, Tinkitina B, Arinaitwe M, Kabatereine NB, Nanyunja M, Tukahebwa EM, et al. Impact of a national deworming campaign on the prevalence of soil-transmitted helminthiasis in Uganda (2004–2016): implications for national control programs. PLoS Negl Trop Dis. 2018;12(7):e0006520. Available from: https://doi.org/10.1371/journal.pntd.0006520.
Exum NG, Kibira SPS, Ssenyonga R, Nobili J, Shannon AK, Ssempebwa JC, et al. The prevalence of schistosomiasis in Uganda: a nationally representative population estimate to inform control programs and water and sanitation interventions. PLoS Negl Trop Dis. 2019;13(8):e0007617.
Muhumuza R, et al. Integrated prevalence mapping of schistosomiasis and soil-transmitted helmintiasis utilizing ecological modelling among communities in Mayuge district: implications for neglected tropical diseases elimination project 2019–2021. Int J Curr Res. 2021;13(1):e0011896.
Vercruysse J, Albonico M, Behnke JM, Kotze AC, Prichard RK, McCarthy JS, et al. Is anthelmintic resistance a concern for the control of human soil-transmitted helminths? Int J Parasitol Drugs Drug Resist. 2011;1(1):14–27.
Kumar V, Gryseels B. Use of praziquantel against schistosomiasis: a review of current status. Int J Antimicrob Agents. 1994;4(4):313–20.
Jiraamonnimit C, Wongkamchai S, Boitano J, Nochot H, Loymek S, Chujun S, et al. A cohort study on anti-filarial IgG4 and its assessment in good and uncertain MDA-compliant subjects in brugian filariasis endemic areas in southern Thailand. J Helminthol. 2009;83(4):351–60 Available from: http://ovidsp.ovid.com/ovidweb.cgi?T=JSandPAGE=referenceandD=emed11andNEWS=NandAN=50507992 .
Gabrie JA, Matamoros G, Rueda MM, Rodriguez C, Canales M, Fontecha G, et al. High endemicity of soil-transmitted helminths in a population frequently exposed to albendazole but no evidence of antiparasitic resistance. Trop Med Infect Dis. 2019;4(2):73 Available from: https://www.mdpi.com/2414-6366/4/2/73/pdf .
Gunawardena GSA, Karunaweera ND, Ismail MM. Effects of climatic, socio-economic and behavioural factors on the transmission of hookworm (Necator americanus) on two low-country plantations in Sri Lanka. Ann Trop Med Parasitol. 2005;99(6):601–9.
Tomono N, Anantaphruti MT, Jongsuksuntigul P, Thongthien P, Leerapan P, Silapharatsamee Y, et al. Risk factors of helminthiases among schoolchildren in southern Thailand. Southeast Asian J Trop Med Public Health. 2003;34:264–8.
Ensink JHJ, van der Hoek W, Mukhtar M, Tahir Z, Amerasinghe FP. High risk of hookworm infection among wastewater farmers in Pakistan. Trans R Soc Trop Med Hyg. 2005;99(11):809–18.
Olsen A, Samuelsen H, Onyango-Ouma W, Riess H, Clowes P, Kroidl I, et al. A study of risk factors for intestinal helminth infections using epidemiological and anthropological approaches. J Biosoc Sci. 2013;7(9):e2408.
World Health Organization. The social context of schistosomiasis and its control: an introduction and annotated bibliography. World Health Organization; 2008.
da Paz WS, Duthie MS, de Jesus AR, de Araújo KCGM, Dos Santos AD, Bezerra-Santos M. Population-based, spatiotemporal modeling of social risk factors and mortality from schistosomiasis in Brazil between 1999 and 2018. Acta Trop. 2021;218:105897.
Liu Y, Zhou YB, Li RZ, Wan JJ, Yang Y, Qiu DC, et al. Epidemiological features and effectiveness of schistosomiasis control programme in mountainous and hilly region of the People’s Republic of China. Adv Parasitol. 2016;92:73–95.
Kish L. Survey sampling. New York: John Wiley & Sons Inc; 1965.
Katz N, Chaves A, Pellegrino J. A simple, device for quantita tive stool thick-smear technique in schistosomiasis mansoni. Rev Inst Med Trop Sao Paulo. 1972;14(6):397–400.
Montresor A, Crompton DWT, Hall A, Bundy DAP, Savioli L. Guidelines for the evaluation of soil-transmitted helminths and schistosomiasis at community level. 1998.
Phillips AE, Ower AK, Mekete K, Liyew EF, Maddren R, Belay H, et al. Association between water, sanitation, and hygiene access and the prevalence of soil-transmitted helminth and schistosome infections in Wolayita, Ethiopia. Parasit Vectors. 2022;15(1):410.
Hotez P. Hookworm and poverty. Ann N Y Acad Sci. 2008;1136(1):38–44.
Kloos H, Fulford AJC, Butterworth AE, Sturrock RF, Ouma JH, Kariuki HC, et al. Spatial patterns of human water contact and Schistosoma mansoni transmission and infection in four rural areas in Machakos District. Kenya Soc Sci Med. 1997;44(7):949–68.
Mabaso MLH, Appleton CC, Hughes JC, Gouws E. The effect of soil type and climate on hookworm (Necator americanus) distribution in KwaZulu‐Natal, South Africa. Trop Med Int Heal. 2003;8(8):722–7.
King CH. The evolving schistosomiasis agenda 2007–2017—why we are moving beyond morbidity control toward elimination of transmission. PLoS Negl Trop Dis. 2017;11(4):e0005517.
Jordan P, Christie JD, Unrau GO. Schistosomiasis transmission with particular reference to possible ecological and biological methods of control. A review. Acta Trop. 1980;37(2):95–135.
Grimes JET, Croll D, Harrison WE, Utzinger J, Freeman MC, Templeton MR. The roles of water, sanitation and hygiene in reducing schistosomiasis: a review. Parasit Vectors. 2015;8(1):1–16.
Gandhi NS, Jizhang C, Khoshnood K, Fuying X, Shanwen L, Yaoruo L, et al. Epidemiology of Necator americanus hookworm infections in Xiulongkan Village, Hainan Province, China: high prevalence and intensity among middle-aged and elderly residents. J Parasitol. 2001;87(4):739–43.
Hotez PJ, Brooker S, Bethony JM, Bottazzi ME, Loukas A, Xiao S. Hookworm infection. N Engl J Med. 2004;351(8):799–807.
Olatunde BO, Onyemelukwe GC. Immunosuppression in Nigerians with hookworm infection. Afr J Med Med Sci. 1994;23(3):221–5.
Loukas A, Prociv P. Immune responses in hookworm infections. Clin Microbiol Rev. 2001;14(4):689–703.
Raso G, Vounatsou P, McManus DP, N’Goran EK, Utzinger J. A Bayesian approach to estimate the age-specific prevalence of Schistosoma mansoni and implications for schistosomiasis control. Int J Parasitol. 2007;37(13):1491–500.
Matthys B, Tschannen AB, Tian-Bi NT, Comoé H, Diabaté S, Traoré M, et al. Risk factors for Schistosoma mansoni and hookworm in urban farming communities in western Cote d’Ivoire. Trop Med Int Heal. 2007;12(6):709–23.
Alemayehu GS. Prevalence and risk factors of soil-transmitted helminthes among school children in Abosa around Lake Zway, Southern Ethiopia. MSc. MSc Addis Ababa Addis Ababa Univ. 2008.
Lello J, Knopp S, Mohammed KA, Khamis IS, Utzinger J, Viney ME. The relative contribution of co-infection to focal infection risk in children. Proc R Soc B Biol Sci. 2013;280(1754):20122813.
Magalhães RJS, Barnett AG, Clements ACA. Geographical analysis of the role of water supply and sanitation in the risk of helminth infections of children in West Africa. Proc Natl Acad Sci. 2011;108(50):20084–9.
Gunawardena K, Kumarendran B, Ebenezer R, Gunasingha MS, Pathmeswaran A, De Silva N. Soil-transmitted helminth infections among plantation sector schoolchildren in Sri Lanka: prevalence after ten years of preventive chemotherapy. PLoS Negl Trop Dis. 2011;5(9):e1341.
Hohmann H, Panzer S, Phimpachan C, Southivong C, Schelp FP. Relationship of intestinal parasites to the environment and to behavioral factors in children in the Bolikhamxay Province of Lao PDR. Southeast Asian J Trop Med Public Health. 2001;32(1):4–13.
Behnke JM, De Clercq D, Sacko M, Gilbert FS, Ouattara DB, Vercruysse J. The epidemiology of human hookworm infections in the southern region of Mali. Trop Med Int Heal. 2000;5(5):343–54.
Khair M, Khanum H, Hossain M, Alam MS. Prevalence, Risk Factors and Comparative Diagnosis of Soil Transmitted Helminths (STH) in children of slum areas of Dhaka and tea garden areas of Sylhet. In: 12th Biennial Conference, BAU, Bangladesh, Abstract. 2016. p. 55.
Ayabina DV, Clark J, Bayley H, Lamberton PHL, Toor J, Hollingsworth TD. Gender-related differences in prevalence, intensity and associated risk factors of Schistosoma infections in Africa: a systematic review and meta-analysis. PLoS Negl Trop Dis. 2021;15(11):e0009083.
Nooman ZM, Hasan AH, Waheeb Y, Mishriky AM, Ragheb M, Abu-Saif AN, et al. The epidemiology of schistosomiasis in Egypt: Ismailia governorate. Am J Trop Med Hyg. 2000;62(2_suppl):35–41.
Mahmud M, Riley E. Household response to an extreme shock: evidence on the immediate impact of the covid-19 lockdown on economic outcomes and well-being in rural Uganda. World Dev. 2021;140:105318.
Sserwanja Q, Kawuki J, Kim JH. Increased child abuse in Uganda amidst COVID-19 pandemic. J Paediatr Child Health. 2021;57(2):188–91.
Acknowledgements
The authors thank the children who participated in the study. The authors thank the field workers and medical staff of the Mayuge district who supported this study. The authors thank Mr. Ilyun Koh, who created a map showing the selected schools for the study. The authors also thank the staff of the Vector-borne and NTDs control division of the Ugandan Ministry of Health, who supervised and conducted stool examinations in the field.
Funding
Korea International Cooperation Agency (KOICA) financially supported the MANE project, and this article was published in collaboration with KOICA and World Vision (Grant No: 2019–04). This study was conducted as part of the MANE project. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
ESK, KS, and ELW conceptualised and designed the study. ESK, KCO, and DL performed field study and collected data. ESK, KS, and ELW analysed the data. MA, KS, and ELW supervised the study. ESK wrote the original manuscript. ESK, MA, KS, and ELW reviewed and edited the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ugandan Vector Control Division Research Ethics Committee (VCDREC; reference number:
UG-REC-018/VCDREC104), Uganda National Council for Science and Technology (UNCST; reference number: HS1411ES), and the London School of Hygiene and Tropical Medicine ethics committee (LSHTM ethic reference:25818) approved this study.
This study was embedded within the Mayuge NTD Elimination (MANE) project, which was funded by the Korean International Cooperation Agency (KOICA).
The child assent and parents/guardians consent forms were designed in English and the local language(Lusoga). Information about the study was provided to children and their parents/guardians, and children who signed the child assent form and whose parents/guardian provided written informed consent were included. Local authorities approved the forms to use them during the ethics approval process.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, E.S., Adriko, M., Oseku, K.C. et al. Factors associated with hookworm and Schistosoma mansoni infections among school-aged children in Mayuge district, Uganda. BMC Public Health 24, 1620 (2024). https://doi.org/10.1186/s12889-024-19092-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-19092-7