Abstract
Background
HIV prevention remains a global priority, especially in sub-Saharan Africa. Our research team previously developed an evidence-based peer group program for HIV prevention called Mzake ndi Mzake (Friend to Friend). A community-engaged collaboration adapted the program for community ownership and implementation. Here we report whether this HIV prevention program, implemented by community volunteers, increased condom use among sexually active individuals in rural Malawi.
Methods
Three communities sequentially rolled out the program. Effectiveness was evaluated using a stepped wedge design. Repeated surveys 11–13 months apart were conducted between 2016 and 2019. At Time 1, no community had offered the intervention. At Time 2, the first community had offered the intervention and two had not (control group). At Time 3, two communities had offered the intervention and one had not (control group). We used two condom use indicators; condom use frequency in the last 2 months (N = 771) and condom use at last sex (N = 880). The analytical sample included all sexually active persons answering that question at one or more time points. Mixed-effects cumulative logit and Generalized Estimating Equation (GEE) models were used to model the two condom indicators over time, controlling for demographic factors, UNAIDS HIV knowledge, safer sex self-efficacy and partner communication.
Results
This peer group intervention implemented by trained community volunteers increased both condom use indicators at Times 2 and 3. In the final adjusted models with non-significant factors removed, condom use in the last two months increased for the intervention group vs. control group [Time 2: Adjusted Odds Ratio (AOR) = 1.59 (1.15, 2.21); Time 3: AOR 2.01 (1.23, 3.30)]. Similarly, condom use at last sex increased for the intervention group vs. control group [Time 2: AOR = 1.48 (1.08, 2.03); Time 3: AOR 1.81 (1.13, 2.90)]. Other significant predictors of greater condom use were also described. Although the intervention increased UNAIDS HIV knowledge, knowledge did not predict condom use.
Conclusions
In this community-engaged implementation study, an evidence-based peer group program for HIV prevention increased condom use when delivered by trained community volunteers. Community ownership and program delivery by trained volunteers offer an innovative and cost-effective strategy to address ongoing HIV prevention needs without overburdening healthcare systems in sub-Saharan Africa.
Trial registration
Clinical Trials.gov NCT02765659 Registered May 6, 2016.
Similar content being viewed by others
Background
Despite global declines in new Human Immunodeficiency Virus (HIV) infections, 1.5 million people are newly infected per year [1]. Achieving the UNAIDS goal of reducing new HIV infections to near-zero by 2030 seems unlikely. Even if achieved, HIV will remain an endemic health problem for decades, necessitating the continuation of primary HIV prevention programs [2]. Even with the greatest decline in new infections, sub-Saharan Africa remains the region the most heavily affected by HIV with 860,000 new infections annually; moreover, there is a significant gender gap, with 63% of new infections occurring among women [1, 3]. In countries outside of the region, 94% of new infections occur among key populations (e.g., sex workers, men who have sex with men, injecting drug users, transgender persons and their partners) [1]. In sub-Saharan Africa, 49% of new HIV infections occur in the general population [1], creating the need for robust community HIV prevention programs for the general population as well as targeted prevention for higher-risk key populations.
This study took place in Malawi, a country in Southern Africa that ranks ninth globally in HIV prevalence [4]. The most recent national survey reported 20,000 annual new adult infections with an incidence rate of 0.21% in 2020-21 [5]. Notably, women experienced twice as many new infections as men. Moreover, the southern region of Malawi had the highest burden of HIV [5, 6].
Despite the introduction of newer strategies such as male circumcision and pre-exposure prophylaxis (PrEP), condom use remains a crucial component of prevention [7]. Condoms are highly effective, safe, easy to store and use, and cost-effective for individuals and the health system [8,9,10,11]. These advantages make condoms ideal for prevention in the general population [5, 7]. Yet condom use remains low in most of sub-Saharan Africa, including Malawi. Only 18% of all adults aged 15 years and older in Malawi reported using a condom the last time they had sex [12]. Although exceptions exist, such as a recent survey in South Africa where 72% of black youth (ages 18–24) reported using a condom at last sex [13], rates of condom use in other sub-Saharan African countries also are low. Reanalysis of data for sexually active men only from a nationwide survey in Nigeria found that fewer than 20% used condoms consistently [14]. In Zambia only 41% of urban youth said they used a condom at last sex [15]. Even among university students, whose higher education might be expected to promote condom use, a large meta-analysis found that only 53% used a condom the last time they had sex [16], and two recent surveys in South Africa and Nigeria found fewer than 40% of sexually active youth used condoms consistently [17, 18]. Additionally, complacency about HIV has increased as new HIV infections decline and treatment spreads, leading to a decline in both condom use and funding for condom use and HIV prevention programs [19,20,21].
Low rates of condom use across sub-Saharan Africa can be attributed to a variety of contextual factors. Factors include unequal gender norms, concerns about sexual pleasure, negative connotations about trust and commitment, especially within marriage, norms restricting discussion of sexuality among partners and between youth and parents, widespread misconceptions about condoms, poverty and limited educational or job opportunities, lack of privacy for purchasing or obtaining condoms at the clinic, and periodic condom shortages [22,23,24]. The influence of contextual factors is evident in the personal characteristics that are consistently related to more condom use. National surveys and other studies generally show that condom use is more frequent among men, youth, urban residents, those with more education and/or wealth, and those having sex with non-regular partners (defined as a partner who is not a spouse and/or not cohabiting) [5, 12,13,14, 26]. Some studies have identified additional factors associated with increased condom use, including peer and parent influences, self-efficacy, HIV status awareness, and access to youth-friendly clinics and condoms [14, 15, 17, 25,26,27,28].
Despite barriers to condom use, it is important to recognize that the cultural and socioeconomic context evolves, and there is some evidence of changing attitudes toward HIV prevention in Malawi and other sub-Saharan African countries. Two qualitative studies indicated some changes in perspectives, viewing condom use as evidence of commitment and caring for one’s partner by protecting them from HIV infection [22, 23]. Condom use rates may be rising among youth in South Africa [13]. Gender differences may also be shifting; two recent studies among sexually active university students in sub-Saharan Africa found no gender differences in condom use [16, 17],
A substantial body of research has demonstrated that peer group behavior change interventions reduced risk behaviors associated with HIV transmission and increased condom use [29,30,31,32,33,34,35,36]. In these peer group interventions, a small group of similar people participate in repeated sessions focused on a c ommon concern. Most are guided by Bandura’s self-efficacy theory which emphasizes building the confidence needed to adopt a new behavior [37]. This approach has been successful among adults, youth, and key populations, such as commercial sex workers, in various African countries. However, recent systematic reviews and meta-analyses yield less consistent evidence [38,39,40,41,42,43], and some have found intervention effects for males only [38]. Another review for young women only in sub-Saharan Africa compared behavioral change interventions, structural change interventions (such as cash transfers for school continuation), and combination interventions. Although at least one study for each type of intervention improved condom use, the only intervention that reduced HIV incidence was a cash transfer program in Malawi [39]. Many of these studies recommended that interventions incorporate contextual and environmental factors beyond the individual level, more formative evaluation to tailor the intervention to context, and greater community involvement.
In line with a growing emphasis on tailoring, two HIV prevention programs in Malawi incorporated contextual and environmental factors. The BRIDGES II Program for both men and women, which involved small group discussions, community-based participation, and radio messages, increased AIDS knowledge, self-efficacy, and condom use at last sex [44]. The Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe (DREAMS) partnership targeted young women ages 15–24 in 10 sub-Saharan African countries. DREAMS components included “club” meetings for young women, family-strengthening and community awareness programs, and youth-friendly health services [45]. Early results from Kenya, Malawi, and Zambia indicated a reduction in violence against young women, but no effects on condom use [46, 47]. In South Africa and Kenya, the DREAMS program coincided with a decline in HIV incidence, however because the decline began before this program’s introduction, it cannot be attributed solely to DREAMS. However, in Kenya the program was linked to a reduction in number of lifetime sexual partners and fewer instances of condomless sex [48].
Overall, previous behavior change interventions have yielded mixed results. However, the Mzake ndi Mzake (hereafter Mzake) peer group intervention, developed and tested by our team and delivered by trained health workers, has shown consistent efficacy in increasing condom use among rural adults, rural youth, and rural and urban health workers in Malawi [49,50,51,52]. Given the broad success of the intervention, the next step was to implement the program more widely, starting in southern Malawi where HIV infections are highest [5, 6]. However, due to health worker shortages and increased demand for HIV testing and treatment [53], delivery of Mzake by health workers became unsustainable. Therefore, in partnership with the community, we decided that trained community volunteers could implement the program, taking responsibility for organizing and implementing Mzake. When implemented by the community, the Mzake peer group intervention substantially increased HIV prevention knowledge among all participants [54]. The purpose of this analysis is to determine whether Mzake increased condom use among the sexually active community members.
Methods
Design
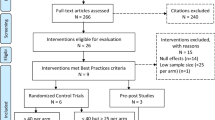
This community-engaged implementation study used a hybrid design to simultaneously examine whether the Mzake peer group program could be implemented by community volunteers and if the program would remain effective when delivered by trained community volunteers. The study took place in Phalombe District, located in the high-prevalence southern region in Malawi [5, 6]. The program was rolled out across three communities using a stepped wedge design. The order in which communities began implementation was randomly assigned. Effectiveness was determined using repeated annual surveys of participants in all 3 communities. The time between surveys ranged between 11 and 13 months. The Time 1 (baseline) survey occurred before any community started rollout. At Time 2, the first community had completed rollout, and the other two communities served as controls. At Time 3, two communities had rolled out the intervention, while the third community had not yet begun rollout and served as controls. As documented by Mzake attendance records, survey retention rates were very high at over 90% at both Times 2 and 3. Participation in the intervention was also very high, with all but four participants attending at least 5 of the 6 sessions as documented by Mzake attendance records.
The design and methods for this analysis are like those of a previously reported study showing the positive impact of the intervention on HIV knowledge [54]. However, because condom use is only relevant for those who are sexually active, the samples used for this analysis differed from those used in the knowledge analysis. Therefore, we briefly present the key features of the overall study, with more detailed methods specific to the condom use analysis, including the sample, variables, and analysis plan. Further details on the study’s general design and methods can be found in the HIV knowledge paper and a protocol paper summarizing the conceptual basis and design of the larger study [54, 55].
Site and sample
This project took place in Phalombe District located in southeastern Malawi. The District’s HIV prevalence rate was 15.6%, nearly 1.5 times the national rate of 10.6% in 2016 when this research began [5]. By 2020-21 when the study ended, the national prevalence rate had decreased to 7.1% but the prevalence where Phalombe is located had only decreased to 14.1%, increasing the regional disparity [6].
To recruit peer group members, the volunteers held community meetings to explain the program. The recruitment criteria included: residing in the specific community, meeting the age criterion of either over 19 for adults or between 13 and 19 for youth, and agreeing to participate in the 6-session intervention when offered in their community and complete the repeated audio-assisted computerized surveys (ACASI). Those who wanted to participate then gave signed consent or, for minors under age 18, both parent and youth signed the consent. Thus, participants self-selected to be in the program.
This article used two indicators of condom use: condom use frequency in the last two months (hereafter, condom use frequency) and condom use at last sex. Only sexually active persons answered the condom use questions. Therefore, the analytic sample for condom use is different from the total study participants. The sample for each condom use indicator included only persons who answered that question for at least one of one survey (Times 1–3). For example, a youth who was not sexually active at Time 1 or Time 2 but became sexually active and answered both condom use questions at Time 3 would be included in both analytical samples. Because more participants answered the question about condom use at last sex than the question about condom use frequency over the last two months, the sample size is larger for condom use at last sex.
Intervention
More detail about Mzake, the conceptual model that guides the intervention, and the peer leader training is available in previous publications [37, 55,56,57,58]. Sessions and content are summarized in Table 1.
Measures
All variables and their operational measures used in this analysis are defined in Table 2. The outcomes of interest were two condom use indicators. The first question asked, “In the last two months, how often did you use a condom?” (hereafter, condom use frequency). The three response categories of never, sometimes, and always, resulted in an interval level indicator of condom use, which was previously used in the Mzake efficacy studies [49,50,51]. Responses from persons who stated they did not have sex in the last two months were treated as missing. The second indicator was the dichotomous question, “Now think about the most recent time you had sexual relations. Did you use a condom?”. There was an option to say that the person had never had sexual intercourse, which was also treated as missing. Developed by UNAIDS, this question is easily understood, widely used, and provides comparative data across different times and places. Because it asks about only the most recent occasion, this question is less subject to recall bias but does not provide any sense of how often condoms are used.
Eight covariates were considered in the multivariate longitudinal models. Baseline variables included sex (self-identified), age group (youth ages 13–19 or adults over 19), education, and level of involvement in religiously affiliated activities (very involved versus somewhat or less involved). Time-varying covariates included whether married or cohabiting versus single and three psychosocial factors previous research has linked to condom use: UNAIDS comprehensive HIV prevention knowledge (hereafter UNAIDS knowledge), a safer sex self-efficacy index (hereafter self-efficacy) and a safer sex partner communication index (hereafter partner communication). The self-efficacy and partner communication measures included several different behaviors and are indices rather than scales.
Procedures
The project used a simple 3-step implementation model: plan, roll out and sustain. During planning, each community’s leaders established a Coordinating Committee. The Committee selected volunteer peer group facilitators and coordinated their training. They then recruited community members to participate in the Mzake program. Program rollout began when recruitment, peer leader training, and implementation plans were complete. In each of the three communities, facilitators offered the peer group program to 12 groups of adults and 16 groups of youth (ages 13–19). After rollout was completed, each community sustained the project at least until the end of grant funding.
Analysis
For each condom use indicator, intervention versus control group differences were first examined using Chi-squared tests at each time point. The intervention effectiveness over time for each condom use indicator was then evaluated using multivariate models for longitudinal design, controlling for baseline and time-varying demographic and psychosocial factors. Mixed-effects cumulative logit models were employed to model the ordinal question about the frequency of condom use. Generalized Estimating Equation models (GEE) were used to model the UNAIDS dichotomous question about condom use at last sex. The number of random effects in the mixed-effects cumulative logit model and variance-covariance structures for repeated measures in GEE were selected using likelihood ratio tests or fit statistics such as Akaike Information Criterion (AIC). Significant covariate effects were selected using backward selection methods, controlling for Type I error probability of 0.05. Time trends were evaluated in all regression models using polynomial terms when necessary. Due to the stepped wedge design, in which all individuals were in the control group at baseline, the group effect was not entered in the regression models as a main effect. Instead, group-by-time interaction were used to indicate group differences over time and were the primary focus of inferences. Covariates-adjusted time-point specific group differences and 95% confidence intervals for their odds ratios from multivariate models were reported for both condom use indicators (ordinal proportional odds for frequency of condom use and adjusted odds ratios for condom use at last sex). The statistical software program SAS (9.4) was used for all statistical analyses [59].
Results
Participant characteristics
The total participants at baseline included 1008 participants. For frequency of condom use, the analytical sample used for multivariate regression included 771 participants (76.5% of the total sample). For condom use at last sex, the analytical sample included 880 participants (87.3% of the total sample). For both questions, the number of eligible respondents at each time point varied slightly.
Demographic and psychosocial information is presented for the analytical sample for each question at baseline and at each time point for the time-varying covariates (Table 3). Sample characteristics differ from the total sample reported earlier [54]. Like the total participant sample, the analytical samples have approximately equal numbers from each group village and roughly equal proportions of males and females. However, many more youth (ages 13–19) than adults were not sexually active, so only around 40% of the analytical samples were youth, compared to 54% of the total sample. Because older youth were more likely to be sexually active, the proportion who attended at least some secondary school was also higher for the analytical samples. The analytical samples also had a substantially higher proportion of persons who were married or cohabiting at baseline than the total sample (62.6% for frequency of condom use and 56.1% for the sample for condom use at last sex). In contrast, only 43.3% of the total sample were married or cohabiting. Although the proportion who were married or cohabiting increased over time, the increase was not large. Like the total sample, a majority of participants in both analytical samples reported high involvement in religiously affiliated activities. Mean scores for all three social-psychological covariates increased over time. The demographic and psychosocial information is also presented for the total participants in Additional File 1 at baseline for all variables and at all times for time-varying co-variates.
Intervention effects on condom use
In bivariate analyses, both indicators of reported condom use were significantly higher for those in the intervention group than the control group at Time 2 and Time 3 (Table 4). For the ordinal variable asking about the frequency of condom use over the last two months, at Time 1 over half (51.3%) of the participants said that they always used a condom, 26.3% used sometimes, and 22.4% never used a condom. At Time 2, reported condom use by those in the control group declined, while reported condom use in the intervention group remained high; 52.9% reported that they used a condom every time and only 17.4% said that they never used a condom. At Time 3, the significant difference between the intervention and control groups remained, with higher percentages reporting more frequent condom use (always or sometimes) in the intervention group.
Greater use of a condom at last sex by the intervention group compared to the control group was also significant at both Time 2 and Time 3. For condom use at last sex, 59% of the sample reported using a condom at Time 1. At Time 2, the control group reported using a condom less often, while the intervention group reported more use (52.7% vs. 71.4%). At Time 3, the group difference was smaller (55.7% vs. 63.6%) yet remained statistically significant.
We then evaluated the impact of the intervention on the condom use indicators using mixed-effects or GEE models when controlling for significant demographic and social-psychological factors (Table 5). After the model selection process, age, partner status, self-efficacy, and communication between partners were found to be associated with both condom use outcomes. Being adult and being married and/or cohabiting related to less condom use for both indicators. Gender was associated only with condom use in the last two months; women reported less frequent condom use. Involvement in religiously affiliated activities was associated only with condom use at last sex; greater involvement increased the odds of condom use at last sex. Both self-efficacy and partner communication significantly increased condom use.
The effect of time on both condom use indicators was negative, indicating that the probabilities of both condom use indicators decreased steadily over time for the control group. However, the intervention by time interaction was positive for both condom use indicators at Time 2 and at Time 3, indicating that the intervention was successful at reversing the decreasing condom use trend in the population (Table 5). At Time 3, the intervention group was about twice as likely to use condoms frequently in the last two months as the control group ([Adjusted Odds Ratio (AOR) = 2.01, 95% CI = 1.23, 3.30], and about 1.8 times more likely to have used a condom at last sex than the control group (AOR = 1.81, 95% CI = 1.13, 2.90).
Discussion
This community-based peer group intervention delivered by trained community volunteers increased the frequency of condom use over the last two months and condom use at last sex. These findings, coupled with the previous finding of increased HIV prevention knowledge [54], indicate the sustained effectiveness of the Mzake program when implemented by community volunteers.
In addition to the impact of the Mzake program on condom use, our multivariate analyses also identified four covariates that related to both frequency of condom use in the past two months and condom use at last sex: age, relationship status, self-efficacy, and partner communication. Consistent with prior studies [5, 12,13,14, 27], being a youth and not having a regular partner were associated with increased condom use.
Higher safer-sex self-efficacy and partner communication also were significant predictors for both condom use variables. These factors are fundamental to the social-cognitive conceptual model that underpins Mzake as well as other peer group interventions. Four studies of youth reported results that were consistent with our findings showing that greater self-efficacy related positively to condom use [17, 18, 33, 41]. However, two systematic reviews of interventions and two additional studies of youth in sub-Saharan Africa had different findings. Although there was often a positive bivariate relationship between self-efficacy and condom use, in multivariate analyses, self-efficacy did not lead to increased condom use or led to greater condom use for young men only [16, 27, 40, 43]. Fewer studies examined partner communication. Three studies reported that partner communication related to greater condom use [15, 18, 27], while another found that partner communication did not relate to condom use in bivariate or multivariate analyses [17]. Our finding demonstrating positive associations of self-efficacy and partner communication with greater condom use contributes to the growing body of evidence supporting the effectiveness of the social-cognitive learning model in facilitating behavior change. However, contrary findings highlight the need for more research to understand the complex relationships among self-efficacy and partner communication, gender and gender-based inequities, and HIV prevention behaviors such as condom use.
Being a man was associated with more frequent condom use over the last two months but did not relate to using a condom at last sex. Congruent with these findings, a large meta-analysis and a survey of university students also found no difference in condom use between men and women [16, 17]. However, our findings contradict many other studies where condom use has been higher for men than women across sub-Saharan Africa regardless of how condom use was measured [5, 12, 13, 18, 27, 37, 40].
Level of involvement in religiously affiliated activities was positively related to condom use at last sex but not to condom use frequency over the last two months. Two other studies examined religious affiliation and condom use [26, 27], but no other studies were located that examined involvement in religiously affiliated activities. Historically, the majority of messages disseminated by faith-based leaders and organizations have opposed condom use. However, there is also evidence that some faith-based leaders and organizations actively contribute to HIV and AIDS initiatives and are receptive to supporting HIV prevention programs as part of their faith-based mission [60,61,62]. Changing perspectives of religious leaders and members about HIV prevention and condom use may relate to this study’s finding of a positive relationship between greater involvement in religious activities and use of a condom at last sexual intercourse. The influence of religious leaders and organizations across sub-Saharan Africa is substantial. One small piece of evidence supporting their continuing importance is that nearly two-thirds of this study’s participants described themselves as highly involved in religiously affiliated activities such as choir, sports, charitable activities, and prayer meetings. A deeper understanding of how religious factors affect condom use and how this is changing over time is very important to increase the effectiveness of HIV prevention interventions.
Two factors, education level and UNAIDS HIV prevention knowledge, are worth noting because these did not show a significant relationship with our indicators of condom use and were therefore excluded from the final regression models. Similar results regarding education emerged in two other studies, which did not find that educational level to be a predictor of condom use in multivariate analyses [15, 26]. Contrary to our findings, in several large surveys higher levels of education were associated with increased condom use [5, 12, 14].
The lack of a positive relationship between UNAIDS HIV knowledge and condom use that we found in our multivariate analyses was also identified in two other publications, a survey in South Africa and an intervention study in Malawi [13, 43]. In the South African survey of young adults ages 18–24, UNAIDS HIV prevention knowledge did not relate to condom use at last sex in either bivariate or multivariate analyses [13]. In the Malawi intervention study, which included small group and community discussions similar to peer groups and a mass media component, exposure to the intervention had a positive impact on both UNAIDS HIV knowledge and condom use at last sex, but in multivariate regression UNAIDS HIV knowledge did not relate to condom use (AOR = 0.98, 95% CI 0.87–1.10) [43]. Contrary to our findings, in three cross-sectional analyses using demographic and health surveys from five African countries a positive relationship was reported between HIV prevention knowledge and greater condom use [14, 25, 28]. These mixed results suggest that knowledge about HIV transmission is important for HIV prevention, but knowledge alone is not sufficient to change behaviors. This pattern of findings is congruent with social-cognitive learning and other behavioral change theories, which posit that other factors, such as self-efficacy and partner communication, may be more directly tied to changing behaviors. Therefore, when knowledge is included in multivariate analyses along with factors like self-efficacy and partner communication, the impact of HIV knowledge may be diminished.
One question that emerges from these results is why the Mzake program has been effective when other similar interventions have not reported similar results. Several factors have been identified by both the research team and community volunteers as potential contributors to Mzake’s effectiveness. In these communities, HIV prevention was a top priority, and the people had strong enthusiasm for implementing an HIV prevention program that had demonstrated success in Malawi. The program was offered to community residents above age 12 regardless of age, gender, or social position, so youth and parents, male and female partners, all types of leaders, and ordinary people, participated in the same HIV prevention program and could support each other. Community members in our previous efficacy studies noted how important mutual support was in helping people change behaviors. Throughout the implementation process, a community-engaged approach was used, which has been shown to increase equitable and effective program implementation [63]. Drawing on their in-depth understanding of the local context, community members actively participated in decision-making processes, including selection and training of peer group facilitators, determining suitable locations and meeting times, and maintaining program records. The research team provided initial training for volunteers and evaluated effectiveness. Moreover, extensive formative evaluations were carried out during initial efficacy studies and for this community implementation program. One example of such an adaptation was having separate peer groups for youth because open discussion of sexuality issues is strongly disapproved by local culture. Youth in groups with adults would probably feel unable to speak about their sexual activities in the presence of a group of other adults. However, the trained adult cofacilitators learned how to establish a trusting relationship with youth peer group members. This strategy fostered retention of Mzake’s core components while allowing for adaptations needed to suit the context. This community-engaged program is congruent with previous researchers’ recommendations that contextual factors at the societal and community levels and formative evaluation to guide adaptation can improve the implementation process and program effectiveness [39,40,41,42].
Limitations
A major limitation, but also likely a strength, of this study, is that neither the community volunteers who delivered the program nor the program participants were randomly selected. Community leaders decided who would serve to coordinate the Mzake program, based largely on their prior volunteer work for the community and proven reliability. This committee then chose individuals who would become peer group facilitators. Selection was based on prior knowledge of who had a record of community service as well as adequate literacy to use the manual effectively. Similarly, community members were invited to an open community meeting, where they decided to participate. While the non-random selection of individuals introduces biases, allowing community autonomy in program implementation is an important strategy for supporting a community-delivered HIV prevention program.
Another important limitation is social desirability bias. Social desirability is probably the most important factor affecting the validity of self-report in an intervention study focused on sensitive issues. Social desirability bias is concerning because it may affect those who completed the intervention more than those who have not yet done so (controls). For example, the Mzake intervention emphasizes condom effectiveness and builds skills for using condoms and discussing this with a partner, strongly suggesting that condom use is the socially desirable response. Using biomarkers as indicators of sexual behaviors strengthens the interpretation of intervention effects because biomarkers are not subject to self-reporting bias. We initially planned to test for the 3 most common sexually transmitted infections in Malawi (chlamydia, gonorrhea, and syphilis) using measures appropriate for use in a community setting with limited facilities. However, just as we started the study, two tests were withdrawn from the market and recent studies documented low reliability for the third. No alternative tests appropriate for use in the community could be located. We consulted with the funding agency and obtained approval to drop these biomarker outcomes.
To reduce social desirability bias as much as possible without the availability of biomarkers, our surveys used Audio-Computer Assisted Self-Interview (ACASI). This evidence-based practice allows participants to listen to recorded questions in their local language using earphones and input their answers on the computer, providing complete privacy and minimal contact with data collectors. ACASI has been shown to elicit greater reporting of sensitive behaviors such as condom use than other survey methods [63, 64]. Our results showed a substantial increase in condom use for those who received the intervention compared to those who had not, but the possibility that social desirability contributed to this difference cannot be ruled out.
Implications
Preventing new HIV infections remains a pressing priority in sub-Saharan Africa. HIV prevention is an essential part of controlling the epidemic [2]. This community-based implementation study found that when an evidence-based peer group program for HIV prevention was organized and delivered by trained community volunteers, the program significantly increased condom use and HIV prevention knowledge [53]. These findings provide valuable evidence that community volunteers can effectively implement peer group programs that result in increased HIV prevention behaviors. This approach is especially pertinent in the face of new challenges including growing complacency toward HIV, declining HIV prevention funding, and decreasing condom use, and persistent health worker shortages [19,20,21, 52]. Leveraging community strengths and human capital resources facilitated the implementation of this effective HIV prevention program in southern Malawi [65]. This community-engaged approach, where the community owns the program which is delivered by trained local volunteers, offers an innovative and cost-effective strategy to address ongoing HIV prevention needs without overburdening healthcare systems in sub-Saharan Africa.
Data availability
The datasets generated and/or analyzed during the current study are not yet publicly available but will be made available based on reasonable request by emailing the corresponding author.
Abbreviations
- HIV:
-
Human immunodeficiency virus
- PMTCT:
-
Prevention of mother to child transmission
- UNAIDS:
-
Joint United Nations Programme on HIV/AID
References
UNAIDS, Global HIV. May & AIDS statistics Fact sheet 2022. https://www.unaids.org/sites/default/files/media_asset/UNAIDS_FactSheet_en.pdf. Accessed 6 2023.
Assefa Y, Gilks CF. Ending the epidemic of HIV/AIDS by 2030: will there be an endgame to HIV, or an endemic HIV requiring an integrated health systems response in many countries? Int J Infect Dis. 2020;100:273–7.
UNAIDS Data. 2022. https://www.unaids.org/sites/default/files/media_asset/data-book-2022_en.pdf. Accessed 6 May 2023.
HIV Rates by Country. 2023. https://worldpopulationreview.com/country-rankings/hiv-rates-by-country. Accessed 6 May 2023.
Ministry of Health Malawi. Malawi population-based HIV impact assessment (MPHIA) 2015–2016.
Malawi Population-based HIV Impact. Assessment 2020–2021 (MPHIA 2020–2021): final report. Lilongwe: MOH, Malawi; November, 2022.
Hearst N, Chen S. Condom promotion for AIDS prevention in the developing world: is it working? Stud Fam Plann. 2004;35(1):39–47.
Pinkerton SD, Abramson PR. Effectiveness of condoms in preventing HIV transmission. Soc Sci Med. 1997;44(9):1303–12.
Giannou FK, Tsiara CG, Nikolopoulos GK, Talias M, Benetou V, Kantzanou M, Bonovas S, Hatzakis A. Condom effectiveness in reducing heterosexual HIV transmission: a systematic review and meta-analysis of studies on HIV serodiscordant couples. Expert Rev PharmacoEcon Outcomes Res. 2016;16(4):489–99.
Weller SC, Davis-Beaty K, Cochrane HIVAIDS, Group. Condom effectiveness in reducing heterosexual HIV transmission. Cochrane Database Syst Reviews. 1996;2012(3).
UNAIDS. Condoms are a critical part of combination prevention. https://www.unaids.org/en/resources/presscentre/featurestories/2021/november/20211122_condoms-critical-part-combination-prevention. Accessed 6 May 2023.
National Statistical Office (NSO). [Malawi] and ICF. Malawi Demographic and Health Survey 2015-16. Zomba, Malawi, and Rockville, Maryland, USA. NSO and ICF. 2017.
Shamu S, Khupakonke S, Farirai T, Slabbert J, Chidarikire T, Guloba G, Nkhwashu N. Knowledge, attitudes and practices of young adults towards HIV prevention: an analysis of baseline data from a community-based HIV prevention intervention study in two high HIV burden districts, South Africa. BMC Public Health. 2020;20:1–10.
Bolarinwa OA, Ajayi KV, Sah RK. Association between knowledge of human immunodeficiency virus transmission and consistent condom use among sexually active men in Nigeria: an analysis of 2018 Nigeria Demographic Health Survey. PLOS Global Public Health. 2022;2(3):e0000223.
Pinchoff J, Boyer CB, Mutombo N, Chowdhuri RN, Ngo TD. Why don’t urban youth in Zambia use condoms? The influence of gender and marriage on non-use of male condoms among young adults. PLoS ONE. 2017;12(3):e0172062.
Izudi J, Okello G, Semakula D, Bajunirwe F. Low condom use at the last sexual intercourse among university students in sub-saharan Africa: evidence from a systematic review and meta-analysis. PLoS ONE. 2022 Aug;10(8):e0272692.
Ajayi AI, Omonaiye O, Nwogwugwu C. Barriers and facilitators of consistent condom use among adolescents and young adults in South Africa: A cross-sectional survey. Preprint from Research Square, 31 Mar 2022 https://doi.org/10.21203/rs.3.rs-1485959/v1 PPR: PPR474526.
Ajayi AI, Olamijuwon EO. What predicts self-efficacy? Understanding the role of sociodemographic, behavioural and parental factors on condom use self-efficacy among university students in Nigeria. PLoS One. 2019 Aug 28;14(8):e0221804.
UNAIDS. Condom use declining. https://www.unaids.org/en/resources/presscentre/featurestories/2020/november/20201123_condom-use-declining. Accessed 9 May 2023.
Complacency a concern as AIDS treatment improves in Africa. https://apnews.com/article/uganda-united-nations-health-international-news-east-africa-c45e18a6f0d04cc899b41973f8c19056. Accessed 9 May 2023.
Hurley R. HIV/AIDS: complacency risks reversing progress on ending epidemic, conference hears. BMJ: British Medical Journal (Online). 2018;362.
Aventin Á, Gordon S, Laurenzi C, Rabie S, Tomlinson M, Lohan M, Stewart J, Thurston A, Lohfeld L, Melendez-Torres GJ, Makhetha M. Adolescent condom use in Southern Africa: narrative systematic review and conceptual model of multilevel barriers and facilitators. BMC Public Health. 2021;21(1):1228.
Chimbiri AM. The condom is an ‘intruder’ in marriage: evidence from rural Malawi. Soc Sci Med. 2007;64(5):1102–15.
Tavory I, Swidler A. Condom semiotics: meaning and condom use in rural Malawi. Am Sociol Rev. 2009;74(2):171–89.
Izudi J, Kadengye DT. Effect of comprehensive knowledge of HIV on risky sexual behaviours associated with HIV transmission among adult ugandans: a propensity score-matched analysis. BMJ open. 2022;12(12):e064011.
Jain A, Tobey E, Ismail H, Erulkar A. Condom use at last sex by young men in Ethiopia: the effect of descriptive and injunctive norms. Reproductive Health. 2018;15:1–9.
Njau B, Mwakalo V, Mushi D. Correlates of use of condoms among sexually active youth in Southern Highlands, Tanzania. SAGE open. 2013;3(2):2158244013491406.
Reynolds HW, Luseno WK, Speizer IS. Consistent condom use among men with non-marital partners in four sub-saharan African countries. AIDS Care. 2013;25(5):592–600.
Albarracin J, Albarracin D, Durantini M. Effects of HIV-prevention interventions for samples with higher and lower percents of latinos and Latin americans: a meta-analysis of change in condom use and knowledge. AIDS Behav. 2008;12:521–43.
Albarracín D, Gillette JC, Earl AN, Glasman LR, Durantini MR, Ho MH. A test of major assumptions about behavior change: a comprehensive look at the effects of passive and active HIV-prevention interventions since the beginning of the epidemic. Psychol Bull. 2005;131(6):856.
Darbes L, Crepaz N, Lyles C, Kennedy G, Rutherford G. The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African americans. AIDS. 2008;22(10):1177–94.
Foss A, Hossain M, Vickerman P, Watts C. A systematic review of published evidence on intervention impact on condom use in sub-saharan Africa and Asia. Sex Transm Infect. 2008;83:510–6.
Heeren GA, Jemmott JB III, Ngwane Z, Mandeya A, Tyler JC. A randomized controlled pilot study of an HIV risk-reduction intervention for sub-saharan African university students. AIDS Behav. 2013;17:1105–15.
Medley A, Kennedy C, O’Reilly K, Sweat M. Effectiveness of peer education interventions for HIV prevention in developing countries: a systematic review and meta-analysis. AIDS Educ Prev. 2009;21(3):181–206.
Noar S. Behavioral interventions to reduce HIV-related sexual risk behavior: review and synthesis of meta-analytic evidence. AIDS Behav. 2008;12(3):335–53.
Okafor UO, Crutzen R, Aduak Y, Adebajo S, Van den Borne HW. Behavioural interventions promoting condom use among female sex workers in sub-saharan Africa: a systematic review. Afr J AIDS Res. 2017;16(3):257–68.
Michielsen K, Chersich MF, Luchters S, De Koker P, Van Rossem R, Temmerman M. Effectiveness of HIV prevention for youth in sub-saharan Africa: systematic review and meta-analysis of randomized and nonrandomized trials. Aids. 2010;24(8):1193–202.
Muthoni CN, Kneipp SM, Gichane MW, Caiola CE, Pettifor AE, Williams JR. A systematic review of HIV interventions for young women in sub-saharan Africa. AIDS Behav. 2020;24:3395–413.
Levy E, Kaufman MR, Gidron Y, Deschepper R, Olley BO. Interventions targeting social cognitive determinants of condom use in the general sub-saharan population: a systematic review. Cogent Psychol. 2019;6(1):1637167.
Closson K, Dietrich JJ, Lachowsky NJ, Nkala B, Palmer A, Cui Z, Beksinska M, Smit JA, Hogg RS, Gray G, Miller CL. Sexual self-efficacy and gender: a review of condom use and sexual negotiation among young men and women in Sub-saharan Africa. J Sex Res. 2018;55(4–5):522–39.
Eggers SM, Aarø LE, Bos AE, Mathews C, Kaaya SF, Onya H, de Vries H. Sociocognitive predictors of condom use and intentions among adolescents in three sub-saharan sites. Arch Sex Behav. 2016;45:353–65.
Protogerou C, Johnson BT, Hagger MS. An integrated model of condom use in sub-saharan African youth: a meta-analysis. Health Psychol. 2018;37(6):586.
Kaufman MR, Rimal RN, Carrasco M, Fajobi O, Soko A, Limaye R, Mkandawire G. Using social and behavior change communication to increase HIV testing and condom use: the Malawi BRIDGE Project. AIDS Care. 2014;26(sup1):S46–9.
Saul J, Bachman G, Allen S, Toiv NF, Cooney C, Beamon TA. The DREAMS core package of interventions: a comprehensive approach to preventing HIV among adolescent girls and young women. PLoS ONE. 2018;13(12):e0208167.
Mathur S, Heck CJ, Patel SK, Okal J, Chipeta E, Mwapasa V, Chimwaza W, Musheke M, Mahapatra B, Pulerwitz J, Pilgrim N. Temporal shifts in HIV-related risk factors among cohorts of adolescent girls and young women enrolled in DREAMS programming: evidence from Kenya, Malawi and Zambia. BMJ open. 2022;12(2):e047843.
Pilgrim N, Mwapasa V, Chipeta E, Chimwaza W, Jani N, McClair T, Tenthani L, Mathur S. Evidence to support HIV prevention for adolescent girls and young women (AGYW) and their male partners: results from Malawi dreams studies with AGYW, male partners of AGYW, men living with HIV, and program implementing partners.
Birdthistle I, Kwaro D, Shahmanesh M, Baisley K, Khagayi S, Chimbindi N, Kamire V, Mthiyane N, Gourlay A, Dreyer J, Phillips-Howard P. Evaluating the impact of DREAMS on HIV incidence among adolescent girls and young women: a population-based cohort study in Kenya and South Africa. PLoS Med. 2021;18(10):e1003837.
Crittenden KS, Kaponda CP, Jere DL, McCreary LL, Norr KF. Participation and diffusion effects of a peer-intervention for HIV prevention among adults in rural Malawi. Soc Sci Med. 2015;133:136–44.
Mbeba MM, Kaponda CP, Jere DL, Kachingwe SI, Crittenden KS, McCreary LL, Norr JL, Norr KF. Peer group intervention reduces personal HIV risk for Malawian health workers. J Nurs Scholarsh. 2011;43(1):72–81.
Dancy BL, Jere DL, Kachingwe SI, Kaponda CP, Norr JL, Norr KF. HIV risk reduction intervention for rural adolescents in Malawi. J HIV/AIDS Social Serv. 2014;13(3):271–91.
Kaponda CP, Norr KF, Crittenden KS, Norr JL, McCreary LL, Kachingwe SI, Mbeba MM, Jere DL, Dancy BL. Outcomes of an HIV prevention peer group intervention for rural adults in Malawi. Health Educ Behav. 2011;38(2):159–70.
Bickton FM. Strengthening human resources for health in resource-limited countries: the case of Medic to Medic in Malawi. Malawi Med J. 2019;31(1):99–101.
Kumbani LC, Jere DL, Banda CK, Chang C, Liu L, McCreary LL, Patil CL, Norr KF. A peer group intervention implemented by community volunteers increased HIV prevention knowledge. BMC Public Health. 2023;23(1):1–5.
Jere DL, Banda CK, Kumbani LC, Liu L, McCreary LL, Park CG, Patil CL, Norr KF. A hybrid design testing a 3-step implementation model for community scale-up of an HIV prevention intervention in rural Malawi: study protocol. BMC Public Health. 2018;18:1–10.
Bandura A. Human agency in social cognitive theory. Am Psychol. 1989;44(9):1175.
Hone T, Macinko J, Millett C. Revisiting Alma-Ata: what is the role of primary health care in achieving the Sustainable Development Goals? Lancet. 2018;392(10156):1461–72.
McHugh SM, Riordan F, Curran GM, Lewis CC, Wolfenden L, Presseau J, Lengnick-Hall R, Powell BJ. Conceptual tensions and practical trade-offs in tailoring implementation interventions. Front Health Serv. 2022;2.
Norr K, Kaponda CP, Crittenden KS, Dancy BL, Jere DL, Kachingwe SI, Kafulafula U, McCreary LL, Mbeba MM, Norr JL, Talashek ML. A primary health care intervention to mobilize health workers for HIV prevention in Malawi. Prim Health Care Res Dev. 2006;7(4):318–30.
SAS 9. 4 Software overview for the customer. https://support.sas.com/software/94/index.html. Accessed 6 May 2023.
Ochillo MA, Van Teijlingen E, Hind M. Influence of faith-based organisations on HIV prevention strategies in Africa: a systematic review. Afr Health Sci. 2017;17(3):753–61.
Jobson G, Khoza S, Mbeng R, Befula N, Struthers HE, Kerongo G, Peters RP. Bridging the gap: reaching men for HIV testing through religious congregations in South Africa. J Acquir Immune Defic Syndr. 2019;81(5):e160.
Wiginton JM, King EJ, Fuller AO. We can act different from what we used to’: findings from experiences of religious leader participants in an HIV-prevention intervention in Zambia. Glob Public Health. 2019;14(5):636–48.
Gorbach PM, et al. Effect of computer assisted interviewing on self-reported sexual behavior data in a microbicide clinical trial. AIDS Behav. 2022;17:790–800.
Kelly CA, Soler-Hampejsek E, Mensch BS, Hewett PC; Social desirability bias in sexual behavior reporting: evidence from an interview mode experiment in rural Malawi. International perspectives on sexual and reproductive health., Gorbach PM et al. Effect of computer assisted interviewing on self-reported sexual behavior data in a microbicide clinical trial. AIDS Behav. 2022;17:790–800.
Wallerstein N. Commentary on community-based participatory research and community engaged research in health for journal of participatory research methods. J Participatory Res Methods. 2020;1(1):13274.
Acknowledgements
The authors acknowledge the many contributions of Professor C.P.N. Kaponda, who played a major role in the development of this proposed research before her retirement, and Professor Diana L. Jere, who served as Co-Principal Investigator and coordinated all project activities in Malawi. Dr Kaponda has retired, while Dr. Jere has moved into government service and now serves as the Malawi Ambassador to Ethiopia. We also are deeply grateful for the opportunity to collaborate with community members and district leaders in Phalombe District of Malawi whose many contributions made this implementation project possible.
Funding
This research is funded by the National Institutes of Health, National Institute for Nursing Research, Grant # NR015409. The funders played no role in research design, data collection, data analysis, manuscript write-up, or decision to publish. Any opinions, findings, conclusions, or recommendations expressed in this article are those of the authors alone and do not necessarily reflect the views of the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
This article was designed collaboratively by KFN, CKB, LCK, LLM, and CLP at two Writing Workshops in Malawi and all contributed significantly to the intellectual content of the manuscript. KFN took primary responsibility for drafting the manuscript. LL designed and oversaw statistical analysis and drafted the methods and results sections. CC carried out the analysis. SK coordinated the review of previous research relevant to this study and developed the tables. All authors reviewed and made substantive contributions to two early drafts. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods and procedures in this study were carried out in accordance with all relevant guidelines and regulations in the Declaration of Helsinki as well as any additional ethical guidelines in Malawi and the USA. The University of Illinois at Chicago (Protocol #2015 − 0691) and the University of Malawi (now Kamuzu University of Health Sciences) College of Medicine Research Committee (COMREC; Protocol P.10/15/1815) approved the protocol. Written signed informed consent prior to engaging in any research activities was obtained for every participant. For adolescents under age 18, the legal age of consent for research participation in Malawi, signed parental consent (permission) and youth assent were obtained. A waiver to obtain consent from only one parent or guardian was obtained. Because the youth participants in this study (ages 13–19) were old enough to understand the basics of what they were agreeing to do, the study was explained to the youth and parent or legal guardian together and questions from both parent and youth were answered. Then both parents and youth signed the consent form. To minimize any perceived parental coercion, youth assent was reconfirmed verbally prior to the first data collection when the parent was not present.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12889_2024_18991_MOESM1_ESM.docx
Additional File 1: Demographic and psychosocial factors for the total participants. (Additional File 1.pdf). This file contains the frequencies for all covariates for the total participants at Time 1 (baseline) and also at Times 2 and 3 for time-varying covariates
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Norr, K.F., Banda, C.K., Chang, C. et al. Condom use increased after a peer group intervention implemented by community volunteers in Malawi. BMC Public Health 24, 1483 (2024). https://doi.org/10.1186/s12889-024-18991-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18991-z