Abstract
Background
Primary osteoporosis (POP) is recognized as a “silent disease” and often ignored. This meta-analysis aimed to determine the prevalence of POP in the Chinese population over the past 20 years to raise awareness of the disease’s epidemiology, which is hoped to help prevent and treat the condition better.
Methods
Eight English and three Chinese language databases were searched systematically from January 2002 to December 2023. Relevant data were analysed using Stata 16.0. Meta-regression and subgroup analyses were performed to explore causes of heterogeneity. A funnel plot was further drawn in combination with Egger and Begg tests to determine publication bias.
Results
A total of 45 studies (241,813 participants) were included. The meta-analysis revealed that the overall prevalence of POP in the Chinese population was 18.2% (95% CI: 14.7–21.7%), showing a positive correlation with age. Specifically, prevalence rates were 23.4% (18.3–28.5%) in women and 11.5% (9.1–13.9%) in men. A notable increase was observed within the span of 20 years (16.9% before 2010 and 20.3% in 2011–2020). Notably, regional variations were observed, with southern China reporting a lower prevalence of 16.4% compared to 20.2% in northern China. Meta-regression suggested that sample size significantly influenced the estimation of point prevalence (P = 0.037).
Conclusions
Over the past two decades, there has been an increase in the prevalence of POP within the Chinese population. The growing prevalence of older individuals and women further highlights the urgency for tailored disease prevention and control measures.
Similar content being viewed by others
Background
Osteoporosis is divided into primary osteoporosis (POP) and secondary osteoporosis. POP is a systemic metabolic disease characterized by bone loss, degradation of bone microstructure, increased bone fragility, and susceptibility to fractures [1]. POP is further categorized into postmenopausal osteoporosis (PMOP), senile osteoporosis, and idiopathic osteoporosis. PMOP predominantly affects postmenopausal women, while senile osteoporosis is closely associated with aging. Idiopathic osteoporosis occurs in children and young adults, characterized by an unknown etiology [2].
Today, POP is the most common form of osteoporosis due to natural aging [3, 4]. The latest seventh national population census of China [5] showed that the country has the largest absolute number of older person in the world, at 260 million and 190 million aged above 60 and 65, respectively. Due to this large number of older people, POP poses a serious social problem among the Chinese population [6]. However, in China, there is a high prevalence of osteoporosis with low awareness, only 7% of patients over 50 having awareness [7]. The complications associated with POP include pain, fractures, disability, and reduced quality of life [8]. Fractures caused by POP, in particular, not only affect the patient’s quality of life but also cause serious burdens to families and the healthcare system [9, 10]. Insufficiently addressed, POP and its consequential fractures pose an imminent threat of imposing substantial medical and economic strains on China’s burgeoning aging population [11].
In recent years, nationwide multicenter studies have been conducted to determine the incidence of osteoporosis in China [12, 13], and the prevalence of osteoporosis has been summarized through systematic reviews and meta-analyses [14, 15]. However, these studies have not differentiated between primary and secondary osteoporosis. In addition, recent scholarly attention has been directed towards the age-standardized prevalence of osteoporosis among middle-aged and older individuals [16, 17]. Nonetheless, according to the classification of POP, it extends beyond the confines of the middle-aged and older population. A nuanced examination of POP prevalence across diverse age strata, geographical locales, and gender demographics within China emerges as imperative for fostering heightened awareness and targeted interventions. Therefore, this study systematically examined the prevalence of POP across all age groups in Chinese adults over the last two decades by comprehensively retrieving relevant literature.
Materials and methods
This review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Guidelines [18]. A review of the PROSPERO International Prospective Register of Systematic Reviews revealed no systematic reviews of the prevalence rate of POP in China.
Search strategy
The electronic PubMed, Web of Science, Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), MEDLINE, EMBASE, OVID, Scopus, China National Knowledge Infrastructure (CNKI) (Chinese), Wan Fang (Chinese), and China Science and Technology Journal Database (VIP) (Chinese) databases were used to search relevant studies published from January 1, 2002, to December 31, 2023. The search was supplemented with the “snowball” method for document tracing, along with manual retrieval of articles from preprint servers to access “grey” literature. Subject terms and free words were used in combination as search terms, including “osteoporosis” or “osteopenia” or “OP” or “primary osteoporosis” or “POP” or “bone mineral density” or “brittle bone disease” and “prevalence” or “epidemiology” or “morbidity” or “incidence” and “China” or “Chinese”. The language of publication was limited to English and Chinese.
Literature inclusion and exclusion criteria
The following inclusion criteria were adopted:
-
(i)
Study type: Cross-sectional studies.
-
(ii)
Measurement of POP: Studies utilized dual-energy X-ray absorptiometry (DXA) for the measurement of POP.
-
(iii)
Diagnostic criteria for POP: Studies adhered to the diagnostic criteria outlined by the World Health Organization (WHO), which defines POP as a bone mineral density (BMD) 2.5 standard deviations below the average value, indicated by a T-score of < -2.5 SD.
-
(iv)
Participation: Studies involving populations aged ≥ 20 years, encompassing young adults, postmenopausal women, middle-aged, and older individuals, drawn mainly from community settings. In addition, population with certain diseases (such as hyperthyroidism, hypogonadism, diabetes, rheumatoid arthritis, systemic lupus erythematosus, multiple myeloma, chronic diarrhea, lymphoma, malabsorption, stroke, chronic heart, lung or kidney diseases, etc.), and those taking medications known to affect bone metabolism (including glucocorticoid, antiepileptic drugs, antitumor chemotherapeutics and excessive thyroid hormone, etc.) were explicitly excluded in the original articles.
-
(v)
Outcomes: Prevalence of POP or osteoporosis. The prevalence rates were reported with age stratification in five-year increments or in multiples of five years (e.g., 20–24 years, 25–29 years, or 20–29 years, and 30–39 years).
The exclusion criteria were as follows:
-
(i)
Studies conducted in a population in which special groups or occupations were excluded (e.g., hospitalized patients and a population working in an environment with lead, cadmium, and aluminum).
-
(ii)
Reviews, commentaries, and case reports.
-
(iii)
Studies with incomplete data, and sample sizes of less than 100 participants.
Literature screening and data extraction
Two reviewers, both trained in systematic review methodologies, conducted a comprehensive search of databases for relevant articles. Independently, they conducted preliminary screenings of titles and abstracts based on predetermined inclusion and exclusion criteria. Articles meeting the inclusion criteria underwent full-text review. Any discrepancies between the researchers were resolved through discussion or, if necessary, by the collective arbitration of the research group.
For each included study, two reviewers independently extracted the following information: (i) Basic Information: This included details such as the first author, year of publication, period of data collection, geographic area (northern or southern), age range, sample size, and the instruments and positions used for BMD measurement. (ii) Calculated Prevalence: This encompassed the number of POP cases and participants in each age-specific group. In cases where specific information was missing, the authors were contacted for clarification. (iii) Assessment of Study Quality: Relevant elements for assessing the quality of the study were also extracted. Any discrepancies between the two reviewers were resolved by a third reviewer.
Quality assessment
The quality assessment of each study considered for further review utilized the quality assessment criteria for cross-sectional studies recommended by the Agency for Healthcare Research and Quality (AHRQ) [19]. These criteria consisted of eleven assessment points, with responses categorized as ‘Yes’ (one point), ‘No’, or ‘Unclear’ (both denoted as zero points). Each study could attain a maximum score of 11 points. Studies accumulating ≤ 5 points were deemed to be of low quality [20].
Data analysis and synthesis
The meta-analysis was conducted using Stata 16.0 software. Firstly, heterogeneity analyses and model selection were performed. A significance level of p < 0.05 and I2 > 50% indicated substantial heterogeneity, leading to the selection of a random effects model (REM). Conversely, if p > 0.05 and I2 < 50%, suggesting lesser heterogeneity, a fixed effects model (FEM) was chosen. Secondly, subgroup analyses were conducted based on various factors, including period of data collection (∼ 2010 and 2011–2020), geographic area (South and North China), gender (men and women), BMD measurement positions (included lumbar spine and other), and age groups (20–29, 30–39, 40–49, 50–59, 60–69, 70–79, ≥ 80 years), both collectively and separately for each gender. Additionally, meta-regression was utilized to explore potential sources of heterogeneity. Thirdly, the impact of individual studies and the stability of the results were assessed using sensitivity analysis. Finally, funnel plots were generated and Egger and Begg tests were conducted to identify publication bias.
Results
Study selection
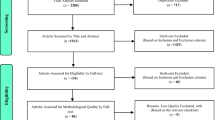
The literature screening process and its outcome are shown in Fig. 1. In brief, 5,713 articles were initially identified, and 1,874 articles were removed for duplication. 3,303 unrelated articles were further excluded after title and abstract screening. After reviewing 536 full-text articles with detailed reading, finally, leaving 45 articles for final analyses.
Characteristics of included studies
Characteristics of the included 45 studies [21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65] are shown in Additional file 1. These studies were published between 2002 and 2023, while data were collected from 1997 to 2021. Among these, 25 studies were conducted in southern China [21,22,23,24,25, 29, 30, 33, 38, 41, 42, 44, 45, 47,48,49, 51,52,53, 55, 56, 59,60,61, 64], 19 studies were in northern China [26,27,28, 31, 32, 34,35,36,37, 39, 40, 46, 50, 54, 57, 58, 62, 63, 65], and only one study was conducted nationwide [43]. Moreover, a total of 23 studies reported the prevalence of the entire population (both men and women) over the age of 20 years [21,22,23, 26,27,28,29, 33, 35,36,37,38,39, 44, 47, 49, 52, 54, 58,59,60, 62, 63]. These 23 studies were analysed for overall data as well as subgroups (period of data collection, gender, area, BMD measurement positions) prevalence. Nineteen studies reported prevalence only of the middle-aged or older population (aged ≥ 40 years) and were thus used for age-specific group analyses [24, 25, 30, 31, 34, 40,41,42, 45, 46, 48, 50, 51, 55,56,57, 61, 64, 65]. Only two studies exclusively reported the prevalence rate among men [32, 65], while seven studies focused on postmenopausal women [25, 30, 40, 48, 55, 57, 61].
The sample size per study ranged from 151 to 75,321 creating a total population of 241,813 participants for this meta-analysis, including 113,613 men and 128,200 women. The point prevalence of POP varied between 1.1% and 63.1%. All studies had a cross-sectional design and all response rates for the survey were above 90%.
Risk of bias in included studies
According to the Agency for Healthcare Research and Quality (AHRQ), among the 45 studies included, nine were categorized as high-quality, while 29 were deemed moderate-quality cross-sectional studies. Additionally, seven studies scored less than five points, indicating low quality. Overall, 84.44% of the included studies demonstrated acceptable quality, falling within the moderate or high categories.
Pooled prevalence rates of osteoporosis
Overall
The meta-analysis of total prevalence estimates of studies with participants aged ≥ 20 years (n = 23, N = 106,725) revealed the prevalence rate of POP in China at 18.2% (95% CI: 14.7–21.7%, Fig. 2), with a high level of heterogeneity (99.6%). Numbers for men were n = 24 (N = 53,746), with 11.5% (95% CI: 9.1–13.9%, Fig. 3) and women were n = 23 (N = 61,879) at 23.4% (95% CI: 18.3–28.5%, Fig. 4), with significant differences between them.
Period of data collection
Period of Data Collection was divided into two groups: before 2010 with the 13 studies and 2011–2020 with eight studies. Meta-analysis results indicated a general upward trend (see Additional file 2). The prevalence rates from studies with data before 2010, and from 2011 to 2020 were 16.9% (95%CI: 11.9–21.8%) and 20.3% (15.1–25.4%), respectively. These data indicated that POP prevalence has increased over the past decade.
Area
The prevalence rate of POP in southern China was 16.4% (95% CI: 12.9–19.9%), which was lower than that in northern China 20.2% (13.4–21.0%) (see Additional file 2).
BMD measurement positions
Most studies measured BMD of lumbar spine, femoral neck, Ward’s triangle and greater trochanter, while only a few studies measured other sites (forearm distal 1/3 of ulna and radius). However, a subgroup analyses of included lumbar spine measurement and results from other anatomical sites revealed an almost similar prevalence rate (18.3% vs. 18.2%) (see Additional file 2).
Sex- and age-specific groups
Among age-specific groups, the prevalence rates of POP generally increased with age, except for the first two age groups (20–29 and 30–39 years old). Specifically, the prevalence was lowest in the 30 to 39 years age group (1.2%), while it peaked in those aged 80 years and older (53.9%). This increasing trend was also evident in other age brackets: 1.4% for 20–29 years, 4.9% for 40–49 years, 16.8% for 50–59 years, 35.2% for 60–69 years, and 44.1% for 70–79 years.
In delineating sex- and age-specific cohorts, the prevalence rates of POP exhibit a discernible consistency across genders and age brackets. Among men, prevalence rates stand at 1.6%, 1.1%, 4.2%, 9.9%, 19.0%, 27.6%, and 38.3%, respectively. Correspondingly, for women, rates are observed at 1.5%, 1.4%, 5.2%, 22.6%, 44.1%, 55.2%, and 63.1%, respectively. Notably, a prevailing trend emerges with higher prevalence rates in women compared to men across most age strata, with the exception noted in the 20–29 age group (see Additional file 2).
Heterogeneity analysis: meta-regression analysis
When assessed collectively, a notable degree of heterogeneity was evident among the studies, with I2 statistics ranging from 63.7 to 99.9%. An exception was observed in the age-specific group 20–29 and men aged 20–29, where the I² values were 8.3% and 0%, respectively (see Additional file 2). Meta-regression analysis (Table 1) revealed that the overall prevalence estimates remained largely unaffected by the period of data collection, geographical area, or BMD measurement positions. However, sample size was found to exert a significant impact on the point prevalence estimate (p = 0.037).
The results of Meta-regression still not fully explain the high level of heterogeneity observed. Alternatively, high heterogeneity may be caused by multiple factors (e.g., sample size, measuring instrument, etc.) with synergistic effects.
Sensitivity analysis
A sensitivity analysis was conducted by systematically excluding each study and re-evaluating the merged statistics. No significant directional changes were noted, indicating the stability of the results (Fig. 5).
Publication bias
No evidence of asymmetry was observed in the funnel plot constructed using data from the 23 studies with participants over the age of 20 (Fig. 6). However, the Begg test (p = 0.086) and Egger test (p = 0.058) suggested a low likelihood of publication bias, although exceptions were noted for certain subgroups (see Additional file 2). The region parameter (urban or rural) was not included as a subgroup in this meta-analysis due to the lack of reporting on participants’ regions of residence in most studies. Additionally, as many studies reported a prevalence of zero for men and women aged 20 to 29 years, it was not possible to calculate publication bias for this age group.
Discussion
This study conducted a systematic review and meta-analysis to determine the prevalence of POP across all age groups of Chinese adults (included young adults, postmenopausal women, middle-aged, and older individuals). The differences of prevalence among different years of data collection, genders, areas and ages were also analysed. Accurate prevalence data assumes paramount significance in fortifying the healthcare system’s efficacy in managing conditions like POP. Such data serves as a cornerstone in devising preventive strategies, formulating robust control measures, and informing strategic decision-making and policy initiatives. In recent years, numerous studies have meticulously investigated and consolidated the prevalence of osteoporosis in China.
This study identified several characteristics of POP in China. Firstly, a meta-analysis involving 106,725 subjects aged over 20 years was conducted. The findings revealed that the overall prevalence of POP in China over the past two decades stood at 18.2%, slightly lower than the global osteoporosis prevalence rate of 19.7% [66]. Notably, women exhibited a significantly higher prevalence rate (23.4%) compared to men (11.5%). Furthermore, the prevalence rate among women surpassed that of men across all age groups except for the 20–29 age bracket. This gender discrepancy can be attributed to men generally experiencing a slower rate of BMD loss [6], while estrogen deficiency in postmenopausal women can accelerate bone loss, contributing to their higher prevalence rate.
Secondly, there has been a discernible rise in the prevalence of POP over the past decade, with rates escalating from 16.9 to 20.3%. This observed trend aligns with the findings of Chen et al. [14], who documented a pronounced increase in osteoporosis prevalence in China from 2008 to 2015. However, the specific drivers behind this upward trajectory were not elucidated by Chen et al. The primary catalyst for this phenomenon is likely the demographic shift towards an aging population [5]. Furthermore, it is conceivable that the surge in POP prevalence is intricately linked to contemporary lifestyle modifications, such as inadequate physical activity, suboptimal calcium intake, and excessive emphasis on weight reduction [67]. Additionally, detrimental modern lifestyle practices, including smoking and excessive alcohol consumption, are well-established risk factors for osteoporosis [68]. Moreover, hormonal imbalances, particularly in postmenopausal women attributable to declining estrogen levels, precipitate accelerated bone resorption and heighten the likelihood of POP.
Thirdly, the prevalence of POP in southern regions is notably lower compared to northern areas. This finding directly contradicts the conclusions drawn by Chen et al. [14], highlighting discrepancies in regional trends of POP prevalence. Some contributing factors may include variations in lifestyle, diet, environmental conditions, and genetics. Notably, the warm and humid climate of southern regions facilitates outdoor physical activities, which can enhance bone density and help prevent osteoporosis [43].
Fourthly, the prevalence of POP observed in this study among the older population was notably elevated, particularly among older women (60–69: 35.2%; 70–79: 44.1%; ≥80: 53.9%), consistent with previous research. Wang et al. [16] reported the age-standardized prevalence of osteoporosis at 33.5% among middle-aged and older Chinese permanent residents, with women consistently exhibiting a higher prevalence compared to men. These findings emphasize the critical importance of prioritizing prevention and management strategies for POP within the older population, especially among older women. The results from studies by He et al. 2016 [69] and Zhu et al. 2022 [15] showed that the prevalence of osteoporosis in older people over 60 years old in China was 36% and 37.7%, respectively. In this study, however, the POP prevalence in 60–69 (35.2%) and 70–79 (44.1%) age group were higher than in previous studies. In much older people aged 80 and above, the POP prevalence was as high as 53.9%, illustrating that increasing age is the most common risk factor for POP [70]. However, a survey showed that only 2.92% older patients treated with anti-osteoporosis drugs [71]. This underscores the importance of non-pharmacological interventions (e.g. Tai Chi exercise or increase consumption of food with higher calcium content) for older patients with poor medication compliance [71, 72].
Finally, the prevalence of POP across various sites for BMD measurement showed close consistency (18.2% vs. 18.3%). This observation suggests that including the forearm as a potential screening site in future osteoporosis screenings could simplify and improve the feasibility of these procedures.
China currently leads the world in the sheer number of older population [5]. Aging, an inevitable factor, emerges as a primary risk element for POP in both genders. Moreover, the incidence of POP closely correlates with modifiable lifestyle factors such as dietary imbalances, sedentary habits, insufficient exposure to sunlight, smoking, and excessive alcohol consumption [73], all of which increase the risk of developing POP. Consequently, recent studies in China have intensified the focus on evaluating the health status of this older demographic.
In recent years, China has undertaken substantial efforts to bolster public awareness and preventive measures against POP. A range of interventions has been implemented, including osteoporosis prevention education, risk factor evaluation, and the identification of high-risk groups through screening initiatives, notably exemplified by the adoption of three-step prevention programs [14]. These initiatives should be further expanded to encompass older populations and communities.
Limitations
This meta-analysis incorporated numerous studies with substantial sample sizes, bolstered by sensitivity analysis to enhance the robustness of the findings. Nevertheless, the study acknowledges several limitations. Firstly, significant heterogeneity was observed, likely stemming from diverse factors such as variations in sample sizes. Moreover, discrepancies in the instruments utilized may contribute to clinical heterogeneity. Secondly, the inclusion criteria limited the analysis to cross-sectional studies, excluding certain original articles that lacked clarity regarding participant characteristics, particularly regarding disease status and medication use affecting bone metabolism. Despite efforts to contact original authors for additional data, such attempts yielded no further information, potentially introducing bias.
Implications for clinical practice and future research
The evidence synthesized in this review underscores the considerable prevalence of POP within China. To advance our understanding and response to this public health challenge, several strategic recommendations emerge. Firstly, optimizing sample sizes is imperative to yield precise epidemiological insights. Initiating comprehensive surveys to ascertain the prevalence of POP, coupled with multifaceted educational campaigns, holds promise in heightening public awareness and engagement with preventive measures. Secondly, embracing a multifaceted research approach encompassing prospective, retrospective, and case-control studies is advocated. Such an approach promises to yield a nuanced understanding of the influence factors of POP, thereby furnishing critical insights for the refinement of clinical interventions. Moreover, prospective investigations or systematic review in emerging areas, such as delineating the prevalence of distinct osteoporosis subtypes (e.g., secondary or primary; senile or postmenopausal), are encouraged. These endeavors serve as indispensable epidemiological cornerstones, empowering tailored prevention and treatment strategies across the osteoporosis spectrum.
Conclusions
In conclusion, the prevalence of POP in the Chinese population stands at 18.2%, with rates increasing gradually with age, and notably higher among females than males, particularly among postmenopausal women who are a high-risk group for POP. It is noteworthy that over the past decade, the prevalence of POP in China has seen a rise due to the surge in the older population. Therefore, urgent action is warranted in the prevention and management of POP. In addition to conventional pharmacological interventions, there is a pressing need to explore simple and feasible non-pharmacological interventions tailored to the older population or postmenopausal women. Following the recommendations of the latest guidelines, targeted exercise programs should be devised and made accessible to community residents.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Abbreviations
- POP:
-
Primary Osteoporosis
- PMOP:
-
Postmenopausal Osteoporosis
- BMD:
-
Bone Mineral Density
- AHRQ:
-
Agency of Healthcare Research and Quality
- REM:
-
Random Effects Model
- FEM:
-
Fixed Effects Model
References
International Osteoporosis Foundation. About Osteoporosis. Accessed March 21. 2024. https://www.osteoporosis.foundation/patients/about-osteoporosis
Aibar-Almazán A, Voltes-Martínez A, Castellote-Caballero Y, Afanador-Restrepo DF, Carcelén-Fraile MDC, López-Ruiz E. Current status of the diagnosis and management of osteoporosis. Int J Mol Sci. 2022;23(16).
Akiyama S, Tanaka T, Udaka J, Inagaki N, Kumagae Y, Chazono M, et al. Factors affecting spine-femur discordance in the percentage of young adult mean on dual-energy X-ray absorptiometry in the elderly population: a retrospective study. BMC Musculoskelet Disord. 2022;23(1):76.
Chinese Medical Association. Guideline for primary care of primary osteoporosis. Chin J Gen Practitioners. 2020;19(4):304–15.
Tu WJ, Zeng X, Liu Q. Aging tsunami coming: the main finding from China’s seventh national population census. Aging Clin Exp Res. 2022;34(5):1159–63.
Bai B, Xie X, Li D, Xu W, LI N, Pang X. Epidemiological studies on osteoporosis in the past five years in China. Chin J Osteoporos. 2018;24(02):253–8.
Osteoporosis and Bone Mineral Disease Branch of Chinese Medical Association. Epidemiological survey of osteoporosis in China and results of the special campaign healthy bones released. Chin J Osteoporos Bone Mineral Res. 2019;12(4):317–8.
Compston JE, McClung MR, Leslie WD. Osteoporos Lancet. 2019;393(10169):364–76.
Briot K, Roux C, Thomas T, Blain H, Buchon D, Chapurlat R, et al. 2018 update of French recommendations on the management of postmenopausal osteoporosis. Joint Bone Spine. 2018;85(5):519–30.
Zmierczak HG, Taylor G, Cundy T. A novel disorder of osteoporosis, osteonecrosis, and metaphyseal fracture. JBMR Plus. 2020;4(6):e10365.
Yu F, Xia W. The epidemiology of osteoporosis, associated fragility fractures, and management gap in China. Arch Osteoporos. 2019;14(1):32.
Wang L, Yu W, Yin X, Cui L, Tang S, Jiang N, et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw Open. 2021;4(8):e2121106.
Cheng X, Zhao K, Zha X, Du X, Li Y, Chen S, et al. Opportunistic screening using low-dose CT and the prevalence of osteoporosis in China: a Nationwide, Multicenter Study. J Bone Min Res. 2021;36(3):427–35.
Chen P, Li Z, Hu Y. Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Public Health. 2016;16(1):1039.
Zhu J, Gao M, Song Q, Ji P, Li H, Zhong M, et al. Prevalence of osteoporosis in Chinese Elderly people:a Meta-analysis. Chin Gen Pract. 2022;25(3):346–52.
Wang J, Shu B, Tang DZ, Li CG, Xie XW, Jiang LJ, et al. The prevalence of osteoporosis in China, a community based cohort study of osteoporosis. Front Public Health. 2023;11:1084005.
Salari N, Darvishi N, Bartina Y, Larti M, Kiaei A, Hemmati M, et al. Global prevalence of osteoporosis among the world older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):669.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Rostom A, Dubé C, Cranney A, Saloojee N, Sy R, Garritty C et al. Celiac disease. Evid Rep Technol Assess (Summ). 2004(104):1–6.
Hu J, Dong Y, Chen X, Liu Y, Ma D, Liu X, et al. Prevalence of suicide attempts among Chinese adolescents: a meta-analysis of cross-sectional studies. Compr Psychiatry. 2015;61:78–89.
Chen C, Xing X, Ye S, Chen R, Xing C, Reng A, et al. A study on bone mineral density of 1162 normal people in Hefei. Chin J Osteoporos. 2008;14(6):419–2140.
Yang C, Zhang S, Wu Y. Bone mineral density and osteoporosis prevalence in 4 123 citizens from Shenzhen. J Clin Rehabilitative Tissue Eng Res. 2008;12(37):7338–40.
Luo C, Zhang Q, Zhou C, Sun J, Huang H, Huang Z, et al. Survey on the present status of primary osteoporosis of Hezhou district of Guangxi. Chin J Osteoporos. 2009;15(5):357–60.
Sun G, Wang H, Lai M, Cai W. Prevalence of primary osteoporosis among people undergoing physical examination in Taizhou. Zhejiang J Prev Med. 2012;24(2):40–1.
Guo H, Yu Y, Chen W, Yu B, deng Q. Analysis of relevant risk factors and prevention of postmenopausal osteoporosis. Chin J Rehabilitation Med. 2011;26(5):424–8.
Yang C, Qiu Q, Zhai X, Cong Z, Wang H, Li S. Investigation of the correlation between bone mineral density and bone metabolism index in healthy adults in Jiaodong Peninsula. Chin J Osteoporos. 2011;17(5):431–49.
Li G, Zhou M, Li C. Investigation and analysis of incidence of osteoporosis for 9735 cases of bone mineral density population in Jilin City region. Chin J Front Med Science(Electronic Version). 2014;6(11):90–3.
Yang H, Qian Z, Li Q, Guo M, Wang C, He X, et al. Investigation of bone mineral density in the distal forearm and analysis of prevalence of osteoporosis in 19609 healthy people in Miyun County of Beijing. Chin J Osteoporos. 2011;17(1):51–5.
Liu H, Chen J, Zhang GL, Chen Z, Lin X. A cross-sectional survey of bone mass and a analysis of risk factors for osteoporosis in 4000 healthy adults in Shaoyang region of Hunan Province. Chin J Osteoporos. 2011;17(12):1087–91.
Tan J, Xiang H, Tan S, Luo Z, Yang M, Luo Y, et al. Survey and analysis of bone density and osteoporosis incidence in Postmenopausal women of Zhuang and Han ethnicities in Guangxi. Guangdong Med J. 2018;39(11):1723–5.
Feng J, Wang X, Zhang T, Cheng L, Wang Q, Cheng X. Analysis of prevalence and influencing factors of abnormal bone density rate in Weifang. Chin J Osteoporos. 2023;29(10):1484–9.
Feng J, Wang X, Sun W, Peng J, Chen G. Measurement of lumbar peak bone mass in healthy men and the investigation of osteoporosis prevalence of all ages. Chin J Practical Intern Med. 2016;36(11):992–4.
Huang J, Song W, Zheng H, Huang H, Feng X. Changes of the bone mineral density and effects of different T-score cut-off on the diagnosis of osteoporosis in healthy people in Chengdu. Chin J Osteoporos. 2016;22(11):1425–934.
Tian L, Yang R, Wei L, Liu J, Yang Y, Shao F, et al. Prevalence of osteoporosis and related lifestyle and metabolic factors of postmenopausal women and elderly men: a cross-sectional study in Gansu province, Northwestern of China. Med (Baltim). 2017;96(43):e8294.
Yang M, Wang S, Wen L, Chen X. Analysis of bone mineral density in normal people in Shenyang and Yingkou of China. Chin J Osteoporos. 2009;15(3):179–82.
Bai M, Ge B, Bai J, Chen K, Zheng R, Yin Y. Analysis of bone mineral density in normal people in Lanzhou area. Chin J Osteoporos. 2008;14(10):736–50.
Zhang M, Li Y, Liu Y, Pan X, Liang B, Liu Z. Study on bone mineral density and prevalence of osteoporosis in 16019 people of Han nationalities in Changchun. Chin J Osteoporos. 2009;15(7):534–7.
Zheng M, Wan Y, Liu G, Gao Y, Pan X, You W, et al. Differences in the prevalence and risk factors of osteoporosis in Chinese urban and rural regions: a cross-sectional study. BMC Musculoskelet Disord. 2023;24(1):46.
Zhang N, Hao Y. The investigation of bone mineral density on 1096 cases Han population in Daqing area and their incidence of osteoporosis. Chin J Osteoporos. 2013;19(10):1095–8.
Li N, Huang Z, Mei J, Liu X, Yang X, Zhang Q, et al. The influence of dietary factors on osteoporosis in Postmenopausal Women. Chin J Public Health. 2011;27(2):182–4.
Zhang P, Feng Y, Zhang Z. Epidemiological investigation of bone mineral density in normal middle-aged and old people in Foshan. Chin J Osteoporos. 2008;14(8):567–9.
Qu P, Deng L, Liu Y, Ma H, Sheng H, Lin X, et al. Prevalence rate of osteopenia and osteoporosis in middle-aged and elderly population in Guangzhou. Chin J Osteoporos. 2002;8(4):314–754.
Zeng Q, Li N, Wang Q, Feng J, Sun D, Zhang Q, et al. The prevalence of osteoporosis in China, a Nationwide, Multicenter DXA Survey. J Bone Min Res. 2019;34(10):1789–97.
Chen Q, Zhang P, Huang C, Liang H. Analysis of bone density by DEXA and prevalence of osteoporosis in southeastern Guangxi. Guangdong Med J. 2018;39(14):2193–59.
Zhao S, Wen Z, Mo X, Zhang X, Li H, Zhang Y, et al. Status and investigation of osteoporosis among peole over 50 years old in the Guangdong-Hong Kong-Macao Greater Bay Area. Chin J Osteoporos. 2023;29(5):665–70.
Wang S, Kong D, Chen J, Rong L, Tang X. Analysis of bone mineral density in 1123 middle-aged and elderly people. Jiangsu Med J. 2016;42(14):1608–10.
Lin S, Peng L, Yao Z, Ma Z, Tan J. Analysis of the results of bone mineral density measurement in healthy regular residents in Shenzhen. Chin J Osteoporos. 2011;17(10):887–91.
Tan S, Luo Y, Luo Z, Yang M, Liu Y, Tan J. Investigation of the epidemic status of postmenopausal osteoporosis in nanning city and the analysis of the influential factors. Chin J Osteoporos. 2017;23(7):942–6.
Lin W, Deng L, Wu H, Wu Z, Ye G, Ouyang Z, et al. Measurement of bone mineral density by DEXA and prevalence rate of osteoporosis in 1530 Guangzhou residents. Chin J Osteoporos. 2003;9(3):257–870.
Luo W, Chen G, Ma X, Tu L. Investigation of bone mineral density and prevalence of bone mass abnormality in middle-aged and elderly healthy subjects in Beijing. J China-Japan Friendsh Hosp. 2021;35(6):328–31.
Chen W, Zhang T, Ding X. Prevalence of osteoporosis and fracture in the elderly in Haikou. Chin J Gerontol. 2010;30(6):824–6.
Yang X, Ding X, Tang W, Mao D, Li C, Chen L. Prevalence of osteoporosis and its influence factors in monitored population in Chongqing. J Pub Health Prev Med. 2022;33(1):90–4.
Yan X, Wang F, Huang Z, Zhu M, Chen Y. Investigation of bone mass density and prevalence rate of osteoporosis in healthy Han and Zhuang people in Nanning region. Chin J Osteoporos. 2003;9(3):268–70.
Zhao X, JIn M, Zhang X. Prevalence of primary osteoporosis(POP) in population parts of Jilin Province. China J Mod Med. 2008;18(8):1084–69.
Xu X. Analysis of risk factors related to osteoporosis in Postmenopausal women and Research on Preventive measures. Jilin Med. 2018;39(5):942–3.
Ding X, Xu X. Prevalence of osteoporosis in the middle-aged and elderly in Chongqing. Lab Med Clin. 2017;14(6):833–4.
Li X, Zhang Q, Xiong C. Incidence and analysis of related risk factors of osteoporosis in Postmenopausal Women. Chin Maternal Child Health Care. 2015;30(29):5047–9.
Liao Y, Peng B, Qiao H. Survey of prevalence of primary osteoporosis (POP) in Kelamayi area of Xinjiang. Chin J Osteoporos. 2010;16(8):598–601586.
Qiu Y, Wu Y, Lan Y, Huang X. Investigation and analysis on bone density of distal forearm in 3796 healthy persons in medical examination in Zhangzhou. Med Pharm J Chin People’s Liberation Army. 2013;25(10):95–7.
Zhou Y, Pan W, Xiao H, Hu Z, Xie H. Changes of bone mineral density and prevalence of osteoporosis in middle-aged and elderly people in Haikou area. Chin J Osteoporos. 2020;26(7):1054–8.
Qin Y, Gu B, Tang M. Analysis of factors influencing osteoporosis incidence in Postmenopausal Women in Jiangsu Province over 3 years. Chin J Med Offic. 2019;47(6):634–7.
Zeng Y, Zhang B, Qiu H, Pan M, Shi J, Liu F. Investigation on the prevalence of osteoporosis in the General Population in Xi’an City. Chin J Clinicians(Electronic Edition). 2012;6(15):173–4.
Ji Z, Ma Y. Characterization of bone mineral density in Beijing urban residents in different age groups:analysis of 3285 cases of bone mineral density results. Chin J Osteoporos. 2011;17(8):687–90.
Wu Z, Wu Y, Hu B, Gao D, Yuan Y, Xu L. Prevalence and related factors of primary osteoporosis in 1263 middle-aged and elderly people in Zhongshan, Guangdong. J New Chin Med. 2013;45(10):51–3.
Fan Z, Lin J, Fei Q, Zhang X, Yang Y, Wu H, et al. Survey on the prevalence of osteoporosis among 1349 community-dwelling elderly males. J Clin Experimental Med. 2018;17(22):2453–6.
Xiao PL, Cui AY, Hsu CJ, Peng R, Jiang N, Xu XH et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporos Int. 2022.
Weaver CM, Gordon CM, Janz KF, Kalkwarf HJ, Lappe JM, Lewis R, et al. The National Osteoporosis Foundation’s position statement on peak bone mass development and lifestyle factors: a systematic review and implementation recommendations. Osteoporos Int. 2016;27(4):1281–386.
Xiao PL, Cui AY, Hsu CJ, Peng R, Jiang N, Xu XH, et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporos Int. 2022;33(10):2137–53.
He L, Sun Y, Yao W, Pan K. The prevalence rate of osteoporosis in the elderly in China between 2010 and 2016: a Meta-analysis of single rate. Chin J Osteoporos. 2016;22(12):1590–6.
Jiang Y, Zhang Y, Jin M, Gu Z, Pei Y, Meng P. Aged-related changes in body composition and association between body composition with bone Mass Density by Body Mass Index in Chinese Han men over 50-year-old. PLoS ONE. 2015;10(6):e0130400.
Liu P, Wen Y, Zhang L, Zhang X, Li H, Gu Y, et al. Cross⁃sectional study on prevalence and treatment of osteoporosis among middle⁃aged and elderly people in Putuo District of Shanghai. J Tongji Univ (Medical Science). 2021;42(1):35–41.
Wang O, Hu Y, Gong S, Xue Q, Deng Z, Wang L, et al. A survey of outcomes and management of patients post fragility fractures in China. Osteoporos Int. 2015;26(11):2631–40.
Tański W, Kosiorowska J, Szymańska-Chabowska A. Osteoporosis - risk factors, pharmaceutical and non-pharmaceutical treatment. Eur Rev Med Pharmacol Sci. 2021;25(9):3557–66.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
FFL performed the methodology, formal analyses, data curation, and was a major contributor in writing the manuscript. VR supervised data curation and analyses, and reviewed and edited the manuscript. PLC analysed and interpreted the data, and reviewed and edited the manuscript. CGN provided guidance on conceptualization and methodology. YZ performed data curation and analysed the data, reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lyu, F.F., Ramoo, V., Chui, P.L. et al. Prevalence rate of primary osteoporosis in China: a meta-analysis. BMC Public Health 24, 1518 (2024). https://doi.org/10.1186/s12889-024-18932-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18932-w