Abstract
Background
The association between bone fracture and cardiovascular diseases is examined in this study. While basic research has established a connection between fractures and heart attacks through the linkage between bones and arteries, population studies have not provided clear evidence. The aim of the present study is to investigate the association between bone fracture and the occurrence of myocardial infarction in a natural population during long-term follow-up.
Methods
A total of 13,196 adult participants with bone fracture history at baseline from the China Health and Nutrition Survey (CHNS) prospective cohort were included in this study. Baseline investigation was performed in 1997–2009 and the outcome was followed up till 2015. Hazard ratios (HRs) and their corresponding 95% confidence intervals (CIs) were calculated using Cox proportional hazards models.
Results
From 1997 to 2015, a total of 329 incident myocardial infarction cases were identified. In univariate and multivariate Cox regression analysis, a history of bone fracture was associated with an increased risk of myocardial infarction incidence in the total population (for the crude model: HR = 2.56, 95% CI 1.83–3.53, P < 0.001; for the multivariate model: HR = 1.43, 95% CI 1.02–1.99, P = 0.036). In the stratified analysis, bone fracture was not associated with an increased risk of incident myocardial infarction in subjects with age < 50 years (HR = 0.71, 95% CI 0.34–1.47, P = 0.356), but significantly associated with an increased risk of incident myocardial infarction in subjects with age ≥ 50 years (HR = 1.80, 95% CI 1.23–2.63, P = 0.003).
Conclusions
It is suggested by the present study that bone fracture may be associated with an increased risk of incident myocardial infarction in the elderly population during long-term follow-up.
Similar content being viewed by others
Background
Myocardial infarction, globally, stands as the foremost cause of mortality. Although traditionally linked to aging, it has increasingly afflicted younger individuals in recent times. The global incidence of myocardial infarction ranges from 1.5 to 2.3 per 1000 person-years, with a particularly notable increase among the young and middle-aged population [1,2,3,4,5]. Similarly, bone fracture poses a significant burden on healthcare systems. A recent Chinese study reported clinical fracture prevalence of 4.1% in men over 40, 4.0% in men over 80, 4.2% in women over 40, and 4.5% in women over 80 years of age [6]. Similar to myocardial infarction, osteoporotic fractures represent another age-related ailment, their occurrence rising with age [6,7,8].
While bone fracture and myocardial infarction are primarily associated with distinct organ systems, they share a connection through the interplay between bones and blood vessels. Fundamental research has shown that arterial calcification constitutes a pivotal pathophysiological mechanism in myocardial infarction, closely linked to atherosclerotic plaque buildup and instability [9], thereby forecasting adverse arterial events, including myocardial infarction [10, 11]. Numerous animal studies have established that osteoporosis and arterial calcification share common molecular pathways [12, 13]. Particularly, smooth muscle cells surrounding blood vessels have the potential to undergo transformation into osteo/chondrogenic cells during arterial calcification [14, 15]. The aging process and chronic kidney disease can induce bone loss, leading to osteoporosis [16, 17], and arterial calcification, resulting in arterial rigidity and plaque instability [18, 19]. Population studies have identified an association between arterial calcification and reduced bone mineral density (even after adjusting for age) [20]. Additionally, correlations have been observed between lower lumbar volumetric bone mineral density and greater coronary artery calcium scores in both women and men, as well as greater abdominal aortic calcium scores in the Multi-Ethnic Study of Atherosclerosis [21]. A case-control study [22], focusing on hip fracture patients matched with those without hip fractures, independently established that hip fractures were associated with an increased risk of subsequent myocardial infarction during follow-up. Another retrospective study [23] demonstrated a correlation between vertebral fractures and myocardial infarction in hemodialysis patients.
Fundamental research has substantiated the potential association between fractures and myocardial infarction through age-related osteoporosis and arterial calcification. Population studies have hinted at this link in high-risk groups, likely due to the relatively low incidence of myocardial infarction in the general population. Nevertheless, research in natural populations is still imperative. In the current study, we have included adult participants from the China Health and Nutrition Survey (CHNS) prospective cohort and have scrutinized the relationship between bone fracture and the occurrence of myocardial infarction in this natural population during long-term follow-up.
Methods
Study population
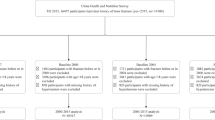
This study utilized longitudinal data from the population-based China Health and Nutrition Survey (CHNS) [24]. The CHNS is an ongoing prospective cohort study comprising over 30,000 participants across China. It is a nationally representative survey that commenced in 1989 and has completed ten survey rounds up to 2015. Detailed survey procedures have been previously documented [25, 26]. Information regarding bone fracture and myocardial infarction was recorded starting from 1997. We analyzed the association between bone fracture and incident myocardial infarction in participants aged 18 years and older during the baseline investigation in surveys 1997–2009 and followed up the outcome till survey 2015. Participants who experienced myocardial infarction before the baseline, were under 18 years of age, or had missing fracture history were excluded (Fig. 1). The research protocol received approval from the Ethics Committee of Beijing Chao-Yang Hospital Affiliated with Capital Medical University in China.
Covariates
Demographic and lifestyle information of participants was gathered through questionnaires, encompassing birth year, gender, medical history, smoking habits, and alcohol consumption. This study was conducted in five different periods, corresponding to five distinct baseline years. Baseline age was determined as the difference between the baseline year and the birth year, with participants under 18 years of age being excluded. Baseline history of hypertension, diabetes, smoking, and alcohol consumption were derived from records before and during the baseline visit. Body mass index (BMI) was computed as the ratio of weight in kilograms to the square of height in meters. Skilled investigators measured body weight and height using standardized measurement techniques.
In 2009, 9549 subjects underwent blood biomarker assessments, including total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), serum creatinine (SCr), among others. For further analysis, we included TC, LDL-C, and estimated glomerular filtration rate (eGFR) to account for the influences of dyslipidemia and kidney function decline. eGFR was calculated using the 2009 Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation [27]: For females, if SCr is ≤ 0.7 mg/dl, eGFR equals 144×(Cr/0.7) −0.329 × (0.993) age, and if SCr is > 0.7 mg/dl, eGFR equals 144×(Cr/0.7) −1.209 × (0.993) age. For males, if SCr is ≤ 0.9 mg/dl, eGFR equals 141×(Cr/0.9) −0.411 × (0.993) age, and if SCr is > 0.9 mg/dl, eGFR equals 141×(Cr/0.9) −1.209 × (0.993) age. These variables were included as both continuous and categorical variables (TC was categorized at 5.2 mmol/L [TC: <5.2 and ≥ 5.2 mmol/L], LDL-C at 3.4 mmol/L [LDL-C: <3.4 and ≥ 3.4 mmol/L], and eGFR at 90 ml/min/1.73 m² [eGFR: <90 and ≥ 90 ml/min/1.73m2]).
Primary exposure and outcome
Bone fracture was defined as a self-reported fracture history. Myocardial infarction was defined as a self-reported diagnosis of myocardial infarction, and the time scale was calculated using baseline year and self-reported incident year of myocardial infarction, for those self-reported incident year missing (< 5%), we filled with the year of first self-reported diagnosis of myocardial infarction. Myocardial infarction served as the primary outcome in this study, with data recorded from the baseline year (not included) up to 2015. Specifically, among the participants, a total of 433 participants experienced myocardial infarction, and 104 occurred prior to 1997 (Fig. 1).
Statistical analyses
All statistical analyses were carried out using R statistical software version 4.2.0, and graphs were generated using GraphPad Prism 6 (GraphPad Software, Inc.). Continuous variables were presented as mean ± standard deviation (SD), while categorical variables were expressed as counts and percentages. Univariate and multivariate Cox regression analyses were employed to assess the relationships between myocardial infarction and bone fracture, along with other variables. The interaction terms between fractures and other covariables were also evaluated. All statistical tests were two-tailed, and P-values less than 0.05 were considered statistically significant.
Results
The baseline characteristics of the participants are displayed in Table 1, both overall and stratified by bone fracture status. Overall, the participants were at the average of 36.0 years old when they were enrolled in the study, with average BMI of 23.1 kg/m2, 8.3% having hypertension, 2.0% having diabetes, 47.8% being males, 23.9% being smokers, and 30.5% being alcohol drinkers. Participants with bone fracture history tended to have higher myocardial infarction incidence, age and BMI, and were more likely to be male, have hypertension, diabetes, smoking and drinking habits. The estimated annual incidence rate is 149, 353, and 138 cases per 100,000 individuals for the total participants, participants with bone fracture, and participants without bone fracture. With increasing age, both the fracture rate and myocardial infarction incidence exhibited significant increases. Participants were categorized into three age groups: <40, 40–60, and ≥ 60 years. In these groups, fracture rates were 3.3%, 7.6%, and 12.3% (P < 0.001), while myocardial infarction incidence was 0.5%, 4.1%, and 13.6% (P < 0.001) (Fig. 2).
In univariate Cox regression analysis, a history of bone fracture was significantly associated with an increased risk of incident myocardial infarction (HR = 2.56, 95% CI 1.83–3.53, P < 0.001). After adjusting for age, gender, BMI, hypertension, diabetes, smoking, and alcohol consumption, a history of bone fracture remained significantly associated with an increased risk of incident myocardial infarction (HR = 1.43, 95% CI 1.02–1.99, P = 0.036) (Table 2). In the stratified analysis, a history of bone fracture was not associated with an increased risk of incident myocardial infarction in subjects with age < 50 years (HR = 0.71, 95% CI 0.34–1.47, P = 0.356), but significantly associated with an increased risk of incident myocardial infarction in subjects with age ≥ 50 years (HR = 1.80, 95% CI 1.23–2.63, P = 0.003), and the interaction between fractures and age was also significant (P for interaction < 0.001); a history of bone fracture was also significantly associated with an increased risk of incident myocardial infarction in subjects with BMI < 24 kg/m2 (HR = 1.62, 95% CI 1.03–2.55, P = 0.035), subjects without diabetes (HR = 1.44, 95% CI 1.01–2.05, P = 0.044), non-smokers (HR = 1.66, 95% CI 1.09–2.51, P = 0.018), non-drinkers (HR = 1.76, 95% CI 1.12–2.76, P = 0.015) (Table 3).
To account for the influences of dyslipidemia and kidney function decline, we included TC, LDL-C, and eGFR data from the 2009 blood marker test. These variables were incorporated as either continuous or categorical variables (TC: <5.2 and ≥ 5.2 mmol/L; LDL-C: <3.4 and ≥ 3.4 mmol/L; eGFR: <90 and ≥ 90 ml/min/1.73 m²). After adjusting for all covariates, including age, gender, BMI, hypertension, diabetes, smoking, alcohol consumption, TC, LDL-C, and eGFR, a history of bone fracture remained significantly associated with an increased risk of incident myocardial infarction (HR = 1.94, 95% CI 1.12–3.33, P = 0.017 in Model 2 [TC, LDL-C, and eGFR were included as continuous variables]; HR = 1.80, 95% CI 1.05–3.10, P = 0.034 in Model 4 [TC, LDL-C, eGFR were included as categorical variables]) (Table 4).
In the analysis of covariates on incident myocardial infarction, an elevated risk of incident myocardial infarction was also associated with higher age (HR = 1.09, 95% CI 1.08–1.10, P < 0.001) and higher BMI (HR = 1.05, 95% CI 1.03–1.07, P < 0.001). A history of hypertension (HR = 1.59, 95% CI 1.22–2.09, P < 0.001) was also associated with an increased risk of incident myocardial infarction (Table 5).
Discussion
The present study has provided several noteworthy insights. Firstly, it showed that a history of bone fracture was significantly associated with an increased risk of myocardial infarction incidence. Secondly, the significant association between fractures and myocardial infarction was observed in the subjects with age ≥ 50 years but not in the subjects with age < 50 years, suggesting that aging plays a pivotal role in the association between fractures and myocardial infarction.
The incidence and estimated annual occurrence of myocardial infarction in this study are consistent with the findings of previous research. In a Danish population [3], over a 17-year period (2005–2021), 116,481 patients experienced their first acute myocardial infarction out of a total population of 4,202,034 to 4,687,295 individuals aged 18 years and older. This indicates a myocardial infarction incidence of 2.5–2.8% over 17 years, which is akin to the 2.5% incidence over 18 years (1997–2015) in this study. These earlier studies [1, 2] also demonstrated a declining trend in myocardial infarction rates, mirroring the present study, with an increasing emphasis on reducing risk factors at both the individual and community levels likely being the primary cause. Studies conducted in Denmark, northern Tanzania, the USA, Europe, and China have also projected similar incidences of myocardial infarction, ranging from 1.5 to 2.3 per 1,000 person-years [1,2,3,4,5].
To identify the association between fractures and incident myocardial infarction, we performed overall and subgroup analysis. The results showed that fractures were significantly associated with incident myocardial infarction, especially in the elderly subjects (age ≥ 50 years). Notably, osteoporotic fracture risk increases with age and is commonly observed in individuals aged over 50 years. The present study indicated that fractures were significantly associated with incident myocardial infarction in subjects more likely to develop osteoporosis. Fractures in younger individuals are rarely caused by age-related osteoporosis. These findings may explain the significant association observed between fractures and myocardial infarction only in the subjects with age ≥ 50 years. Age is the most important confounding factor in the present study. Aging may induce bone loss from normal skeletal system and anomalous deposition in the extra-skeletal system, which usually presents as osteoporotic fractures and heterotopic ossification [16]. Arterial calcification is a form of heterotopic ossification [28]. Arterial calcification may induce plaque instability, which leads to malignant cardiovascular events, such as myocardial infarction [9]. Aging is likely the link between fractures and myocardial infarction.
In a previous case-control study of 8,758 patients diagnosed with hip fractures matched with 35,032 controls without hip fractures [22], hip fractures were independently associated with a higher risk of subsequent acute myocardial infarction during a median 3.2-year follow-up (interquartile range 1.4–5.8 years). However, the myocardial infarction incidence in this study (6.82–8.7 per 1,000 person-years) was significantly higher than in previous studies, suggesting the inclusion of a high-risk population. A retrospective study [23] demonstrated that vertebral fractures (but not femoral or fractures in other sites) were correlated with myocardial infarction in hemodialysis patients but not in pre-dialysis patients with chronic kidney disease (also in a high-risk population). In the present study, within a natural population, we showed that fractures might be associated with an increased risk of incident myocardial infarction in the elderly population during long-term follow-up.
The present study had several limitations. Firstly, the absence of bone mineral density (BMD) or other related data in the CHNS dataset makes it challenging to establish a direct link between osteoporosis and the connection between bone fracture and myocardial infarction. This connection can only be inferred from the findings of other studies. Secondly, in our natural population, the incidence of myocardial infarction was relatively low. As a result, we were unable to conduct age-subgroup analyses in more detail ways.
In conclusion, based on our results and a review of the literature, it appears that the association between fractures and the risk of developing myocardial infarction is more likely to be significant in high-risk populations, particularly in elderly individuals or those with chronic kidney disease. Both aging and chronic kidney disease are recognized risk factors for osteoporosis. Intriguingly, glucocorticoids, another strong risk factor for osteoporosis [29], may also increase the risk of myocardial infarction [30]. These findings have the potential to contribute to the development and refinement of relevant theories.
Data availability
All data generated or analyzed during this study are included in this published article.
References
Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. N Engl J Med. 2010;362(23):2155–65. https://doi.org/10.1056/NEJMoa0908610.
Reynolds K, Go AS, Leong TK, Boudreau DM, Cassidy-Bushrow AE, Fortmann SP, et al. Trends in incidence of hospitalized Acute myocardial infarction in the Cardiovascular Research Network (CVRN). Am J Med. 2017;130(3):317–27. https://doi.org/10.1016/j.amjmed.2016.09.014.
Hertz JT, Madut DB, Rubach MP, William G, Crump JA, Galson SW, et al. Incidence of Acute myocardial infarction in Northern Tanzania: a modeling Approach within a prospective observational study. J Am Heart Association. 2021;10(15):e021004. https://doi.org/10.1161/jaha.121.021004.
Chang J, Deng Q, Guo M, Ezzati M, Baumgartner J, Bixby H, et al. Trends and inequalities in the incidence of Acute myocardial infarction among Beijing Townships, 2007–2018. Int J Environ Res Public Health. 2021;18(23). https://doi.org/10.3390/ijerph182312276.
McManus DD, Gore J, Yarzebski J, Spencer F, Lessard D, Goldberg RJ. Recent trends in the incidence, treatment, and outcomes of patients with STEMI and NSTEMI. Am J Med. 2011;124(1):40–7. https://doi.org/10.1016/j.amjmed.2010.07.023.
Wang L, Yu W, Yin X, Cui L, Tang S, Jiang N, et al. Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw open. 2021;4(8):e2121106. https://doi.org/10.1001/jamanetworkopen.2021.21106.
Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C. The epidemiology of osteoporosis. Br Med Bull. 2020;133(1):105–17. https://doi.org/10.1093/bmb/ldaa005.
Global regional, Global Burden of Disease Study 2019. National burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the. Lancet Healthy Longev. 2021;2(9):e580–92. https://doi.org/10.1016/s2666-7568(21)00172-0.
Sangiorgi G, Rumberger JA, Severson A, Edwards WD, Gregoire J, Fitzpatrick LA, et al. Arterial calcification and not lumen stenosis is highly correlated with atherosclerotic plaque burden in humans: a histologic study of 723 coronary artery segments using nondecalcifying methodology. J Am Coll Cardiol. 1998;31(1):126–33. https://doi.org/10.1016/s0735-1097(97)00443-9.
Ehara S, Kobayashi Y, Yoshiyama M, Shimada K, Shimada Y, Fukuda D, et al. Spotty calcification typifies the culprit plaque in patients with acute myocardial infarction: an intravascular ultrasound study. Circulation. 2004;110(22):3424–9. https://doi.org/10.1161/01.Cir.0000148131.41425.E9.
Taylor AJ, Burke AP, O’Malley PG, Farb A, Malcom GT, Smialek J, et al. A comparison of the Framingham risk index, coronary artery calcification, and culprit plaque morphology in sudden cardiac death. Circulation. 2000;101(11):1243–8. https://doi.org/10.1161/01.cir.101.11.1243.
De Maré A, Opdebeeck B, Neven E, D’Haese PC, Verhulst A. Sclerostin protects against vascular calcification development in mice. J bone Mineral Research: Official J Am Soc Bone Mineral Res. 2022;37(4):687–99. https://doi.org/10.1002/jbmr.4503.
Wei X, Huang X, Liu N, Qi B, Fang S, Zhang Y. Understanding the Stony Bridge between osteoporosis and vascular calcification: impact of the FGF23/Klotho axis. Oxidative Med Cell Longev. 2021;2021:7536614. https://doi.org/10.1155/2021/7536614.
Durham AL, Speer MY, Scatena M, Giachelli CM, Shanahan CM. Role of smooth muscle cells in vascular calcification: implications in atherosclerosis and arterial stiffness. Cardiovascular Res. 2018;114(4):590–600. https://doi.org/10.1093/cvr/cvy010.
Chen PY, Qin L, Li G, Malagon-Lopez J, Wang Z, Bergaya S, et al. Smooth muscle cell reprogramming in aortic aneurysms. Cell Stem Cell. 2020;26(4):542–e557511. https://doi.org/10.1016/j.stem.2020.02.013.
Farr JN, Xu M, Weivoda MM, Monroe DG, Fraser DG, Onken JL, et al. Targeting cellular senescence prevents age-related bone loss in mice. Nat Med. 2017;23(9):1072–9. https://doi.org/10.1038/nm.4385.
Zhang Q, Liu L, Lin W, Yin S, Duan A, Liu Z, et al. Rhein reverses Klotho repression via promoter demethylation and protects against kidney and bone injuries in mice with chronic kidney disease. Kidney Int. 2017;91(1):144–56. https://doi.org/10.1016/j.kint.2016.07.040.
Santhanam L, Liu G, Jandu S, Su W, Wodu BP, Savage W, et al. Skeleton-secreted PDGF-BB mediates arterial stiffening. J Clin Investig. 2021;131(20). https://doi.org/10.1172/jci147116.
Li W, Feng W, Su X, Luo D, Li Z, Zhou Y, et al. SIRT6 protects vascular smooth muscle cells from osteogenic transdifferentiation via Runx2 in chronic kidney disease. J Clin Investig. 2022;132(1). https://doi.org/10.1172/jci150051.
Elmariah S, Delaney JA, O’Brien KD, Budoff MJ, Vogel-Claussen J, Fuster V, et al. Bisphosphonate use and prevalence of valvular and vascular calcification in women MESA (the multi-ethnic study of atherosclerosis). J Am Coll Cardiol. 2010;56(21):1752–9. https://doi.org/10.1016/j.jacc.2010.05.050.
Hyder JA, Allison MA, Wong N, Papa A, Lang TF, Sirlin C, et al. Association of coronary artery and aortic calcium with lumbar bone density: the MESA Abdominal aortic calcium study. Am J Epidemiol. 2009;169(2):186–94. https://doi.org/10.1093/aje/kwn303.
Chiang CH, Liu CJ, Chen PJ, Huang CC, Hsu CY, Chen ZY, et al. Hip fracture and risk of acute myocardial infarction: a nationwide study. J bone Mineral Research: Official J Am Soc Bone Mineral Res. 2013;28(2):404–11. https://doi.org/10.1002/jbmr.1714.
Kwon YE, Choi HY, Oh HJ, Ahn SY, Ryu DR, Kwon YJ. Vertebral fracture is associated with myocardial infarction in incident hemodialysis patients: a Korean nationwide population-based study. Osteoporosis international: a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2020;31(10):1965–1973. https://doi.org/10.1007/s00198-020-05423-y.
Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Reviews: Official J Int Association Study Obes. 2014;15(Suppl 10 1):2–7. https://doi.org/10.1111/obr.12119.
Popkin BM, Du S, Zhai F, Zhang B. Cohort Profile: the China Health and Nutrition Survey–monitoring and understanding socio-economic and health change in China, 1989–2011. Int J Epidemiol. 2010;39(6):1435–40. https://doi.org/10.1093/ije/dyp322.
Wang Y, Howard AG, Adair LS, Wang H, Avery CL, Gordon-Larsen P. Waist Circumference Change is Associated with blood pressure change Independent of BMI change. Obes (Silver Spring Md). 2020;28(1):146–53. https://doi.org/10.1002/oby.22638.
Levey AS, Inker LA, Coresh J. GFR estimation: from physiology to public health. Am J Kidney Diseases: Official J Natl Kidney Foundation. 2014;63(5):820–34. https://doi.org/10.1053/j.ajkd.2013.12.006.
Sutton NR, Malhotra R, St Hilaire C, Aikawa E, Blumenthal RS, Gackenbach G et al. Molecular mechanisms of Vascular Health: insights from vascular aging and calcification. Arteriosclerosis, thrombosis, and vascular biology. 2023;43(1):15–29. https://doi.org/10.1161/atvbaha.122.317332.
Buckley L, Humphrey MB, Glucocorticoid-Induced, Osteoporosis. N Engl J Med. 2018;379(26):2547–56. https://doi.org/10.1056/NEJMcp1800214.
Ozen G, Pedro S, Michaud K. The risk of Cardiovascular events Associated with Disease-modifying Antirheumatic drugs in rheumatoid arthritis. J Rhuematol. 2021;48(5):648–55. https://doi.org/10.3899/jrheum.200265.
Acknowledgements
Not applicable.
Funding
This research was supported by National Natural Science Foundation of China (82170335, 81800304).
Author information
Authors and Affiliations
Contributions
MZ: Formal analysis, Investigation; Data curation, Writing–original draft; XD and XY Conceptualization, Data curation, Investigation, Writing–original draft, Methodology; MZ: Supervision, Visualization, Project administration, Writing–review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Mei-Liang Zheng, Xiang-Peng Du, Xin-Chun Yang, and Mei-Li Zheng declare that they have no conflict of interest.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zheng, ML., Du, XP., Yang, XC. et al. Bone fracture is associated with incident myocardial infarction in long-term follow-up. BMC Public Health 24, 1387 (2024). https://doi.org/10.1186/s12889-024-18897-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18897-w