Abstract
Context
Both the aging of the population and the increase in noncommunicable diseases may influence the progression and outcomes culminating in death, changing the evolution of ischemic heart diseases (IHDs) and their associated causes. Using the multiple causes of death method could help understand the magnitude of these relationships and enable better targeting of investments in health.
Objectives
To evaluate the mortality from IHD in Brazil between 2006 and 2020 using the method of multiple causes and identify differences in the distribution pattern of IHD mortality by sex and geographic region.
Methods
Based on information extracted from death certificates (DCs) obtained from the database of the Department of Informatics of the Unified Health System (DATASUS), we used the multiple causes method to analyze the causes of death associated with IHD when IHD was defined as the underlying cause of death (UC) and the causes of death listed as the UC when IHD was recorded in any other lines of the DC, from 2006 to 2020, in Brazil. Subsequently, the proportion of these causes of death and differences between sexes and geographic regions were evaluated, with statistical relevance analyzed using the chi-square test, and the dependence between factors illustrated using stacked bar charts and small-world network graphs.
Results
When IHD was listed as the UC of death, the most frequent associated causes of death were, in descending order of frequency, acute myocardial infarction (AMI), arterial hypertension (AH), chronic ischemic heart disease (CHID), heart failure (HF), and diabetes mellitus (DM). When IHD was mentioned in any line of the DC, the most frequent UCs of death were AMI followed by DM, CIHD, chronic obstructive pulmonary disease (COPD), stroke, dyslipidemia, and, in the year 2020, COVID-19. The most frequent cause of death in women were DM as the UC and associated cause of death, AH as the UC, and CIHD and Alzheimer's disease as associated causes of death, while the most frequent causes of death in men were substance dependence as the UC and associated cause of death, and cancer as an associated cause of death. The most frequent causes of death were DM and stroke in the North and Northeast, dyslipidemia and obesity in the Midwest, Alzheimer's disease in the South and Southeast, and atherosclerotic heart disease (AHD) and COPD in the South.
Conclusions
Several diseases – including AMI, AH, CIHD, HF, and DM – were the most frequent associated causes of death when IHD was recorded as the UC. In contrast, AMI, DM, CIHD, COPD, and stroke were the most frequent UCs when IHD was listed as an associated cause of death. The degree of these associations varied between sexes and geographic regions.
Similar content being viewed by others
Introduction
The evaluation of mortality based on the underlying cause (UC) of death enables the analysis of the cause that triggered the events that culminated in the death [1]. The evaluation of mortality using the method that considers multiple causes (MCs) of death expands this concept. This method investigates the sequence of events that occurred in association with the UC in addition to the associated causes by including in the analysis all causes mentioned in the death certificate (DC), that is, those present in lines B, C, and D of Part I and Part II [2, 3]. These data may be obtained from DCs but can also be collected from a review of medical records, diagnostic tests, and autopsy reports [3, 4]. The importance of the analysis by MCs has been known for more than 50 years, but this method is still scarcely studied, especially with regard to cardiovascular diseases (CVDs) [4].
From a global perspective, a classic Dutch study from the 1990s confirmed that analyses based on UCs tend to overestimate deaths due to certain etiologies and underestimate the importance of chronic associated diseases, e.g., the weight of arterial hypertension (AH) as the most important associated cause of death in CVDs [3, 5]. A 2015 study from New York observed a higher prevalence of diabetes mellitus (DM) and inflammatory diseases among patients with premature death from ischemic heart disease (IHD); specifically, DM and inflammatory disease were five times more frequent in patients with premature death from IHD compared with individuals of the same age in the general population [6]. More recently, a 2020 Australian study using data from the United States and Australia and analysis with the MC method found that overweight and obesity were associated with a reversal in the downward trend in CVD mortality rates in these countries [7].
A 2007 Brazilian study based on data from 2003 also showed that analyses by UCs underestimate the mortality from chronic diseases, especially that from heart failure (HF) and AH [8]. In 2018, another Brazilian study, that gave rise to our project, based on 2004–2013 data showed that deaths due to AH increased by approximately 400% when the analysis was performed using the MC compared with the UC method [9]. A similar trend was observed in a 2021 study of this same project, in which deaths due to HF increased by almost 300% when the analysis used the MC instead of the UC method [10].
Few studies have analyzed the mortality from IHDs using the MC method over time to evaluate the contribution of other causes to deaths in which IHD was listed as the UC [6, 11,12,13]. With the aging of the population and presenting multiple comorbidities, it is essential to know the causes associated with ischemic heart disease so that we can prevent and treat them completely. Thus, the present study aimed to evaluate the mortality from IHD in Brazil between 2006 and 2020 using the MC method to identify differences in the occurrence of IHD deaths by sex and geographic region.
Methods
This ecological study used data from DCs recorded between 2006 and 2020 in Brazil. The choice for this period was based on information from previous studies that showed improvement in the completion of DC since the early 2000s [14]; this was accomplished after the addition (in 1999) of another line in Part I to include more antecedent causes of death in the DC [3]. Further improvements in the completion of DCs came after a 2004 advertisement campaign by the Brazilian Ministry of Health to reduce the listing of deaths from ill-defined causes [15, 16].
The DC data were obtained from the Mortality Information System (Sistema de Informações sobre Mortalidade, SIM) available on an electronic site maintained by the Department of Informatics of the Unified Health System (Departamento de Informática do Sistema Único de Saúde, DATASUS) of the Brazilian Ministry of Health [17]. Data from 2006 to 2020 were obtained from all Brazilian federative units. The data were downloaded in their original.DBC format and converted to.DBF using the software Tabwin (DATASUS, Brazil). The data were then exported, converted to.CSV, and saved as.XLS in an Excel 2016 spreadsheet (Microsoft Corporation, Seattle, WA, USA). The.XLS format was then used throughout the study.
Next, a filter was applied for each year, and a formula was used to select the Excel rows in which the UCs had International Classification of Disease 10 (ICD-10) codes starting with I2, as detailed in Supplementary Material 1. Manual filtering of all Excel rows was then carried out consecutively to select only the rows in which the UCs had ICD-10 codes I20.0 to I25.9 (IHD group) and exclude the rest of the rows. After this selection, the 13 most frequent causes of death listed in any line when IHD was selected as the UC were identified in Brazil and subsequently stratified by sex and geographic region (North, Northeast, Midwest, Southeast, and South).
Subsequently, the degree of dependence between the causes of death, sexes, and geographic regions was evaluated using small-world networks (igraph package [Csardi & Nepusz, 2006] of R [R Core Team, 2021], in which the path thickness in the graphs is proportional to the number of links between the nodes [18].
For the analysis of the most listed causes of death, ICD-10 codes with similar clinical significance were grouped together. For example, Acute Ischemic Heart Disease (I24), Angina Pectoris (I20), and Acute Myocardial Infarction (I21) were grouped as "acute myocardial infarction" (AMI). Chronic Ischemic Heart Disease (I25) and Generalized Atherosclerosis (I70) were grouped as "atherosclerotic heart disease" (AHD). Heart Failure (I50), Cardiomyopathies (I42), and Pulmonary Edema (J81) were grouped as "heart failure" (HF). Infectious processes, represented by Pneumonia (J189 and J159) and Sepsis (A419), were grouped as "infection." Diabetes Mellitus (DM) was mentioned with several different ICD-10 codes (ICD-10 E10.0 to E14.9), thus requiring unification. After selection, we merged clinically similar codes. Finally, codes with small clinical significance that did not help define the cause of death, e.g., Respiratory Arrest (R09), Respiratory Failure (J96), Cardiac Arrest (I46), Cardiac Arrhythmia (I49 and I48), Other General Symptoms and Signs (R68), Senility (R54), Unspecified Heart Disease (I51), Sudden Death (I46 and R96), and Ill-Defined Causes (R99), were grouped as "garbage codes" (GCs), i.e., ill-defined causes that do not define a UC.
In a second moment, a new data filter was applied for each year, and the Excel rows in which the ICD-10 started with I2 in any line of the DC were selected using the formula described in Supplementary Material 2. This was followed by a manual selection of cases in which IHD (i.e., ICD-10 I20.0 to I25.9) was listed in any of the lines (B, C, D, or Part II). Next, the 16 most frequent causes of death listed in the "UC" column when IHD was selected in lines B, C, D, or Part II were identified and further stratified by sex and region. Small-world network graphs were also used to evaluate the degree of dependence between these causes of death, sexes, and geographic regions [18, 19].
Table S1 shows the number of mentions per DC, by year, and geographic region. There was no relevant increase in the number of mentions per certificate in almost all Geographic Regions. It is also noted that the Southern Region has the lowest averages over time, while the central-western region has the highest averages for the number of mentions per DC.
Finally, in analyses by sex and geographic region, the chi-square test was used to assess the frequency in which the observed event deviated significantly or not (p value) from the frequency in which it was expected.
Results
Table 1 presents the distribution by sex of the 13 causes of death most frequently associated causes listed in any line from DC when IHD (ICD-10 I20.0 to I25.9) was listed as the UC, and the 16 most frequent UCs of death listed when IHD was recorded in one of the lines of the DC. The associations were statistically significant, reflected by p values < 0.05. The most frequent associated causes in both sexes were AMI, HF, and AH. Also noteworthy was the frequency of GCs, which accounted for approximately 13% of the associated causes when IHD was coded as the UC.
Table 2 shows the distribution by geographic region of the 13 associated causes of death most listed in any line from the DC when IHD (ICD-10 I20.0 to I25.9) was listed as the UC of death ("Associated Causes") and the 16 most frequent UCs of death listed when IHD was recorded in one of the lines of the DC ("Underlying Causes"). The frequency of the distribution of all causes of death varied significantly across geographic regions (p < 0.0001 for all). Notably, AMI, HF, and AH presented the highest rates, and GCs were frequent in all regions. The most frequent associated causes per geographic region were AH and AMI in the North and Northeast; DM in the Northeast; GC in the North and Midwest; CIHD, DM, and HF in the Midwest and Southeast; and stroke, CIHD, COPD, and infections in the South. The most frequent UCs of death listed when IHD was recorded in one of the lines of the DC were AMI, DM, and stroke in the North and Northeast regions; COVID-19, AKD, CKD, and infections in the North; DEP in the North and Midwest; ChD and dyslipidemia in the Midwest; HF in the Midwest and South; Alzheimer's disease and CKD in the Southeast and South; infections in the Southeast; and stroke, CIHD, and COPD in the South.
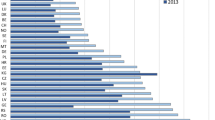
The stacked bar chart in Fig. 1 shows the proportional mortality of the 13 most frequent associated causes listed when IHD was recorded as the UC, stratified by sex and geographic region. The colors, individualized for each associated cause, indicate a similar distribution pattern between the associated causes and a higher proportional frequency of AMI, followed by HF. Between sexes, the associated causes most frequently listed were AH and DM in women and DEP in men. In the analysis by geographic regions, the associated causes more frequently listed were AH in the North and Northeast, DEP in the Midwest, CIHD in the South and Southeast, and COPD in the South.
Associated Causes with Ischemic Heart Diseases by sex and geographic region in Brazil from 2006 to 2020. Stacked bar graph showing the associate causes of death related with ischemic heart disease in Brazil from 2006 to 2020, stratified by sex and geographic region. The colors are individualized for each of the 13 most frequent associated causes listed when ischemic heart disease was recorded as the underlying cause. Abbreviations: AH, arterial hypertension; AKD, acute kidney disease; AMI, acute myocardial infarction; CIHD, chronic ischemic heart disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; DEP, substance dependence; DM, diabetes mellitus; GC, garbage code; HF, heart failure; PE, pulmonary embolism
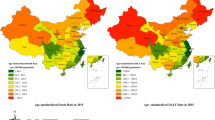
Figure 2 shows the 16 most frequent UCs reported when IHD was listed as associate causes of death, stratified by sex and geographic region. The proportional frequency was highest for AMI across all geographic regions and in both sexes, followed by DM and AHD. Between sexes, the most frequent UCs when IHD was listed in one of the lines of the DC were DM and stroke in women and DEP, HF, and cancer in men. Across geographic regions, the frequency was highest for DM and stroke in the North and Northeast; dyslipidemia and HF in the Midwest; obesity and CKD in the Southeast; and Alzheimer's disease, CIHD, and COPD in the South. During 2020, a short period of the analysis, COVID-19 emerged as one of the most cited UCs, with the highest proportion in the North region. Considering only the last year of the analysis (2020) and DCs in which IHD was listed in one of the lines of the DC, COVID-19 was listed as the UC of death in 2.4% of the DCs in the country and in 5.1% of those in the North, 2.3% in the Northeast, 2.8% in the Midwest, 2% in the Southeast, and 0.5% in the South.
Underlying Causes of death associated with Ischemic Heart Diseases by sex and geographic region in Brazil from 2006 to 2020. Stacked bar chart showing the underlying causes of death associated with ischemic heart disease in Brazil from 2006 to 2020, stratified by sex and geographic region. The colors are individualized for each of the 16 most frequent underlying causes listed when ischemic heart disease was recorded in one of the lines of the death certificate. Abbreviations: AKD, acute kidney disease; Alzheimer's, Alzheimer's disease; AMI, acute myocardial infarction; CA, cancer; ChD, Chagas' disease; CIHD, chronic ischemic heart disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease 2019; DEP, substance dependence; DLP, dyslipidemia; DM, diabetes mellitus; HF, heart failure
The small-world graphs in Fig. 3 a and b show the degree of relationship between IHD as the UC (Fig. 3a and b) and as MCs. The degree of relationship is illustrated by the thickness of the path connecting two nodes ("vertices"), which is proportional to the number of connections between the nodes. This depiction displays the most listed associated causes of death and their relationships between sexes and geographic regions. In Fig. 3, we observe the 13 most frequent associated causes of death listed when IHD was recorded as the UC and their associations with sex and geographic region. As shown, AMI was, proportionally, the most frequently listed associated cause of death in both men and women and in the Northeast region. Other associated causes of death with strong relationship with each sex were PE and CIHD in men and DM in women. Notably, AH was proportionally more associated with the male sex and the Northeast region. Fig 3a and b shows the same relationship with the 16 causes of death listed as the UC when IHD was recorded in any line of the DC. Likewise, the strongest association was with AMI in men and in the Northeast region. Notably, there was a high frequency of mentions of CIHD in the male sex and DM in the female sex.
Small-world network models interconnecting Associated Causes with Ischemic Heart Diseases and Underlying Causes related with Ischemic Heart Diseases with sex and geographic regions. Graph representation of small-world network models of (3) the 13 most frequent associated causes of death listed when IHD was recorded as the underlying cause of death and (4) the 16 most frequent causes of death listed as the underlying cause of death when ischemic heart disease was recorded in any line of the death certificate. Both (3) and (4) are stratified by sex and geographic region. The thickness of the path is proportional to the number of links between nodes. Abbreviations: AH, arterial hypertension; AKD, acute kidney disease; Alzheimer's, Alzheimer's disease; AMI, acute myocardial infarction; CA, cancer; ChD, Chagas' disease; CIHD, chronic ischemic heart disease; CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; COVID-19, coronavirus disease 2019; DEP, substance dependence; DLP, dyslipidemia; DM, diabetes mellitus; F, female sex; GC, garbage code; HF, heart failure; M, male sex; MW, Midwest region; N, North region; NE, Northeast region; PE, pulmonary embolism; S, South region; SE, Southeast region.
Discussion
Several diseases – including AMI, AH, CIHD, HF, and DM – were the most frequent associated causes of death when IHD was recorded as the UC. In contrast, AMI, DM, CIHD, COPD, and stroke were the most frequent UCs when IHD was listed as an associated cause of death. The degree of these associations varied between sexes and geographic regions.
The results of the present study showed that AMI is the cause of death listed most frequently when IHD is recorded as the UC or one of the MCs, as previously demonstrated [12]. Besides AMI, the other most frequent associated causes were AH, CIHD, HF, and DM, which had a similar distribution between sexes. Specifically, between sexes, the most frequent associated causes of death were DEP in men and DM and AH in women. The relevance of AH as an associated cause of CVD was pointed out by Villela et al. in a 2018 Brazilian study and by Santo et al. in a 2011 study on the association of cerebrovascular diseases and AH, which concluded that blood pressure control is associated with a reduction in deaths from IHD and cerebrovascular diseases. [9, 20, 21]
The importance of DM as an associated cause when IHD is listed as the UC was reported in a 2015 Italian study. Fedeli et al. observed that the frequency in which DM was listed increased by up to five times when the authors analyzed DM listed in any line of the DC compared with this cause of death listed only as the UC [5]; this finding is aligned with previous publications showing that DM is underreported when the analysis is limited to the UC [22, 23]. An American study by Quinone et al.confirmed the same finding with IHD, particularly in women and younger individuals [6].
In the analysis by geographic regions in the present study, AH was listed most frequently in the North region. These data corroborate a finding by Ishitani et al., who demonstrated a significant increase in AH mentions when the analysis considering AH as an associated cause of death instead of the UC [3]. The high number of mentions of GCs reflects an inadequate completion of the DC that hinders the analysis of mortality in Brazil. Using data from the 2019 Global Burden of Disease, Johnson et al.mentioned in 2021 that GCs are frequent and harmful to DC analyses and inversely proportional to the social indicators of a community [24]. These codes were proportionally less frequent in the North and Northeast regions, suggesting an improvement in DC completion in these regions [15, 16, 25, 26].
The UCs most frequently associated with IHD when IHD was listed in at least one line of the DC were AMI, DM, CIHD, COPD, stroke, and dyslipidemia. The most frequently listed UCs in this context were DM, CIHD, and Alzheimer's disease among women and DEP and CA in men. Of note, DM is considered one of the main cardiovascular risk factors, and the relationship between DM and IHD has been known for many years, as has been the relevance of DM in the female sex [27,28,29]. The results of the present study indicate that IHD may be underestimated in analyses that consider DCs reporting DM only as the UC. The same bias has been observed when COPD, stroke, and dyslipidemia (which share similar risk factors and pathophysiology with IHD) have been each reported as the UC [7, 30, 31]. A similar finding was reported by Santo et al. in a 2022 Brazilian study with data from 2000 to 2019 [32]. In an analysis by MC, the authors observed that circulatory diseases were the most frequent causes of death associated with deaths from COPD as the UCs, both of which share smoking as an important risk factor, and confounding factors such as age. The association of CVDs with obesity was also reported by Adair et al.in a 2020 Australian study using the MC method; the authors found an increased mortality from CVD as associated cause, and DM, CKD, AH, and dyslipidemia as UCs, as found in the present work [7]. Additionally, a 2004 Brazilian study suggested an association of IHD with obesity, CVD, dyslipidemia, and AH as UCs [33].
In the present analysis by geographic regions, a greater importance of DM and stroke as UCs was observed in the North and Northeast regions, while the Midwest presented proportionally more mentions of dyslipidemia and obesity. These findings corroborate those of a study with data from France, Italy, and the United States, which observed an increased number of mentions of obesity when the MC method was used compared with the UC method [34]. The Southeast and South regions had a greater number of mentions of Alzheimer's disease, which is in line with a 2016 study that suggested an increase of up to 20% in listed mental illnesses (including dementias) when analyzed by MC [35]. These data may indicate better social indicators and longer life expectancy associated with dementia in these last two regions [13]. There was a predominance of CIHD and COPD in the South, which is the region with the highest proportional consumption of tobacco in the country [36]. The predominance of ChD in the Midwest region confirms data from other Brazilian studies, which have shown that this cause of death is underreported in DCs and has IHD as one of its associated causes along with arrhythmias, HF, CVD, and AH [37, 38].
During 2020, a short period in our analysis, COVID-19 was among the main UCs to which IHD was listed as an associated cause; this finding was more frequent in the North region. In 2020, COVID-19 was frequently listed as a UC when IHD was recorded as an associate cause. Notably, COVID-19 ranked fifth among the most relevant causes of death in this period, reinforcing the importance of this disease in worsening the prognosis of patients with IHD [39, 40]. A study by the Brazilian Ministry of Health that used the MC method to analyze the occurrence of CVD when COVID-19 was listed as the UC also observed an increased number of deaths from CVD in this period; as reported in the present study, this finding was also more frequent in the North region of Brazil [41]. These data corroborate the results of a 2022 Brazilian study that highlighted the importance of comorbidities in patients with COVID-19 as an associated cause of death, with the most cited comorbidities being DM, AH, CKD, obesity, and IHD [42].
The fact that mortality analyses rely on the quality of completion of the DC is a limitation of the present study. Since physicians complete the DC according to their knowledge and experience, the DCs could have presented biases and errors depending on the professionals' qualifications and training. Another relevant point is that the format of the DC, which is standardized worldwide, is designed with the main objective of identifying the UC of death and its course; this may discourage professionals from listing previous diseases and risk factors that may have influenced the deaths, thus compromising the analysis of mortality by the MC method [3, 4]. Another limitation of the present study is its observational design, which hinders the assessment of causality.
Future studies are needed for a better understanding of the associations found in the present study and to help guide investments in public health to reduce IHD mortality. There is also a need to further elucidate the differences between sexes and geographic regions to make investments more specific and personalized, yielding better results.
Conclusion
The analysis of deaths from IHD using the MC method reinforced the relevance of this method and identified many causes of death associated with IHD and causes of death with which IHD is associated. Several causes of death, including AMI, AH, AHD, HF, and DM, were associated with IHD when IHD was listed as the UC. On the other hand, IHD was associated with AMI, DM, AHD, COPD, and stroke when these causes of death were listed as the UC. The degree of these associations varied between sexes and across geographic regions. Investments in resources to diagnose and treat these diseases can reduce the number of deaths from IHD, just as better care for IHD can lead to a reduction in deaths from DM, COPD, stroke, dyslipidemia, pneumonia, and obesity.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
Abbreviations
- AH:
-
Arterial hypertension
- AHD:
-
Atherosclerotic heart disease
- AHD:
-
Acute kidney disease
- AMI:
-
Acute myocardial infarction
- CA:
-
Cancer
- CIHD:
-
Chronic ischemic heart disease
- ChD:
-
Chagas' disease
- CKD:
-
Chronic kidney disease
- COPD:
-
Chronic obstructive pulmonary disease
- COVID-19:
-
Coronavirus disease 2019
- CVD:
-
Cardiovascular disease
- DATASUS:
-
Departamento de Informática do Sistema Único de Saúde (Department of Informatics of the Unified Health System)
- DC:
-
Death certificate
- DEP:
-
Substance dependence
- DLP:
-
Dyslipidemia
- DM:
-
Diabetes mellitus
- F:
-
Female sex
- GC:
-
Garbage code
- HF:
-
Heart failure
- I:
-
Infections
- ICD-10:
-
International Classification of Disease 10
- IHD:
-
Ischemic heart disease
- M:
-
Male sex
- MC:
-
Multiple cause
- MW:
-
Midwest region
- N:
-
North region
- NE:
-
Northeast region
- PE:
-
Pulmonary embolism
- S:
-
South region
- SE:
-
Southeast region
- SIM:
-
Sistema de Informações sobre Mortalidade (Mortality Information System)
- UC:
-
Underlying cause
References
- Mackenbach, J.P. et al. Competing causes of death: an analysis using multiple-cause-of-death data from The Netherlands. Am J Epidemiol. 1995. 1;141(5):466–75. doi: https://doi.org/10.1093/oxfordjournals.aje.a117449. PMID: 7879791.
- Wall, M.M. et al. Factors associated with reporting multiple causes of death. BMC Med Res Methodol. 2005. 17;5(1):4. Doi: https://doi.org/10.1186/1471-2288-5-4. PMID: 15655070; PMCID: PMC548504.
Ishitani LH, França E. Uso das causas múltiplas de morte em saúde pública. Inf Epidemiol Sus. 2021;10(4):163–75. https://doi.org/10.5123/S0104-16732001000400003.
- Laurenti, R.; SILVEIRA, M.H. Causas múltiplas de morte. Rev Saúde Pública. 1972. 6:97–102. https://doi.org/10.1590/S0034-89101972000100011.
Fedeli U, et al. Multiple causes of death analysis of chronic diseases: the example of diabetes. Popul Health Metr. 2015;25(13):21. https://doi.org/10.1186/s12963-015-0056-y.PMID:26309427;PMCID:PMC4549015.
Quinones A, et al. Diabetes and ischemic heart disease death in people age 25–54: a multiple-cause-of-death analysis based on over 400 000 deaths from 1990 to 2008 in New York City. Clin Cardiol. 2015;38(2):114–20. https://doi.org/10.1002/clc.22367.PMID:25716311;PMCID:PMC6711024.
- Adair, T.; LOPEZ, A.D. The role of overweight and obesity in adverse cardiovascular disease mortality trends: an analysis of multiple cause of death data from Australia and the USA. BMC Med. 2020. 4;18(1):199. doi: https://doi.org/10.1186/s12916-020-01666-y. PMID: 32746822; PMCID: PMC7401233.
Santo AH. Potencial epidemiológico da utilização das causas múltiplas de morte por meio de suas menções nas declarações de óbito, Brasil, 2003. Rev Panam Salud Publica. 2007;22(3):178–86.
Villela PB, Klein CH, Oliveira GMM. Cerebrovascular and hypertensive diseases as multiple causes of death in Brazil from 2004 to 2013. Public Health. 2018;161:36–42. https://doi.org/10.1016/j.puhe.2018.04.006. PMID: 29870833.
- Villela, P.B.; Santos, S.C.; Oliveira, G.M.M. Heart failure quantified by underlying cause and multiple cause of death in Brazil between 2006 and 2016. BMC Public Health. 2021. 15;21(1):2100. doi: https://doi.org/10.1186/s12889-021-12173-x. PMID: 34781911; PMCID: PMC8594227.
- Rahimi, K. et al. Mortality from heart failure, acute myocardial infarction and other ischaemic heart disease in England and Oxford: a trend study of multiple-cause-coded death certification. J Epidemiol Community Health. 2015. 69(10):1000–5. Doi: https://doi.org/10.1136/jech-2015-205689. Epub 2015 Jul 1. PMID: 26136081; PMCID: PMC4602272.
Goldacre MJ, Roberts SE, Griffith M. Multiple-cause coding of death from myocardial infarction: population-based study of trends in death certificate data. J Public Health Med. 2003;25(1):69–71. https://doi.org/10.1093/pubmed/fdg014. PMID: 12669922.
- Bastos, L.A.V.M. et al. Mortality from diseases of the circulatory system in Brazil and its relationship with social determinants focusing on vulnerability: an ecological study. BMC Public Health. 2022. 20;22(1):1947. doi: https://doi.org/10.1186/s12889-022-14294-3. PMID: 36266678; PMCID: PMC9583513.
Ferreira LCM, et al. Mortality Due to Acute Myocardial Infarction in Brazil from 1996 to 2016: 21 Years of Disparities in Brazilian Regions - ABC Cardiol. Arq Bras Cardiol. 2020;115(5):849–59. https://doi.org/10.36660/abc.20190438.PMID:33295447;PMCID:PMC8452190.
Santo AH, Pinheiro CE. Reavaliação do potencial epidemiológico das causas múltiplas de morte no Brasil. Revista Ibero-Americana de Humanidades, Ciências e Educação. 2022;8(1):2675–3375. https://doi.org/10.51891/rease.v8i1.4008.
- Teixeira, R.A. et al. Quality of cause-of-death data in Brazil: Garbage codes among registered deaths in 2000 and 2015. Rev Bras Epidemiol. 2019. 28;22Suppl 3(Suppl 3):e19002.supl.3. doi: https://doi.org/10.1590/1980-549720190002.supl.3. PMID: 31800854.
- Departamento de informática do sistema único de saúde (datasus). Disponível em: http://www2.datasus.gov.br/DATASUS/index.php?area=0901&item=1&acao=26&pad= 31655. Acesso em: 03 jun 2022.
- Csardi, G.; Nepusz, T. The igraph software package for complex network research. InterJournal. Complex Systems 1695. 2006.
- Team, R Core. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. MSOR connections 1 (2014): n. pag.
- Furukawa, T.S.; Santo, A.H.; Mathias, T.A. Multiple causes of death related to cerebrovascular diseases in the State of Parana, Brazil. Rev Bras Epidemiol. 2011. 14(2):231–9. English, Portuguese. doi: https://doi.org/10.1590/s1415-790x2011000200005. PMID: 21655690.
Martinez R, et al. Association between population hypertension control and ischemic heart disease and stroke mortality in 36 countries of the Americas, 1990–2019: an ecological study. Rev Panam Salud Publica. 2022;16(46): e143. https://doi.org/10.26633/RPSP.2022.143.PMID:36133429;PMCID:PMC9484333.
- KIM, D. et al. Trends in overall, cardiovascular and cancer-related mortality among individuals with diabetes reported on death certificates in the United States between 2007 and 2017. Diabetologia. 2019. 62(7):1185–1194. doi: https://doi.org/10.1007/s00125-019-4870-9. Epub 2019 Apr 22. PMID: 31011776; PMCID: PMC7063897.
Rodriguez F, et al. Diabetes-attributable mortality in the United States from 2003 to 2016 using a multiple-cause-of-death approach. Diabetes Res Clin Pract. 2019;148:169–78. https://doi.org/10.1016/j.diabres.2019.01.015. Epub 2019 Jan 11 PMID: 30641162.
- Johnson, S.C. et al. GBD Cause of Death Collaborators; Lopez AD, Murray CJL, Naghavi M. Public health utility of cause of death data: applying empirical algorithms to improve data quality. BMC Med Inform Decis Mak. 2021. 2;21(1):175. doi: https://doi.org/10.1186/s12911-021-01501-1. PMID: 34078366; PMCID: PMC8170729.
Ishitani LH, et al. Desigualdade social e mortalidade precoce por doenças cardiovasculares no Brasil. Rev Saúde Pública. 2006;40(4):684–91. https://doi.org/10.1590/S0034-89102006000500019.
- Gaui, E.N.; Klein, C.H.; OLiveira, G.M.M. Proportional Mortality due to Heart Failure and Ischemic Heart Diseases in the Brazilian Regions from 2004 to 2011. Arq Bras Cardiol. 2016. 107(3):230–238. doi: https://doi.org/10.5935/abc.20160119. PMID: 27533259; PMCID: PMC5053191.
Kannel WB, Mcgee DL. Diabetes and Cardiovascular Disease: The Framingham Study. JAMA. 1979;241(19):2035–8. https://doi.org/10.1001/jama.1979.03290450033020. PMID: 430798.
Cheng WS, et al. Sensitivity and specificity of death certificates for diabetes: as good as it gets? Diabetes Care. 2008;31(2):279–84. https://doi.org/10.2337/dc07-1327.PMID:17959866;PMCID:PMC2654202.
Pedersen LR, et al. Risk Factors for Myocardial Infarction in Women and Men: A Review of the Current Literature. Curr Pharm Des. 2016;22(25):3835–52. https://doi.org/10.2174/1381612822666160309115318. PMID: 26956230.
André S, et al. GI DPOC-Grupo de Interesse na Doença Pulmonar Obstrutiva Crónica. COPD and Cardiovascular Disease Pulmonology. 2019;25(3):168–76. https://doi.org/10.1016/j.pulmoe.2018.09.006. PMID: 30527374.
Ileri C, et al. Predictors of Concomitant Coronary Artery Disease and Major Cardiovascular Events in Patients with Acute Ischemic Stroke. Neurol India. 2021;69(4):916–22. https://doi.org/10.4103/0028-3886.323893. PMID: 34507412.
Santo AH, Fernandes FLA. Chronic Obstructive Pulmonary Disease-Related Mortality in Brazil, 2000–2019: A Multiple-Cause-of-Death Study. COPD. 2022;19(1):216–25. https://doi.org/10.1080/15412555.2022.2061934. PMID: 35416733.
Rezende EM, Sampaio IBM, Ishitani LH. Causas múltiplas de morte por doenças crônico-degenerativas: uma análise multidimensional. Cad Saúde Pública. 2004;20(5):1223–31. https://doi.org/10.1590/S0102-311X2004000500016.
- BARBIERI, M. et al. Obesity-related mortality in France, Italy, and the United States: a comparison using multiple cause-of-death analysis. Int J Public Health. 2017. 62(6):623–629. doi: https://doi.org/10.1007/s00038-017-0978-1. PMID: 28497238; PMCID: PMC5947997.
Piffaretti C, et al. Quantifying cause-related mortality by weighting multiple causes of death. Bull World Health Organ. 2016;94(12):870–9. https://doi.org/10.2471/BLT.16.172189.PMID:27994280;PMCID:PMC5153928.
Barros AJD, et al. Tabagismo no Brasil: desigualdades regionais e prevalência segundo características ocupacionais. Ciênc saúde coletiva. 2011;16(9):3707–16. https://doi.org/10.1590/S1413-81232011001000008.
Santo AH. Tendência da mortalidade relacionada à doença de Chagas, Estado de São Paulo, Brasil, 1985 a 2006: estudo usando causas múltiplas de morte [Chagas disease-related mortality trends, state of São Paulo, Brazil, 1985 to 2006: a study using multiple causes of death]. Rev Panam Salud Publica. 2009;26(4):299–309. https://doi.org/10.1590/s1020-49892009001000003. PMID: 20107677.
Martins-melo FR, et al. Multiple causes of death related to Chagas’ disease in Brazil, 1999 to 2007. Rev Soc Bras Med Trop. 2012;45(5):591–6. https://doi.org/10.1590/s0037-86822012000500010. PMID: 23152342.
Slater TA, et al. Dying “due to” or “with” COVID-19: a cause of death analysis in hospitalised patients. Clin Med (Lond). 2020;20(5):e189–90. https://doi.org/10.7861/clinmed.2020-0440.PMID:32753516;PMCID:PMC7539724.
Liang C, et al. Coronary heart disease and COVID-19: A meta-analysis. Med Clin (Barc). 2021;156(11):547–54. https://doi.org/10.1016/j.medcli.2020.12.017.PMID:33632508;PMCID:PMC7843088.
- Botelho, M.B. et al. Doenças cardiovasculares como causas associadas de mortalidade durante a pandemia de covid-19 no Brasil: uma análise de causas de morte relatório ministério da saúde. Ministério da Saúde. Universidade de Minas Gerais.
Vasconcelos AMN, et al. Covid Adult Mortality in Brazil: An Analysis of Multiple Causes of Death. Front Public Health. 2022;9: 788932. https://doi.org/10.3389/fpubh.2021.788932.PMID:35111718;PMCID:PMC8801696.
Acknowledgements
Not applicable
Funding
None.
Author information
Authors and Affiliations
Contributions
LAMVB collected the data, performed the analysis and was a major contributor in writing the manuscript. The other authors did also the analysis of the data and contribute to the writing of the manuscript. All authors read and approved the final manuscript.
Author’s information
Luiz Antonio Viegas de Miranda Bastos Mastering at Federal University of Rio de Janeiro, Jose Lucas Peres Bichara Mastering at Federal University of Rio de Janeiro, Basilio de B Pereira BSc, MD, MSc, PhD, DIC and Professor emeritus at Federal University of Rio de Janeiro, Emilia M do Nascimento MD, MSc, PhD and Professor at Rio de Janeiro State University, Eduardo Luiz Viegas de Miranda Bastos graduated in Engineering at Federal University of Rio de Janeiro, Paolo Blanco Villela MD, MSc, PhD, FESC and Professor at Federal University of Rio de Janeiro, Glaucia Maria Moraes de Oliveira MD, MSc, PhD, FACC, FESC and Professor at Federal University of Rio de Janeiro.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. The present work involves data in the public domain, with unrestricted access through the datasus website that did not contain confidential information. No experiment was performed on humans and there was no use of human tissue samples. All methods were carried out in accordance with relevant guidelines and regulations. It belongs to a larger project with ethics and research committee (ERC) – nº 783/09. Informed consent was not necessary for the reasons mentioned above.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bastos, L.A.V.M., Villela, P.B., Bichara, J.L.P. et al. Ischemic heart disease-related mortality in Brazil, 2006 to 2020. A study of multiple causes of death. BMC Public Health 24, 849 (2024). https://doi.org/10.1186/s12889-024-18162-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-18162-0