Abstract
Background
Studies on the association between estimated cardiorespiratory fitness (CRF) and changes in metabolic risk in the Chinese population are limited. This study aims to examine the associations between CRF and changes in metabolic risk.
Subjects and methods
We included 4,862 and 2,700 participants recruited from 28 provinces in the China Health and Retirement Longitudinal Study (CHARLS) in the baseline (Wave 1) and follow-up (Wave 4) analyses, respectively. CRF was calculated using sex-specific longitudinal non-exercise equations. Metabolic indicators included systolic blood pressure (SBP), diastolic blood pressure (DBP), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and fasting plasma glucose (FPG) levels. The metabolic score was calculated as the number of changes in the above metabolic indicators above the 75th percentile of the distribution of changes (equal to or below the 25th percentile for HDL-C).
Results
In the baseline analysis, CRF was negatively associated with SBP, DBP, TG, and FPG, and positively correlated with HDL-C after adjusting for age, smoking status, and drinking status (all P < 0.0001) in both males and females. In the follow-up analysis, higher baseline CRF was significantly related to a decrease in SBP, DBP, TG, FPG, and metabolic score (all P < 0.0005), and increased HDL-C (P < 0.0001) after further adjustment for corresponding baseline metabolic indicators. The associations remained significant after stratification by sex, except for the changes in HDL-C levels in females. Furthermore, improved CRF was associated with favorable changes in DBP, TG, HDL-C, FPG, and metabolic scores in all populations and males. Significant associations between changes in CRF and DBP, TG, and FPG levels were found in females.
Conclusion
Higher baseline CRF and improved CRF were associated with favorable changes in metabolic indicators.
Key points
1. We applied CRF non-exercise equations in a Chinese cohort study.
2. Higher CRF was negatively associated with SBP, DBP, TG, and FPG, and positively correlated with HDL-C at baseline.
3. Higher baseline and improved CRF were related to favorable changes in metabolic indicators.
Similar content being viewed by others
Introduction
Cardiorespiratory fitness (CRF) is a comprehensive indicator of the ability to acquire, transport, and utilize oxygen during exercise, and is quantified by maximal oxygen uptake [1]. Both cross-sectional and prospective studies have reported a significant inverse association between measured CRF and metabolic risk, mainly in European, American, and Canadian populations [2,3,4,5]. In practice, access to CRF is limited because the measurement of CRF using either maximal or submaximal exercise tests requires specialized equipment, trained staff, long time, and high cost. In addition, measurement poses difficulties for the elderly with limited mobility and severe disease [6].
Non-exercise algorithms that estimate CRF using easily measured and self-reported clinical variables, mostly based on cross-sectional studies provide a promising alternative for overcoming the limitations of CRF measurement [7,8,9,10]. Considering that CRF declines nonlinearly with age, Jackson et al.developed a group of sex-specific longitudinal non-exercise equations based on common physical parameters [11]. Metabolic risk has been established to be associated with a higher risk of cardiovascular diseases and mortality, which has become a major public health problem in China [12,13,14]. In the study derived from The China Chronic Disease and Risk Factors Surveillance, the estimated overall prevalence of diabetes was 12.4%, prediabetes was 38.1%, and hypertension was 24.7% for Chinese adults in 2018 [15, 16]. The prevalence of dyslipidemia was 33.8% in community residents aged 35–75 years using data from China-PEACE (Patient-Centered Evaluative Assessment of Cardiac Events) Million Persons Project [12]. There is increasing evidence that estimated CRF is associated with a variety of outcomes, such as cardiovascular disease, cancer, and all-cause mortality, showing comparable results to directly measured CRF [17,18,19,20,21,22,23]. For metabolic health, estimated CRF was inversely associated with the risk of developing hypertension and abnormal glucose levels in the US population [24, 25]. The estimated CRF and its changes predicted the incidence of major biological cardiovascular risk factors, especially hypertension and type 2 diabetes mellitus (T2DM), in the Taiwan MJ Cohort [26]. The Taiwanese participants had higher socioeconomic status, which may affect representativeness of Chinese population. CRF and Metabolic risk changed over time during the follow-up. Longitudinal studies overcoming the limitations of cross-sectional design on the association between estimated CRF and changes in metabolic risk in the Chinese population are limited.
Thus, the study aimed to examine the association between CRF and changes in metabolic risk among middle-aged and older Chinese individuals in a large prospective cohort. This study not only provides evidence for the application of CRF estimation in different populations but also for the recommendations to promote metabolic health and therefore to prevent long-term adverse outcomes for the Chinese population.
Methods
Study population
The China Health and Retirement Longitudinal Study (CHARLS) is a longitudinal cohort study recruiting a nationally representative sample of individuals aged ≥ 45 years from 150 counties of 28 provinces in China [27]. CHARLS was conducted for five rounds (2011, 2013, 2014, 2015, and 2018), among which the 2011 (baseline) and 2015 rounds provided biomarker data, and the 2014 round was the Life History Survey [28]. Details of the sampling method and data collection are reported elsewhere [27]. In this study, we used Wave 1 (2011–2012) as the baseline for biomarker measurements. Wave 4 (2015–2016) was included as a follow-up survey, in which the blood test was performed the second time.
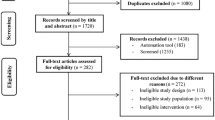
In the baseline study, 9,622 participants aged ≥ 45 years participated in biomarker measurements. Participants who met the following criteria were excluded: (1) missing CRF component data [age, sex, height, weight, waist circumference (WC), resting heart rate (rHR), physical activity level, and smoking]; (2) missing data on metabolic biomarkers [SBP, DBP, TG, HDL-C, and FPG]; (3) treatment for hypertension, diabetes, and dyslipidemia. Ultimately, 4,862 participants were included in the baseline analysis (Wave 1). We excluded individuals with missing data on metabolic biomarkers or using drugs for hypertension, diabetes, and dyslipidemia in Wave 4 to analyze the association between baseline CRF and changes in metabolic indicators based on the baseline analysis (Wave 1). Furthermore, we excluded individuals with missing CRF component data in Wave 4 to explore the associations between changes in CRF and changes in metabolic indicators. Finally, we recruited 2,700 and 2,516 subjects for the two steps in the follow-up analysis, respectively. The study protocol was approved by the ethics committee of Peking University. Informed consent was obtained from all the participants in this cohort.
Background characteristics and anthropometric measurements
In the CHARLS, trained interviewers collected information on demographics, socioeconomic status, health-related behaviors, and history of diseases using a structured questionnaire. Smoking was defined as 1 if the participant reported smoking at a certain point or if they were still smoking. Drinking was defined as 1 if the participant reported having an alcoholic drink in the past or the past 12 months. Marriage was defined as married or partnered. Rural area is coded as follows: 0 indicates the household is located in an urban region and 1 indicates the household is located in a rural region. Education level is coded as follows: 1. Less than lower secondary education, 2. Upper secondary & vocational training, and 3. Tertiary education. Respondents are assigned a code of 1 if the respondent reports an education level of “No Formal Education (Illiterate)”, “Did Not Finish Primary School but can Read”, “Sishu (Private Tutoring)”, “Elementary School” or “Middle School”. If the respondent reports an education level of “High School” or “Vocational School” a code of 2 is assigned. Respondents are assigned a code of 3 if the respondent reports an education level of “Two/three-year College”, “College Grad” or “Post-graduate degree”. We used self-reported weekly physical activity including vigorous physical activity (VPA), moderate physical activity (MPA), and light physical activity (LPA). Subjects who had conducted VPA/MPA/LPA for at least 10 min continuously in a typical week were further asked about the frequency and duration of VPA/MPA/LPA. Active physical activity was defined as a total VPA or MPA of more than 4 days/week. Self-reported hypertension or stroke indicates whether the respondent reported ever having hypertension or stroke. Self-reported heart diseases included heart attack, coronary heart disease, angina, congestive heart failure, or other heart problems. Self-reported diabetes indicates whether the respondent reported having diabetes or high blood sugar. Self-reported dyslipidemia indicates whether the respondent reported ever having dyslipidemia (elevation of low-density lipoprotein cholesterol, TG, and total cholesterol, or a low HDL-C).
Physical measurements were performed by trained staff following a standard protocol. Anthropometric indicators included weight, height, WC, pulse rate, SBP, and DBP. The pulse rate obtained during the blood pressure measurements was approximately equal to the rHR. The BMI was calculated as weight (kg)/height (m)2.
Venous blood samples were collected from each subject after a 12-h overnight fast by professional nurses. Blood TG, HDL-C, and FPG levels were measured.
Assessment of CRF
We estimated CRF in METs by using sex-specific BMI models developed by Jackson et al. [11]. The models used were as follows:
-
Male: CRF = 21.2870 + (age × 0.1654) – (age2 × 0.0023) – (BMI × 0.2318) – (WC × 0.0337) – (rHR × 0.0390) + (active physical activity × 0.6351) – (smoker × 0.4263);
-
Female: CRF = 14.7873 + (age × 0.1159) – (age2 × 0.0017) – (BMI × 0.1534) – (WC × 0.0088) – (rHR × 0.0364) + (active physical activity × 0.5987) – (smoker × 0.2994).
Active physical activity = 1 if the participant was classified as having active physical activity and 0 otherwise. Smoker = 1 if the participant is a current or ever smoker and 0 if not. These models were used to calculate the estimated CRF in baseline and follow-up analyses. The change in CRF per year was calculated as the change in CRF between Waves 4 and 1 divided by the number of years of follow-up. The relative change in CRF was the change in CRF between Wave 4 and Wave 1 divided by baseline CRF.
Calculation of changes in metabolic indicators
Similarly, changes in metabolic indicators per year were calculated by dividing the changes in metabolic indicators between Waves 4 and 1 by the years of follow-up. Relative changes in metabolic indicators were calculated as the change in metabolic indicators between Waves 4 and 1 divided by the corresponding baseline metabolic indicators. Based on the changes in metabolic risk markers over the follow-up period (SBP, DBP, TG, HDL-C, and FPG levels), a metabolic score was developed to represent the changes in the severity indices of metabolic variables [4]. The metabolic score was defined as the number of metabolic indicators with changes above the 75th percentile of the distribution of changes in males and females observed over 4 years in the follow-up analysis (equal to or below the 25th percentile for HDL-C).
Statistical analysis
Continuous variables are described as mean (standard deviation [SD]) and analyzed using the t-test. Categorical variables are described as numbers (%) and compared using the chi-square test.
A linear regression model was used to estimate the coefficient (β) and 95% confidence interval (CI) of CRF associated with the metabolic indicators at baseline and follow-up. To maximize the statistical power, we used continuous CRF and continuous metabolic indicators in this study. In the baseline analysis models, exposure was CRF, and the outcomes were SBP, DBP, TG, HDL-C, and FPG with adjustment for the common demographic and lifestyle confounders including age (continuous), sex, smoking status (current or previous and never), and drinking status (current or previous and never). In the models of follow-up analysis, the exposure was baseline CRF and annual change in CRF, respectively, and the outcomes were annual changes in SBP, DBP, TG, HDL-C, FPG, and metabolic score with further adjustment for corresponding metabolic indicators at baseline. In the sensitivity analyses, we performed follow-up analyses using relative changes in CRF and metabolic variables. We further adjusted marriage (married or partnered and others), rural area (rural area and urban area), education level (Less than lower secondary education, Upper secondary & vocational training, and Tertiary education.), and baseline waist circumference (continuous) in baseline and follow-up analyses. Additionally, we performed analyses only excluding individuals with missing age and sex after full adjustment. Subgroup analyses were performed by separating the populations according to sex in the above models.
Statistical P < 0.05 was defined as a two-tailed significance. All statistical analyses were conducted using the R software (version 4.2.0).
Results
Characteristics of the participants at baseline
A total of 4,862 participants from CHARLS were included in the baseline analysis. The mean age of the subjects was 58.6 years (SD 9.4), and 2,559 (52.6%) were females. The mean CRF was 10.22 METs (SD 2.00) among all participants, and was significantly higher in males (11.80 METs) than in females (8.81 METs).
Table 1 presents the baseline characteristics of the participants stratified by sex. Females were younger, less likely to be smokers and drinkers, lower in education level, higher in BMI and TG levels, lower in DBP levels, and higher in prevalence of dyslipidemia (P < 0.05). There were no significant differences in marriage, rural area, active PA, WC, rHR, SBP, HDL-C, FPG, and the prevalence of hypertension, diabetes, heart diseases, and stroke between males and females.
Characteristics of the participants during follow-up
After a median follow-up of 4 years, 2,700 participants had complete metabolic data and a subgroup of 2,516 subjects had both complete metabolic and CRF component data. The mean CRF level after follow-up was 9.76 METs with an average decrease of 0.17 METs per year (Table 1). The CRF declined significantly faster in men than in females.
The mean levels of SBP and DBP increased 0.51 mmHg/year and 0.49 mmHg/year, respectively, in males and increased 0.16 mmHg/year and 0.17 mmHg/year, respectively, in females (Table 1). In terms of lipid-related indicators, TG levels increased and HDL-C levels decreased slowly in both males and females after the follow-up. Reduced FPG levels were consistently observed in both sexes. The metabolic score reflects the severity of the changes in metabolic risk variables. The proportions of all metabolic scores were similar between male and female subjects.
Association between CRF and metabolic indicators at baseline
Table 2 presents the results of the association between CRF and the metabolic indicators in the baseline analysis. In all populations, CRF was negatively associated with SBP, DBP, TG, and FPG (coefficients per 1-MET increase in CRF ranged from -2.968 to -0.153) and positively correlated with HDL-C (coefficient: 0.101) after adjusting for age, sex, smoking status, and drinking status (all P values < 0.0001). Consistent results were obtained for CRF and all metabolic variables in the subgroup analyses of men and women.
Association between CRF and change in metabolic indicators
In all subjects, higher baseline CRF was significantly associated with decreases in SBP, DBP, TG, FPG, and metabolic score (coefficients per 1-MET increase in CRF ranged from -0.386 to -0.032) and increased HDL-C (coefficient: 0.005, P < 0.0001) after adjusting for all confounders (Table 3). The associations were consistent between males and females except for the changes in HDL-C levels in females.
Improved CRF was associated with favorable changes in DBP, TG, HDL-C, FPG, and metabolic scores in all the populations (Table 3). The results were consistent in males while a significant association was found between changes in CRF and changes in DBP, TG, and FPG in females.
Sensitivity analyses
Sensitivity analyses were conducted on the relative changes in CRF and metabolic variables. Overall, the results presented in this section were consistent with the main results. Baseline CRF was positively associated with relative changes in SBP, DBP, TG, and FPG in all subjects, both males and females, and negatively associated with HDL-C, except in females (Supplementary table 1). Relative changes in CRF were associated with favorable relative changes in DBP and TG, HDL-C, and FPG levels in all populations. The effects were weak for the relative changes in HDL-C levels in males (footnote e inside Supplementary table 1) and relative changes in TG and HDL-C in females (footnote f inside Supplementary table 1).
We further adjusted marriage, rural area, education level, and baseline waist circumference in baseline and follow-up analyses. In baseline analyses, the associations remained significant, but the beta coefficients were slightly attenuated after further adjustment (Supplementary table 2). Similarly, the associations became relatively weaker in the follow-up analyses of baseline CRF and changes in metabolic indicators, especially for changes in blood pressure in men (Supplementary table 3). The protective effect of the change in CRF to the change in DBP remained strong after full adjustment.
Additionally, we performed analyses only excluding individuals with missing age and sex after full adjustment (Supplementary tables 4 and 5). The results were consistent with those presented in Supplementary tables 2 and S3.
Discussion
In this study, we examined the association between estimated CRF and metabolic health in a nationally representative cohort study of a Chinese population. At baseline, higher CRF was positively associated with SBP, DBP, TG, and FPG and negatively associated with HDL-C in both males and females. In the 4-year longitudinal analysis, a higher CRF at baseline was associated with favorable changes in all metabolic variables. The protective effects of improved CRF were significant for favorable changes in most metabolic indicators, except for changes in SBP. After stratification by sex, the effects of higher and improved CRF were slightly weaker in females than in males. Specifically, the beta coefficients between CRF and blood pressure (SBP, DBP) at baseline, as well as the beta coefficients between changes in CRF and changes in DBP, were both less than -2 and -1 mmHg·METs−1, respectively. However, the effect size was relatively weak for associations between CRF and blood glucose and lipids in baseline and follow-up. The above results provided potential evidence that CRF has a greater protective effect on blood pressure in this study. Taken together, these results provide evidence that maintaining high levels of CRF is important for maintaining metabolic health in Chinese individuals, mainly for blood pressure control.
Numerous cross-sectional and longitudinal studies have explored the relationship between measured CRF, cardiometabolic risk factors, and metabolic syndrome (MetS). In a cross-sectional analysis of 38,659 participants from the Aerobics Center Longitudinal Study (ACLS) participants, CRF showed a strong inverse association with MetS in males and females [2]. Using transformed metabolic values, CRF was significantly associated with DBP, TG, and HDL-C (coefficients: -0.07, -0.29, and 0.25 in males; -0.05, -0.17, and 0.19 in females) in both sexes and FPG (-0.09) in males. Similarly, a higher CRF lowered the odds of metabolic syndrome, prediabetes, and T2DM in 1,933 adults aged 40–75 years living in the Netherlands [3]. With a relatively small sample size of 168 Japanese adult males aged 25–64, CRF below 29.84 ml·kg·min−1 (P = 0.028) was a significant risk component for pre-MetS and MetS [29]. In middle-aged and older Japanese men, CRF has inverse associations (OR: 0.46, 0.21–0.98) with diabetes prevalence [30]. However, CRF was inversely related to the prevalence of pre-diabetes/diabetes only in high visceral fat Japanese individuals aged 40–87 years old (P for trend = 0.024) [31]. As for Korean males, measured CRF had a graded inverse association with the prevalence of Mets and its components, remaining unchanged when adjusted for muscle fitness except for HDL-C [32, 33]. Another study included 1,007 Korean adults (488 men and 519 women) a low level of CRF was significantly associated with a higher level of DBP and FPG, a lower level of HDL-C, and a higher prevalence of Mets in men but not in women [34]. The significant associations between CRF and fasting insulin concentrations could be found in men but not in women for Canadian adults [35]. CRF was inversely associated with TG only in Japanese men aged 20–69, while this association was attenuated to nonsignificant when adjusting visceral fat instead of waist circumference [36]. Additionally, low and moderate CRF was independently associated with having ≥ 3 main CVD factors (overweight, hypertension, and dyslipidemia) in 231 urban-dwelling Chinese middle-aged women [37]. The role of gender-specific distribution of adiposity and level of physical activity appears to be important to explain the discrepancy. The estimated CRF was associated with all metabolic indicators at baseline in all population and two sexes in our study. In two studies using CRF as VO2max divided by body mass, CRF was independently related to the prevalence of metabolic syndrome [38, 39]. However, in two other studies that used CRF as VO2max divided by fat-free mass, the association between CRF and metabolic syndrome was weak and non-significant [40, 41]. Further studies are needed on CRF and metabolic health considering the effects of body composition.
Longitudinal studies of measured CRF and changes in metabolic health are limited. In the Quebec Family Study, the CRF of 132 middle-aged individuals was measured using a submaximal exercise test at baseline (1980–1982) and at a follow-up of 6 years (1997–2001) [4]. The results indicated that changes in CRF levels were significantly associated with changes in HDL-C and metabolic syndrome scores (same calculation as the metabolic score in our study). In a longitudinal ACLS study, 3,148 middle-aged adults underwent CRF measurement twice using a maximal treadmill test and were followed up for 6 years after the second examination [5]. Maintaining [0.16 (-0.03–0.46) METs per year] or improving [1.22 (-0.03–0.46) METs per year] CRF lowered the risk of developing hypertension, metabolic syndrome, and hypercholesterolemia. In three studies focusing on Korean men with relatively short follow-up (3.3–5 years), CRF was associated with lower incident risk of hypertension, Mets, and T2DM [42,43,44]. In Japanese male workers, high CRF and consistently high level of CRF was associated with a lower risk of T2DM over an extended follow-up of nearly 20 years [45,46,47]. During the follow-up period of ≤ 16 years (median 1 year), CRF was inversely related to a lower incidence of dyslipidemia with low BMI in Japanese women [48]. In addition, several studies have focused on CRF in younger populations, such as children and young adults. Among 5,869 Chinese children aged 6–13 years, CRF was assessed a 50-m × eight-shuttle run in May 2009 and May 2010 with a relatively short follow-up period [49]. Both higher baseline levels and improved CRF were independently associated with favorable changes in TC, LDL-C, HDL-C, and FPG. In young adults aged 18–30 years, the associations between baseline and improved CRF and cardiovascular disease risk factors were attenuated after adjusting for BMI (baseline study) and weight (follow-up study) during a 15-year follow-up period. The results of our follow-up analysis indicating the protective effects of higher and improved CRF on metabolic health were consistent and comparable with evidence based on measured CRF.
Evidence on estimated CRF and metabolic health is scarce. In cross-sectional studies including Korean adults and older adults, estimated CRF was independently and inversely associated with the prevalence of MetS in both men and women [50, 51]. Compared with quartile 1, HRs (95% CI) of quartiles 2, 3, and 4 were 0.75 (0.61–0.91), 0.54 (0.43–0.68), and 0.42 (0.32–0.55), respectively, during a 6 years’ follow-up in rural Chinese population [52]. In Taiwan MJ cohort, the baseline estimated CRF was inversely associated with the incidence of all CVD risk factors (hypertension, hypercholesterolemia, atherogenic dyslipidemia, T2DM, and systemic inflammation) in both sexes, except hypercholesterolemia in females [26]. The change in estimated CRF over a relatively short time of 1.94 years was related to a lower risk of the above outcomes, especially in men with hypertension and in women with T2DM. Recently, the associations between CRF and abnormal glucose risk as well as hypertension were confirmed in a longitudinal ACLS study [24, 25]. In our study, higher baseline CRF was associated with favorable changes in all metabolic variables, except HDL-C, in females. The inverse relationship between changes in CRF and changes in metabolic indicators was maintained, except for SBP in males and SBP, HDL-C, and metabolic score in females. Overall, the protective effects of CRF and its change to metabolic risk were slightly stronger in males than that in females. The proportions of active physical activity with comparable sample size were similar in two sexes. The difference may result from the adverse changes in body composition (loss of lean mass and body fat redistribution) and other cardiometabolic risks brought by post-menopausal in women [53, 54]. Considering the cross-sectional design of this analysis, further longitudinal studies with longer follow-up periods are needed to explore the changes in CRF and metabolic outcomes.
CHARLS was a prospective cohort study including a nationally representative sample recruited from 28 provinces via multistage probability sampling in China. This study was mainly based on apparently healthy individuals aged ≥ 45 years. Therefore, age and disease status might affect the external validity of the findings. To our knowledge, three previous studies derived from The Rural Chinese Cohort Study and Taiwan MJ Cohort with different socioeconomic status have established that CRF estimated by the same Jackson equations was inversely associated with multiple outcomes including all-cause mortality, CVD mortality, other-cause mortality, T2DM and other CVD risk factors [17, 26, 52]. These studies provided validated evidence for the usage of Jackson equations in the Chinese population. Based on these results, we added the implication of the CRF estimation in a large national representative Chinese cohort.
The major strength of this study is that the metabolic indicators were measured both at baseline and after the 4-year follow-up period, and the longitudinal equations generated more accurate estimates than those derived from cross-sectional studies [17]. The present study has several limitations. First, the four-year follow-up period was relatively short and did not reflect long-term changes in CRF and metabolic health. Both high baseline CRF and improvements in CRF were associated with favorable changes in metabolic factors, suggesting the reliability of our findings. Second, our sample size was relatively small in the follow-up analysis, which included only subjects who underwent two blood tests. This may lead to relatively low statistical power and false negative results. Third, one of the CRF components is self-reported physical activity, which may have induced recall bias and reduced the accuracy of estimating CRF. We used the frequency of physical activity rather than the physical activity index, which may cause a misclassification. Additionally, the initial Jackson equation was validated in a Caucasian population. Participants in this study were older than ACLS, differed in ethnicity, and had a higher proportion of female participants, which may result in misclassification. Finally, some important confounding factors such as diet were not investigated in CHARLS. Therefore, we could not determine the effects of common dietary factors (vegetables, fruits, meat, eggs, etc.) on this study.
Conclusions
Higher baseline CRF and improved CRF over time were associated with favorable changes in metabolic indicators in both males and females in the Chinese population. Our study provides evidence for applying longitudinal equations to estimate CRF and supports the positive effect of CRF on metabolic health. The longitudinal estimation method is readily available from population-based investigations. In practice, routine CRF assessment could be an effective alternative to identify individuals with a higher metabolic risk and improve interventions for metabolic-related chronic diseases, such as T2DM and CVD. Conducting the interventions to improve CRF including improving physical activity, controlling body weight, reducing smoking and balancing the diet would benefit the public in metabolic health and preventing long-term adverse outcomes.
Availability of data and materials
The authors thank the China Center for Economic Research, National School of Development, and Peking University, for providing data. CHARLS could be downloaded from the CHARLS CHARLS (pku.edu.cn).
References
Ross R, Blair SN, Arena R, et al. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134(24):e653–99.
Earnest CP, Artero EG, Sui X, Lee DC, Church TS, Blair SN. Maximal estimated cardiorespiratory fitness, cardiometabolic risk factors, and metabolic syndrome in the aerobics center longitudinal study. Mayo Clin Proc. 2013;88(3):259–70.
van der Velde J, Schaper NC, Stehouwer CDA, et al. Which is more important for cardiometabolic health: sedentary time, higher intensity physical activity or cardiorespiratory fitness? The Maastricht Study. Diabetologia. 2018;61(12):2561–9.
Rhéaume C, Arsenault BJ, Dumas MP, et al. Contributions of cardiorespiratory fitness and visceral adiposity to six-year changes in cardiometabolic risk markers in apparently healthy men and women. J Clin Endocrinol Metab. 2011;96(5):1462–8.
Lee DC, Sui X, Church TS, Lavie CJ, Jackson AS, Blair SN. Changes in fitness and fatness on the development of cardiovascular disease risk factors hypertension, metabolic syndrome, and hypercholesterolemia. J Am Coll Cardiol. 2012;59(7):665–72.
Balady GJ, Arena R, Sietsema K, et al. Clinician’s Guide to cardiopulmonary exercise testing in adults: a scientific statement from the American Heart Association. Circulation. 2010;122(2):191–225.
Wier LT, Jackson AS, Ayers GW, Arenare B. Nonexercise models for estimating VO2max with waist girth, percent fat, or BMI. Med Sci Sports Exerc. 2006;38(3):555–61.
Nes BM, Janszky I, Vatten LJ, Nilsen TI, Aspenes ST, Wisløff U. Estimating V·O 2peak from a nonexercise prediction model: the HUNT study, Norway. Med Sci Sports Exerc. 2011;43(11):2024–30.
Jurca R, Jackson AS, LaMonte MJ, et al. Assessing cardiorespiratory fitness without performing exercise testing. Am J Prev Med. 2005;29(3):185–93.
Cáceres JM, Ulbrich AZ, Panigas TF, Benetti M. Equações de predição da aptidão cardiorrespiratória de adultos sem teste de exercícios físicos. Rev Brasil Cineantropome Desempenho Hum. 2012;14(3):287–95.
Jackson AS, Sui X, O’Connor DP, et al. Longitudinal cardiorespiratory fitness algorithms for clinical settings. Am J Prev Med. 2012;43(5):512–9.
Lu Y, Zhang H, Lu J, et al. Prevalence of dyslipidemia and availability of lipid-lowering medications among primary health care settings in China. JAMA Netw Open. 2021;4(9):e2127573.
Xing L, Tian Y, Jing L, et al. Status and disparities of diabetes among urban and rural residents aged 40 years and older: insight from a population-based study in northeast China, 2017–2019. J Epidemiol Community Health. 2021;75(8):800–8.
Zhu J, Zhang Y, Wu Y, et al. Obesity and dyslipidemia in Chinese adults: a cross-sectional study in Shanghai, China. Nutrients. 2022;14(11):2321.
Zhang M, Shi Y, Zhou B, et al. Prevalence, awareness, treatment, and control of hypertension in China, 2004–18: findings from six rounds of a national survey. BMJ. 2023;380:e071952.
Tu WJ, Xue Y, Nie D. The prevalence and treatment of diabetes in China from 2013 to 2018. JAMA. 2022;327(17):1706.
Zhao Y, Sun H, Qie R, et al. Association between cardiorespiratory fitness and risk of all-cause and cause-specific mortality. Eur J Clin Invest. 2022;52(7):e13770.
Zhang Y, Zhang J, Zhou J, et al. Nonexercise estimated cardiorespiratory fitness and mortality due to all causes and cardiovascular disease: the NHANES III study. Mayo Clin Proc Innov Qual Outcomes. 2017;1(1):16–25.
Wang Y, Chen S, Zhang J, et al. Nonexercise estimated cardiorespiratory fitness and all-cancer mortality: the NHANES III study. Mayo Clin Proc. 2018;93(7):848–56.
Martinez-Gomez D, Guallar-Castillón P, Hallal PC, Lopez-Garcia E, Rodríguez-Artalejo F. Nonexercise cardiorespiratory fitness and mortality in older adults. Med Sci Sports Exerc. 2015;47(3):568–74.
Gander JC, Sui X, Hébert JR, et al. Addition of estimated cardiorespiratory fitness to the clinical assessment of 10-year coronary heart disease risk in asymptomatic men. Prev Med Rep. 2017;7:30–7.
Stamatakis E, Hamer M, O’Donovan G, Batty GD, Kivimaki M. A non-exercise testing method for estimating cardiorespiratory fitness: associations with all-cause and cardiovascular mortality in a pooled analysis of eight population-based cohorts. Eur Heart J. 2013;34(10):750–8.
Artero EG, Jackson AS, Sui X, et al. Longitudinal algorithms to estimate cardiorespiratory fitness: associations with nonfatal cardiovascular disease and disease-specific mortality. J Am Coll Cardiol. 2014;63(21):2289–96.
Patel PH, Gates M, Kokkinos P, Lavie CJ, Zhang J, Sui X. Non-exercise estimated cardiorespiratory fitness and incident hypertension. Am J Med. 2022;135(7):906–14.
Sloan RA, Kim Y, Kenyon J, et al. Association between estimated cardiorespiratory fitness and abnormal glucose risk: a cohort study. J Clin Med. 2023;12(7):2740.
Cabanas-Sánchez V, Artero EG, Lavie CJ, et al. Prediction of cardiovascular health by non-exercise estimated cardiorespiratory fitness. Heart. 2020;106(23):1832–8.
Zhao Y, Hu Y, Smith JP, Strauss J, Yang G. Cohort profile: the China Health and Retirement Longitudinal Study (CHARLS). Int J Epidemiol. 2014;43(1):61–8.
Chen G, Yi Q, Hou L, et al. Transition of hypertriglyceridemic-waist phenotypes and the risk of type 2 diabetes mellitus among middle-aged and older Chinese: a national cohort study. Int J Environ Res Public Health. 2021;18(7):3664.
Kim B, Ku M, Kiyoji T, Isobe T, Sakae T, Oh S. Cardiorespiratory fitness is strongly linked to metabolic syndrome among physical fitness components: a retrospective cross-sectional study. J Physiol Anthropol. 2020;39(1):30.
Wang D, Sawada SS, Tabata H, et al. The combination of cardiorespiratory fitness and muscular fitness, and prevalence of diabetes mellitus in middle-aged and older men: WASEDA’S Health Study. BMC Public Health. 2022;22(1):626.
Usui C, Kawakami R, Tanisawa K, et al. Visceral fat and cardiorespiratory fitness with prevalence of pre-diabetes/diabetes mellitus among middle-aged and elderly Japanese people: WASEDA’S Health Study. PLoS One. 2020;15(10):e0241018.
Ko KJ, Kang SJ, Lee KS. Association between cardiorespiratory, muscular fitness and metabolic syndrome in Korean men. Diabetes Metab Syndr. 2019;13(1):536–41.
Kim J, Lee N, Jung SH, Kim EJ, Cho HC. Independent and joint associations of cardiorespiratory fitness and muscle fitness with metabolic syndrome in Korean men. Metab Syndr Relat Disord. 2011;9(4):273–9.
Hong S, Lee J, Park J, et al. Association between cardiorespiratory fitness and the prevalence of metabolic syndrome among Korean adults: a cross sectional study. BMC Public Health. 2014;14:481.
Kriska AM, Hanley AJ, Harris SB, Zinman B. Physical activity, physical fitness, and insulin and glucose concentrations in an isolated native Canadian population experiencing rapid lifestyle change. Diabetes Care. 2001;24(10):1787–92.
Aoyama T, Asaka M, Ishijima T, et al. Association between muscular strength and metabolic risk in Japanese women, but not in men. J Physiol Anthropol. 2011;30(4):133–9.
Zhu W, Hooker SP, Sun Y, Xie M, Su H, Cao J. Associations of cardiorespiratory fitness with cardiovascular disease risk factors in middle-aged Chinese women: a cross-sectional study. BMC Womens Health. 2014;14:62.
Lee S, Kuk JL, Katzmarzyk PT, Blair SN, Church TS, Ross R. Cardiorespiratory fitness attenuates metabolic risk independent of abdominal subcutaneous and visceral fat in men. Diabetes Care. 2005;28(4):895–901.
Ekblom Ö, Ekblom-Bak E, Rosengren A, Hallsten M, Bergström G, Börjesson M. Cardiorespiratory fitness, sedentary behaviour and physical activity are independently associated with the metabolic syndrome, results from the SCAPIS pilot study. PLoS One. 2015;10(6):e0131586.
Jukarainen S, Holst R, Dalgård C, et al. Cardiorespiratory fitness and adiposity as determinants of metabolic health-pooled analysis of two twin cohorts. J Clin Endocrinol Metab. 2017;102(5):1520–8.
Franks PW, Ekelund U, Brage S, Wong MY, Wareham NJ. Does the association of habitual physical activity with the metabolic syndrome differ by level of cardiorespiratory fitness? Diabetes Care. 2004;27(5):1187–93.
Jae SY, Kurl S, Laukkanen JA, et al. Relation of C-reactive protein, fibrinogen, and cardiorespiratory fitness to risk of systemic hypertension in men. Am J Cardiol. 2015;115(12):1714–9.
Jae SY, Heffernan KS, Kim DK, Park WH, Choi YH, Kim SH. Cardiorespiratory fitness and incident metabolic syndrome in middle-aged Korean men. Ann Hum Biol. 2014;41(5):477–80.
Jae SY, Franklin BA, Choo J, Yoon ES, Choi YH, Park WH. Fitness, body habitus, and the risk of incident type 2 diabetes mellitus in Korean men. Am J Cardiol. 2016;117(4):585–9.
Momma H, Sawada SS, Lee IM, et al. Consistently high level of cardiorespiratory fitness and incidence of type 2 diabetes. Med Sci Sports Exerc. 2017;49(10):2048–55.
Sawada SS, Lee IM, Naito H, Tsukamoto K, Muto T, Blair SN. Muscular and performance fitness and the incidence of type 2 diabetes: prospective study of Japanese men. J Phys Act Health. 2010;7(5):627–32.
Kawakami R, Sawada SS, Lee IM, et al. Long-term impact of cardiorespiratory fitness on type 2 diabetes incidence: a cohort study of Japanese men. J Epidemiol. 2018;28(5):266–73.
Ohta T, Nagashima J, Sasai H, Ishii N. Relationship of cardiorespiratory fitness and body mass index with the incidence of dyslipidemia among Japanese women: a cohort study. Int J Environ Res Public Health. 2019;16(23):4647.
Shang X, Li Y, Xu H, et al. Independent and Interactive associations of fitness and fatness with changes in cardiometabolic risk in children: a longitudinal analysis. Front Endocrinol. 2020;11:342.
Lee I, Kim S, Kang H. Non-exercise based estimation of cardiorespiratory fitness is inversely associated with metabolic syndrome in a representative sample of Korean adults. BMC Geriatr. 2020;20(1):146.
Kim S. Association between cardiorespiratory fitness and metabolic syndrome in Korean older adults. Int J Environ Res Public Health. 2022;19(6):3671.
Zhao Y, Qie R, Han M, et al. Independent and joint associations of non-exercise cardiorespiratory fitness and obesity with risk of type 2 diabetes mellitus in the Rural Chinese cohort study. Nutr Metab Cardiovasc Dis. 2022;32(4):929–36.
Douchi T, Yamamoto S, Yoshimitsu N, Andoh T, Matsuo T, Nagata Y. Relative contribution of aging and menopause to changes in lean and fat mass in segmental regions. Maturitas. 2002;42(4):301–6.
Gohlke-Bärwolf C. Coronary artery disease–is menopause a risk factor? Basic Res Cardiol. 2000;95(Suppl 1):I77–83.
Acknowledgements
All authors thank CHARLS for providing the data. We are grateful to those who designed, conducted, and participated in the study.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Yuanjiao Liu, Jinghan Zhu, Jiazhou Yu, Xuhui Zhang designed this study. Yuanjiao Liu analyzed the data and wrote the manuscript. Zhu and Yu conducted literature review and interpreted the results. Xuhui Zhang revised the manuscript. All the authors have read and approved the final manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval for the study was granted by the Ethical Review Committee of Peking University and was conducted by the National School for Development (China Centre for Economic Research) at Peking University, following the Helsinki guidelines. The Institutional Review Board (IRB) approval number for the main household survey, including anthropometrics, was IRB00001052-11015, and the IRB approval number for biomarker collection was IRB00001052-11014 [28]. Informed consent was obtained from all participants involved in the CHARLS, and all participants signed written informed consent forms. All methods were performed by the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary Table 1.
Associations between baseline CRF and relative change in CRF and relative changes in metabolic indicators.
Additional file 2: Supplementary Table 2.
Associations between CRF and metabolic indicators at baseline after further adjustment.
Additional file 3: Supplementary Table 3.
Associations between CRF and changes in metabolic variables after further adjustment.
Additional file 4: Supplementary Table 4.
Associations between CRF and metabolic indicators at baseline only excluding individuals with missing age and sex after further adjustment.
Additional file 5: Supplementary Table 5.
Associations between CRF and changes in metabolic variables only excluding individuals with missing age and sex after further adjustment.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, Y., Zhu, J., Yu, J. et al. Cardiorespiratory fitness and metabolic risk in Chinese population: evidence from a prospective cohort study. BMC Public Health 24, 522 (2024). https://doi.org/10.1186/s12889-024-17742-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17742-4