Abstract
Background
Unmet health needs are particularly important to people with disabilities; however, these unmet needs owing to limitations in daily life have been under-researched thus far. This study examined the effects of disability-related limitations in daily life on unmet needs.
Methods
This study included 5,074 adults with disabilities from the 2018–2020 Korea Disability and Life Dynamics Panel. We analyzed the effects of disability-related limitations in daily life on unmet needs using logistic regression with a generalized estimating equation model.
Results
Overall, 4.8% men and 4.6% women with disabilities had unmet needs. For men, unmet needs were 1.46 times (95% confidence interval [CI] 1.09–1.96) higher for those with moderate limitations in daily life. For women, unmet needs were 1.79 times (95% CI 1.22–2.39) higher when there were moderate limitations in daily life. The prominent factors causing this effect were physical or brain lesion disability for men and internal or facial disability and burden of medical expenses for women.
Conclusions
Limitations in daily life due to disability increase the risk of having unmet needs, an effect that is significantly more pronounced in men. These unmet needs differ depending on an individual’s sex, disability type, limited body parts, and other specific causes. Efforts are required to reduce the unmet needs of people with disabilities by considering the type of disability, impaired body parts, and causes of unmet needs in daily life.
Similar content being viewed by others
Introduction
Although access to medical care has gradually improved, unmet health needs still remain an important public health concern. Unmet health needs are defined as the medical gap between perceived or assessed needs and the actual resources available [1]. Unmet health needs harm independence, overall health, and quality of life from an individual’s perspective [2,3,4] and give rise to health inequalities from a social perspective. Health-vulnerable groups are more sensitive to the adverse effects of these unmet needs.
According to prior research, disability increases an individual’s odds of not receiving necessary routine care by more than 50% [5]. Individuals with disabilities have three times more unmet needs than those without disabilities [6]. Studies have found that the prevalence of disability is 35.2% in Finland, 27.3% in the United Kingdom, 12.7% in the United States, and 7.6% in Japan [7, 8]. Since the global population of people with a disability is estimated to be 15.6% [9], their unmet needs constitute a significant portion of the population dealing with health inequality.
In 2020 in South Korea, the prevalence of disabilities was 5.1%, of which 87.9% represented individuals who had acquired disabilities [10]. Additionally, in South Korea, single-person households accounted for the largest share of household types at 27.9% in 2017; as per a prior study the proportion of aging people with disabilities (51.3%) will reach three times that of the total population in 2021 [8]. Put differently, concerning situations like an increased risk of acquired disabilities due to longer lifespans, and an aging population can lead to an increase in the potential risk group for limitations in daily life due to disabilities.
Individuals with disabilities experience both physical and mental limitations in their daily lives. Therefore, they may have varying degrees of unmet needs compared to individuals without disabilities. Nonetheless, previous studies on unmet medical care for people with disabilities were limited to specific types of disabilities or diseases, or have focused on functional performance, such as daily life or instrumental activities of daily living [11,12,13,14].
Therefore, identifying unmet needs based on the areas and degrees of everyday limitations caused by physical or mental disabilities can help fill this knowledge gap. This study aims to provide evidence on the association between daily living limitations due to disability and unmet needs. This study primarily focused on analyzing the unmet needs according to the degree of limitation; however, it also analyzed specific physical or mental limitations and types of disabilities and causes of unmet needs. This study hypothesized that increased limitations of daily activities due to disability increase the risk of having unmet needs.
Methods
Data
This study used Disability and Life Dynamics Panel (DLDP) data from waves 1–3 (2018–2020), as surveyed by the Korea Disabled People’s Development Institute (KODDI). DLDP is a comprehensive nationwide dataset designed to assess changes in various aspects of life after individuals register for disability in the country. This longitudinal time-series survey was double-sampled with stratified variables for disability type, degree of disability, and sex, based on the Registered Disabled Persons Register of the Ministry of Health and Welfare of Korea (National approved statistics number: 438,001). The final panel consisted of 6,121 individuals with disabilities, and the relative standard error, calculated using weights, was found to be less than 5% at the national level. The survey was conducted with the consent of the participants by a professional interviewer, with a focus on four major areas (acceptance of and change in disability, health and medical care, self-reliance, and social participation), through face-to-face tablet-assisted personal interviews. In cases where the respondents were unable to communicate due to physical or mental disabilities, conditional proxy responses were allowed from guardians or authorized representatives. The DLDP dataset comprises de-identified secondary public data [15]. This study was approved for review exemption by the Institutional Review Board of the Yonsei University Health System Severance Hospital (Assignment approval number: 4-2022-1374).
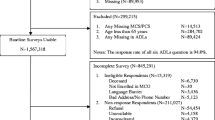
Participants
The DLDP had 6,121 respondents at baseline, of whom 1,047 aged under 19 years were excluded. Response rates were 90.3% and 95.2% in the second and third waves, respectively. The final number of participants aged 19 years or older per wave were as follows: first wave: 5,074 (2,676 men, 2,307 women); second wave: 4,610; and third wave: 4,401.
Variables
The dependent variable in this study was unmet needs. Having unmet needs was categorized as either “yes” and “no” according to an individual’s response to the question “During the past six months, were you in the need of a medical treatment at a hospital or clinic (excluding dental clinics) but did not receive it?”
The independent variable was disability-related limitations in daily living. Disability-related limitations in daily living were categorized into “low (0–13 points),” “mid (14–27 points),” and “high (28–39 points)” by dividing into three equal parts based on the totaled scores of 14 items, each measured on a 4-point Likert scale. These 14 items were created based on the Disability Identification Module used in Australia’s Survey of Disability, Aging, and Carers. This questionnaire is divided into six categories: “sensory,” “intellectual,” “physical,” “psychosocial,” “head injury, stroke or acquired brain injury,” and “other.”
The covariates were demographic (sex, age, and region), socioeconomic (marital status, education level, and household income), and health behavioral factors (drinking, smoking, and exercise). The other covariates included chronic diseases related to health status, as well as disability type and level. The type and level of disability were determined according to Korean disability classification criteria and KODDI’s panel survey design. Chronic diseases include diseases that affect daily life, including cancer, diabetes, high blood pressure, chronic renal failure, arthritis, mental illness, etc.
Statistical analysis
Descriptive statistical analysis including chi-squared test were conducted to investigate the frequency and distribution of the study participants’ general characteristics in Tables 1 and 2. For the main and sub-analyses, the generalized estimating equation model (GEE) was used to determine the effect of daily limitations due to disability on unmet needs. The results of the main analysis conducted in this study to provide evidence for the relationship between disability-related limitations in daily living and unmet needs are presented in Table 3. Sub-analyses were performed on covariates closely related to the main association, sub-question items of the independent variable indicators, and factors of the dependent variable. A subgroup analysis was conducted and stratified according to the type and level of disability (Table 4). Sub-analyses were also conducted on the sub-questions to determine limitations in daily life due to disability (Table 5), and factors contributing to the existence of unmet health needs by sex (Figs. 1 and 2). All analyses using GEE are presented as adjusted odds ratios (AOR) with 95% confidence intervals (95% CI). In our statistical analyses, a p-value of less than 0.5 was considered to be statistically significant, and SAS version 9.4 (SAS Institute Inc; Cary, NC, USA) was used.
Results
Table 1 shows the general characteristics of study participants at baseline. Among the 5,074 participants, 2,767 (54.5%) were men and 2,307 (45.5%) were women. In terms of age, the proportion of elderly people was high (19–29 years old: 6.1%; 30s: 7.2%; 40s: 13.7%; 50s: 32.6%; 60s or older: 40.4%). Approximately, three out of five participants had chronic diseases (3,089/5,074). The low and high disability severity groups were similar in size (Disability level, low: 2,490, 49.1%; high: 2,584, 50.9%).
Table 2 presents the results of descriptive statistics analysis of unmet needs by disability-related limitations of daily living. Among those with disabilities, 4.8% (133/2,767) of men and 4.6% (105/2,307) of women had unmet needs. Among men, the proportion of unmet needs gradually increased with an increase in daily life limitations (level of disability-related limitations in daily living: low, 4.0%; mid, 5.8%; high, 8.1%). Among women, the proportion of individuals with unmet needs decreased when disability-related limitations in daily living were high; the proportion of individuals with unmet needs in this high group was 3 out of 109 (level of disability-related limitations in daily living: low, 3.6%; mid, 6.5%; high, 2.8%).
In the main analysis of Table 3, it was noted that men with medium and high levels of disability-related limitations in daily living had 1.46 times (95% CI 1.09–1.96) and 2.79 times (95% CI 1.57–4.94) as many unmet needs compared to men with low levels of unmet health needs, respectively. Unmet needs were 1.79 times (95% CI 1.22–2.39) higher in women with mid-levels of disability-related limitations in daily living than in women with low levels; however, this was not statistically significant in women with high levels of unmet health needs (AOR 1.58, 95% CI 0.80–3.12).
Disability type was stratified as a sub-analysis in Table 4. Among men, there was a dose-response tendency for disability-related limitations in daily living and unmet needs, and a large effect size was statistically significant for physical or brain lesion disability (disability-related limitations in daily living, high: AOR 2.77, 95% CI 1.22–6.29). Conversely, among women, disability-related limitations in daily living and unmet needs showed an inverse U-shape, and the effect size was prominent for internal or facial disabilities (disability-related limitations in daily living, high: AOR 7.45, 95% CI 1.11–50.00).
According to an itemized analysis of disability-related limitations in daily living in Table 5, individuals with difficulties in using their legs and feet were most at risk for having unmet health needs (men: AOR 2.35, 95% CI 1.73–3.19; women: AOR 2.68, 95% CI 2.01–3.58). The next highest risk of unmet needs was having head injuries from a bruise or fall in men (AOR 2.24, 95% CI 1.61–3.11) and pain from chronic disease in women (AOR 2.34, 95% CI 1.78–3.06).
As for unmet needs by cause, men were more likely to face factors other than medical expenses in Fig. 1 (disability-related limitations in daily living, mid: AOR 2.08, 95% CI 1.06–4.05; high: AOR 7.15, 95% CI 2.72–18.78), and women were more likely to face medical expense burdens in Fig. 2 (disability-related limitations in daily living, mid: AOR 1.99, 95% CI 1.38–2.85; high: AOR 1.23, 95% CI 0.46–3.33).
Contents of the effect of disability-related limitations of daily living on the causes of the unmet needs in men. a Adjusted for other covariates. Reference group: Low disability-related limitations of daily living. Statistically significant *: p ≤ 0.05, **: p ≤ 0.01, ***: p ≤ 0.001, ****: p ≤ 0.0001
Contents of the effect of disability-related limitations of daily living on the causes of the unmet needs in women. a Adjusted for other covariates. Reference group: Low disability-related limitations of daily living. Statistically significant *: p ≤ 0.05, **: p ≤ 0.01, ***: p ≤ 0.001, ****: p ≤ 0.0001
Discussion
This study found that the risk of having unmet medical care needs increased with an increase in disability-related limitations in daily living, and this effect was more pronounced in men. Men with physical, brain lesion-related, or mild disabilities, and women with internal, facial, or severe disabilities were vulnerable to having unmet health needs due to limitations in daily life. In both men and women, pain due to leg and foot limitations increased the risk of having unmet health needs. Regarding causes of unmet needs, women were more likely to have the burden of medical expenses as a cause, while men were more likely to have factors other than this as causes.
We found that the risk of having unmet needs was higher when an individual’s disabilities severely affected their activities of daily living and limited their daily life. This is similar to prior findings that unmet needs increase due to limitations in daily life caused by old age or diseases such as cancer, dementia, asthma, and osteoarthritis in previous studies [16,17,18,19,20,21,22]. Our results and those of previous studies, both, confirm the relationship between unmet needs and chronic or incurable diseases, including disabilities. Additionally, this study is meaningful because it is generalizable by conducting a national survey and examines the impact of disability on unmet needs based on severity, both generally and in detail.
The study found that daily limitations owing to disabilities increase the risk of having unmet needs. Women were more vulnerable to having unmet needs when their limitations in daily life were moderate. However, men were more likely to have unmet needs if their daily life limitations were severe. In previous studies, women with disabilities were found to be at a higher risk of having unmet needs than men [6, 23, 24]. Nevertheless, when care is lacking, men with disabilities are more vulnerable to unmet needs than women [25]. However, the results may have been uncertain because the absolute number of women in this study who fell into the high daily-life limitation group was small.
To examine the effect of daily life limitations on unmet needs in detail, we used the subdivisions of disability type, severity, health aspect that limits daily life, and cause of unmet needs in this study. Regarding disability type, this effect differed by sex. Men with physical or brain lesion disabilities were 2.77 times more likely to have unmet needs when their daily life limitations were higher than those with no limitations. In South Korea, physical disabilities in men were due to (1) joint injuries (60.0%), (2) amputation (19.1%), (3) paralysis (16.2%), and (4) deformity (4.6%) in 2017 [26]. Among joint injuries, 25.7% involved the spinal discs and 12.4%, the knees [26]. Additionally, one in four people with physical disabilities did not have assistance in their daily life [27]. Physical disabilities may result in gait disturbances while accessing medical institutions thereby leading to unmet health needs.
Disabilities related to brain lesions are characterized by overlapping disorders. The main comorbidities in men with brain lesions were (1) language (45.7%), (2) intellectual (24.3%), (3) visual (21.9%), and (4) hearing (17.3%) in 2017 in South Korea [26]. Among people with brain lesions, nine out of ten had helpers to execute activities of daily life. However, 44.6% respondents said that they lacked assistance from others. The reasons were (1) limited help from family (54.9%), (2) lack of time from personal assistants (23.7%), and (3) severe disability (16.0%) [26]. Brain lesions can make it difficult to obtain independent medical care because of communication or intellectual impairments. People with brain lesions may also have unmet needs owing to insufficient help from others.
Meanwhile, women with internal or facial disabilities and severe daily life limitations were 7.45 times more likely to have unmet needs. Internal disabilities include renal, cardiac, respiratory, liver, stoma, urostomy, and epileptic disabilities. External physical disability typically results from the initial cessation of the pathology caused by an injury or disease, after which disability and impairment persist. However, internal organ disabilities require continuous medical attention, including treatment, diagnosis, and testing, because disabilities and diseases exist simultaneously, and usually worsen over time [28]. In South Korea, where national health insurance is available, the average additional monthly cost due to internal disabilities was higher than the average in 2017 (average: $144.8; liver: $405.4; kidney: $257.5; stoma or urostomy $205.9) [26].
Facial disabilities had the second-highest average monthly cost of disability (at $288.8, after autism at $533.7) [26]. Additionally, people with facial disabilities were the group that most often responded that they could not visit hospitals or clinics even if they wanted to due to economic reasons [26]. The economic burden of internal or facial disabilities can create a gap between the need for and use of medical services.
Regarding limiting factors in daily life due to disability, difficulties in using legs and feet had the greatest effect on the existence of unmet needs, regardless of sex. Mobility impairment is a major concern for adults with disabilities [29, 30]. With the exception of non-face-to-face treatment and home nursing, discomfort in the legs and feet is directly related to unmet needs as physical movement becomes difficult.
The primary cause of unmet needs in women was the burden of medical expenses. Women with disabilities face a dual barrier to the labor market: being a woman and a person with disabilities [31]. The employment rate of women with disabilities was only 49.8% of that of men [26]. Considering that difficulty performing work due to disability (34.0%) and health problems (20.5%) are the main reasons for non-employment for women with disabilities who do not work, it can be concluded that limitations due to disability and unmet needs due to household difficulties are closely related.
This study has certain limitations. First, the data used in this study excluded facility residents, individuals with unknown addresses, and the deceased. However, as this accounted for 2.6% of the registered disabled persons surveyed (residence in facilities: 0.6%, expungement or death: 2.0%) [32], this would not have had a significant impact on the overall results. Second, unmet needs based on time-series changes in the degree of limitation in daily life were not analyzed. However, we can consider that disability is chronic and has a relatively stable severity. Third, we adjusted for various covariates that could affect our hypothesis testing; however, some variables were not included in the study. Congenital presence or absence of disability, acceptance of disability, and support status due to disability were not considered to be covariates. Therefore, follow-up studies that consider these factors are warranted. Fourth, it was difficult to analyze each disability type individually because of the limited number of participants. However, we attempted to differentiate disability types by categorizing them in this study.
Conclusions
The risk of unmet needs increases as disabilities severely restrict activities of daily living. Men with high disability-related limitations of daily living had 2.79 times greater unmet needs than men with low disability-related limitations of daily living. Men are more vulnerable to unmet needs owing to limitations in daily life and due to physical or brain lesion disabilities whereas women are more likely to have unmet needs due to internal or facial disabilities. The factor that had the greatest influence on limitations in daily life due to disability was the inability in using legs or feet, and the main factor affecting unmet needs for women was medical expenses. It is thus, necessary to find ways to alleviate the unmet needs of individuals with disabilities by considering the type of disability, the aspects that restrict daily life, and the causes of unfulfillment.
Data availability
Public secondary data used in this study can be obtained by submitting a data application to KODDI according to the notice on the following site. https://www.koddi.or.kr/bbs/notice01_view.jsp?brdNum=7415269.
Abbreviations
- GEE:
-
Generalized estimating equation model
- AOR:
-
Adjusted odds ratios
- CI:
-
Confidence interval
- DLDP:
-
Disability and Life Dynamics Panel
- KODDI:
-
Korea Disabled People’s Development Institute
References
Aday LA, Andersen R. Development of indices of access to medical care. Health Administration Press; 1975.
Neri MT, Kroll T. Understanding the consequences of access barriers to health care: experiences of adults with disabilities. Disabil Rehabil. 2003;25(2):85–96.
Hansen DG, Larsen PV, Holm LV, Rottmann N, Bergholdt SH, Søndergaard J. Association between unmet needs and quality of life of cancer patients: a population-based study. Acta Oncol. 2013;52(2):391–9.
Grønkjær LL, Lauridsen MM. Quality of life and unmet needs in patients with chronic liver disease: a mixed-method systematic review. JHEP Rep. 2021;3(6):100370.
Sanmartin C, Pierre F, Tremblay S. Waiting for care in Canada: findings from the health services access survey. Healthc Policy. 2006;2(2):43.
McColl MA, Jarzynowska A, Shortt S. Unmet health care needs of people with disabilities: population level evidence. Disabil Soc. 2010;25(2):205–18.
Ministry of Health and Welfare. 2020 Report on Abuse of Persons with Disabilities. In. The Rights and Interests of the Disabled, Ministry of Health and Welfare; 2021.
Korea Disabled People's Development Institute. 2022 Disability Statistical Yearbook. In. Korea Disabled People’s Development Institute; 2021.
World Health Organization and World Bank Group. World report on disability 2011. World Health Organization; 2011.
Korean Statistical Information Service. Disability occurrence and disability status. Korean Statistical Information Service; 2021. &tblId=DT_383003_P020&conn_path=I2. Accessed 11.13. 2021.
Dodge HH, Kadowaki T, Hayakawa T, Yamakawa M, Sekikawa A, Ueshima H. Cognitive impairment as a strong predictor of incident disability in specific ADL–IADL tasks among community-dwelling elders: the Azuchi study. Gerontologist. 2005;45(2):222–30.
Zwicker J, Zaresani A, Emery JH. Describing heterogeneity of unmet needs among adults with a developmental disability: an examination of the 2012 Canadian survey on disability. Res Dev Disabil. 2017;65:1–11.
Mitra M, Long-Bellil LM, Iezzoni LI, Smeltzer SC, Smith LD. Pregnancy among women with physical disabilities: unmet needs and recommendations on navigating pregnancy. Disabil Health J. 2016;9(3):457–63.
Millán-Calenti JC, Tubío J, Pita-Fernández S, González-Abraldes I, Lorenzo T, Fernández-Arruty T, et al. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch Gerontol Geriatr. 2010;50(3):306–10.
Korea Disabled People's Development Institute. Handbook for users of the disability and life dynamics panel survey (1st ~ 3rd). In: Korea Disabled People’s Development Institute; 2022.
Liu Y-H, Chang H-J, Huang C-C. The unmet activities of daily living (ADL) needs of dependent elders and their related factors: an approach from both an individual-and area-level perspective. Int J Gerontol. 2012;6(3):163–8.
Chen S, Zheng J, Chen C, Xing Y, Cui Y, Ding Y, et al. Unmet needs of activities of daily living among a community-based sample of disabled elderly people in eastern China: a cross-sectional study. BMC Geriatr. 2018;18(1):1–11.
Momtaz YA, Hamid TA, Ibrahim R. Unmet needs among disabled elderly malaysians. Soc Sci Med. 2012;75(5):859–63.
Thewes B, Butow P, Girgis A, Pendlebury S. Assessment of unmet needs among survivors of breast cancer. J Psychosoc Oncol. 2004;22(1):51–73.
Gaugler JE, Kane RL, Kane RA, Newcomer R. Unmet care needs and key outcomes in dementia. J Am Geriatr Soc. 2005;53(12):2098–105.
Canonica G, Baena-Cagnani C, Blaiss M, Dahl R, Kaliner M, Valovirta E, et al. Unmet needs in asthma: global asthma physician and patient (GAPP) survey: global adult findings. Allergy. 2007;62(6):668–74.
Jo H, Kim E-s, Jung B, Sung S-H, Ha I-H. Association between osteoarthritis and unmet medical needs in Korea: limitations in activities as a mediator. BMC Public Health. 2020;20(1):1–11.
Jetha A, Gignac MA, Ibrahim S, Martin Ginis KA. Disability and sex/gender intersections in unmet workplace support needs: findings from a large Canadian survey of workers. Am J Ind Med. 2021;64(2):149–61.
Hwang B, Chun S-M, Park J-H, Shin H-I. Unmet healthcare needs in people with disabilities: comparison with the general population in Korea. Annals of Rehabilitation Medicine. 2011;35(5):627–35.
Jang S-n, Kawachi I. Care inequality: care received according to gender, marital status, and socioeconomic status among Korean older adults with disability. Int J Equity Health. 2019;18(1):1–14.
Ministry of Health and Welfare. 2017 Survey of the Disabled. In: Ministry of Health and Welfare; 2017.
Lalloo C, Hundert A, Harris L, Pham Q, Campbell F, Chorney J, et al. Capturing Daily Disease experiences of adolescents with Chronic Pain: mhealth-mediated Symptom Tracking. JMIR Mhealth Uhealth. 2019;7(1):e11838. https://doi.org/10.2196/11838.
Jeong BG. Medical security for the persons with internal organ impairments. J Korean Med Association. 2010;53(4):266–8.
Picavet H, Hoeymans N. Physical disability in the Netherlands: prevalence, risk groups and time trends. Public Health. 2002;116(4):231–7.
Okoro CA, Hollis ND, Cyrus AC, Griffin-Blake S. Prevalence of disabilities and health care access by disability status and type among adults—United States, 2016. Morb Mortal Wkly Rep. 2018;67(32):882.
Baldwin ML, Johnson WG. Labor market discrimination against women with disabilities. Industrial Relations: A Journal of Economy and Society. 1995;34(4):555–77.
Kim H, Kim T-y. A study on Sample Design in Disability and Life Dynamics Panel. Surv Res. 2021;22(2):105–28.
Acknowledgements
We would like to express our gratitude to KODDI for providing us with the DLDP dataset.
Funding
This work was supported by the National Research Foundation of Korea(NRF) grant funded by the Korea government(MSIT) (No. 2022R1F1A1062794).
Author information
Authors and Affiliations
Contributions
Conceptualization: HK; Data curation: YHJ; Formal analysis: YHJ; Methodology: YHJ, SP, JS and SIJ; Research administration: SIJ; Resources: HK; Supervision: SP, JS and SIJ; Visualization: YHJ; First draft of the manuscript: YHJ and HK; Review and editing: YHJ, HK and SIJ.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved for review exemption by the Institutional Review Board of the Yonsei University Health System Severance Hospital (Assignment approval number: 4-2022-1374).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
1 Confidence Interval (CI); Disability and Life Dynamics Panel (DLDP); Korea Disabled People’s Development Institute (KODDI); Generalized Estimating Equation Model (GEE); Adjusted Odds Ratio (AOR).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kim, H., Jung, Y.H., Park, S. et al. Effects of disability-related limitations in daily living on unmet needs: a longitudinal-study1. BMC Public Health 24, 351 (2024). https://doi.org/10.1186/s12889-024-17674-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-024-17674-z