Abstract
Background
The quality of the statistics on causes of death (CoD) does not present consolidated indicators in literature further than the coding group of ill-defined conditions of the International Classification of Diseases. Our objective was to assess the territorial quality of CoD by reliability of the official mortality statistics in Spain over the years 1980–2019.
Methods
A descriptive epidemiological design of four decades (1980-, 1990-, 2000-, and 2010–2019) by region (18) and sex was implemented. The CoD cases, age-adjusted rates and ratios (to all-cause) were assigned by reliability to unspecific and ill-defined quality categories. The regional mortality rates were contrasted to the Spanish median by decade and sex by the Comparative Mortality Ratio (CMR) in a Bayesian perspective. Statistical significance was considered when the CMR did not contain the value 1 in the 95% credible intervals.
Results
Unspecific, ill-defined, and all-cause rates by region and sex decreased over 1980–2019, although they scored higher in men than in women. The ratio of ill-defined CoD decreased in both sexes over these decades, but was still prominent in 4 regions. CMR of ill-defined CoD in both sexes exceeded the Spanish median in 3 regions in all decades. In the last decade, women’s CMR significantly exceeded in 5 regions for ill-defined and in 6 regions for unspecific CoD, while men’s CMR exceeded in 4 and 2 of the 18 regions, respectively on quality categories.
Conclusions
The quality of mortality statistics of causes of death has increased over the 40 years in Spain in both sexes. Quality gaps still remain mostly in Southern regions. Authorities involved might consider to take action and upgrading regional and national death statistics, and developing a systematic medical post-grade training on death certification.
Similar content being viewed by others
Introduction
The quality of statistics on causes of death (CoD) does not present consolidated indicators in papers nor in official health or statistical publications [1,2,3,4,5]. The quality of CoD statistics is assessed with several approaches and limited continuity. Only the great group of symptoms, signs, and ill-defined conditions of the International Classification of Diseases has achieved a generalised use [6,7,8,9]. This great quality group was often scored in wide ranges across nations when publicised, to suggest to take action [10]. The quality of statistics literature has also considered the impossible CoD, incompatible CoD to sex and age, and a variety of unspecific CoD; all referred as garbage medical causes [11,12,13,14,15,16,17,18].
Some collaborations have improved the reliability of ill-defined and garbage CoD by applying informatics algorithms to minimize the garbage codes in different ways: a) replacing the underlying CoD (which is the cause used in mortality statistics) with other causes filled out on the same death certificate; b) making expert data redistributions, or applying regression statistic models; or c) matching cases from health administrative databases for CoD extraction [11, 13, 15, 19,20,21,22].
Quality of death statistics have varied among countries for centuries. In the mid-eighteenth century, a little later than in North and Western European countries, Spain started to publish official vital statistics [23]. Recently, with the restoration of the Spanish democracy in 1978 and the decentralisation in the regions, a renewed boost was given to the improvement of civil registration and vital statistics to Western European standards [24]. Although the mortality rate decrease had begun time before, the amount of ill-defined causes of death has gradually decreasing throughout the new democratic time in Spain, to achieve, nowadays, an intermediate international position [10, 12].
The poor quality of CoD statistics involved a double miscertification issue concerning validity and reliability. Several validity studies showed a lack of uniformity across great and leading CoD, in Western context [25,26,27,28,29].
Our objective was to assess the national and regional quality of causes of death by analysing the reliability of the official mortality statistics over the years 1980–2019 across Spain.
Methods
We implemented an observational descriptive epidemiological design over annual mortality cases by the administrative territorial division of Spain in 18 regions (named Autonomous Cities and Communities) (Supplementary Figure 1 Map). Every region supports the National Institute of Statistics (INE acronym in Spanish) by coding the CoD, except the cities Ceuta and Melilla where coding is carried out by the INE itself. We assessed reliability by 3 indicators. We grouped the underlying causes of death (CoD) into unspecific and ill-defined quality categories from the 9th and 10th revisions of the International Classification of Diseases. This assessment was performed by experts (three coding nurses, and epidemiologist and forensic physicians) and by taking into account the literature (Supplementary Annex A) [6, 12, 15]. Territorial case counts and populations of INE data are publicly available by an informed request (https://www.ine.es/infoine/?L=1). Time was tabulated in 4 decades (1980-, 1990-, 2000-, and 2010–2019). We estimated age-adjusted rates of quality categories for 100,000 inhabitants by using the direct method and the European Standard Population (WHO, 1976), as one indicator, and the weights {wa: a = 1,2,…,19} appear as Supplementary Table 1. For the second indicator, we presented the age-adjusted rates ratios (proportions, in percentage) of the quality category divided by its region all death causes. Both indicators, by decade and sex.
Each regional mortality rate was contrasted with the Spanish median of each decade by means of the Comparative Mortality Ratio (CMR) in a Bayesian framework, as the third indicator. The estimation was implemented as the number of deaths by region (\({\text{r}}=1, 2, \dots , 18\)) and age group (\({\text{a}}=1 , 2, \dots , 19\)), and it was modelled as a Poisson random variable \({{\text{d}}}_{{\text{ra}}} \sim \mathrm{ Poisson}({\upmu }_{{\text{ra}}})\), with the Jeffreys’s prior distribution [30] \(\uppi ({\upmu }_{{\text{ra}}})\propto {{\upmu }_{{\text{ra}}}}^{-1/2}\). Again, we have used the European Standard Population for the age-adjusted rates. The mortality rate by region and age group is \({\uplambda }_{{\text{ra}}}={\upmu }_{{\text{ra}}}/{{\text{P}}}_{{\text{ra}}}\), where \({{\text{P}}}_{{\text{ra}}}\) is the population in the region \({\text{r}}\) and age group \({\text{a}}\). The mortality rate in Spain by age group is \({\uplambda }_{{\text{a}}}={\upmu }_{{\text{a}}}/{{\text{P}}}_{{\text{a}}}\), where \({\upmu }_{{\text{a}}}={\sum }_{{\text{r}}}{\upmu }_{{\text{ra}}}\) and \({{\text{P}}}_{{\text{a}}}={\sum }_{{\text{r}}}{{\text{P}}}_{{\text{ra}}}\). For each region, the adjusted rate is given by \(\sum_{{\text{a}}}{{\text{w}}}_{{\text{a}}}{\uplambda }_{{\text{ra}}}\), and the comparative mortality rates ratio is the parameter:
The posterior distribution of each \({\upmu }_{{\text{ra}}}\) is a gamma distribution. The posterior distribution of the adjusted rate and of \({{\text{CMR}}}_{{\text{r}}}\) were obtained using the Monte Carlo method, generating \({\upmu }_{{\text{ra}}}^{{\text{i}}} \sim \mathrm{ Gamma}({{\text{d}}}_{{\text{ra}}}+1/2, 1)\) and computing \({\uplambda }_{{\text{ra}}}^{{\text{i}}}={\upmu }_{{\text{ra}}}^{{\text{i}}}/{{\text{P}}}_{{\text{ra}}}\), \({\uplambda }_{{\text{a}}}^{{\text{i}}}={\upmu }_{{\text{a}}}^{{\text{i}}}/{{\text{P}}}_{{\text{a}}}\), and \({{\text{CMR}}}_{{\text{r}}}^{{\text{i}}}=\sum_{{\text{a}}}{{\text{w}}}_{{\text{a}}}{\uplambda }_{{\text{ra}}}^{{\text{i}}}/\sum_{{\text{a}}}{{\text{w}}}_{{\text{a}}}{\uplambda }_{{\text{a}}}^{{\text{i}}}\), \({\text{i}}=1, \dots , 10 000\). The posterior estimation was performed using the median as the point estimator, and the 95% credible intervals (95% CrI) were the intervals from 0.025th to 0.975th quantile of the posterior distribution. The \({{\text{CMR}}}_{{\text{r}}}\) was considered statistically significant if the 95% CrI did not contain the value 1, to assess excess or defect on mortality. The analysis was performed using R version 3.6.1. The CMR function and the database are available on request.
Results
Spain by decade, sex, and quality category in rates indicator
All-cause deaths have decreased in in both sexes Spain as a whole over the years 1980 to 2019 (age-adjusted rates of 1 543 per 100,000 inhabitants in the first decade 1980–1989 to 867 per 100,000 inhabitants in the last decade of 2010–2019). The ill-defined CoD have declined in both sexes (from rates of 181, 101, 75, to 52 in the four decades studied) (Table and Fig. 1). The unspecific CoD have declined in both sexes, as well (from rates of 49, 39, 33, to 25 over decades) (Table 1, and cases distribution are available at Supplementary Table 2).
Women and men rates have decreased over the decades in all quality categories. Men have showed higher rates than women have in all quality categories in Spain (Tables 2 and 3, and cases distribution are available at Supplementary Tables 3 and 4).
In the whole period of 1980–2019, 8 of the 18 regions (that was, Andalusia, Asturias, Balearic and Canary Islands, Ceuta & Melilla, Extremadura, Murcia, and Valencia; with rate range from 1,147 to 1,291) have had higher all-cause age-adjusted rates than Spain (rate of 1,098) (Table 1).
Spain has achieved a 7.6% of ill-defined CoD in the whole period and both sexes. Ill-defined CoD were higher in women than men were (9.0 versus 6.3%). The proportion of Ill-defined CoD by sex has decreased over the decades, but is still prominent in women in all four decades (13.4, 9.8, 8.5, and 6.9%) (Table 2). In unspecific CoD, Spain has registered a 3.1% in the whole period and sex. This proportion has remained steady at rounded 3% over decades by sex (Table 3).
Whole period, region and sex with rates indicator
In the whole period and in both sexes, seven of 18 regions (Ceuta & Melilla’s rate of 131, Andalusia 106, Madrid 103, Extremadura 101, Galicia 92, Castile & Lion 90, and Balearic Islands 85) have presented higher regional age-adjusted rates than Spain for ill-defined CoD. The same regions, excluding Balearic Islands, have displayed higher rates in women. Ill-defined rates were higher in men than women were in the whole period, with Murcia exception (rates of 71 versus 78, respectively). Men have showed higher rates in the same regions than in both sexes, plus Cantabria (Table 1).
All regions rates have decreased in all quality categories over time and sex. Five of the regions (Ceuta & Melilla rate of 107, Andalusia 81, Madrid 68, Extremadura 59, and Valencia 53) have exceed the Spanish rate in the last decade (2000–2019), for ill-defined CoD in both sexes. Women and men have showed the same pattern in the last decade but excluding Valencia in men (Table 1).
On unspecific CoD rates, 7 of 18 regions have exceed the Spanish rate in the last decade in both sexes (Extremadura 34, Andalusia 31, Murcia 30, Ceuta & Melilla 28, and Valencia 25). Women have pointed the same regions than have exceed in both sexes, while men have added one different more (Madrid), but excluding another (Valencia) (Table 1).
Quality categories with proportions indicator
The regional ill-defined CoD have lowered in proportions through the most recent decades and sex, but three regions (Ceuta & Melilla, Andalusia, and Madrid) have maintained or increased proportions by sex, except in women in one region (Madrid), although it was higher than Spain (9 versus 7%) (Table 2). Regional unspecific CoD in both sexes have maintained the proportions over decades, meanwhile 6 of 18 regions have registered the lowest proportions in the last decade compared to Spain (Asturias, Balearic Islands, Cantabria, Castile & Lion, Navarre, and Rioja), and previous regional decades. Women have included 4 of 18 regions, while men have sex-specified this both sexes pattern, including one region (Aragon) (Table 3).
Regional quality versus Spain by decade and sex with CMR indicator
The CMR of ill-defined CoD in both sexes have statistically exceeded Spain in 3 of the 18 regions (Andalusia, Extremadura, and Madrid) in all decades. The same excess has occurred in one other region (Ceuta & Melilla) in the last three decades. Another (Valencia) has registered excess mortality in the last decade (CMR = 1.02, 95% CrI 1.01 to 1.03). On the contrary, two regions (Castile & Lion and Galicia) that exceeded in the first three decades have decreased in the last (0.86, 0.85 to 0.88; and 0.95, 0.93 to 0.96, respectively) (Fig. 1 and Supplementary Table 5).
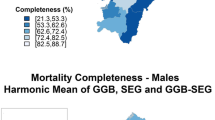
Women have showed an ill-defined mortality excess over Spain in 2 regions (Andalusia and Extremadura) in all decades; in one region (Ceuta & Melilla) in the last three decades; and in two different regions (Madrid and Valencia) in the last two decades (Fig. 2 and Supplementary Table 6). While, men have showed the same both sexes regional ill-defined pattern excess over all decades in the same 3 regions (Andalusia, Extremadura, and Madrid), and the same one in the last three decades (Ceuta & Melilla) (Fig. 3 and Supplementary Table 7).
The CMR of unspecific CoD in both sexes has statistically exceeded Spain in one region (Ceuta & Melilla) in all decades adding 5 more regions to the last decade (Andalusia, Canary Islands, Extremadura, Galicia, and Murcia) (Fig. 1 and Supplementary Table 8). Women and men have exceeded in 3 regions (Andalusia, Canary Islands, and Murcia) in in the last two decades; but also, Murcia and Extremadura in the last three decades, in women (Figs. 2 and 3, and Supplementary Tables 9 and 10, respectively).
Discussion
The quality of mortality statistics of causes of death has increased throughout the 40 years studied in Spain in women and men. However, quality gaps still remain in specific regions. Meanwhile, the best regional quality results have showed that there is scope for targeted upgrade.
In our experience, two major components comprise reliable quality of CoD statistics: First component involves medical certification (professionalism, health record access, and healthcare administration type) and the second involves post-certification and related to mortality registers [31, 32], coding skills [33], and the capacity for documental health information recovery [12].
Our purpose was the internal comparison of the regions with Spain over a long period. The age-standardised rates to the European Standard Population fulfilled our purpose of national and international comparison. However, given the general rates decrease in the two quality of mortality categories, we chose to describe its proportion composition with respect to all-cause of deaths between year periods, thus giving a better description.
This study has some limitations. The CoD selection and quality grouping may lack of comparability. However, our consensus on ICD10 code selection was based on the ICD10 instructions manual [34] and literature revision [6, 12, 35]. The two major proposals of quality assessment of CoD come from the Centers for Disease Control [6] and Anaconda software® [35], but these showed some qualitative differences. The CDC paper established 3 subtypes of CoD (unknown & ill-defined, immediate & intermediate, and nonspecific). The unknown and ill-defined causes included fewer codes than the ICD10 (18th chapter and annex 7.3). These immediate or intermediate CoD could also be reassigned to a general unspecific group, as well as to the ill-defined group by WHO criteria (ICD10 code I50 for heart failure). The annual national summary of 2.2% for unknown and ill-defined causes versus a 32.5% for the other unsuitable CoD, seems a broad gap to take action (Supplementary Annex B) [6, 12]. The Anaconda software encompasses 3 axes: the 1st axe, five qualify for uninformative subtypes (1- symptoms, sign, and ill-defined conditions; 2- impossible as CoD; 3- intermediate CoD; 4- immediate CoD; and 5- insufficiently specified CoD extracted from Global Burden Disease (GBD) [36]; the 2nd axe, four levels of health impact policies of 800 codes (Supplementary Annex B); and the 3rd axe, a vital performance index (of completeness, and garbage and impossible codes by age and sex). Although, GBD is dynamically updated [37], this praiseworthy effort, also expresses complex assessment outcomes, to take action further than lack of completeness [27, 38] and high numbers for ill-defined CoD, especially in low-income countries [10, 39]. In our case, for example, we considered dementia, ictus, pneumonia, or accidental poisoning by narcotics, reliable as primary health care diagnostics, however a detailed hospital-like testing technology may improve their accuracy.
The health and judicial administration framework matters in medical certification. Spain is supported by a Welfare State with National Health and Social Systems (public funding, universal access, a majority of centres of governmental propriety, and regional competences in health and social care budget and management), as well as a judicial system with forensic pathology and laboratory facilities at every regional centre. The Western European context of public funding and universal health care provision (private versus governmental) could be associated with completeness and validity of causes of death [40]. Likewise, the majority of diseases can be diagnosed through anamnesis and conventional physical examination and complementary tests at the Primary Health Care subsystem.
The process of completing and accurately coding a death certificate according to the ICD is challenging for all countries. Not all of them have achieved a good-quality threshold on mortality data. The WHO included in the medium-quality category several high-income Western European countries (such as Austria, Belgium, Denmark, France and Germany, regulated by universal Health Insurance systems) [14, 41]. Furthermore, in the present decade six high-income countries worldwide achieved a 9—31%, adding ill-defined (ICD10, 18th chapter) to impossible CoD [15]. Similarly, it would be a specificity error to classify 67.3% of the vital registration deaths as least-specific codes, without any further geographical or social context reference [21]. Providing the magnitude of poor quality death certification, health authorities did not seem to play a role in the probable random underestimation of the great and leading CoD [7, 13, 26,27,28, 31]. Currently, the COVID-19 pandemic has probably worsened death certification [42]. Statistics and health authorities may consider implementing the framework conditions to avoid miscertification. In addition, the WHO may include ill-defined conditions in the same ICD chapter in future revisions. Meanwhile, some national CoD registries have achieved top quality [32], and could be a standard target to replicate.
Some papers have emphasised the weakness of imputations made by case identification algorithms based on available health and population record information. The imputations from multiple search assignments of unsuitable CoD were proportionally predicted [11, 13, 15, 19,20,21, 43, 44] without a representative sample of validation [7, 13, 27, 28, 31].
Related to sex differences, we have assessed lower quality death certification in men than women at any territory and decade. Results, that are aligned to multi-country study that stated a no clear bias against women in death registration [45]. The three indicators applied adjusted for age groups. Sex differential in longer life might partially contributed to major medical unspecificity by polipathology bias. The general (not much) higher proportion quality in women than men on bad mortality quality, should consider that the magnitude of the population involved is described by the rates, which were higher in men than in women.
The poor statistical death quality showed in regions is much coincident to regional distribution of the Gross Domestic Product per Capita by regions of Spain (Supplementary Figure 2 Map). Moreover, poor death certification may be linked to individual characteristics (such as medical professionalism, the social stratum of the deceased, etc.) [46, 47]. This misclassification would imply regional and individual differential errors. The long-time evidence of our results is suggestive of a new organisational model with a multilevel health experts support to the National Institute of Statistics for a better regional and national standards upgraded [33].
Some studies have associated the deficiency of medical specialist education on death certification with miscertification in mortality statistics [48]. Courses for the improvement of CoD notification have oftentimes been imparted with diverse approaches and to different alumni, such as medical students or physicians in their specialisation [43, 49, 50]. Nowadays, this training is available through new communication technologies such as mobile phones [44], websites and e-learning platforms [43, 51]. Additionally, the WHO may introduce a certification of “medical competence on certification of causes of death” to foster the quality of mortality statistics worldwide.
As stated before, there is a general need of representative national validity studies of causes of death to address properly the post-certification informatics reassignment in CoD.
Conclusion
The reliability of the CoD has been improving over the last 40 years in Spain in both sexes. Regional gaps have persisted along those years and even in the last decade. Regional gaps mostly focused in Southern regions. Authorities involved might consider to take action and upgrade bad quality, and to develop a systematic medical post-grade training on death certification to improve regional differences and the quality of death statistics of Spain.
Availability of data and materials
The dataset and the analysis R-script file used during the current study are available from the corresponding author.
References
Campbell A. Quality of mortality data during the coronavirus pandemic, England and Wales: 2020. Office for National Statistics; 2020. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/articles/qualityofmortalitydataduringthecoronaviruspandemicenglandandwales/2020. Accessed 17 November 2023.
INE. Death statistics according to cause of death. https://www.ine.es/dyngs/INEbase/en/operacion.htm?c=Estadistica_C&cid=1254736176780&menu=resultados&idp=1254735573175#!tabs-1254736194710. Accessed 17 November 2023.
World Health Organization. Who Mortality Database - WHO. https://www.who.int/data/data-collection-tools/who-mortality-database. Accessed 17 November 2023.
EuroStat. Causes of death. Data Browser. https://ec.europa.eu/eurostat/databrowser/view/hlth_cd_aro/default/table?lang=en. Accessed 17 November 2023.
Xu J, Murphy S, Arias E, Kochanek K. Deaths: Final data for 2019. Natl Vital Stat Reports. 2021;70:1–87. https://doi.org/10.15620/cdc:106058.
Flagg LA, Anderson RN. Unsuitable underlying causes of death for assessing the quality of cause-of-death reporting. Natl Vital Stat Reports. 2021;69(14):1–25.
Foreman KJ, Naghavi M, Ezzati M. Improving the usefulness of US mortality data: New methods for reclassification of underlying cause of death. Pop Health Metrics. 2016;14(1):1–9. https://doi.org/10.1186/s12963-016-0082-4.
WHO. Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (chapter 18th). In: International Statistical Classification of Diseases and Related Health Problems 10th Revision. https://publications.aap.org/aapbooks/book/689/chapter/8403399/Symptoms-signs-and-abnormal-clinical-and. Accessed 17 November 2023.
Bogdanović MD, Marić GD, Pekmezović TD, Alempijević ĐM. Evaluation of coding ill-defined and unknown causes of death in the Republic of Serbia. J Forensic Leg Med. 2019;62:34–9. https://doi.org/10.1016/j.jflm.2018.12.009.
World Health Organization. Health Statistics 2017. Monitoring health for the sustainable development goals. Completeness and quality of cause-of-death data. WHO; 2017. https://www.who.int/publications-detail-redirect/9789241565486. Accessed 17 November 2023.
Adair T, Firth S, Phyo TP, Bo KS, Lopez AD. Monitoring progress with national and subnational health goals by integrating verbal autopsy and medically certified cause of death data. BMJ Glob Health. 2021;6(5):1–8. https://doi.org/10.1136/bmjgh-2021-005387.
Cirera L, Salmerón D, Martínez C, Bañón RM, Navarro C. More than a decade improving medical and judicial certification in mortality statistics of death causes. Rev Esp Salud Publica. 2018;92:e201806031:1–13.
Iburg KM, Mikkelsen L, Adair T, Lopez AD. Are cause of death data fit for purpose? evidence from 20 countries at different levels of socio-economic development. PLoS ONE. 2020;15(8):1–17. https://doi.org/10.1371/journal.pone.0237539.
Mathers CD, Fat DM, Inoue M, Rao C, Lopez AD. Counting the dead and what they died from: an assessment of the global status of cause of death data. Bull World Health Organ. 2005;83(3):171–7.
Mikkelsen L, Iburg KM, Adair T, Fürst T, Hegnauer M, von der Lippe E, et al. Assessing the quality of cause of death data in six high-income countries: Australia, Canada, Denmark, Germany, Japan and Switzerland. Int J Public Health. 2020;65(1):17–28. https://doi.org/10.1007/s00038-019-01325-x.
Regidor E, Rodríguez C, Ronda E, Gutiérrez JL, Redondo JL. The quality of the basic cause of death in the Statistical Bulletin of Mortality. Spain, 1985. Gac Sanit. 1993;7(34):12–20. https://doi.org/10.1016/s0213-9111(93)71128-0.
Ribotta BS, Escanés GA. “Garbage codes” in death records in Argentina, Chile, Colombia and Mexico (2000–2011). Med Salud y Soc. 2014;5:4–17. https://doi.org/10.1590/0102-311X00113016.
Teixeira RA, Naghavi M, Guimarães MDC, Ishitani LH, França EB. Quality of cause-of-death data in Brazil: Garbage codes among registered deaths in 2000 and 2015. Rev Bras Epidemiol. 2019;22 Suppl 3:e19002.supl.3:1–14. https://doi.org/10.1590/1980-549720190002.supl.3.
Canova C, Simonato L, Barbiellini Amidei C, Baldi I, Dalla Zuanna T, Gregori D, et al. A systematic review of case-identification algorithms for 18 conditions based on Italian healthcare administrative databases: A study protocol. Epidemiol Prev. 2019;43(4 Suppl 2):8–16. https://doi.org/10.19191/EP19.4.S2.P008.089.
Ge H, Gao K, Li S, Wang W, Chen Q, Lin X, et al. An automatic approach designed for inference of the underlying cause-of-death of citizens. Int J Environ Res Public Health. 2021;18(5):2414:1–15. https://doi.org/10.3390/ijerph18052414.
Johnson SC, Cunningham M, Dippenaar IN, Sharara F, Wool EE, Agesa KM, et al. Public health utility of cause of death data: applying empirical algorithms to improve data quality. BMC Med Inform Decis Mak. 2021;21(1):175–95. https://doi.org/10.1186/s12911-021-01501-1.
Wengler A, Gruhl H, Plaß D, Leddin J, Rommel A, von der Lippe E, et al. Redistributing ill-defined causes of death - a case study from the BURDEN 2020-project in Germany. Arch Public Health. 2021;79(1):33–51. https://doi.org/10.1186/s13690-021-00535-1.
INE. INEbase. History. https://ine.es/inebaseweb/libros.do?tntp=25687&L=1. Accessed 17 November 2023.
Cirera L, Segura A. Updated medical death documents: Medical death certificate and the birth statistic bulletin. Aten Primaria. 2010;42(8):431–7. https://doi.org/10.1016/j.aprim.2009.09.029.
Cirera L, Tormo MJ, Martínez C, Contreras J, García J, Navarro C. Usefulness of the statistical bulletin of deaths to identify extrahospital deaths in the context of a myocardial infarction population registry. Rev Esp Cardiol. 2001;54(9):1041–7.
Pérez-Gómez B, Aragonés N, Pollán M, Suárez B, Lope V, Llácer A, et al. Accuracy of cancer death certificates in Spain: A summary of available information. Gac Sanit. 2006;20(Suppl 3):42–51. https://doi.org/10.1157/13101089.
Gotsens M, Marí-Dell’Olmo M, Rodríguez-Sanz M, Martos D, Espelt A, Pérez G, et al. Validation of the underlying cause of death in medicolegal deaths. Rev Esp Salud Pública. 2011;85(2):163–74. https://doi.org/10.1590/S1135-57272011000200005.
Puigdefàbregas A, Freitas A, Gispert R, Castellà J, Vidal Gutiérrez C, Medallo Muñiz J, et al. Deaths with medicolegal intervention and its impact on the cause-of-death statistics in Catalonia. Spain Rev Esp Med Leg. 2017;43(1):13–9. https://doi.org/10.1016/j.remle.2017.02.001.
Moreno-Iribas C, Guevara M, Díaz-González J, Álvarez-Arruti N, Casado I, Delfrade J, et al. Completeness of mortality statistics in Navarra. Spain Rev Esp Salud Publica. 2013;87(6):651–7. https://doi.org/10.4321/S1135-57272013000600009.
Simpson D, Rue H, Riebler A, Martins TG, Sørbye SH. Penalising model component complexity: A principled, practical approach to constructing priors. Stat Sci. 2017;32(1):1–28. https://doi.org/10.1214/16-sts576.
Zucker I, Shohat T. Variations in death certification practices distort international comparisons of mortality from diabetes. Eur J Public Health. 2017;27(2):247–50. https://doi.org/10.1093/eurpub/ckw121.
Brooke HL, Talbäck M, Hörnblad J, Johansson LA, Ludvigsson JF, Druid H, et al. The Swedish cause of death register. Eur J Epidemiol. 2017;32(9):765–73. https://doi.org/10.1007/s10654-017-0316-1.
Cirera L, Ballesta M, Arana BM, Chirlaque MD. Professional and activities profiles heterogeneity in the mortality registries in Spain. Gac Sanit. 2022;36(6):553–6. https://doi.org/10.1016/j.gaceta.2022.04.001.
WHO. Internacional Statistical Classification of Diseases and Related Health Problems. Tenth Revision (ICD10). Annex 7.3. 2016;2:213. International Classification of Diseases (ICD). World Health Organization. https://www.who.int/standards/classifications/classification-of-diseases. Accessed 17 November 2023.
Mikkelsen L, Moesgaard K, Hegnauer M, Lopez AD. Anaconda: A new tool to improve mortality and cause of death data. BMC Med. 2020;18(1):1–13. https://doi.org/10.1186/s12916-020-01521-0.
Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. https://doi.org/10.1016/S0140-6736(20)30925-9.
Monasta L, Alicandro G, Pasovic M, Cunningham M, Armocida B, J L Murray C, et al. Redistribution of garbage codes to underlying causes of death: a systematic analysis on Italy and a comparison with most populous Western European countries based on the Global Burden of Disease Study 2019. Eur J Public Health. 2022;32(3):456–462. https://doi.org/10.1093/eurpub/ckab194.
Queiroz BL, Gonzaga MR, Vasconcelos AMN, Lopes BT, Abreu DM. Comparative analysis of completeness of death registration, adult mortality and life expectancy at birth in Brazil at the subnational level. Popul Health Metr. 2020;18(Suppl 1):11–25. https://doi.org/10.1186/s12963-020-00213-4.
World Health Organization. Strengthening civil registration and vital statistics for births, deaths and causes of death. RESOURCE KIT. 2013. https://www.who.int/publications/i/item/strengthening-civil-registration-and-vital-statistics-for-births-deaths-and-causes-of-death. Accessed 17 November 2023.
Jakubowski E. Health care systems in the EU a comparative study. 1998. EPRS: European Parliamentary Research Service. Belgium. 2021. https://policycommons.net/artifacts/1340929/health-care-systems-in-the-eu/1951972/ on 16 Nov 2023. CID: 20.500.12592/wx4w99. Accessed 17 November 2023.
.Papanicolas I, Kringos D, Klazinga NS, Smith PC. Health system performance comparison: new directions in research and policy. Health Policy. 2013;112(1–2):1–3. https://doi.org/10.1016/j.healthpol.2013.07.018.
Cirera L, Zurriaga O. Updating of the official statistics of deaths causes: “Let’s get stronger after the COVID-19 pandemic”. Rev Esp Salud Publica. 2021;95:Perspectivas 1–7.
Hart JD, Sorchik R, Bo KS, Chowdhury HR, Gamage S, Joshi R, et al. Improving medical certification of cause of death: effective strategies and approaches based on experiences from the Data for Health Initiative. BMC Med. 2020;18(1):74, 1–11. https://doi.org/10.1186/s12916-020-01519-8.
Ishitani LH, Cunha CCD, Ladeira RM, Corrêa PRL, Santos MRD, Rego MAS, et al. Evaluation of a smartphone application to improve medical certification of the cause of death. Rev Bras Epidemiol. 2019;22(suppl 3):1–14. https://doi.org/10.1590/1980-549720190014.supl.3.
Adair T, Gamage USH, Mikkelsen L, Joshi R. Are there sex differences in completeness of death registration and quality of cause of death statistics? Results from a global analysis. BMJ Glob Health. 2021;6(10):e006660:1–9. https://doi.org/10.1136/bmjgh-2021-006660.
Erikson R, Torssander J. Social class and cause of death. Eur J Public Health. 2008;18(5):473–8. https://doi.org/10.1093/eurpub/ckn053.
Cirera L, Huerta JM, Chirlaque MD, Overvad K, Lindström M, Regnér S, et al. Socioeconomic effect of education on pancreatic cancer risk in western Europe: An update on the EPIC cohorts study. Cancer Epidemiol Biomarkers Prev. 2019;28(6):1089–92. https://doi.org/10.1158/1055-9965.epi-18-1153.
Washirasaksiri C, Raksasagulwong P, Chouriyagune C, Phisalprapa P, Srivanichakorn W. Accuracy and the factors influencing the accuracy of death certificates completed by first-year general practitioners in Thailand. BMC Health Serv Res. 2018;18(1):478:1–8. https://doi.org/10.1186/s12913-018-3289-1.
Gamage USH, Mahesh PKB, Schnall J, Mikkelsen L, Hart JD, Chowdhury H, et al. Effectiveness of training interventions to improve quality of medical certification of cause of death: systematic review and meta-analysis. BMC Medicine. 2020;18(1):384:1–22. https://doi.org/10.1186/s12916-020-01840-2.
Cirera L, Martínez C, Contreras J, Navarro C. Learning and satisfaction in the workshops of pre- and post-graduate medicine for the improvement of the accuracy of certifications of causes of death 1992–1996. Rev Esp Salud Publica. 1998;72(3):185–95. https://doi.org/10.1590/s1135-57271998000300004.
Cirera L, Vázquez E, Cerdeira S, Sangrador LA, Pérez G, Audicana C. Medical self-training for death certification - Certifica. Rev Esp Salud Publica. 2004;78(3):403–5. https://doi.org/10.1590/S1135-57272004000300010.
Acknowledgements
We like to acknowledge to medical doctor María-Begoña Adiego for results reviewing and to nurses Yugo Floristán, Gloria Gracia and Mariela Sanz for the coding assessment contribution. Also to doctors Inés Sánchez and Humberto Gómez for different medical contributions. Besides, scientists against sexism.
Funding
Public Health Authority, Regional Health Council of Murcia, Spain.
Author information
Authors and Affiliations
Consortia
Contributions
LC made the concept, design, indicators, statistical methods and data interpretation; coordinate and supervised the work, and drafted the first and final version of the manuscript submitted. RB made major contributions on judicial and forensic issues, revised, and approved the submitted version. SM made the bibliographic research, wrote the introduction and results first draft, and revised and approved the submitted version. PM reviewed selected the causes of death, part on materials and supplementary annexes, and revised and approved the submitted version. MB performed the R statistic function software for statistical analysis presentations; made the maps, reviewed results part, and approved the submitted version. MDC checked first draft; allowed administrative placet for Open Access payment; and approved the submitted manuscript version. DS created the R statistic function software, performed statistics analysis, wrote the statistical part of materials and methods, revised different manuscripts, and approved the submitted version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used the secondary data INE collected, verified and published by INE (Instituto Nacional de Estadística, Spanish acronym of the National Statistical Institute of Spain), https://www.ine.es/dyngs/INEbase/en/operacion.htm?c=Estadistica_C&cid=1254736176780&menu=resultados&idp=1254735573175#!tabs-1254736194710. Authorized researchers were allowed to access the micro datasets with de-identification in accordance with the European Union regulations on the Protection of Natural Persons with Regard to the Processing of Personal Data, https://eur-lex.europa.eu/legal-content/EN/TXT/PDF/?uri=CELEX:32016R0679. The data used in this study were anonymized before its use.
The authors did not conduct human subjects research with the INE data for two reasons: (1) The research did not directly involve individual participants, only their aggregated and reported data; and (2) the data available were carefully checked and altered to remove identifying information while preserving its scientific utility.
The authors confirmed that all methods were carried out in accordance with relevant guidelines and regulations.
The need for consent to participate or Ethical approval was deemed unnecessary according to the European Union and national regulations and was waived by the Instituto Nacional de Estadística (INE).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cirera, L., Bañón, RM., Maeso, S. et al. Territorial gaps on quality of causes of death statistics over the last forty years in Spain. BMC Public Health 24, 361 (2024). https://doi.org/10.1186/s12889-023-17616-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17616-1