Abstract
Background
Understanding risk factors linked to work-related musculoskeletal disorders (WMSDs) is crucial for enhancing health promotion and ensuring workplace safety among healthcare professionals particularly physical therapists (PTs). However, in Vietnam, there has been lack of an investigation. Therefore, this study was to determine whether potential risk factors contributed to the occurrence of WMSDs among PTs in Ho Chi Minh City.
Method
An online self-reported questionnaire for WMSDs comprising the Nordic Musculoskeletal Questionnaire (NMQ), Job-risk and Environmental factors, the Perceived Stress Scale (PSS-4) and the coping strategies, were distributed to PTs. They were enrolled if they had: age ≥ 22 years, graduated from PT program, a full-time job with ≥1 year of experience. Unadjusted and adjusted odds ratios (ORs) with 95% confidence intervals (CIs) were determined using Logistic regression.
Results
Our study found that within the past 12 months, the prevalence of WMSDs was 76.4% (n = 204/267): neck 58.4% and lower back 57.3%. PTs aged 22–29 years, < 4 years of education, and < 7 years of working experience were more likely to have WMSDs 2–3 times than those who did not. After adjusting for age, education, and work experience, PTs who engaged in manual techniques/exercises, lifting/transferring patients, and maintaining awkward postures were 5–7 times more likely to have WMSDs in the neck and lower back than those who did not. Environmental and psychological factors, such as number of treatment tables, size of electrotherapy rooms, using PTs modalities, and stress were significantly associated with WMSDs. More than 50% of PTs used modified positions and new treatment/techniques that did not aggravate their symptoms, as coping strategies.
Conclusions
This study indicates potential risk factors associated with WMSDs, affecting the neck and lower back among PTs in Vietnam. These risk factors should be addressed to improve overall PTs health, retain skilled workers, and encourage them to continue working.
Similar content being viewed by others
Introduction
Work-related musculoskeletal disorders (WMSDs) are mainly concerned, not only due to their status as a major health problem with consequences for individual workers, but also because of their substantial impact on socioeconomic aspects [1]. WMSDs typically contribute to a significant portion of occupational morbidity, resulting in lost work days, loss of skilled workers and significant increase of economic costs [2]. Health care professionals such as physicians, dentists, technicians, nurses and physical therapists (PTs) are reported to be vulnerable to sustaining occupational health including WMSDs during the course of their work routine [3]. In Vietnam, Luan et al. (2018) conducted a study on nurses and found that the 12-month prevalence of WMSDs was 74.7%, with low back pain (44.4%) and neck pain (44.1%) being frequently reported [4]. Nong et al. (2020) investigated healthcare workers, including physicians, nurses, technicians, pharmacists, and dentists, and found that 62.4% of them experienced WMSDs. The most commonly affected areas were the lower back (48.2%) and neck (40%) [3]. However, there is currently no report on the prevalence and risk factors associated with WMSDs specifically among Vietnamese PTs.
Physical therapy (PT) has gained significant recognition in Vietnam, resulting in a substantial increase in the number of patients seeking treatment from PTs. However, there is a limited workforce of PTs in Vietnam, which poses a challenge in meeting the demand for healthcare services (40,000 population per physical therapist) [5]. This shortage can lead to stress and overwhelm among PTs, negatively impacting their health and potentially giving rise to occupational diseases such as WMSDs within their workplace [6]. Consequently, it would be advantageous to identify all potential risk factors associated with WMSDs among PTs in order to promote health prevention and make policy recommendations within the profession.
Previous studies have identified and categorized common risk factors for WMSDs among PTs worldwide [6,7,8,9,10,11,12]. Individual and job-risk factors are mainly influenced on WMSDs occurence in PTs. In the systematic review, Vieira et al. (2015) revealed that WMSDs were highly prevalent among PTs worldwide, reaching up to 90% and at least 50% in those who worked 5 years of PT experience [7]. The most commonly affected area was the low back, attributable to WMSDs [7, 9, 10]. Strong evidence suggests that both individual and work-related factors are significantly associated with WMSDs among PTs [7]. In terms of individual risk factors, female PTs aged ≤30 years with a BMI > 25 kg/m2 were more likely to experience WMSDs compared to male who are younger and have lower BMI [11, 12]. Work-related risk factors such as having less than five years of experience, specialization, performing manual therapy techniques, patient transfer, demanding postures, awkward postures, treating a large number of patients, repetitive movements, working while injured, and excessive workload are all significantly associated with WMSDs among PTs (p < 0.05) [6,7,8, 12]. However, there is limited evidence regarding the association between WMSDs and two remaining risk factors: environmental factors and psychological factors among PTs.
WMSDs have a significant impact on PTs, and it is important to explore how they can effectively cope with this situation? Many PTs who have experienced WMSDs reported implementing various reactive/coping strategies such as modifying their techniques, seeking PT treatment, taking medication, consulting doctors, changing their duties, altering clinical habits and work settings, or even leaving their professional positions [6, 8, 13]. However, relying on these coping strategies may not guarantee the sustainability of the PT’s workforce in providing healthcare services [6]. Furthermore, prolonged exposure to this situation can adversely affect their health and quality of life, leading to work inefficiency or early resignation [6, 10].
Therefore, there are two research gaps that need to be addressed. Firstly, lack of the prevalence and risk factors of WMSDs among PTs in Vietnam. Secondly, limited evidence of the association of environmental and psychological factors with WMSDs among PTs. Bridging these gaps and gaining a better understanding of these factors would greatly enhance our approach to preventing and managing WMSDs among physical therapists. Hence, the purpose of this study is to investigate the prevalence of WMSDs and identify potential risk factors contributing to their development among PTs in Ho Chi Minh City (HCMC), Vietnam.
Methods
This study was an online cross-sectional survey started from February to May 2022. It was approved by the Mahidol University Central Institutional Review Board (MUIRB COA No. 2021/412.2009).
Participants were recruited from government and private hospitals, clinics, and centers in Ho Chi Minh City (HCMC). They were screened using the inclusion criteria as follows: a) Vietnamese individuals aged ≥22 years, b) graduated from a PT program, and c) have a full-time job with at least one year of working experience. They were excluded if they worked in administrative jobs and were not involved with PT clinical practice or unable to work as PTs in the last six months due to pregnancy or illness (including mental, neurological, cardio-pulmonary conditions, or other diseases and injuries).
This study developed an online self-reported questionnaire based on many standardized questionnaires used for WMSD’s survey among PTs [10, 13,14,15,16,17,18]. It was translated into Vietnamese language using cross-cultural validation and reported elsewhere [19]. An online self-reported questionnaire (the Vietnamese version) had acceptable content validity and test-retest reliability [19]. It consisted of six sections with 25 items as follows. Section I: individual factor collects information including age, gender, BMI, level of PT education (vocational, diploma, 3-year/4-year Bachelor’s degree, and postgraduate), sport/exercise duration (min/week), current smoking status (yes/no), monthly income (in USD), working hours, years of working experience, number of patients treated per day, and the specialty of hospital/clinic/center (including orthopedic, neurology, pediatric, cardiopulmonary, or general). Section II: musculoskeletal pain asked the participants to rate pain or discomfort in any body part within the last 12 months using the standardized Nordic Questionnaire (NMQ) [14]. If they answered “yes” it referred to having WMSDs and indicated the most pain area by the numeric rating scale (NRS). Section III: work-related factors contained 9 items of job-risk factors [15, 16] that can contribute to WMSD among PTs including manual techniques, manual chest PT, exercise, functional activities training, lift/transfer, clerical work, postures/positions, workload, and personal factor. The rating scale represented the significant problems ranging from 1 to 4. The score < 3 was irrelevant, mild to moderate problems and score ≥ 3 was a major problem. Section IV: environmental factor comprised of 4 items [17] as follows: number of PTs, number of treatment tables, size of treatment room (including electrotherapy, therapeutic and pediatric rooms) and PT electrical modalities (including ultrasound, TENSE/NMES, LASER, SWD, shockwave and others machines). Section V: psychological factor was adopted on the 4-item scale of the Perceived Stress Scale (PSS-4) [18]. Participants were asked to rate their perceived stress over the past month using a 5-point scale ranging from “never” to “almost always.” A score ranged from 0 to 16 and high scores indicate high stress. Section VI: coping strategies for WMSDs [10, 13] included eight items for asking participants to rate the effectiveness of coping strategies from “almost always,” “sometimes,” and “almost never.” This section contains a question prompting participants to propose any additional factors they believe might contribute to their work-related musculoskeletal disorders, if relevant.
For data collection, we initially contacted the manager in each setting located in HCMC for permission to invite PTs participating in this study. PTs received a link of survey using Google Forms (Google Inc., Mountain View, CA, USA) via email, Facebook, messenger, Zalo, or text message. It consisted of a self-reported screening questionnaire and an online self-reported questionnaire (Vietnamese version). A total time to administer an online-survey requires 30 minutes and they have two weeks for completing it.
The sample size was estimated using a formula for prevalence study [20]. Based on the previous studies [11, 21, 22], a prevalence of WMSDs was 0.71 among PTs. The significance level (α) was set at 0.05, and the margin of error was set at 5%. After considering for a non-response rate of 20%, the total sample size was 232 participants.
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 23.0. Descriptive statistics, including the number and percentage (n, %), mean or median, and standard deviation (SD), were present as demographic data. The association between risk factors and WMSDs was examined through multivariate logistic regression. Both unadjusted and adjusted odds ratios (ORs) were calculated and interpreted with their corresponding 95% confidence intervals (95% CIs). An OR is defined as the strength of association between risk factors and WMSDs occurrence among PTs. The formula is the ratio of the odds of risk factors in the WMSDs and the odds of risk factors in none WMSDs. If OR greater than 1.0 indicated a risk factor and positive associated with WMSDs, while an OR less than 1.0 indicated a protective factor and negative associated with WMSDs. Age, level of PT education, and years of experience were identified as potential confounders based on their statistical significance. A p-value was set less than 0.05.
Results
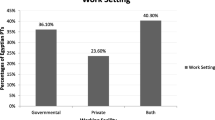
Three hundred twenty-eight PTs working at 27 government hospitals, 17 private hospitals, 27 clinics and 4 centers in HCMC were screened for eligibility by the questionnaire. Of total, 61 PTs were excluded because they did not graduate from PT program (n = 7), less than 1 year of experience in PT practice (n = 7), did not a fulltime job (n = 38) and unable to work as PT in the last 6 months (n = 9) as shown in Fig. 1.267 were enrolled for data analysis. They had 29.5 ± 6.6 years of age and PT experience ranged from 1 to 35 years and provided service for approximately 10 patients per day. Their working hours were 7.9 ± 0.6 hours per day and average 43.1 ± 5.4 hours per week (Table 1).
The results showed that the prevalence of WMSDs among Vietnamese PTs in HCMC was 76.4% (n = 204/267). The most pain of WMSDs (NRS > 3) were reported in the neck (58.4%), lower back (57.3%), shoulders (51.7%), wrists/hands (34.8%), knees (33.0%), upper back (31.5%), thumbs (22.9%), ankles/feet (14.6%), hips/thighs (11.6%) and elbows (7.9%) as illustrated in Fig. 2.
For individual factors, age, level of education, year of experience as PTs and the specialty of hospital/clinic (p < 0.05) were associated with WMSDs among Vietnamese PTs (Table 1). PTs who work at orthopedics settings were less likely to have WMSDs than PTs in general settings 0.42 times (95% CI 0.19 to 0.89, p-value = 0.025).
The results showed the association between work-related factors and WMSDs for overall body area among Vietnamese PTs. Nonsignificant association between work-related factors and WMSDs overall area were observed. Except for PTs who used soft tissue technique were more likely to have WMSDs than those who did not (unadjusted OR = 8.71, 95%CI = 1.15–65.63, p-value = 0.036). After adjusting for age, education and working experience, the soft tissue work was a risk factor of WMSDs among PTs (adjusted OR = 9.05, 95%CI = 1.19–68.77, p-value =0.033).
Tables 2 and 3 demonstrated the work-related factors associated with WMSD at neck and lower back among Vietnamese PTs. The results showed that manual techniques, manual chest PT, exercise, functional activities training, lift/transfer, postures/positions and workload were major contributors to neck and lower back problems among PTs. The unadjusted and adjusted ORs increased the probability of WMSD occurrence at neck related with PTs who performed manual therapy (i.e., joint mobilization, soft tissue work, trigger point release, and segmental breathing), implementing exercise programs (i.e., PROM, performing resistance exercises, manual stretching and PNF techniques), lift or transfer and postures/positions (i.e., maintaining a position for prolonged period of time, bending or twisting in awkward way, squatting or kneeling, and reaching or working away from your body). These findings were also found in the association between work-related risk factors and WMSD at lower back (Table 4). The probability of lower back problems was increased among PTs who performed the same task over and over and continued to work when injured after adjusting for age, education and year of experience.
Table 4 demonstrated the results of environmental and psychological factors associated with WMSDs among Vietnamese PTs. Environmental factors including number of treatment tables (< 12), the size of electrotherapy room (< 20 m2), PT’s modalities (use of US, TENSE/NMES, LASER and SWD) were significantly associated with WMSDs occurrence among PTs. The result showed that PTs who reported high stress (PSS > 5.8) were 1.91 times more likely to develop WMSDs when compared with those who reported low stress (PSS ≤ 5.8) (95% CI 1.00 to 3.60, p-value = 0.047). The unadjusted and adjusted OR of environmental and psychological factors demonstrated the increasing of probability of WMSDs.
The results about the reactive or coping strategies of Vietnamese PTs used for managing WMSDs was illustrated in Fig. 3. To address their WMSDs many of them reported almost always modified their positions or patient positions (52.8%, n = 141/267) and halted the treatment which was aggravated their symptoms and selected the new treatment techniques (40.8%, n = 109/267). More than 20% of them reported almost never to select the plinth/bed height adjustment before treating patients or call someone to handle a heavy patient as the coping strategies for mitigating their WMSD symptoms.
Discussion
This study demonstrated a prevalence of WMSDs within a 12-month among PTs in HCMC, Vietnam, reaching up to 76.4%. The most commonly WMSD affected body areas were the neck (58.4%) and low back (57.3%). Corresponding with many countries, they reported the prevalence of WMSDs ranged from 32 to 99.5% [6,7,8,9,10,11,12,13, 23,24,25]. Our findings corresponded with the prevalence of WMSDs among PTs reported in Southeast Asia [11], which was 71.6%. When compared to the prevalence of WMSDs within a 12-month among other healthcare professions in Vietnam, such as physicians, nurses, technicians, pharmacists, and dentists (ranging from 62.4 to 74.7%) [3, 4], PTs displayed the highest prevalence of WMSDs among health care professions. As a consequence, it is crucial to prioritize the prevention and management of WMSDs as a major concern in order to mitigate the impacts on PTs health and improve occupational health standards in Vietnam.
The association between individual factors and WMSD among Vietnamese PTs
The results also revealed a significant association of individual factors (i.e., age, level of PT education, year of experience as PT and the specialty of hospital/clinic/center) and WMSDs within 12 months among PTs in HCMC. PTs aged lower than 30 years were more likely to have WMSDs than those who are older which are consistent with many previous findings [12, 13, 15]. Younger PTs may not know how to use self-protection strategies such as modifying treatment techniques, alternating treatment modalities, reducing demanding tasks/activities to alleviate the workload issues and have enough rest breaks between cases [12, 13]. PTs who have less years of experience in PT practice (≤7 years) were more likely to develop WMSDs than those who have> 7 years. Our study found that 97.6% (n = 163/167) of PTs aged 22–29 years had less year of experience in PT practice (< 7 years) and 80% of them (n = 131/163) reported WMSDs within 12 months. In addition, young PTs with less experience are more prone to make themselves in dangerous positions at work and face a higher risk of WMSDs compared to senior PTs [12, 13, 26].
Interestingly, our findings found increased risk of WMSDs occurence in Vietnamese PTs who graduated higher degree (4 years and more). Because they learned more intensive courses of 4-year Bachelor and postgraduate programs and led to PTs graduated higher academic degrees taking responsibility in multiple tasks in their work more than those who graduated from the 3-year Bachelor and vocational or diploma programs [25, 27]. Additionally, in Vietnam PTs who graduated 4-year of Bachelor’s program learn more in PT techniques such as joint mobilization and PNF techniques that have been exposed to increase the WMSD risk [12, 13, 25]. These reasons lead to an increase in workloads contributing to WMSDs.
The study found that PTs who work at the hospital/clinic/center with orthopedic specialty were significantly associated with WMSDs. Orthopedic PTs were less likely to develop WMSDs when compared with general PTs (OR = 0.42, 95%CI = 0.19–0.89, p-value = 0.025). General PTs defined more and multiple workloads/activities than specialist PTs (ie., orthopedic PTs defined as clinical specialists in treatment of the musculoskeletal conditions) and it can be a cause of non-specialized PTs had higher risk to develop WMSDs [13]. Additionaly, our study found that general PTs treated more number of patients than orthopedic PTs (10.7 ± 4.9 patients per day for general setting vs. 8.0 ± 4.3 patients per day for orthopedic setting) which one day working is averaged 8 hours. Therefore, the organizations should redesign workload and schedule as well as recruit more PT workforce to reduce the risk of WMSDs and lost effective workers.
The association between work-related factors and WMSD at neck and low back among Vietnamese PTs
Our findings found that performing manual therapy, implementing exercise programs, lifting or transferring, postures or positions, workload issues and personal factors were reported by PTs as the major contributing factors for WMSDs at neck and lower back. After minimizing the effect of age, education and year of PT experience, the probability to develop WMSDs at neck and lower back increased twice as much among PTs who were exposed to work-related risk factors. Many previous studies [6, 10, 11] reported that performing manual therapy techniques were the most common work-related risk factors contributing to WMSDs at neck and lower back problems among PTs. Mobilization and soft tissue work and trigger point release techniques are hand-on treatment which can cause of neck, lower back, thumb symptoms [12, 13].
Functional activities training including ADL, gait and stair training were significantly associated with neck and lower back problems among Vietnamese PTs. This might be explained by prolonged standing with lifting or caring patients with frequent twisting and bending when taking care of patients to perform ADL, walking and stair climbing [11]. It is a common cause of neck, upper-limb and lower back problems among PTs.
Lifting or transferring patients and posture/position were the most common cause of neck pain and low back pain in all workers including PTs. Our findings aligned with many previous studies which reported lifting or carrying patients, sustained in the same position or in the awkward twisting position or uncomfortable position, increased risk of neck and lower back problems among PTs [6, 9,10,11, 13]. Therefore, PTs should be trained and followed preventive strategies at work incorporated with strengthening and flexibility exercise for preventing WMSDs [26].
The previous studies reported that repetitive task and continuing work when having musculoskeletal injuries contributed to more than double times of lower back problem because of prolonged stress of soft tissue [12, 13]. In Vietnam, there are limited number of PT workforce which lead them to response to treat large number of patients per day in various conditions. Although our study found nonsignificant association between number of treating patients per day and WMSDs among Vietnamese PTs (p = 0.09), the maximum number of treating patients reached up to 20 patients per day and the average was 9.93 ± 4.79 patients per day. This might contribute to increased clinical workloads and risk of WMSDs among PTs. Consistent with many previous studies [11, 13, 22, 28], Cromie et al. (2000) [13] discovered PTs who treat a large number of patients simultaneously had a statistically significant 2.5 times higher odds of experiencing WMSDs compared to those who did not (95% CI 1.6 to 3.8). Ezzatvar et al. (2020) [22] similarly highlighted that PT who treat a substantial number of patients were 2.14 times more likely to develop WMSDs when compared with those who did not (95% CI 1.53 to 2.99).
The association between environmental and psychological factors and WMSD among Vietnamese PTs
This study found that environmental factors including number of treatment tables < 12, size of electrotherapy room < 20 m2 and using PT electrical modalities were significantly associated with WMSDs among Vietnamese PT in HCMC (p < 0.05). Using PT electrical modalities including US, TENSE/NMES, LASER and SWD increased the odds of WMSDs occurrence 2–3 times among PTs. Our findings are contrasted to the previous studies. They reported using electrical modalities are less commonly practice among PTs which might not expose PTs to a high level of risk for WMSDs [11]. Cromie et al. found that injured PTs selected electrotherapy modalities as reactive/coping strategies for self-preservation and enabling themselves to continue working [11, 13]. However, using electrical modalities are most commonly treatment among PTs in Asia particularly in Vietnam. Normally, PTs are assigned to work in an electrotherapy room for one week or month and they might hold the ultrasound transducer for 8 hours of workday or provide various type of PT modalities to consecutive patients. Combined with a high workload of large number of treating patients per day with insufficient number of treatment tables and small treatment room can lead to increase the risk of WMSDs. Therefore, we suggested to modify working scheduling for PTs to avoid performing high workload with a long period.
This study also indicated a notable association between psychological factor including perceived stress and the occurrence of overall WMSDs among PTs in HCMC. This observation aligns with previous studies [18, 28, 29], specifically highlighting that Vietnamese PTs experiencing high stress levels were more prone to the risk of developing WMSDs.
Reactive or coping strategies used to mitigate risk of WMSDs by Vietnamese PTs
Our study showed the responses about the self-protection to reduce WMSDs symptoms on their body whilst completing work duties. The most coping strategies were modifying the patients’/therapists’ position, selecting techniques that will not aggravate discomfort, stopping treatment if it causes discomfort and adjusting the plinth/bed height before treating a patient. The coping strategies of WMSDs among Vietnamese PTs are the same as those of PTs from other countries [9, 10, 13]. Additionally, to reduce the prevalence of WMSDs among PTs, Campo et al. (2008) [30] proposed that protective measures for lifting or transferring patient should be considered and used suitable equipment such as height-adjustable beds and sliding/lifting equipment. The protevtive measures for performing manual therapy by using assistive devices (e.g., thumb splints, mobilization wedges and instruments assisted soft tissue working) and by considering only applying these techniques on patients who truly needs were also recommended [30]. The role of the Physical Therapy Association is important in formulating and promoting the prevention strategies [30].
Based on Passier and McPhail (2011) [31], Cromie et al. (2001) [32] and the hierarchy of control for improving the work process [33], this study recommended six strategies for prevention WMSDs among PTs. First was an organisational strategy to manage task/workload such as defining PT roles to reduce physical demands and ensuring an appropriate workforce to help. Second was workload arrangement including PTs should take rest of breaks during working or while injuries, regularly perform stretching exercises on targeting muscles affected, and plan an acceptable number of patients treated by PTs per working hour per day. Third, PTs should allow to modify treatment techniques to avoid injuries or aggravate the symptom. Fourth, work setting and provision of equipment suitable for appropriate purpose and sufficient quantities. Fifth focused on improving overall physical health, maintaining a healthy lifestyle, engaging in regular physical activity outside of work, managing stress and having schedule check-ups with professionals to address any health issues especially discomfort or pain. Sixth was education and training PTs can attend workshop or training sessions for proper body mechanics and injury preventions during working.
Limitations
This study had some limitations that need to be acknowledged. Firstly, being an online self-reported cross-sectional survey, there might have been a potential for recall and information bias among participants. However, to mitigate these issues, we provided clear descriptions and examples in the questionnaire, and participants were encouraged to provide honest responses. Secondly, the data collection occurred during the COVID-19 outbreak in HCMC, Vietnam, which could have influenced respondents’ answers. Some PTs may have experienced changes in their tasks and settings due to the pandemic’s impact. During the three-month lockdown from July to September 2021, PTs were redirected to support the treatment of COVID-19 patients, leading to a high clinical workload and potential challenges in developing WMSDs. Despite these circumstances, we explicitly instructed respondents to base their answers on their usual work-related activities as PTs.
Conclusion
This study revealed a 12 months prevalence of WMSDs among PTs in HCMC, Vietnam reaching 76.4%. Notably, neck pain and low back pain were the most commonly affected areas. Our investigation comprehensively identified all potential risk factors associated with WMSDs among physical therapists, encompassing individual, work-related, environmental, and psychological factors to promote health prevention and workplace safety recommendations within the profession.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to organizational confidential but are available from the corresponding author on reasonable request.
Abbreviations
- WMSDs:
-
Work-related musculoskeletal disorders
- PTs:
-
Physical Therapists
- HCMC:
-
Ho Chi Minh City
- BMI:
-
Body Mass Index
- PT:
-
Physical Therapy
- NMQ:
-
the standardized Nordic Questionnaire
- NRS:
-
Numerical pain rating scale
- US:
-
Ultrasound
- TENS/NMES:
-
Transcutaneous Electrical Nerve Stimulation/Neuromuscular Electrical Stimulation
- LASER:
-
Light amplification by stimulated emission of radiation
- SWD:
-
Shortwave diathermy
- PROM:
-
Passive range of motion exercises
- AAROM:
-
Active-assisted range of motion exercises
- ADL:
-
Activity of daily living
- PNF:
-
Proprioceptive Neuromuscular Facilitation
- PSS:
-
The Perceived Stress Scale.
References
Schneider E, Irastorza X, Safety E, Copsey S, Verjans H, Eeckelaert L: OSH in Figures: Work-related musculoskeletal disorders in the EU — Facts and Figures 2010. Avialable from https://osha.europa.eu/en/publications/osh-figures-work-related-musculoskeletal-disorders-eu-facts-and-figures. Accessessed on 21 Nov 2022.
World Health Organization (WHO). Occupational health: health workers. Avialable from https://www.who.int/news-room/fact-sheets/detail/occupational-health%2D%2Dhealth-workers Accessed on 30 July 2022.
Nong TV, Kesornthong S, Homkham N. Work–related musculoskeletal disorders among healthcare workers in a general provincial hospital in Vietnam. IJEG. 2020;10(1):18–26.
Luan HD, Hai NT, Xanh PT, Giang HT, Van Thuc P, Hong NM, et al. Musculoskeletal disorders: prevalence and associated factors among district hospital nurses in Haiphong. Vietnam BioMed Res Int. 2018; https://doi.org/10.1155/2018/3162564.
World Physiotherapy (WPT) Vietnam Physical Therapy Association. Avialable from https://world.physio/membership/vietnam Accessed on 30 July2022.
West DJ, Gardner D. Occupational injuries of physiotherapists in north and Central Queensland. Aust J Physiother. 2001;47(3):179–86.
Vieira E, Schneider P, Guidera C, Gadotti I, Brunt D. Work-related musculoskelet disorders among physical therapists: a systematic review. J Back Musculoskeletal Rehabil. 2015;29:417–28. https://doi.org/10.3233/BMR-150649.
Khairy WA, Bekhet AH, Sayed B, Elmetwally SE, Elsayed AM, Jahan AM. Prevalence, profile, and response to work-related musculoskeletal disorders among Egyptian physiotherapists. Maced J Med Sci. 2019;7(10):1692–9.
Salik Y, Ozcan A. Work-related musculoskeletal disorders: a survey of physical therapists in Izmir-Turkey. BMC Musculoskelet Disord. 2004;5:27.
Adegoke BO, Akodu AK, Oyeyemi AL. Work-related musculoskeletal disorders among Nigerian physiotherapists. BMC Musculoskelet Disord. 2008;9:112.
Nordin NAM, Leonard JH, Thye NC. Work-related injuries among physiotherapists in public hospitals: a southeast Asian picture. Clinics (Sao Paulo). 2011;66(3):373–8.
Chen CY, Lu SR, Yang SY, Liang FW, Wang JJ, Ho CH, et al. Work-related musculoskeletal disorders among physical therapists in Taiwan. Medicine (Baltimore). 2022;101(7):e28885. https://doi.org/10.1097/MD.0000000000028885.
Cromie JE, Robertson VJ, Best MO. Work-related musculoskeletal disorders in physical therapists: prevalence, severity, risks, and responses. Phys Ther. 2000;80(4):336–51.
Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon. 1987;18(3):233–7.
Bork BE, Cook TM, Rosecrance JC, Engelhardt KA, Thomason ME, Wauford IJ. Work-related musculoskeletal disorders among physical therapists. Phys Ther. 1996;76(8):827–35.
Holder NL, Clark HA, DiBlasio JM, Hughes CL, Scherpf JW, Harding L. Cause, prevalence, and response to occupational musculoskeletal injuries reported by physical therapists and physical therapist assistants. Phys Ther. 1999;79(7):642–52.
Darragh AR, Campo M, King P. Work-related activities associated with injury in occupational and physical therapists. Work. 2012;42(3):373–84.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Le TTT, Jalayondeja C, Jalayondeja W, Mekhora K, Bhuanantanondh P: Content validity and test-retest reliability of self-reported online questionnaire for work-related musculoskeletal disorders among physical therapists at Ho Chi Minh city, Vietnam. Proceedings of the International Physical Therapy Research Symposium 2022 Thailand 2022 June 9; 131–44. [https://allied.tu.ac.th/data/proceedings/].
Naing L, Winn T, Rusli BN. Practical issues in calculating the sample size for prevalence studies. Arch Orofac Sci. 2006;1:9–14.
Dao HT, Pichaiyongwongdee S, Sullivan PE, Prasertsukdee S, Apinonkul B. Are physical therapists in Viet Nam ready to implement evidence-based practice? A survey. BMC Med Educ. 2018;18(1):317.
Ezzatvar Y, Calatayud J, Andersen LL, Aiguadé R, Benítez J, Casaña J. Professional experience, work setting, work posture and workload influence the risk for musculoskeletal pain among physical therapists: a cross-sectional study. Int Arch Occup Environ Health. 2020;93(2):189–96.
Meh J, Bizovičar N, Kos N, Jakovljević M. Work-related musculoskeletal disorders among Slovenian physiotherapists. J Health Sci. 2020;10(2):115–24.
Gorce P, Jacquier-Bret J. Global prevalence of musculoskeletal disorders among physiotherapists: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2023;24(1):265.
Abu-Taleb W, Rehan YA. Work-related musculoskeletal disorders among Egyptian physical therapists. Bull Fac Phys Ther. 2021;26:7.
Desai RG, Shah MK. Prevention of work-related musculoskeletal disorders in physiotherapist - a review. IJRR. 2021;8(12) https://doi.org/10.52403/ijrr.20211261.
Tembo LN, Munyikwa JP, Musoro C, Majonga G, Mavindidze E. Prevalence of work-related musculoskeletal disorders and associated factors among University of Zimbabwe Faculty of medicine and health sciences non-academic workers: a cross-sectional study. BMC Musculoskelet Disord. 2023;24:792. https://doi.org/10.1186/s12891-023-06900-1.
Anderson SP, Oakman J. Allied health professionals and work-related musculoskeletal disorders: a systematic review. Saf Health Work. 2016;7(4):259–67. https://doi.org/10.1016/j.shaw.2016.04.001.
Campo MA, Weiser S, Koenig KL. Job strain in physical therapists. Phys Ther. 2009;89:946–56.
Campo M, Weiser S, Koenig KL, Nordin M. Work-related musculoskeletal disorders in physical therapists: a prospective cohort study with 1-year follow-up. Phys Ther. 2008;88(5):608–19.
Passier L, McPhail S. Work related musculoskeletal disorders amongst therapists in physically demanding roles: qualitative analysis of risk factors and strategies for prevention. BMC Musculoskelet Disord. 2011;12:24.
Cromie JE, Robertson VJ, Best MO. Occupational health and safety in physiotherapy: guidelines for practice. Aust J Physiother. 2001;47:43–51.
The National Institute for Occupational Safety and Health (NIOSH). Hierarchy of Controls. Available from https://www.cdc.gov/niosh/topics/hierarchy/default.html. Accessed on 23 Nov 2023.
Acknowledgments
This study was supported by the Global Talent Research Funding of Mahidol University, Thailand. We would like to thank all physical therapists in Ho Chi Minh City (HCMC) who participated in this study for data collection.
Funding
Open access funding provided by Mahidol University This study was supported by the Global Talent Research Funding of Mahidol University, Thailand.
Author information
Authors and Affiliations
Contributions
TTT.L and C.J. conducted literature review and designed the study. W.J., K.M. and P.B. advised and supported equipment for data collection. TTT.L and C.J. collected and analyzed data. All authors help to write and prepare manuscript for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Mahidol University Institutional Review Board (MUIRB COA No. 2021/412.2009) and an informed consent was obtained from all subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Le, T.T.T., Jalayondeja, W., Mekhora, K. et al. Prevalence and risk factors of work-related musculoskeletal disorders among physical therapists in Ho Chi Minh City, Vietnam. BMC Public Health 24, 6 (2024). https://doi.org/10.1186/s12889-023-17527-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17527-1