Abstract
Background
Fractures present serious health challenges for older adults, including premature mortality and reduced quality of life. Obesity has become significantly prevalent in China. However, the association between obesity and fractures remains unclear. This study aimed to assess the association between obesity and fractures among Chinese women above 50 years of age.
Methods
A prospective cohort study was designed based on the China Health and Nutrition Survey, using data from 1997 to 2015. The average follow-up duration was seven years. Trained investigators measured body mass index (BMI) and waist circumference (WC) at baseline. Obesity was defined according to World Health Organization recommendations. Waist-to-height ratio (W-HtR) was calculated, with 0.5 as the cutoff value. Onset of fractures, self-reported by the participants during the follow-up period, was the primary outcome. Cox hazard regression models were used to assess the association between BMI, WC, W-HtR and subsequent risk of fracture. A sensitivity analysis was conducted by multiple imputation of missing data on the variables at baseline.
Results
A total of 2,641 women aged ≥ 50 years were involved in the study. In all the models, no significant association existed between BMI and fracture risk. However, women with WC ≥ 88 cm had significantly higher risk of fracture than those with WC < 80 cm according to both the unadjusted (HR = 1.744, 95% CI: 1.173–2.591) and adjusted models (HR = 1.796, 95% CI: 1.196–2.695). In addition, W-HtR and fracture risk were positively associated according to both the unadjusted (HR = 1.798, 95% CI: 1.230–2.627) and adjusted models (HR = 1.772, 95% CI: 1.209–2.599). Results of the sensitivity analysis were consistent with those of the above analyses.
Conclusions
Abdominal obesity increased the risk of all-cause fractures in Chinese women ≥ 50 years old. Intervention strategies and measures to prevent or address abdominal obesity would be helpful to decrease the fracture incidence.
Similar content being viewed by others
Introduction
Fractures are a health problem associated with premature mortality and reduced quality of life in older adults [1]. From 1990 to 2019, the absolute number of fractures worldwide increased by 33.4%, with older people involved in the majority of events [2]. Older women have a higher risk of fractures than do older men. In the China National Fracture Study, a nationally representative study including more than half a million people, women aged > 55 years had a significantly higher incidence of fracture than did women of other age groups and males of the same age group [3].
Multiple factors affect the risk of fractures. However, the association between obesity and fractures remains unclear. Several cohort studies have evaluated the relationship between obesity and fractures in older women in different regions worldwide. Even for the same fracture type, the results were conflicting. For example, for hip fractures, multiple studies have observed the protective role of obesity [4,5,6,7], whereas others have reported the risk effect of obesity based on a linear or U-shaped relationship [8,9,10]. The inconsistency in the results may be related to the heterogeneity of the population in terms of race, levels of obesity, and status of exposure to other risk factors for fracture (such as age, body composition, and lifestyle) [11].
The biological mechanisms underlying the impact of obesity on fractures are complex, and include biological and mechanical factors [12]. Excess fat mass plays an important role in bone loss by increasing the release of inflammatory cytokines, which are more pronounced in central obesity [13]. In addition, differences in the distribution of adipose tissue in the body may result in different mechanical mechanisms [13]; therefore, the impact of general and central obesity on fracture risk may differ [14].
In recent decades, the prevalence of obesity in China has increased significantly because of the acceleration of industrialisation and lifestyle transformation. According to the Report on Nutrition and Chronic Diseases in China (2020), more than 50% of adults assessed between 2015 and 2019 were overweight or obese [15]. In 2019, China had the second-highest disability-adjusted life years score owing to fractures related to low bone mass among 204 countries and territories [16]. Therefore, it is necessary to evaluate the relationship between obesity and fractures in China, where the population is ageing rapidly [17]. However, there is limited prospective research in China. In this study, we aimed to provide such relevant evidence from China. Based on a nationwide sample, a prospective study design was adopted to evaluate the association between general and abdominal obesity and fracture risk in Chinese women ≥ 50 years old.
Methods
Study population
The data for this study were obtained from the China Health and Nutrition Survey (CHNS), a longitudinal survey initiated in 1989 in China to observe how the social and economic transformation of Chinese society affects the health and nutritional status of the Chinese population [18]. Nine additional waves followed in 1991, 1993, 1997, 2000, 2004, 2006, 2009, 2011, and 2015. More than 30,000 participants from more than 7,200 households, comprising 15 provinces and autonomous cities or districts, participated in the study, were selected using multistage random cluster sampling [19]. The CHNS was approved by the Institutional Review Boards at the University of North Carolina at Chapel Hill and the National Institution for Nutrition and Food Safety, China Center for Disease Control and Prevention. All participants provided signed informed consent [18].
Selection of participants
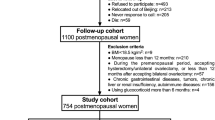
In this study, data from 1997 to 2015 were used because fracture data were only available from 1997. A total of 2,641 women were included in this study. The selection procedure for the study participants is shown in Fig. 1.
Participants were included according to the following criteria: (1) women aged ≥ 50 years; (2) had participated in at least two waves; (3) had never undergone a fracture at baseline; (4) had reported their age at first fracture; and (5) were fracture-free at baseline year.
Measure of exposure
Height, weight, and waist circumference (WC) of the participants were determined. The height of the participants was measured without footwear, using a portable SECA stadiometer (SECA, Hamburg, Germany) accurate to 0.1 cm [20]. The weight of the participants (who wore light clothing and no footwear), was measured using a calibrated beam scale (SECA882) before 2015 and a body composition tester (TANITA BC601) in 2015 with a measurement accuracy of 0.1 kg [20]. WC was measured to the nearest 0.1 cm above the navel with the participant breathing naturally and standing upright, using a Seca201 non-elastic tape [21]. Body mass index (BMI) was calculated as weight in kg divided by height in metres squared (m2). To enhance comparability of our findings with those from other countries, the World Health Organization’s recommendations for overweight and obesity were used. The BMI was classified into underweight (< 18.5 kg/m2), normal (18.5 kg/m2–24.9 kg/m2), overweight (25.0 kg/m2–29.9 kg/m2), and obese (≥ 30 kg/m2) [22]. WC was categorised as normal (< 80 cm), pre-obese (80–87.9 cm), or abdominal obesity (≥ 88 cm) [23]. In this study, waist-to-height ratio (W-HtR) was calculated as the ratio of WC to height. The cutoff value of W-HtR was defined as 0.5 [24].
Measure of outcome
The onset of fractures was the primary outcome of this study. During each wave, the investigators asked the participants whether they had undergone fractures, and if so, the total number of fractures, and their age at the time of the first fracture. Participants who did not report having undergone a fracture during any wave were considered to have undergone no fractures. Among women who reported fractures, those who could not recall their age at the time of the first fracture were excluded. For any wave, participants reporting the first fracture at an age lower than the baseline age or higher than the current age at the time of the interview were also excluded. Among the remaining participants who had undergone a fracture, the first recalled age of the first fracture was used as the time of occurrence of the outcome to reduce information bias. The follow-up period considered was the number of years from the participant’s first interview to the endpoint or last interview.
Definition of covariates
The baseline information of the following factors, which were measured using a structural questionnaire, was adopted as covariates: demographic factors (age, nationality, marital status, education level, income, place of residence, and wave); lifestyle behaviours (smoking, alcohol consumption, and physical activity); personal disease history (hypertension and/or diabetes); and dietary intake (energy, protein, fat, and carbohydrates). Family income per capita was inflated to values prevalent in 2015, and was then adopted as an indicator of income. Place of residence was recorded as rural or urban. Smoking status was recorded with the following question: “Have you ever smoked cigarettes?” (yes or no). Alcohol consumption was recorded via the query: “Did you drink beer or any other alcoholic beverage last year?” (yes or no). Physical activity was measured based on occupational, home, transportation, and leisure activities. The weekly consumption of the metabolic equivalent of task (MET) hours was used to measure the physical activity of the participants, calculated by multiplying the MET per hour and the duration (hours) per week of the activities. The MET per hour for each physical activity type was obtained from the Compendium of Physical Activities [25]. To obtain the daily dietary intake of energy (kcal), protein (g), fat (g), and carbohydrates (g), the dietary records method of three consecutive days was used [26]. In the present study, menopause status could not be included since CHNS did not collect information regarding menopause in adults from 1997.
Statistical analysis
Skewed continuous variables were described as medians (interquartile ranges). Quantitative variables were described as frequencies and proportions. The distributions of covariables among the groups of BMI, WC, and W-HtR were compared using the rank sum test (for skewed distribution quantitative data) or the chi-squared test (for qualitative data). The log-rank test was used to compare fracture incidences among the exposure groups for each covariable. Factors associated with both anthropometric indexes (BMI, WC, and W-HtR) and fracture incidence were considered potential confounders, with the screening criteria set at P ≤ 0.1. The Cox hazard regression model was used to assess the association between obesity and subsequent risk of fracture. Hazard ratio (HR) was calculated using unadjusted and adjusted models that included the potential confounders mentioned above.
Owing to the missing baseline values of some variables, a sensitivity analysis was conducted. We imputed the missing data of the variables in Table 1 under the missing-at-random assumption using multiple imputation with a regression switching approach (chained equations with m = 10). The imputation procedure was performed using a linear regression method for continuous variables, and an ordinal or binary logistic regression model for categorical variables. Partial regression coefficients with 95% CI were combined with those in different imputed datasets using Rubin’s rules [27].
Statistical analyses were performed using STATA 12.0, using a two-tailed test with significance set at 0.05.
Results
Distribution of basic characteristics among participants
The basic characteristics of the participants are shown in Table 1. The median age of the participants was 60 (54, 66) years. The median BMI, WC, and W-HtR at baseline were 23.4 (20.9, 26.1) kg/m2, 81.0 (74.0, 89.0) cm, and 0.53 (0.48, 0.58), respectively (Table 1).
Analysis of BMI of the participants showed that compared with underweight women, normal weight, overweight, or obese women were more likely to live in urban areas, be of Han nationality, be educated up to senior high school level or above, be married, be non-smokers, and have a history of hypertension and diabetes (all P < 0.05). They were also younger, had a higher income, and had a higher dietary intake of fat and protein, but a lower dietary intake of carbohydrates (all P < 0.05) (Table 2).
Analysis of WC of the participants showed that compared with women of normal weight, pre-obese and obese women were more likely to live in cities, be of Han nationality, be educated up to junior high school or above, be married, be non-smokers, and have a history of hypertension and diabetes (all P < 0.05). They also had a higher income, a lower intensity of physical activity, a higher dietary intake of protein, but a lower dietary intake of carbohydrates (all P < 0.05) (Table 2).
Compared with women whose W-HtR ≤ 0.5, women with W-HtR > 0.5 were more likely to be younger, be of Han nationality, be non-smokers, and have a history of hypertension and diabetes (all P < 0.05). They also had higher income, a lower intensity of physical activity, and a lower dietary intake of carbohydrates (all P < 0.05) (Table 2).
In addition, the distribution of waves at baseline differed significantly among the BMI, WC, and W-HtR groups (all P < 0.05) (Table 2).
Association between basic characteristics and fracture risk
The median (interquartile range) follow-up period was 7.0 (4.0, 14.0) years with 22,977 person-years. A total of 149 fractures were reported during follow-up. Women living in urban areas, educated up to junior high school education or below, and with a high dietary intake of fat had a significantly higher risk of fractures (all P < 0.05). Women aged ≥ 60 years or with a higher dietary energy intake had a marginal higher risk of fracture (all P < 0.1) (Table 3).
Association between BMI and fracture risk
Fracture incidence among participants with BMI < 18.5 kg/m2, 18.5–24.9 kg/m2, 25–29.9 kg/m2, and ≥ 30 kg/m2 was 5.7, 5.8, 7.6, and 9.2 per 1000 person-years, respectively. First, we assessed the association between BMI and fracture risk without including missing data. There was no association between BMI and fracture risk in either the unadjusted (model 1) or adjusted (model 2) models. Similarly, after imputing the missing baseline data for the variables shown in Table 1, no significant association was observed between BMI and fracture risk in either the unadjusted (model 3) or adjusted (model 4) models (Table 4).
Association between WC and fracture risk
Fracture incidence among participants with WC < 80 cm, 80–87.9 cm, and ≥ 88 cm was 5.1, 6.3, and 8.8 per 1000 person-years, respectively. Without imputation of missing data at baseline, and considering WC < 80 cm as a reference, a significant increase in fracture risk was observed for the group with WC ≥ 88 cm in both the unadjusted (model 1: HR = 1.744, 95% CI: 1.173–2.591) and adjusted models (model 2: HR = 1.796, 95% CI:1.196–2.695) after adjusting for age, wave, geographic region, education level, and dietary fat intake. After imputation of missing data at baseline, women with WC ≥ 88 cm had a significantly higher risk of fracture than did those with WC < 80 cm in both the unadjusted (model 3: HR = 1.680, 95% CI: 1.137–2.482) and adjusted models (model 4: HR = 1.704, 95% CI: 1.143–2.541) involving age, wave, geographic region, education level, and dietary fat intake (Table 4).
Association between W-HtR and fracture risk
Fracture incidence among participants with W-HtR ≤ 0.5 was 4.3/1000 person-years, while those for women with W-HtR > 0.5 was 7.7/1000 person-years. Without imputation of missing data at baseline, the fracture risk was significantly higher for the W-HtR > 0.5 group than for the W-HtR ≤ 0.5 group, no matter the unadjusted (model 1: HR = 1.798, 95% CI: 1.230–2.627) or adjusted model (model 2: HR = 1.772, 95% CI: 1.209–2.599) after adjusting for age, wave, and dietary fat intake. After imputation of missing data at baseline, women with W-HtR > 0.5 had a significantly higher risk of fracture than did those with W-HtR ≤ 0.5 in both the unadjusted (model 3: HR = 1.701, 95% CI: 1.160–2.495) and adjusted models (model 4: HR = 1.693, 95% CI: 1.149–2.494) involving age, wave, and dietary fat intake (Table 4).
Discussion
In this study, we did not observe a significant association between BMI and all-cause fracture risk, whereas positive associations between WC, W-HtR, and fracture risk were observed among Chinese women above 50 years of age.
Obesity was originally thought to reduce the risk of fractures, owing to a higher bone mineral density (BMD) in obese individuals, and the protective role of soft tissue padding against falls [28]. However, this viewpoint has been challenged by several epidemiological studies, especially those in postmenopausal women, which have observed a positive association between obesity and fracture [29,30,31]. The mechanism underlying obesity-related fractures is also controversial. In addition to the higher BMD owing to mechanical loading [28], oestrogen synthesis mechanisms may help postmenopausal obese women maintain bone homeostasis. After menopause, oestrogen biosynthesis is catalysed by aromatase, mainly in the adipose tissue, which converts adrenal androgens into oestrogens [32]. This promotes osteoclast apoptosis, osteogenesis, and mesenchymal stem cell differentiation, while inhibiting osteoclastogenesis from preosteoblasts to osteoblasts [33].
However, studies have also revealed the negative effects of obesity on bones. First, obese individuals have a higher risk of falls [34]. Moreover, multiple epidemiological studies have found that obese individuals have lower vitamin D concentrations than do non-obese individuals [35]. The underlying mechanisms may include volumetric dilution, sequestration of vitamin D into adipose tissue, limited sunlight exposure, and decreased vitamin D synthesis in vivo [35]. In addition, the hypermetabolic status of bone marrow stromal cells, and an accelerated senescent bone marrow microenvironment (such as expanded bone marrow adipose tissue) in obese individuals, leads to increased bone fragility [36].
In our study, we did not observe an association between BMI and fracture risk in women ≥ 50 years old. In a meta-analysis of 12 cohort studies, of which 11 used BMI as the obesity level indicator, overweight and obesity was associated with an decreased risk of all-cause fractures in postmenopausal women (HR = 0.86, 95% CI: 0.77–0.97) [11]. However, a recent cohort study with 456,921 participants from the UK biobank revealed a U-shape relationship between BMI and fracture, with the lowest risk of fracture in overweight participants [14].
In the present study, we noted that the all-cause fracture incidence was similar for both underweight and normal weight women, which then increased with BMI. The lack of an association between BMI and fracture risk may be related to the limitations of the sample size. In our study, the median BMI of the participants was 23.4 kg/m2, and the proportion of obese participants was only 5.39%, with a highest BMI value of 37.5 kg/m2. Therefore, the association between BMI and fracture risk in Chinese women above 50 years of age may need to be evaluated in a larger sample.
However, it is worth noting that the BMI has certain limitations. It cannot distinguish individuals with excess body fat from those with high muscle mass. And it cannot reflect the characteristics of fat distribution either [24]. Therefore, when assessing the relationship between BMI and fracture risk, different body fat mass and fat distribution among study populations may lead to different observations among studies.
In the present study, apart from WC, W-HtR, which has a superiority over WC and BMI for detecting cardiometabolic risk factors in adults, was used to assess abdominal obesity [37]. The results showed that abdominal obesity significantly increased the risk of fracture in all models based on either WC or W-HtR. This finding is consistent with the results of several previous studies. A recent prospective study in Iran found that postmenopausal women with WC ≥ 95 cm had a significantly higher risk of incident-hospitalised fracture (HR = 2.43, 95% CI: 1.53–3.86) [38]. In Zhu’s study [14], a linear positive correlation between WC adjusted for BMI and fracture risk was observed in older women (HR = 1.02, 95% CI: 1.01–1.02, P = 1.72E-11), which was supported by leveraging genetic instrumental variables.
Abdominal obesity is characterised by excessive visceral fat and is often accompanied by metabolic disorders [39]. The crucial role of cytokines (such as TNF-ɑ, IL-6) produced in adipose tissue in increasing the risk of osteoporosis has been revealed [12]. TNF-ɑ could promote the production of osteoclasts, synergise with cytokine RANKL, facilitate RANK-RANKL binding [40], and up-regulate the expression of RANKL, which promotes resorptive activity of osteoclasts [41]. IL-6 promotes osteoclast production and bone resorption by stimulating mesenchymal progenitor differentiation into the osteoblastic lineage and mediating the stimulatory effects of TNF [42]. Compared with subcutaneous fat, visceral fat secretes cytokines more actively. This could explain the increase in the risk of fractures with increased WC in postmenopausal women.
The distribution of fat tissue changes with age, being marked by increasing visceral adipose tissue and decreasing subcutaneous adipose tissue [12]. In this study, the median WC of the participants was 81 cm, and the proportion of abdominal obesity was 28.7%, suggesting that abdominal obesity may be more common than general obesity in Chinese women above 50 years of age. According to the data from the China PEACE Million Persons Project, from 2014 to 2018, the proportion of women with WC ≥ 85 cm in the 55–64 and 65–75 years old groups was 42.5% and 46.3%, respectively [43]. Thus, the population attributable risk proportion of abdominal obesity on fracture risk may be relatively high in Chinese women ≥ 50 years of age, which requires the attention of health departments.
The strength of our study is that it was based on a nationwide sample combined with a prospective study design to assess the association between obesity and fracture in Chinese women above 50 years of age. To the best of our knowledge, this is the first nationwide prospective study to assess the association between obesity and fracture risk in China. However, this study has some limitations. First, fracture history and age at first fracture were mainly self-reported by the participants; thus, information bias may exist. Second, we did not collect information regarding the fracture site. The associations between obesity and fracture may differ for different sites. Last, the study did not collect information on bone density or on the reason behind the first fracture; therefore, it was difficult to analyse the mechanism underlying the relationship between obesity and fracture.
Conclusions
Abdominal obesity increased all-cause fracture risk for Chinese women ≥ 50 years, which suggests the importance of abdominal obesity intervention in preventing fracture in middle aged and older Chinese women. Further studies with larger sample sizes are required to elucidate the relationship between general obesity and fracture.
Availability of data and materials
The data that support the findings of this article are available from the public, open access website (https://www.cpc.unc.edu/projects/china/data/datasets).
Abbreviations
- BMD:
-
Bone mineral density
- BMI:
-
Body mass index
- CHNS:
-
China Health and Nutrition Survey
- HR:
-
Hazard ratio
- MET:
-
Metabolic equivalent of task
- WC:
-
Waist circumference
- W-HtR:
-
Waist-to-height ratio
References
Alajlouni DA, Bliuc D, Tran TS, Blank RD, Center JR. Muscle strength and physical performance contribute to and improve fracture risk prediction in older people: A narrative review. Bone. 2023. https://doi.org/10.1016/j.bone.2023.116755.
Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev. 2021. https://doi.org/10.1016/s2666-7568(21)00172-0.
Chen W, Lv H, Liu S, et al. National incidence of traumatic fractures in China: a retrospective survey of 512 187 individuals. Lancet Glob Health. 2017. https://doi.org/10.1016/s2214-109x(17)30222-x.
Armstrong ME, Cairns BJ, Banks E, Green J, Reeves GK, Beral V. Different effects of age, adiposity and physical activity on the risk of ankle, wrist and hip fractures in postmenopausal women. Bone. 2012. https://doi.org/10.1016/j.bone.2012.03.014.
Shen J, Leslie WD, Nielson CM, Majumdar SR, Morin SN, Orwoll ES. Associations of Body Mass Index With Incident Fractures and Hip Structural Parameters in a Large Canadian Cohort. J Clin Endocrinol Metab. 2016. https://doi.org/10.1210/jc.2015-3123.
Søgaard AJ, Holvik K, Omsland TK, et al. Age and Sex Differences in Body Mass Index as a Predictor of Hip Fracture: A NOREPOS Study. Am J Epidemiol. 2016. https://doi.org/10.1093/aje/kww011.
Prieto-Alhambra D, Premaor MO, Fina Avilés F, et al. The association between fracture and obesity is site-dependent: a population-based study in postmenopausal women. J Bone Miner Res. 2012. https://doi.org/10.1002/jbmr.1466.
Kim SH, Yi SW, Yi JJ, Kim YM, Won YJ. Association Between Body Mass Index and the Risk of Hip Fracture by Sex and Age: A Prospective Cohort Study. J Bone Miner Res. 2018. https://doi.org/10.1002/jbmr.3464.
Rikkonen T, Sund R, Sirola J, Honkanen R, Poole KES, Kröger H. Obesity is associated with early hip fracture risk in postmenopausal women: a 25-year follow-up. Osteoporos Int. 2021. https://doi.org/10.1007/s00198-020-05665-w.
Meyer HE, Willett WC, Flint AJ, Feskanich D. Abdominal obesity and hip fracture: results from the Nurses’ Health Study and the Health Professionals Follow-up Study. Osteoporos Int. 2016. https://doi.org/10.1007/s00198-016-3508-8.
Liu HF, Meng DF, Yu P, De JC, Li HY. Obesity and risk of fracture in postmenopausal women: a meta-analysis of cohort studies. Ann Med. 2023. https://doi.org/10.1080/07853890.2023.2203515.
Piñar-Gutierrez A, García-Fontana C, García-Fontana B, Muñoz-Torres M. Obesity and Bone Health: A Complex Relationship. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23158303.
Gkastaris K, Goulis DG, Potoupnis M, Anastasilakis AD, Kapetanos G. Obesity, osteoporosis and bone metabolism. J Musculoskelet Neuronal Interact. 2020;20(3).
Zhu XW, Liu KQ, Yuan CD, et al. General and abdominal obesity operate differently as influencing factors of fracture risk in old adults. iScience. 2022. https://doi.org/10.1016/j.isci.2022.104466.
The State Council Information Office. A press conference on the Report on Nutrition and Chronic Diseases in China (2020).News Office website. 2020. https://www.gov.cn/xinwen/2020-12/24/content_5572983.htm the Report on Nutrition and Chronic Diseases in China (2020).Accessed 17 Jul 2023.
Shen Y, Huang X, Wu J, et al. The Global Burden of Osteoporosis, Low Bone Mass, and Its Related Fracture in 204 Countries and Territories, 1990–2019. Front Endocrinol (Lausanne).2022.https://doi.org/10.3389/fendo.2022.882241.
Yang C, Jia C, Yin S, Mao Z, Cui D. The effect of informal social support on the health of Chinese older adults: a cross-sectional study. BMC Public Health. 2023. https://doi.org/10.1186/s12889-023-15837-y.
Zhang B, Zhai FY, Du SF, Popkin BM. The China Health and Nutrition Survey, 1989–2011. Obes Rev. 2014. https://doi.org/10.1111/obr.12119.
China Health and Nutrition Survey (CHNS) (unc.edu).2015. https://www.cpc.unc.edu/projects/china China Health and Nutrition Survey .Accessed December 17, 2022.
Wang Q, Song X, Du S, et al. Multiple Trajectories of Body Mass Index and Waist Circumference and Their Associations with Hypertension and Blood Pressure in Chinese Adults from 1991 to 2018: A Prospective Study. Nutrients. 2023. https://doi.org/10.3390/nu15030751.
Wang Q, Song X, Du S, et al. Waist circumference trajectories in relation to blood pressure and the risk of hypertension in Chinese adults. Nutrients. 2022. https://doi.org/10.3390/nu14245260.
Binsbergen JJv. WHO Technical Report Series 916. Diet, nutritition and the prevention of chronic diseases. Huisarts En Wetenschap. 2004;386:386–386.
Organization WH. Waist circumference and waist-hip ratio: report of a WHO expert consultation, Geneva, 2008. World Health Organization. 2011.
Yoo EG. Waist-to-height ratio as a screening tool for obesity and cardiometabolic risk. Korean J Pediatr. 2016. https://doi.org/10.3345/kjp.2016.59.11.425.
Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000. https://doi.org/10.1097/00005768-200009001-00009.
Hao L, Jiang H, Zhang B, et al. High diet quality is linked to low risk of abdominal obesity among the elderly women in China. Nutrients. 2022. https://doi.org/10.3390/nu14132623.
D R. Multivariate Imputation for Nonresponse in Surveys. J Wiley & Sons;1987.
Bouxsein ML, Szulc P, Munoz F, Thrall E, Sornay-Rendu E, Delmas PD. Contribution of trochanteric soft tissues to fall force estimates, the factor of risk, and prediction of hip fracture risk. J Bone Miner Res. 2007. https://doi.org/10.1359/jbmr.070309.
Premaor MO, Pilbrow L, Tonkin C, Parker RA, Compston J. Obesity and fractures in postmenopausal women. J Bone Miner Res. 2010. https://doi.org/10.1359/jbmr.091004.
Compston JE, Watts NB, Chapurlat R, et al. Obesity is not protective against fracture in postmenopausal women: GLOW. Am J Med. 2011. https://doi.org/10.1016/j.amjmed.2011.06.013.
Tanaka S, Kuroda T, Saito M, Shiraki M. Overweight/obesity and underweight are both risk factors for osteoporotic fractures at different sites in Japanese postmenopausal women. Osteoporos Int. 2013. https://doi.org/10.1007/s00198-012-2209-1.
Picon-Ruiz M, Morata-Tarifa C, Valle-Goffin JJ, Friedman ER, Slingerland JM. Obesity and adverse breast cancer risk and outcome: Mechanistic insights and strategies for intervention. CA Cancer J Clin. 2017. https://doi.org/10.3322/caac.21405.
Wang LT, Chen LR, Chen KH. Hormone-related and drug-induced osteoporosis: a cellular and molecular overview. Int J Mol Sci. 2023. https://doi.org/10.3390/ijms24065814.
S GRN, J SO, A BD, R ML, Tiedemann A. Does Obesity Increase the Risk and Severity of Falls in People Aged 60 Years and Older? A Systematic Review and Meta-analysis of Observational Studies. J Gerontol A Biol Sci Med Sci. 2020. https://doi.org/10.1093/gerona/glz272.
Karampela I, Sakelliou A, Vallianou N, Christodoulatos GS, Magkos F, Dalamaga M. Vitamin D and obesity: current evidence and controversies. Curr Obes Rep. 2021. https://doi.org/10.1007/s13679-021-00433-1.
Ali D, Tencerova M, Figeac F, Kassem M, Jafari A. The pathophysiology of osteoporosis in obesity and type 2 diabetes in aging women and men: The mechanisms and roles of increased bone marrow adiposity. Front Endocrinol (Lausanne). 2022. https://doi.org/10.3389/fendo.2022.981487.
Ashwell M, Gunn P, Gibson S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: systematic review and meta-analysis. Obes Rev. 2012. https://doi.org/10.1111/j.1467-789X.2011.00952.x.
Amouzegar A, Asgari S, Azizi F, Momenan AA, Bozorgmanesh M, Hadaegh F. The role of metabolic syndrome and its components in incident fracture: A 15-year follow-up among the iranian population. J Clin Endocrinol Metab. 2021. https://doi.org/10.1210/clinem/dgab023.
Aparecida Silveira E, Vaseghi G, de Carvalho Santos AS, et al. Visceral obesity and its shared role in cancer and cardiovascular disease: A scoping review of the pathophysiology and pharmacological treatments. Int J Mol Sci. 2020. https://doi.org/10.3390/ijms21239042.
Wu Y, Yang Y, Wang L, et al. Effect of Bifidobacterium on osteoclasts: TNF-α/NF-κB inflammatory signal pathway-mediated mechanism. Front Endocrinol (Lausanne).2023. https://doi.org/10.3389/fendo.2023.1109296.
Tat SK, Pelletier JP, Ruiz-Velasco C, et al. Influence of Tumor Necrosis Factor α, Parathyroid Hormone, and Vitamin D3 on Modulation of the RANKL2 Isoform: A Pilot Study. Cartilage. 2012. https://doi.org/10.1177/1947603511405837.
Kwan Tat S, Padrines M, Théoleyre S, Heymann D, Fortun Y. IL-6, RANKL, TNF-alpha/IL-1: interrelations in bone resorption pathophysiology. Cytokine Growth Factor Rev. 2004. https://doi.org/10.1016/j.cytogfr.2003.10.005.
Mu L, Liu J, Zhou G, et al. Obesity prevalence and risks among Chinese adults: Findings From the China PEACE Million Persons Project, 2014–2018. Circ Cardiovasc Qual Outcomes. 2021. https://doi.org/10.1161/circoutcomes.120.007292.
Acknowledgements
This research used data from China Health and Nutrition Survey. We are grateful to research grant funding from the National Institute for Health (NIH), the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) for R01 HD30880 and R01 HD38700, National Institute on Aging (NIA) for R01 AG065357, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) for R01 DK104371 and P30 DK056350, National Heart, Lung, and Blood Institute (NHLBI) for R01 HL108427, the NIH Fogarty grant D43 TW009077, the Carolina Population Center for P2C HD050924 and P30 AG066615 since 1989, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Center at Shanghai since 2009, and Beijing Municipal Center for Disease Prevention and Control since 2011. We thank the National Institute for Nutrition and Health, China Center for Disease Control and Prevention, Beijing Municipal Center for Disease Control and Prevention, and the Chinese National Human Genome Center at Shanghai.
Funding
This study was funded by the Sichuan Province Science and Technology Support Program (2022YFS0634-C2), Luzhou Science and Technology Bureau (2022-SYF-33), Program of Southwest Medical University (2022ZD015).
Author information
Authors and Affiliations
Contributions
LH, YYL and LGW conceived the study. LH and LGW prepared the data of this study. LH and XQY performed the statistical analyses for the study. LH drafted the manuscript. YYL, XQY, CB, WR revised the manuscript. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The CHNS was approved by the Institutional Review Board at the University of North Carolina at Chapel Hill and the National Institution for Nutrition and Food Safety, China Center for Disease Control and Prevention. All participants provided signed informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, H., Xu, Q., Ye, Y. et al. Association between obesity and fracture risk in Chinese women above 50 years of age: a prospective cohort study. BMC Public Health 24, 28 (2024). https://doi.org/10.1186/s12889-023-17494-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17494-7