Abstract
Objective
Early onset of adiposity rebound (AR) is considered an early indicator of obesity risk. Our objective was to investigate the association of birth outcomes and early physical growth patterns with early AR in children.
Methods
Study subjects (n = 2705) were enrolled from the Ma’anshan birth cohort (MABC). The body mass index (BMI), head circumference, waist circumference, and body fat were collected. Rapid weight gain (RWG) was defined by the change in weight standard-deviation score in the first two years of life. Group-based trajectory modeling (GBTM) was used to determine children’s physical growth trajectories. The age of AR was fitted using fractional polynomial function models.
Results
Children with very high BMI trajectories (RR = 2.83; 95% CI 2.33 to 1.40), rising BMI trajectories (RR = 3.15; 95% CI 2.66 to 3.72), high waist circumference trajectories (RR = 4.17; 95% CI 3.43 to 5.06), and high body fat trajectories (RR = 3.01; 95% CI 2.62 to 3.46) before 72 months of age were at a greater risk of experiencing early AR. Low birth weight (LBW) (RR = 1.86; 95% CI 1.28 to 2.51), preterm birth (PTB) (RR = 1.50; 95% CI 1.17 to 1.93), and small for gestational age (SGA) (RR = 1.37; 95% CI 1.14 to 1.64) associated with increased risk of early AR. Moreover, infants experiencing RWG (RR = 1.59; 95% CI 1.40 to 1.83), low BMI trajectories (RR = 1.27; 95% CI 1.06 to 1.53) and rising BMI trajectories (RR = 1.50; 95% CI 1.22 to 1.84) in the first two years were at higher risk of developing early AR subsequently. Compared to the group with non-early AR, the BMI of children with early AR tended to be lower first (from birth to 6 months of age) and then higher (from 18 to 72 months of age).
Conclusions
Children with overall high BMI, high waist circumference, and high body fat before 72 months of age are more likely to experience early AR, but infants with low BMI trajectories, rising BMI trajectories and infants experiencing RWG in the first two years of life similarly increase the risk of early AR. These results can help to understand the early factors and processes that lead to metabolic risks.
Similar content being viewed by others
Introduction
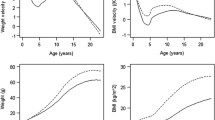
The body mass index (BMI) pattern in humans during childhood presents an interesting phenomenon. The first peak value occurs around the first year after birth, followed by a period of decline until the onset of adiposity rebound (AR), and then the BMI slowly increases again [1]. AR was first reported in 1984 by Rolland-Cachera et al. [1], who identified the timing of AR as an early physiological predictor of obesity in late childhood and adulthood. Studies have confirmed that early age at AR is associated with an increased risk of diabetes [2], cardiometabolic disease [3], and other obesity-related comorbidities [4]. A recent systematic review reported that the overall prevalence of early AR (age at AR < 5.0-5.1 years) is 40%, and it is continuously increasing, with a particularly high overall prevalence of 52% in children born in 2002–2009 [5].
AR is an important physiological milestone during the early stages of physical growth. Exploring AR with changes in physical development in children will lead to an understanding of the early factors and processes that contribute to metabolic risk. Despite the widespread interest in the long-term health effects of age at AR, there is limited understanding of the causes of earlier age at AR. Bhargava et al. [6] found that children with the earlier AR had a higher BMI in late childhood and persisted into adulthood while having the lowest BMI at birth and at 2 years of age. Furthermore, they found a slight increase in BMI from birth to two years of age in individuals [6]. Rolland and Cole [7] also reported that the BMI trajectory of individuals with early age at adiposity rebound (EAR) was characterized by average or low levels of BMI before or after rebound and a rapid increase in gain in BMI after rebound. However, Koyama et al. [8] revealed no association between body weight gain during infancy and the timing of AR. Furthermore, there is inconsistency in the understanding of adverse birth outcomes in relation to the onser of AR. Results from limited cohort studies suggest an earlier age of AR in children with small for gestational age (SGA) compared with non-SGA [9, 10]. It has also been proposed that the higher the birth weight, the earlier the age of AR onset [11]; children with large for gestational age (LGA) are more likely to develop early AR than those with appropriate for gestational age (AGA) [12]. Eriksson et al. [13] observed that early AR was not associated with BMI, birthweight at birth.
There is not enough clarity about the association between early childhood physical growth patterns and early AR. High-density repeated measures of physical growth based on infancy and preschool years may help to further deepen the comparison of early physical growth patterns in children with different AR ages. In addition. existing studies have mostly focused on BMI, and it is not clear whether other physical indicators of the human body, such as head circumference, body fat and body weight, are similarly associated with AR.
Therefore, the present study aimed to investigate the relationship of birth outcomes and early growth patterns with age at AR based on a cohort study in China.
Methods
Study population
Participants (n = 3474) in this study were from the Ma’anshan Birth Cohort Study (MABC), an ongoing longitudinal prospective birth cohort study in Ma’anshan City, Anhui Province, China. Women (age > 18 years and gestational age < 14 weeks) who planned to undergo prenatal and childbirth follow-up visits at the Maternal and Child Health Center in Ma’anshan City were recruited from May 2013 to September 2014. The detailed inclusion criteria were described in our previous study [14]. Additional exclusion criteria for this study were as follows: (1) adverse pregnancy outcomes (embryo arrest, spontaneous abortion, therapeutic abortion, stillbirth, and ectopic pregnancy) (n = 162) and multiple pregnancies (n = 39); (2) children with missing information on birth weight or gestational age (n = 14); (3) children whose BMI was recorded less than six times from birth to six years of age (n = 554) (that is less than twice from 0 to 9 months; less than twice from 12 to 36 months and less than twice from 42 to 72 months). Finally, 2705 pairs of mother–child were included in the study. The recruitment of participants is shown in Fig. 1.
The study procedure was approved by the Ethics and Research Committee of Anhui Medical University (No. 20,131,195). All participants provided their informed consent in writing.
Birth outcomes
The characteristics of the newborn, including the sex of the infant, gestational age, birth length and birth weight, were obtained from medical records. Based on gestational age and birth weight, infants were classified into preterm birth (PTB), non-PTB, SGA, AGA, LGA, low birth weight (LBW), adequate birth weight (ABW) and high birth weight (HBW). PTB and non-PTB were defined as the birth of infants ≤ 37 weeks and > 37 weeks of gestation, respectively [15]. SGA, AGA, and LGA were defined as infants whose birth weight was below the 10th percentile, between the 10th -90th percentile, and above the 90th percentile of infants of the same gestational age and sex, respectively [16]. LBW, ABW, and HBW were defined as newborn birth weights < 2500 g, 2500–3999 g, and ≥ 4000 g at birth, respectively [17].
Early physical growth
The physical growth of the children was repeatedly evaluated from birth to 6 years of age. Five follow-up visits were made in the first year, i.e., at 42 days, 3 months, 6 months, 9 months, and 12 months, after delivery. Subsequently, the children underwent anthropometric measurements every six months until 6 years of age. Anthropometric measurements were performed by pediatricians at Ma’anshan Maternal and Child Health Hospital.
The height and weight were measured at 16 follow-up visits from birth to 72 months. The body weight of the infants was measured with a pan-type lever scale of 0.01 kg; and the weight of the toddlers was measured with a seated lever scale of 0.05 kg. The length of the infant was evaluated with a standard measuring bed, accurate to 0.1 cm; and height and weight in children aged 3 to 6 years were measured with a mechanical height and weight scale (model: RRZ-50-RP), accurate to 0.1 kg for weight and 0.1 cm for height, respectively. During the measurements, children were asked to remove their shoes and hats and wear light clothing. The BMI was calculated using the following formula: BMI = weight (kg)/height (m2).
The children’s head circumference was measured at birth and at 42 days, then at 3, 6, 9, 12, 18, and 24 months after delivery. It was measured by trained pediatricians using a non-stretchable tape around the maximum diameter of the forehead and occiput, accurate to 0.1 cm. Waist circumference was measured at 30, 36, 42, 48, 54, 60, 66, and 72 months of age. The children were asked to remain standing, with the abdomen relaxed, and a soft measuring tape was placed 1 cm above the umbilicus of the child, with an accuracy of 0.1 cm. Body fat was evaluated at 48, 54, 60, 66, and 72 months of age and was measured using an InBody J20 body composition analyzer. The test requires the child to cooperate and remain stationary for 1–2 min to obtain the body fat content.
Weight-for-age z-score (WAZ), BMI-for-age z-score (BMIZ), and head circumference -for-age z-score were determined and classified using the World Health Organization (WHO) child growth standards and growth reference data [18].
Early growth patterns
Rapid weight gain
Weight gain of the children was determined by the difference in WAZ between birth and 12, 18, and 24 months (∆z-scores = z-scores larger months - z-scores smaller months). We defined the criteria for RWG in childhood as a change in the SD score > + 0.67 from birth to 12, 18, and 24 months, which is the most frequent and widely accepted definition of RWG [19]. Early childhood weight gain was classified as RWG (∆z-scores > 0.67) and non-RWG (∆z-scores ≤ 0.67).
Estimation of the trajectory of physical development
Previous studies have suggested that multiple approaches such as longitudinal mixed-effects and latent growth curve models were used to explore BMI trajectories in childhood, but these methods allow for individual variability and assume that individuals belong to the same underlying population [20, 21]. Group-based trajectory modeling (GBTM) assumes no individual variation in trajectories within groups and describes underlying subgroups or classes within a population based on different trajectories [22].
We used GBTM to fit children’s BMI trajectories (from birth to 24 months and from birth to 72 months of age), head circumference trajectories (from birth to 24 months of age), waist circumference trajectories (from 30 months to 72 months of age), and body fat trajectories (from 48 months to 72 months of age). Children with at least three age-specific physical measurements were allowed to examine quadratic trajectory models. The BMI and head circumference z-scores were used, and raw data on waist circumference and body fat were used to fit the respective trajectories. Latent trajectory patterns of physical growth were identified using GBTM applied to longitudinal data.
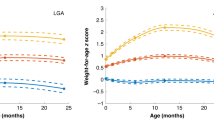
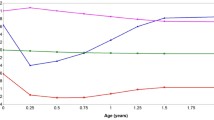
The maximum likelihood method was adopted for parameter estimation and model fitting. First, by combining existing studies on children’s physical growth trajectories [20], we explored two to six latent classes of trajectory models. Next, we tested statistical significance from the perspective of cubic, quadratic, and linear degrees (that is, from high to low, respectively). If the high degree was not significant, a lower degree was tested. Based on the recommendations of previous studies [22, 23], the detailed selection criteria for the best-fit trajectory model were as follows: (1) Bayesian information criteria (BIC), i.e., the closer the BIC values are to 0, the better the fit of the model; (2) the value of entropy indicated how well the classification distinguished from one group to another; (3) an average posterior probability greater than 0.7; and (4) each trajectory contained at least 5% of participants. Table S1 shows the results of the estimation of the trajectory parameters using GBTM. Finally, five different BMI growth trajectories were determined from birth to 24 months: a low BMI trajectory (14.6%), a rising BMI trajectory (8.3%), a medium BMI trajectory (35.2%), a high BMI trajectory (32.0%), and a very high BMI trajectory (9.9%) (Fig. 2). From birth to 72 months of age, five BMI trajectories were also determined: low (20.9%), rising (8.9%), medium (43.7%), high (20.1%), and very high (6.4%) (Fig. 3A). For head circumference, we identified three trajectories: a low trajectory (26.9%), a medium trajectory (52.7%), and a high trajectory (20.4%) (Fig. 3B). As for waist circumference, we identified three trajectories: a normal trajectory (53.9%), a high trajectory (38.8%), and a very high trajectory (7.3%)] (Fig. 3C). We also identified two body fat trajectories: a normal trajectory (85.5%) and a high trajectory (14.5%) (Fig. 3D).
Early childhood physical growth trajectories (A, BMI trajectories of children from birth to 72 months of age; B, Head circumference trajectories of children from birth to 24 months of age; C, waist circumference trajectories of children from 30 to 72 months of age; D, body fat trajectories of children from 48 to 72 months of age)
Estimation of AR
Age at AR was defined as the last minimum (nadir) BMI before a sustained increase in BMI, usually occurring at 4–6 years of age [1]. The average number of BMI follow-ups for the included children (n = 2705) from birth to 6 years of age was 13.7 (interquartile range 13–15). Based on the requirement for more data points near the turning points and during periods of rapid change, we set these age intervals and the corresponding minimum numbers of visits [11, 24]. The number of follow-ups in this study was large (16 times in total); in particular, the number of follow-ups in the first year of life was up to five times, which ensured the accuracy of the model fitting. Furthermore, another study by our team obtained a similar median age in AR (4.38 years old) and the prevalence of early AR (39.3%) based on different inclusion criteria (number of BMI measurements > 8) [25]. Given the high number of repeated BMI measurements in this study, to obtain an accurate age in AR, we used the method recommended by Wen et al. [11] to fit the overall BMI trajectory. The fractional polynomial method (using diverse combinations of age terms—Agepj; powers pj were selected from a fixed set of eight candidate values, including–2, − 1, − 0.5, or log 0.5, 1, 2, and 3) to simulate children’s BMI trajectory as a function of age. The detailed methodology is described in our previous study [26].
We fit the BMI trajectory using a mixed effects model that specified the fixed effects for each fractional polynomial term, which reflected the trend of the population mean and random effects for each term for each child and modeled each child’s deviation from the population mean. We selected the optimal mean and residual variance-covariance structures before model selection based on the Bayesian information criterion (BIC).
We selected the best combination of age (−2), age (−1), age (−0.5), log (age), and age 0.5 by comparing different combinations of fractional polynomial functions that could effectively reflect the BMI trajectory in children 0–6 years of age. From the model, we derived the age at AR for each child and defined children with AR < 48 months as early AR.
Covariates
We relied on a review of the literature and a directed acyclic graph (DAG) to identify possible confounders, including maternal age [27], family monthly income per capita (< 2500 RMB; 2500–4000 RMB; >4000 RMB) [28], parental education level (junior high school or below; senior middle school; junior college; bachelor’s degree or above) [29], maternal pre-pregnancy BMI [30], paternal BMI [31], parity (multipara; nulliparous) [32], maternal metabolic dysfunctions (yes; no) [33], alcohol use (yes; no) [34], tobacco use (yes; no) [35], maternal iron supplementation (yes; no) [36], maternal folic acid supplementation (yes; no) [37] during pregnancy, and sex of children (male; female) [38] (Figure S1).
Data on maternal age, parental educational level, family income, parity, paternal BMI, alcohol use, tobacco use, iron supplementation, and folic acid supplementation during pregnancy were collected using a questionnaire survey. Maternal weight was measured during recruitment and considered before pregnancy. Information on maternal metabolic dysfunction and parity was extracted from medical notes. Maternal metabolic dysfunction included gestational diabetes and hypertensive disorders during pregnancy, and women with at least one dysfunction were defined as having maternal metabolic dysfunction. Information on alcohol and tobacco use during pregnancy was obtained from maternal and child health records. Furthermore, the data on exclusive breastfeeding for the first 6 months (yes, no), primary caregivers before 3 years (parents; grandparents), screen time (≤ 1 h/day; >1 h/day), and outdoor activity time (≤ 1 h/day; >1 h/day) were reported by the children’s caregivers in the follow-up questionnaire survey. These variables were collected as precision variables for sensitivity analysis.
Statistical analysis
SPSS (IBM, version 23.0) was used for the statistical analyses. A P-value < 0.05 was considered statistically significant. STATA 15.0 was used to fit physical growth trajectories and to estimate children’s AR.
The normality of age-specific distributions of the physical growth data was examined using Q-Q plots and the Kolmogorov-Smirnov test. This showed that BMI, head circumference, waist circumference, and body fat were normally distributed at all age points.
The χ2 tests and t tests were adopted to evaluate the basic demographic differences between the included and excluded population and the differences in physical values for each exam point between the early AR and non-early AR groups. Poisson regression models (parameter estimation using robust standard errors) were used to examine the association of birth outcomes and early growth patterns (RWG, BMI trajectory, head circumference trajectory, waist circumference trajectory, and body fat trajectory) with early AR. All the above analyses were performed in the crude model (model 1) and the model adjusted for confounders (model 2).
Multiple imputations were used to interpolate missing data from confounders to increase statistical power and validate the study conclusions, and twenty sets of interpolations were created. According to Rubin’s Law [39], the effects were aggregated to obtain new results.
To examine the stability of the results, we performed three sensitivity analyses. Breastfeeding affects physical development in children [40], and other factors in early childhood such as outdoor activity time [41], the main caregiver before 3 years old [42] and screen time [43]) were also strongly associated with early childhood physical development. These variables may be mediating/moderating variables and it is important to do as the sensitivity analysis rather than the main analysis. Therefore, we first further adjusted for exclusive breastfeeding in the first six months based on model 2. Second, we further adjusted for these important covariates (outdoor activity time, main caregiver and screen time) based on model 2. Furthermore, considering that we used the BMI z-score for trajectory fitting, we further used the raw BMI values for trajectory fitting to compare the consistency of the association with the early AR (Figure S4).
Results
Basic characteristics of participants
The characteristics of the participants are listed in Table 1. The average maternal age was 26.5 (3.6) years, and the average maternal BMI before pregnancy was 20.9 (2.9) kg/m2. Most women were primiparas (90.8%), nonsmokers (99.8%), nonalcohol consumers (92.0%), and had no pregnancy-related complications (82.8%). Among the children, 264 (9.8%) were SGA, 60 (2.2%) had LBW, and 111 (4.1%) were PTB (Table S2). The proportion of children with RWG from birth to 12 months of age, 18 months of age, and 24 months of age was 45.2%, 37.8%, and 37.9%, respectively. The parents of the included children had a higher educational level, and mothers were more likely to be primiparous and have slightly higher gestational weeks.
Figure S2 shows an overall plot of the BMI trajectory. Among the included children, 39.9% had AR before the age of 48 months and 16.0% after 72 months (Table S2). The estimated median age in AR was 52 months (4 years and 4 months).
Children with early AR were found to have lower levels of parental education compared to children without early AR. Additionally, mothers of children with early AR had higher rates of pregnancy complications, and these mothers had lower rates of taking folic acid supplements during pregnancy. Furthermore, children with early AR had smaller physical measurements at birth, including weight, length, BMI, and head circumference (Table S3).
Birth outcomes and AR
Table 2 shows the relationship between birth outcomes and early AR. Children with PTB (vs. non-PTB) (RR = 1.50; 95% CI 1.17 to 1.93), SGA (vs. AGA) (RR = 1.37; 95% CI 1.14 to 1.64), and LBW (vs. ABW) (RR = 1.86; 95% CI 1.28 to 2.51) had increased risk of early AR. Furthermore, children with LGA children (vs. AGA) (RR = 0.79; 95% CI 0.66 to 0.94) and HBW (vs. ABW) (RR = 0.65; 95% CI 0.50 to 0.85) had a lower risk of early AR.
Early growth patterns and AR
RWG and AR
As shown in Table 3, RWG (from birth to 12 months of age [RR = 1.21; 95% CI 1.07 to 1.37]); from birth to 18 months of age (RR = 1.48; 95% CI 1.30 to 1.67); from birth to 24 months of age (RR = 1.59; 95% CI 1.40 to 1.81]) was significantly associated with an increased risk of early AR in children.
BMI trajectory and AR
Compared to non-EAR, the BMI of children with early AR tended to be initially lower (from birth to 6 months) and then higher (from 18 to 72 months). In particular, from the age of 18 months (mean difference = 0.3 kg/m2) to the age of 72 months (mean difference = 1.6 kg/m2), the difference in mean BMI between children with early AR and non-early AR showed a gradual increase (Figure S3). The detailed data are shown in Table S4.
For the BMI trajectory from birth to 24 months of age, we found that a significantly higher proportion of early AR occurred between the low BMI trajectory (44.7%) and the increasing BMI trajectory (56.0%) compared to the medium BMI trajectory (36.8%). For the BMI trajectory of children from birth to 72 months of age, we found that a significantly higher proportion of early AR occurred on the increasing BMI trajectory (99.6%) and the high BMI trajectory (90.8%) than in the medium BMI trajectory (30.2%) (Table S5).
After adjusted the confounders, it was observed that children with a low BMI trajectory (RR = 1.27; 95% CI 1.06 to 1.53) and a rising BMI trajectory (RR = 1.50; 95% CI 1.22 to 1.84) in the first two years of life had a higher risk of early AR than those with a medium-level trajectory (Table 3). Children with a very high BMI trajectory (RR = 2.83; 95% CI 2.33 to 3.43) and a rising BMI trajectory (RR = 3.15; 95% CI 2.66 to 3.72) from birth to 72 months of age both increased the risk of early AR (Table 4).
Head circumference trajectory and AR
Compared to children with non-EAR, children with early AR had a lower trajectory of head circumference from birth to 9 months of age, a similar trajectory of head circumference from 12 to 18 months of age, and finally a higher trajectory of head circumference at 24 months of age (Figure S3). The detailed data are shown in Table S4.
Despite subtle differences in head circumference between children with early AR and children with non-early AR, we did not find a significant association between head circumference trajectories and early AR in the logistic regression (Table 3).
Body fat trajectory and AR
In children aged 48 to 72 months, mean body fat values were significantly higher in the early AR group than in the non-early AR group (Figure. S3). The detailed data are shown in Table S4. A significantly higher proportion of early AR was observed in children with a high body fat trajectory (79.9%) than in those with a normal body fat trajectory (25.0%) (Table S5).
After adjusted the confounders, we found that children with a high body fat trajectory was associated with an elevated risk of early AR (RR = 3.01; 95% CI 2.62 to 3.46) (Table 4).
Waist circumference trajectory and AR
In children aged 30 to 72 months, mean waist circumference values were significantly higher in the early AR group than in the non- early AR group (Figure. S3). The detailed data are shown in Table S4 A significantly higher proportion of early AR was observed in the high- waist circumference trajectory (55.2%) and very high waist circumference trajectory (95.9%) than in the normal waist circumference trajectory (21.4%) (Table S5).
After adjusted the confounders, we found that children with a high body fat trajectory (RR = 2.52; 95% CI 2.19 to 2.90) and very high body fat trajectory (RR = 4.17; 95% CI 3.43 to 5.06) were associated with an elevated risk of early AR (Table 4).
Sensitivity analyses
The sensitivity analyses did not fundamentally change the main results (Tables S6 to S9).
Discussion
We comprehensively assessed the association of early childhood physical growth trajectories, particularly growth patterns in the first two years of life, with early AR. Our findings support a positive association of overall very high BMI, high waist circumference and high body fat trajectories in early childhood with a higher risk of early AR in childhood. Moreover, the pattern of physical growth in the first two years of a child’s life showed a particular association with early AR. In detailed, children born to PTB, SGA and LBW had a higher risk of early AR; children with RWG, rising BMI trajectory and low BMI trajectory from birth to 24 months all related to an increased risk of early AR.
We found that a high BMI trajectory from birth to 72 months was significantly associated with early AR in children. These findings were consistent with the current main findings that children at a younger age at AR have a higher BMI and are at higher risk of being overweight and obesity [5, 44]. We also found that a high waist circumference trajectory and body fat trajectory were significantly associated with early AR, especially in children with very high waist circumference and body fat trajectories, with early AR rates of up to 95.6% and 96.8%, respectively. This suggests that the strong association between the early onset of AR and high BMI may be related to the fat mass index (FMI). It is worth noting that the BMI trajectory of children birth to 24 months of age showed a unique association with early AR. Children with a low BMI trajectory and an increasing BMI trajectory in the first two years of life had a higher risk of experiencing early AR than those with a medium BMI trajectory. Children with a low BMI trajectory are more likely to experience RWG after birth, but they also had difficulties fully catching up to the level of normal children, and thus there may remain a low trajectory in their first year [45]. Two previous studies also indirectly supported our findings that children with early AR had a low BMI before AR [6, 7]. Furthermore, we compared the BMI levels of children with early AR and non-early AR at each age and found that children with early AR had a lower BMI from birth to 6 months, but a higher BMI from 18 to 72 months. The two categories of BMI trajectories (low trajectory and rising trajectory) were associated with early AR; however, the possible metabolic risk later needs to be considered in the context of changes in body composition. BMI includes both the components of FMI and lean mass index (LML), while the appearance of AR (the second rise in adiposity) corresponds to the beginning of an increase in the number of fat cells after an early phase of increasing and then decreasing in size [46], which represents an overall cessation of the decline in FMI [47]. Rolland-Cachera et al. [48] proposed two main growth trajectories associated with adult obesity: a high BMI for all ages, reflecting both high lean body mass and high-fat body mass, and a low or normal BMI, followed by an early AR reflecting increased fat mass rather than lean body mass. Early rapid growth patterns can be detrimental if they correspond to catch-up growth, but they can also correspond to a more favorable outcome if they correspond to increased LML. Rapid increases in BMI before the age of 2 years have been shown to increase LML in adults without excess fat accumulation, while rapid increases in BMI in late childhood result in relatively large increases in fat mass despite a concomitant increase in LML [49].
The mean age at AR was earlier for the children in current study. The proportions of early AR (age at AR < 48 months) and AR < 5 years were 39.9% and 66.9%, respectively. This phenomenon is not surprising, as there is a general trend toward an earlier age for AR in children [5]. The Korean National Health Information Database (2008–2015), also located in East Asia, found that the median time point for AR was 45 months and the proportion of patients with AR before 4.75 years was as high as 79.6% [50]. Because of the differences in physical development of children in different countries and regions, there are currently no uniform standards for early AR. Consequently, most of the criteria for Rolland-Cachera et al. [1] were adopted, as he was the first to propose the concept of AR. Our group’s systematic review of all published AR-related studies found that the overall prevalence of early AR according to Rolland-Cachera et al.’s definition is 40% [5]. Combined with the age cutoff value of the first 40% of children in this study, this is almost consistent with 48 months of age as a criterion for defining early AR. This criterion has also been used in other studies [10, 25].
Our results indicated that children born to PTB, SGA and LBW all associated with early AR. Researchers in the EDEN cohort found that the risk of early AR was higher in children with SGA than in children with AGA, but no differences in early AR were found between children with LGA and AGA or between children with PBT and non-PTB [9]. Baldassarre et al. [51], based on a small cohort study of preterm infants, found that PTB was an independent risk factor for late AR. This difference may be due to different definitions of early AR and different study populations. The study by Baldassarre et al. [9] was limited to premature infants and early AR was defined as being in the lowest quintile of age in AR in the EDEN cohort, which could have contributed to the observed differences. Numerous population-based observational studies have shown that children with SGA, LBW, and PTB undergo rapid growth in early childhood [52,53,54]. Our study found that children with RWG in the first two years were more likely to experience early AR. The phenomenon of AR is that the BMI starts to increase, whereas the essence is that the fat mass index (FMI) stops declining [47]. Studies have found that infants with RWG between birth and 2 years of age have higher FMI at 2 years of age than those without RWG [55]. Focusing on trends in both BMI and FMI may provide further insight into early childhood physical development. The RWG and early AR are associated with later obesity and metabolic risk, suggesting the importance of focusing on early physical growth patterns to prevent and control long-term obesity. A study by Koyama et al. [8] found no association between early weight gain and the timing of AR, possibly because this study did not use a definition of sustained early RWG (from birth to 12 months or 24 months) but instead adopted increments every four months of weight gain (from birth to 4 months, 4–8 months, and 8–12 months), which can underestimate the association between RWG and early AR.
In this study, the GBTM was used to fit trajectories to children’s repeated measures of physical indicators. Existing studies have demonstrated that both GBTM and growth mixture modelling are suitable for modeling trajectories [56], and although both methods have different approaches to longitudinal noble modeling, studies have observed strong agreement on the optimal number of trajectories su and have recommended the use of GBTM because it is less computationally intensive [57]. The strengths of GBTM for fitting somatic growth indicators have been reported and adopted in a number of studies, primarily because it allows researchers to identify and characterize potential subgroups or categories within populations based on different trajectories [22].
The age of AR in children is getting younger and upstream factors such as prenatal or early life factors may be important contributors to its variability. Existing studies suggest that limited maternal education, low socioeconomic status, increased maternal BMI, gestational diabetes, and increased caloric intake are significant predictors of early AR [9, 58,59,60]. Previous studies by our group have also found that maternal pre-pregnancy BMI and gestational diabetes have independent and combined effects on the timing of early AR [25], and elective cesarean section increases the risk of early AR in girls [26]. There are fewer other studies from Chinese birth/children cohorts, and only one longitudinal study from Shanghai reported that older mothers, shorter duration of breastfeeding, and SGA were associated with a higher risk of developing early AR [10]. Some studies have shown that increasing the duration of breastfeeding, rationalizing protein intake, and reducing processed and processed foods are possible diet interventions that delay the early onset of AR [61, 62].
It needs to be recognized that both parents of the included children had a higher educational level, with mothers having higher rates of iron supplementation and folic acid supplementation during pregnancy as well as longer gestational weeks compared to the non-included children. Thus, potential selection bias may exist. Compared with children who did not have early AR, children with early AR had both parents with lower educational levels, a higher proportion of mothers with pregnancy complications during pregnancy, a lower proportion of mothers with folic acid supplementation during pregnancy, and smaller physical measures at birth including weight, length, BMI, and head circumference. Although we controlled for multiple important confounders during pregnancy and at birth, the above differences also suggest that factors affecting maternal pregnancy complications and birth outcomes may be important residual confounders.
This study has several strengths. This is a prospective birth cohort study to explore the relationship between early growth trajectories and the timing of AR, and all information on exposure, outcome and potential confounders was collected prospectively. Second, the high frequency of anthropometric measurements, with up to 16 repetitions of BMI measurements from birth to 6 years, provided a realistic prediction of age at AR. Third, we considered other postnatal factors affecting a child’s physical development, such as breastfeeding, primary caregivers, and screen time and outdoor activities time. These factors are not confounders between exposure and outcome but are important precision variables. The inclusion of these variables is expected to improve the precision of our findings.
Several limitations need to be acknowledged. First, we only have follow-up data for children up to age six years. According to the model, 13.2% of children did not undergo AR. Longer follow-up periods are required to determine the age of AR in these children. Second, although we collected information prospectively, we could not avoid some recall/reporting biases, such as maternal smoking, outdoor activity time, and exclusive breastfeeding. However, the use of repeated data collection in this cohort largely reduced the unreliability of reporting. Third, there are some drivers in early childhood that may influence physical development have not been collected, such as in-home nurturance, child feeding, diet, and sleep quality, stimulation, and some family and school environment factors. Therefore, we cannot further explore the potential modifying effects of these important early childhood covariates. Fourth, smaller numbers of low and high birth weights may increase the probability that the association is a false positive. However, the associations of SGA and LGA with outcome showed consistent direction and close association strength, which suggests the reliability of our findings regarding HBW and LBW with outcome.
Conclusions
This study showed that children with high BMI, waist circumference, and body fat trajectories in early childhood had a high prevalence of early AR. Infants born to SGA, LBW and PTB were at higher risk for early AR. Furthermore, children with a low head circumference trajectory, low BMI trajectory, rising BMI trajectory, and RWG in the first two years of life were associated with an increased risk of early AR. The effect of early life physical developmental indicators, especially BMI, on early AR appears to be in different directions of association before and after 12 months of age. These results can help to understand the early factors and processes that lead to metabolic risks.
Data Availability
Because this data was derived from the Ma’anshan birth cohort, the datasets generated and/or analyzed in the current study are not publicly available, but are available from the corresponding authors upon reasonable request.
Abbreviations
- AR:
-
adiposity rebound
- BMI:
-
body mass index
- RWG:
-
rapid weight gain
- GBTM:
-
group-based trajectory modeling
- SGA:
-
small for gestational age
- PTB:
-
preterm birth
- LBW:
-
low birth weight
- WAZ:
-
Weight-for-age z-score
- BMIZ:
-
BMI-for-age z-score
- WHO:
-
World Health Organization
- BIC:
-
Bayesian information criterion
- DAG:
-
directed acyclic graph
- MABC:
-
Ma’anshan Birth Cohort Study
References
Rolland-Cachera MF, Deheeger M, Bellisle F, Sempé M, Guilloud-Bataille M, Patois E. Adiposity rebound in children: a simple indicator for predicting obesity. Am J Clin Nutr. 1984;39(1):129–35.
Wadsworth M, Butterworth S, Marmot M, Ecob R, Hardy R. Early growth and type 2 Diabetes: evidence from the 1946 British birth cohort. Diabetologia. 2005;48(12):2505–10.
Fonseca MJ, Moreira C, Santos AC. Adiposity rebound and cardiometabolic health in childhood: results from the Generation XXI birth cohort. Int J Epidemiol. 2021;50(4):1260–71.
Koivuaho E, Laru J, Ojaniemi M, Puukka K, Kettunen J, Tapanainen JS, Franks S, Järvelin MR, Morin-Papunen L, Sebert S et al. Age at adiposity rebound in childhood is associated with PCOS diagnosis and obesity in adulthood-longitudinal analysis of BMI data from birth to age 46 in cases of PCOS. International journal of obesity (2005) 2019, 43(7):1370–1379.
Zhou J, Zhang F, Qin X, Li P, Teng Y, Zhang S, Tao F, Huang K. Age at adiposity rebound and the relevance for obesity: a systematic review and meta-analysis. Int J Obes. 2022;46(8):1413–24.
Bhargava SK, Sachdev HS, Fall CH, Osmond C, Lakshmy R, Barker DJ, Biswas SK, Ramji S, Prabhakaran D, Reddy KS. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med. 2004;350(9):865–75.
Rolland-Cachera MF, Cole TJ. Does the age at adiposity rebound reflect a critical period? Pediatr Obes 2019, 14(1).
Koyama S, Sairenchi T, Shimura N, Arisaka O. Association between timing of adiposity rebound and body weight gain during infancy. J Pediatr. 2015;166(2):309–12.
Cissé AH, Lioret S, de Lauzon-Guillain B, Forhan A, Ong KK, Charles MA, Heude B. Association between perinatal factors, genetic susceptibility to obesity and age at adiposity rebound in children of the EDEN mother-child cohort. Int J Obes. 2021;45(8):1802–10.
Lin D, Chen D, Huang J, Li Y, Wen X, Wang L, Shi H. Pre-birth and early-life factors Associated with the timing of Adiposity Peak and Rebound: a large Population-based longitudinal study. Front Pead. 2021;9:742551.
Wen X, Kleinman K, Gillman MW, Rifas-Shiman SL, Taveras EM. Childhood body mass index trajectories: modeling, characterizing, pairwise correlations and socio-demographic predictors of trajectory characteristics. BMC Med Res Methodol. 2012;12:38.
Wang X, Liang L, Junfen FU, Lizhong DU. Metabolic syndrome in obese children born large for gestational age. Indian J Pediatr. 2007;74(6):561–5.
Eriksson JG, Kajantie E, Lampl M, Osmond C, Barker DJ. Small head circumference at birth and early age at adiposity rebound. Acta Physiologica (Oxford England). 2014;210(1):154–60.
Zhou J, Teng Y, Zhang F, Ru X, Li P, Wang J, Yan S, Zhu P, Tao F, Huang K. Sex-specific association between placental inflammatory cytokine mRNA expression and preschoolers’ behavioral development: the Ma’anshan birth cohort study. Brain Behav Immun. 2022;104:110–21.
Fleischman AR, Oinuma M, Clark SL. Rethinking the definition of term pregnancy. Obstet Gynecol. 2010;116(1):136–9.
Zhu L, Zhang R, Zhang S, Shi W, Yan W, Wang X, Lyu Q, Liu L, Zhou Q, Qiu Q, et al. [Chinese neonatal birth weight curve for different gestational age]. Zhonghua Er Ke Za Zhi. 2015;53(2):97–103.
Stern R, Behrman R, Kliegman R, Jenson H. Nelson’s Textbook of Pediatrics. 2003.
Organization WH. WHO child growth standards: length/height-for-age, weight-for-age, weight-for-length, weight-for-height and body mass index-for-age: methods and development. World Health Organization; 2006.
Zheng M, Lamb KE, Grimes C, Laws R, Bolton K, Ong KK, Campbell K. Rapid weight gain during infancy and subsequent adiposity: a systematic review and meta-analysis of evidence. Obes Reviews: Official J Int Association Study Obes. 2018;19(3):321–32.
Mattsson M, Maher GM, Boland F, Fitzgerald AP, Murray DM, Biesma R. Group-based trajectory modelling for BMI trajectories in childhood: a systematic review. Obes Reviews: Official J Int Association Study Obes. 2019;20(7):998–1015.
Bauer DJ, Reyes HL. Modeling variability in Individual Development: differences of degree or kind? Child Dev Perspect. 2010;4(2):114–22.
Nagin DS. Group-based trajectory modeling: an overview. Ann Nutr Metab. 2014;65(2–3):205–10.
Kim SY. Determining the number of latent classes in single- and multi-phase growth mixture models. Struct Equation Modeling: Multidisciplinary J. 2014;21(2):263–79.
Cole TJ, Freeman JV, Preece MA. British 1990 growth reference centiles for weight, height, body mass index and head circumference fitted by maximum penalized likelihood. Stat Med. 1998;17(4):407–29.
Fan SQ, Yan SQ, Zhu XZ, Li J, Tong CG, Li H, Cao XY, Wu LL, Xie ZL, Wei FB, et al. [Independent and combined effects of pre-pregnancy BMI and gestational Diabetes on early adiposity rebound timing in children]. Zhonghua Liu Xing Bing Xue Za Zhi = Zhonghua Liuxingbingxue Zazhi. 2022;43(10):1626–31.
Zhang S, Zhou J, Yang M, Zhang F, Tao X, Tao F, Huang K. Sex-specific association between elective cesarean section and growth trajectories in preschool children: a prospective birth cohort study. Front Public Health. 2022;10:985851.
Restrepo-Méndez MC, Lawlor DA, Horta BL, Matijasevich A, Santos IS, Menezes AM, Barros FC, Victora CG. The association of maternal age with birthweight and gestational age: a cross-cohort comparison. Paediatr Perinat Epidemiol. 2015;29(1):31–40.
Demment MM, Haas JD, Olson CM. Changes in family income status and the development of overweight and obesity from 2 to 15 years: a longitudinal study. BMC Public Health. 2014;14:417.
Bramsved R, Regber S, Novak D, Mehlig K, Lissner L, Mårild S. Parental education and family income affect birthweight, early longitudinal growth and body mass index development differently. Acta paediatrica (Oslo, Norway: 1992) 2018, 107(11):1946–1952.
Liu P, Xu L, Wang Y, Zhang Y, Du Y, Sun Y, Wang Z. Association between perinatal outcomes and maternal pre-pregnancy body mass index. Obes Reviews: Official J Int Association Study Obes. 2016;17(11):1091–102.
Sørensen T, Ajslev TA, Ängquist L, Morgen CS, Ciuchi IG, Davey Smith G. Comparison of associations of maternal peri-pregnancy and paternal anthropometrics with child anthropometrics from birth through age 7 y assessed in the Danish National Birth Cohort. Am J Clin Nutr. 2016;104(2):389–96.
Lin L, Lu C, Chen W, Li C, Guo VY. Parity and the risks of adverse birth outcomes: a retrospective study among Chinese. BMC Pregnancy Childbirth. 2021;21(1):257.
Grieger JA, Bianco-Miotto T, Grzeskowiak LE, Leemaqz SY, Poston L, McCowan LM, Kenny LC, Myers JE, Walker JJ, Dekker GA, et al. Metabolic syndrome in pregnancy and risk for adverse pregnancy outcomes: a prospective cohort of nulliparous women. PLoS Med. 2018;15(12):e1002710.
Nykjaer C, Alwan NA, Greenwood DC, Simpson NA, Hay AW, White KL, Cade JE. Maternal alcohol intake prior to and during pregnancy and risk of adverse birth outcomes: evidence from a British cohort. J Epidemiol Commun Health. 2014;68(6):542–9.
Di HK, Gan Y, Lu K, Wang C, Zhu Y, Meng X, Xia WQ, Xu MZ, Feng J, Tian QF, et al. Maternal Smoking status during pregnancy and low birth weight in offspring: systematic review and meta-analysis of 55 cohort studies published from 1986 to 2020. World J Pediatrics: WJP. 2022;18(3):176–85.
Tofail F, Persson LA, El Arifeen S, Hamadani JD, Mehrin F, Ridout D, Ekström EC, Huda SN, Grantham-McGregor SM. Effects of prenatal food and micronutrient supplementation on infant development: a randomized trial from the maternal and Infant Nutrition Interventions, Matlab (MINIMat) study. Am J Clin Nutr. 2008;87(3):704–11.
Persson L, Arifeen S, Ekström EC, Rasmussen KM, Frongillo EA, Yunus M. Effects of prenatal micronutrient and early food supplementation on maternal hemoglobin, birth weight, and infant mortality among children in Bangladesh: the MINIMat randomized trial. JAMA. 2012;307(19):2050–9.
Cattaneo A, Monasta L, Stamatakis E, Lioret S, Castetbon K, Frenken F, Manios Y, Moschonis G, Savva S, Zaborskis A, et al. Overweight and obesity in infants and pre-school children in the European Union: a review of existing data. Obes Reviews: Official J Int Association Study Obes. 2010;11(5):389–98.
Toutenburg H, Rubin DB. Multiple imputation for nonresponse in surveys. Stat Pap. 1990;31(1):180–0.
Yan J, Liu L, Zhu Y, Huang G, Wang PP. The association between breastfeeding and childhood obesity: a meta-analysis. BMC Public Health. 2014;14:1267.
Zhang Y, Zhang X, Li J, Zhong H, Pan CW. Associations of outdoor activity and screen time with adiposity: findings from rural Chinese adolescents with relatively low adiposity risks. BMC Public Health. 2020;20(1):1769.
Sata M, Yamagishi K, Sairenchi T, Ikeda A, Irie F, Watanabe H, Iso H, Ota H. Impact of caregiver type for 3-Year-old children on subsequent between-meal eating habits and being overweight from childhood to Adulthood: a 20-Year follow-up of the Ibaraki Children’s cohort (IBACHIL) study. J Epidemiol. 2015;25(9):600–7.
Fang K, Mu M, Liu K, He Y. Screen time and childhood overweight/obesity: a systematic review and meta-analysis. Child Care Health Dev. 2019;45(5):744–53.
Rolland-Cachera MF, Deheeger M, Maillot M, Bellisle F. Early adiposity rebound: causes and consequences for obesity in children and adults. International journal of obesity (2005) 2006, 30 Suppl 4:S11-17.
Olbertz DM, Mumm R, Wittwer-Backofen U, Fricke-Otto S, Pyper A, Otte J, Wabitsch M, Gottmann P, Schwab KO, Scholten M, et al. Identification of growth patterns of preterm and small-for-gestational age children from birth to 4 years - do they catch up? J Perinat Med. 2019;47(4):448–54.
Rolland-Cachera M, Deheeger M, Bellisle F. The adiposity rebound: its contribution to obesity in children and adults. In: NESTLE NUTRITION WORKSHOP SERIES: 2002: Philadelphia; Lippincott-Raven; 1999; 2002: 99–118.
Campbell MW, Williams J, Carlin JB, Wake M. Is the adiposity rebound a rebound in adiposity? Int J Pediatr Obesity: IJPO : Official J Int Association Study Obes. 2011;6(2–2):e207–215.
Rolland-Cachera MF, Péneau S. Growth trajectories associated with adult obesity. World Rev Nutr Diet. 2013;106:127–34.
Ylihärsilä H, Kajantie E, Osmond C, Forsén T, Barker DJ, Eriksson JG. Body mass index during childhood and adult body composition in men and women aged 56–70 y. Am J Clin Nutr. 2008;87(6):1769–75.
Hwang IT, Ju YS, Lee HJ, Shim YS, Jeong HR, Kang MJ. Body mass index trajectories and adiposity rebound during the first 6 years in Korean children: based on the National Health Information Database, 2008–2015. PLoS ONE. 2020;15(10):e0232810.
Baldassarre ME, Di Mauro A, Caroli M, Schettini F, Rizzo V, Panza R, De Giorgi A, Capozza M, Fanelli M, Laforgia N. Premature birth is an Independent risk factor for early adiposity rebound: longitudinal analysis of BMI data from birth to 7 years. Nutrients 2020, 12(12).
Martin A, Connelly A, Bland RM, Reilly JJ. Health impact of catch-up growth in low-birth weight infants: systematic review, evidence appraisal, and meta-analysis. Matern Child Nutr 2017, 13(1).
Cooke RJ. Catch-up growth: implications for the preterm and term infant. Eur J Clin Nutr. 2010;64(Suppl 1):8–s10.
Karlberg J, Albertsson-Wikland K. Growth in full-term small-for-gestational-age infants: from birth to final height. Pediatr Res. 1995;38(5):733–9.
Jain V, Kumar B, Devi S, Jain A, Jana M, Kurpad AV. Body composition from birth to 2 years in term healthy Indian infants measured by deuterium dilution: Effect of being born small for gestational age and early catch-up growth. European journal of clinical nutrition 2022.
van der Nest G, Lima Passos V, Candel M, van Breukelen GJP. An overview of mixture modelling for latent evolutions in longitudinal data: modelling approaches, fit statistics and software. Adv life Course Res. 2020;43:100323.
Dalrymple KV, Vogel C, Godfrey KM, Baird J, Hanson MA, Cooper C, Inskip HM, Crozier SR. Evaluation and interpretation of latent class modelling strategies to characterise dietary trajectories across early life: a longitudinal study from the Southampton women’s Survey. Br J Nutr. 2023;129(11):1945–54.
Ip EH, Marshall SA, Saldana S, Skelton JA, Suerken CK, Arcury TA, Quandt SA. Determinants of Adiposity Rebound timing in children. J Pediatr. 2017;184:151–156e152.
Vollrath ME, Hampson SE, Péneau S, Rolland-Cachera MF, Ystrom E. Child temperament predicts the adiposity rebound. A 9-year prospective sibling control study. PLoS ONE. 2018;13(11):e0207279.
Hakanen T, Saha MT, Salo MK, Nummi T, Harjunmaa U, Lipiäinen L, Vuorela N. Mothers with gestational Diabetes are more likely to give birth to children who experience early weight problems. Acta Paediatr (Oslo Norway: 1992). 2016;105(10):1166–72.
Günther AL, Buyken AE, Kroke A. The influence of habitual protein intake in early childhood on BMI and age at adiposity rebound: results from the DONALD Study. Int J Obes. 2006;30(7):1072–9.
Bergmann KE, Bergmann RL, Von Kries R, Böhm O, Richter R, Dudenhausen JW, Wahn U. Early determinants of childhood overweight and adiposity in a birth cohort study: role of breast-feeding. Int J Obes Relat Metabolic Disorders: J Int Association Study Obes. 2003;27(2):162–72.
Acknowledgements
The authors thank all participants of the Ma’anshan birth cohort and those who contributed to the cohort follow-up efforts, and the Key Laboratory of Population Health Across Life Cycle (AHMU) for providing the birth cohort platform support for this study.
Funding
This work was supported by the National Natural Science Foundation of China (82273639), the National Key Research and Development Program of China (2022YFC2702901), Regional Innovation and Development Joint Fund of the National Natural Science Foundation of China (U22A20361), and Research Fund of Anhui Institute of translational medicine (ZHYX2020A001).
Author information
Authors and Affiliations
Contributions
FBT, HK, and SQY were responsible for the conception and design of the cohort. JXZ, SSZ, YZT, MTY, SQY, FBT, and HK were responsible for the follow-up of the cohort. JXZ and SSZ were responsible for the acquisition and analysis of data. JXZ performed the statistical analyses. All authors took part in drafting the manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
all participants have signed an informed consent form; the study was approved by the ethics committees of Anhui medical university (No. 20131195). We confirm that all methods in this study were performed in accordance with the relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1
: Table S1 Results of group-based trajectory model. Table S2 Age at AR in children with different birth outcomes. Table S3 The basic characteristics of participants with and without early AR. Table S4 Physical growth levels of children in the early AR and non-early AR groups at each age. Table S5 Proportions of EAR and NEAR in children with different physical trajectories. Table S6 Sensitivity analysis on the association between birth outcomes and early AR. Table S7 Sensitivity analysis on the association of RWG, BMI trajectories and head circumference trajectories with early AR. Table S8 Sensitivity analysis on the association between the trajectories of physical growth and early AR in children. Table S9 Associations of BMI trajectories (using raw BMI data) and early AR in children. Figure S1 Directed acyclic graph of the relationship between birth outcome/early growth patterns and age at AR. Figure S2 The overall trajectory plot based on the BMI fit of 2705 children. Figure S3 Physical growth trajectory of children in the early AR (EAR) and non-early AR (NEAR) groups. Figure S4 Trajectories fitted using raw BMI data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhou, J., Teng, Y., Zhang, S. et al. Birth outcomes and early growth patterns associated with age at adiposity rebound: the Ma’anshan birth cohort (MABC) study. BMC Public Health 23, 2405 (2023). https://doi.org/10.1186/s12889-023-17236-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-023-17236-9